Back to Journals » OncoTargets and Therapy » Volume 11
Re-biopsy status among Chinese non-small-cell lung cancer patients who progressed after icotinib therapy
Authors Wang H , Zhang L, Si X , Zhang X, Wang M
Received 14 May 2018
Accepted for publication 17 September 2018
Published 26 October 2018 Volume 2018:11 Pages 7513—7519
DOI https://doi.org/10.2147/OTT.S174075
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Geoffrey Pietersz
Hanping Wang, Li Zhang, Xiaoyan Si, Xiaotong Zhang, Mengzhao Wang
Department of Respiratory Medicine, Peking Union Medical College Hospital, Dongcheng District, Beijing 100730, China
Objective: Acquired T790M mutations account for 50%–60% of tyrosine kinase inhibitor (TKI)-resistant mechanisms in EGFR mutation-positive (m+) non-small-cell lung cancer (NSCLC) patients, and re-biopsy is recommended to detect these mutations. We investigated the re-biopsy status and the T790M incidence rate in patients after treatment with icotinib, which is the first-generation EGFR-TKI widely used in China.
Patients and methods: Target patients had EGFRm+NSCLC, who were progressed after icotinib therapy. The primary end point was the re-biopsy rate (number of cases in which re-biopsies were performed successfully/total number of patients progressed after icotinib therapy). Secondary end points included the T790M mutation incidence rate, differences between the first biopsy and re-biopsy, and details of why re-biopsy was not performed in relevant patients.
Results: A total of 77 adenocarcinoma patients were evaluated (median age, 58 years). Tissue re-biopsy was successful in 41 patients (53.2%). Compared with the first biopsy, percutaneous tissue biopsies increased from 51.2% to 70.7% (P=0.008), while bronchoscopy biopsies and the surgical rate decreased from 19.5% to 14.6% (P<0.001) and 17.1% to 7.3% (P<0.001), respectively. Primary lung lesions were more common in the first biopsy than in re-biopsy (80.5% vs 65.9%, P=0.008), but metastatic lesions were more often selected for re-biopsy (14/41 [34.1%], including metastases in the bone, lymph nodes, and liver). The incidence rate of T790M was 56.1% (23/41). The reasons for not performing re-biopsies included lesion sizes and/or locations unsuitable for biopsy (n=17), a positive circulating tumor DNA (ctDNA) result (n=3), patient unwillingness (n=7), older age or severe comorbidity (n=4), and poor health (n=5). No severe complications were found.
Conclusion: In this real-world study, the re-biopsy rate was 53.2% and the incidence rate of T790M mutations was 56.1%. Further efforts are needed to increase the re-biopsy rate in patients who progress after icotinib therapy.
Keywords: re-biopsy, T790M mutation, resistant mechanism, EGFR-TKI, icotinib, non-small-cell lung cancer
Introduction
Lung cancer is the leading cause of cancer death worldwide,1 and the treatment guidance based on genetics has brought great benefits to patients. Some lung cancers are associated with mutations, including EGF gene (EGFR) mutations which are the most common in the Eastern non-small-cell lung cancer (NSCLC) population. Patients who harbor EGFR mutations account for ~50% of NSCLC cases2 and are sensitive to EGFR tyrosine kinase inhibitor (TKI) therapy, with the first-generation EGFR-TKI treatment shown to achieve control in around 1 year.3,4 However, subsequent treatment depends on the mechanism of drug resistance. Acquired T790M mutations account for 50%–60% of the resistance mechanisms and are targeted by the third-generation EGFR-TKIs.5–7 These include osimertinib, which achieved a progression-free survival (PFS) of 10.1 months and an overall response rate (ORR) of 71% in T790M mutation patients.8 To predict whether patients can benefit from osimertinib treatment, it is critical to identify T790M mutations in TKI-resistant patients.
Suitable specimens for EGFR mutation detection include tissue and plasma. Tissue analysis remains the gold standard for the identification of EGFR mutations, with blood used as an effective alternative when tissue specimens are not available.9 However, the rate of re-biopsy to obtain tissue samples is very low in China; hence, more efforts are needed to improve the status of re-biopsy.
The most commonly used first-generation EGFR-TKIs outside China are gefitinib and erlotinib. Icotinib is a widely used Chinese first-generation EGFR-TKI with independent intellectual property rights whose non-inferiority to gefitinib was previously established in the ICOGEN study.10 It is thought to have similar resistance mechanisms to other EGFR-TKIs, but this has not been proven.
This retrospective study analyzed the re-biopsy and T790M mutation statuses of NSCLC patients with EGFR mutations, who were progressed after icotinib therapy between July 2015 and July 2017.
Patients and methods
Patients
Patients with histologically or cytologically determined advanced-stage (stage IIIB or IV) NSCLC with an activating EGFR mutation or patients with a documented prolonged partial response or stable disease (>24 weeks) to icotinib (according to Response evaluation criteria in solid tumors [RECIST] criteria11), who were progressed after icotinib therapy between July 2015 and July 2017 and who had a complete medical record, were retrospectively analyzed. Patients with de novo T790M mutations were excluded.
Details of biopsies, including those performed prior to TKI treatment (pre-TKI biopsy) and/or after TKI treatment (post-TKI biopsy), were collected. Reasons not to perform a post-TKI biopsy were obtained from medical records or by telephone follow-up. The quality of the post-TKI biopsy and the method of mutation detection were determined from the pathological report. Demographic data and details of prior TKI treatments (including time to progress and response to treatment) were collected from medical records.
Biopsies underwent histological assessment using H&E staining. A successful re-biopsy was defined if the number of tumor cells in the specimens exceeded 100 to meet the needs of detecting EGFR mutations.
Methods and results of EGFR mutation detection (especially T790M) were collected from medical records or the pathological department.
For those patients whose plasma circulating free DNA (cfDNA) was analyzed to detect T790M mutations, detailed information about the methods and results of cfDNA analysis was also collected from medical records. This study was approved by the institutional review board of Peking Union Medical College Hospital (approval No. S-K374). The patient consent was not required for this retrospective study, since the subjects cannot be identified directly or through identifiers linked to the subjects.
Data and statistical analyses
RECIST 1.1 criteria were used for response evaluation.11 Survival curves were constructed using the Kaplan–Meier method. Survival data were compared using the log-rank test. The primary end point was the re-biopsy rate (number of cases in which re-biopsies were performed successfully/total number of patients who progressed after icotinib therapy). Secondary end points included the incidence rate of T790M mutations, differences between the first biopsy and re-biopsy as determined by the chi-squared test, and details of why re-biopsy was not performed in relevant patients. IBM SPSS Statistics for Windows software (version 19.0; IBM Corporation, Armonk, NY, USA) was used for statistical analyses.
Results
Patient characteristics
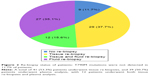
Figure 1 shows the flowchart of patients’ recruitment. A total of 77 adenocarcinoma patients who progressed after icotinib therapy between July 2015 and July 2017 were evaluated (Table 1). The median age was 58 years (range, 36–81 years); 48 patients (62.3%) were females, and 20 (26%) were smokers.
  | Figure 1 Flowchart of patients’ recruitment. |
Initial EGFR mutation status of patients
Initial biopsy specimens were analyzed for primary EGFR mutations by the Scorpion amplification refractory mutation system (ARMS; Qiagen NV, Venlo, the Netherlands) in 75 patients. No tissue biopsy was obtained from the remaining two patients during the initial diagnoses, and their EGFR mutation status was determined by digital PCR of plasma cfDNA (AmoyDx, Xiamen, China).
According to the initial detection, 33 (42.9%) patients had an exon 19 deletion, 40 (51.9%) had an L8585 mutation, and two had uncommon mutations (one had the L861 mutation, and the other had a complex mutation of L861Q+G719X).
Icotinib treatment and its efficacy in patients
Icotinib was used as the first-line therapy in 72 (93.5%) patients, as the second-line therapy in four patients (whose prior first-line therapy was pemetrexed plus cisplatin/carboplatin), and as the third-line therapy in one patient (treated by vinorelbine plus cisplatin as the first-line therapy and pemetrexed as the second-line therapy).
The median PFS of icotinib in the full set of patients was 13.3 months (95% CI: 10.6–16.0 months), the ORR was 57.1% (95% CI: 45.8%–68.4%), and the disease control rate was 97.4% (95% CI: 93.8%–101.0%).
Re-biopsies after progress from icotinib
The general status of re-biopsy is shown in Figure 2. Tissue re-biopsies were successful in 41 patients (41/77, 53.2%), and plasma analysis was successful in 39 patients (39/77, 50.6%). Tissue re-biopsies and plasma analysis were concurrently successfully performed in 12 patients (15.6%). However, nine (11.7%) patients underwent neither tissue re-biopsy nor plasma analysis.
The median interval duration from icotinib progression to first re-biopsy was 1.0 months (range, 0.1–6.0 months). Only two patients accepted chemotherapy before re-biopsies.
Differences in the types and sampling sites of both pre-TKI biopsies and post-TKI re-biopsies in 41 patients are summarized in Table 2. Compared with pre-TKI biopsies, percutaneous tissue biopsies increased from 51.2% to 70.7% (P=0.008), while bronchoscopy biopsies and the surgical rate decreased from 19.5% to 14.6% (P<0.001) and 17.1% to 7.3% (P<0.001), respectively.
Regarding the site of biopsy, primary lung lesions were more common for pre-TKI biopsies than re-biopsies (80.5% vs 65.9%, P=0.008), and metastatic lesions outside the lung were more often selected for re-biopsies (14/41, 34.1%), including metastases in the bone, lymph nodes, and liver.
No severe re-biopsy-associated complications were found. Only one patient had mild hemoptysis, and one patient had mild pneumothorax after percutaneous puncture; both of these were reversible.
ARMS methods (Qiagen NV) were used in 39 patients, and next-generation sequencing (NGS) was used in two patients.
Reasons for unsuccessful tissue re-biopsy
Re-biopsies were unsuccessful after progress after icotinib therapy in 36 patients. The reasons for no re-biopsy included lesion size and/or an unsuitable location for biopsy (n=17), positive circulating tumor DNA (ctDNA) result (n=3), patient unwillingness (n=7), older age or severe comorbidity (n=4), and poor health (n=5).
Plasma cfDNA analysis
The plasma of 39 patients was analyzed for T790M mutations. In 36 non-re-biopsy patients, 27 had their plasma cfDNA analyzed for EGFR mutations instead.
Regarding the methods of cfDNA analysis, droplet digital PCR (ddPCR) technology was used in 22 patients (56.4%), Scorpion ARMS in 14 (35.9%), and NGS in three (7.7%).
T790M mutation status according to tissue/plasma analysis
The results of T790M mutation detection are summarized in Table 3.
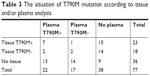  | Table 3 The situation of T790M mutation according to tissue and/or plasma analysis |
Twenty-three of 41 patients were found to have acquired T790M mutations according to tissue re-biopsy. The incidence rate of T790M was 56.1%. Initial EGFR mutations were identified in all re-biopsied tissues.
According to plasma analysis, T790M mutations were found in 22 (56.4%) patients together with their initial EGFR mutation. Initial EGFR mutations conferring sensitivity to EGFR-TKIs were found in cfDNA without T790M mutations in 14 patients. Three patients showed neither initial EGFR mutations nor acquired T790M mutations in their cfDNA.
The total incidence rate of T790M mutations according to both tissue and plasma analysis was 55.9% (38/68).
Among the 12 patients who underwent both tissue re-biopsy and plasma cfDNA analysis, nine had consistent results of T790M mutation status, while three had inconsistent results. Two patients were T790M(−) in their tissue re-biopsy but T790M(+) in plasma analysis. Tissues of both patients were re-biopsied after progression from icotinib, and both were shown to be 19del(+), which is consistent with their initial EGFR mutation status, but T790M(−). Both were then treated with chemotherapy, one with pemetrexed plus cisplatin and avastin, and one with gemcitabine plus cisplatin. Their cfDNA was then analyzed at 10 months and 15 months after icotinib progression, respectively, and shown to be T790M(+). They were both administered osimertinib, and both achieved partial remission. The third patient was shown to be T790M(−) in plasma analysis, then, T790M(+) in tissue re-biopsy 6 months later.
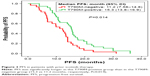
Correlation analysis between T790M mutations and clinical characteristics
Kaplan–Meier analysis showed that the median PFS of prior icotinib therapy in patients with acquired T790M mutations was significantly longer than in patients without acquired T790M mutations (P=0.014; Figure 3). No other clinical characteristics, including sex, age, smoking status, type of initial EGFR mutation, ORR, and disease control rate of icotinib, were found to be associated with the acquired T790M mutation status.
Subsequent therapy of patients with acquired T790M mutations
All 38 patients with acquired T790M mutations were treated by a third-generation EGFR-TKI: three received axitinib and 35 received AZD9291 (some labeled and some unlabeled). The efficacy could not be calculated because of the diversity of treatment.
Discussion
Acquired T790M mutations in EGFR exon 20 account for around 50%–70% of the mechanism of EGFR-TKI resistance. According to the AURA3 trial, osimertinib had a significantly greater efficacy than platinum therapy plus pemetrexed in patients with T790M(+) advanced NSCLC in whom disease had progressed during the first-line EGFR-TKI therapy.8 Therefore, it is important to detect T790M mutations when patients progress from the first-generation TKIs.
T790M mutation detection relies mainly on tissue specimens, although plasma cfDNA detection can also be efficient.12 Indeed, plasma T790M(+) patients showed similar curative effects to tissue-positive patients in the AURA3 trial.8 However, cfDNA detection can give false-negative results, so patients who could potentially benefit from the third-generation TKIs might be missed. Therefore, tissue sample analysis remains the standard method of detecting T790M mutations to guide further treatment,12 although plasma cfDNA detection has rapidly increased in recent years. However, the rate of successful re-biopsy is very low in real-world China.
Among our EGFR-mutated NSCLC patients treated with icotinib, re-biopsies were successful in more than half. Feasibility and safety are the core problems associated with re-biopsy. Patients with recurrence often develop new metastatic lesions outside the thorax or in the peripheral regions of the lung, which are more suited to percutaneous needle biopsy than bronchoscopic mucosal biopsy.13 Even in Japan where bronchoscopies are more widely used for biopsies, their role is being reduced.14 The success of re-biopsy can also be influenced by the heterogeneity of the cancer or prior therapy which may affect the lesions through fibrosis or scarring. In such cases, positron emission tomography–computed tomography (CT) or contrast CT could be helpful for re-biopsy.
In terms of safety, no biopsy-related deaths occurred in our patients, and no serious adverse effects were observed, including mass pneumothorax or large hemoptysis causing unstable hemodynamics. Nevertheless, careful evaluation of the method, site, and safety of re-biopsy was required before it was conducted.
Plasma cfDNA was analyzed for T790M mutations in half of our patients. The accuracy of NGS in China is unsatisfactory because of developments in other detection technologies, so we used ARMS and ddPCR more often than NGS. Both methods showed a good positive rate, which supported the previously reported high accuracy of ddPCR for EGFR mutation detection in plasma and its clinical usefulness in selecting patients who progressed during the first-line EGFR-TKI therapy for treatment with the third-generation TKIs.15,16
A retrospective study that conducted cfDNA analysis on over 200 samples from patients treated with osimertinib from the AURA study found 70% sensitivity for detecting the T790M mutation.17 Outcomes in patients whose plasma proved positive for T790M were equivalent to those seen in patients with positive tissue tests. The study also suggested that, upon the availability of validated plasma-based T790M assays, some patients could avoid a tumor biopsy for T790M genotyping.17 However, the 30% false-negative rate of plasma genotyping indicates that those patients with T790M(–) plasma results still need a tumor biopsy to determine the T790M mutation status. Moreover, pooled AURA extension and AURA2 data demonstrated that the plasma test did not detect the T790M mutation in plasma ctDNA of approximately 40% of patients with a T790M(+) tissue test result.18 A recent study compared T790M mutation detection rates in cfDNA and circulating tumor cells (CTCs) against biopsies in 40 patients. The T790M mutation was found in 75% of biopsies, 70% of CTC samples, and 80% of ctDNA samples, so it was concluded that the various detection methods give similar results.19 Thus, for patients progressing from prior icotinib, cfDNA analysis for T790M mutations could be used first because it is more convenient and noninvasive.20 However, for plasma T790M(–) patients, tissue re-biopsy should be performed as often as possible.
We identified two patients who were negative for tissue T790M mutations but positive for plasma T790M mutations at a later stage. Chemotherapy was administered to both patients during the period from tissue re-biopsy to plasma analysis, so we hypothesized that the observed increase in T790M positivity after chemotherapy might reflect tissue heterogeneity.21 This also indicated that further detection of the T790M mutation status could be helpful in patients shown to be T790M(–) by re-biopsy to identify those with “delayed” T790M mutations. Moreover, cfDNA analysis may be better for dynamic detecting.
Li et al found that patients with secondary T790M mutations at the time of gradual or local progress after acquired resistance to EGFR-TKI benefit more from EGFR-TKI treatment beyond progress compared with those without T790M mutations.22 Our study found a significantly longer prior PFS in T790M(+) patients than in T790M(–) patients. This indicated that acquired T790M mutations might be associated with an improved response to icotinib. However, this should be confirmed in a larger sample size.
The main limitation of this study is its retrospective nature. In addition, we did not include an evaluation of other resistance mechanisms in our re-biopsies, such as MET and HER2 amplifications, mutations in Ros-1, K-ras, BRAF, and PIK3CA, and epithelial-to-mesenchymal transitions,5,6,23,24 thereby limiting our conclusion. Moreover, although T790M mutations were detected in some patients, their subsequent therapies were varied, so the relationship between therapeutic findings and the T790M mutation status could not be properly analyzed.
Conclusion
The re-biopsy rate was 53.2% in this real-world Chinese study, and the incidence rate of T790M mutations was 56.1% in these patients after icotinib therapy. More efforts are needed to increase the re-biopsy rate.
Acknowledgments
We thank our colleagues at the Interventional Radiology Department of Peking Union Medical College Hospital for their hard work in conducting the re-biopsies. We also thank our colleagues at the Department of Pathology of Peking Union Medical College Hospital. We are grateful to the patients for contributing to this study. We also thank Sarah Williams, PhD, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn), for editing the English text of a draft of this manuscript. The abstract of this paper was presented at the 54th American Society of Clinical Oncology conference as publication format with interim findings. The abstract was published in the Journal of Clinical Oncology: http://ascopubs.org/doi/abs/10.1200/JCO.2018.36.15_suppl.e21146.
Disclosure
The authors report no conflicts of interest in this work.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. | ||
Han B, Tjulandin S, Hagiwara K, et al. EGFR mutation prevalence in Asia-Pacific and Russian patients with advanced NSCLC of adenocarcinoma and non-adenocarcinoma histology: The IGNITE study. Lung Cancer. 2017;113:37–44. | ||
Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12(8):735–742. | ||
Fukuoka M, Wu YL, Thongprasert S, et al. Biomarker analyses and final overall survival results from a phase III, randomized, open-label, first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer in Asia (IPASS). J Clin Oncol. 2011;29(21):2866–2874. | ||
Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3(75):75ra26. | ||
Yu HA, Arcila ME, Rekhtman N, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res. 2013;19(8):2240–2247. | ||
Arcila ME, Oxnard GR, Nafa K, et al. Rebiopsy of lung cancer patients with acquired resistance to EGFR inhibitors and enhanced detection of the T790M mutation using a locked nucleic acid-based assay. Clin Cancer Res. 2011;17(5):1169–1180. | ||
Mok TS, Wu Y-L, Ahn M-J, et al. Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung cancer. N Engl J Med. 2017;376(7):629–640. | ||
NCCN. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Non-Small Cell Lung Cancer Version 3; 2018. Available from: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Accessed October 01, 2018. | ||
Shi Y, Zhang L, Liu X, et al. Icotinib versus gefitinib in previously treated advanced non-small-cell lung cancer (ICOGEN): a randomised, double-blind phase 3 non-inferiority trial. Lancet Oncol. 2013;14(10):953–961. | ||
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–247. | ||
Tan DS, Yom SS, Tsao MS, et al. The International Association for the Study of Lung Cancer Consensus Statement on Optimizing Management of EGFR Mutation-Positive Non-Small Cell Lung Cancer: Status in 2016. J Thorac Oncol. 2016;11(7):946–963. | ||
Hasegawa T, Sawa T, Futamura Y, et al. Feasibility of Rebiopsy in Non-Small Cell Lung Cancer Treated with Epidermal Growth Factor Receptor-Tyrosine Kinase Inhibitors. Intern Med. 2015;54(16):1977–1980. | ||
Nosaki K, Satouchi M, Kurata T, et al. Re-biopsy status among non-small cell lung cancer patients in Japan: A retrospective study. Lung Cancer. 2016;101:1–8. | ||
Feng WN, Gu WQ, Zhao N, et al. Comparison of the SuperARMS and Droplet Digital PCR for Detecting EGFR Mutation in ctDNA From NSCLC Patients. Transl Oncol. 2018;11(2):542–545. | ||
Buder A, Hochmair MJ, Schwab S, et al. Cell-Free Plasma DNA-Guided Treatment With Osimertinib in Patients With Advanced EGFR-Mutated NSCLC. J Thorac Oncol. 2018;13(6):821–830. | ||
Oxnard GR, Thress KS, Alden RS, et al. Association between plasma genotyping and outcomes of treatment with osimertinib (AZD9291) in advanced non-small-cell lung cancer. J Clin Oncol. 2016;34(28):3375–3382. | ||
Jenkins S, Yang JC, Ramalingam SS, et al. Plasma ctDNA Analysis for Detection of the EGFR T790M Mutation in Patients with Advanced Non-Small Cell Lung Cancer. J Thorac Oncol. 2017;12(7):1061–1070. | ||
Sundaresan TK, Sequist LV, Heymach JV, et al. Detection of T790M, the Acquired Resistance EGFR Mutation, by Tumor Biopsy versus Noninvasive Blood-Based Analyses. Clin Cancer Res. 2016;22(5):1103–1110. | ||
Santarpia M, Karachaliou N, González-Cao M, Altavilla G, Giovannetti E, Rosell R. Feasibility of cell-free circulating tumor DNA testing for lung cancer. Biomark Med. 2016;10(4):417–430. | ||
Oxnard GR, Arcila ME, Chmielecki J, Ladanyi M, Miller VA, Pao W. New strategies in overcoming acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in lung cancer. Clin Cancer Res. 2011;17(17):5530–5537. | ||
Li W, Ren S, Li J, et al. T790M mutation is associated with better efficacy of treatment beyond progression with EGFR-TKI in advanced NSCLC patients. Lung Cancer. 2014;84(3):295–300. | ||
Ohashi K, Sequist LV, Arcila ME, et al. Lung cancers with acquired resistance to EGFR inhibitors occasionally harbor BRAF gene mutations but lack mutations in KRAS, NRAS, or MEK1. Proc Natl Acad Sci U S A. 2012;109(31):E2127–E2133. | ||
Takezawa K, Pirazzoli V, Arcila ME, et al. HER2 amplification: a potential mechanism of acquired resistance to EGFR inhibition in EGFR-mutant lung cancers that lack the second-site EGFRT790M mutation. Cancer Discov. 2012;2(10):922–933. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.