Back to Journals » Clinical Ophthalmology » Volume 17
Rates of Fellow Eye Macular Hole Development During Long Term Follow-Up
Authors Staropoli PC, Moolani HV, Elhusseiny AM , Flynn HW Jr , Smiddy WE
Received 8 November 2022
Accepted for publication 16 December 2022
Published 5 January 2023 Volume 2023:17 Pages 47—52
DOI https://doi.org/10.2147/OPTH.S394933
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Patrick C Staropoli,1 Harsh V Moolani,1 Abdelrahman M Elhusseiny,2 Harry W Flynn Jr,1 William E Smiddy1
1Department of Ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine, Miami, FL, USA; 2Department of Ophthalmology, Jones Eye Institute, University of Arkansas for Medical Sciences, Little Rock, AR, USA
Correspondence: William E Smiddy, Department of Ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine, 900 NW 17th Street, Miami, FL, 33136, USA, Tel +1 305-302-2704, Fax +1 305-326-6114, Email [email protected]
Purpose: Identify the long-term rate of fellow eye full-thickness macular hole (FTMH) development.
Patients and Methods: In this single site, single provider retrospective consecutive case series, idiopathic FTMH patients who underwent surgery from 2003 to 2014 who also had at least 5 years of follow-up information within our electronic medical record (EMR) which was started in 2014 were identified. Cases with secondary causes (ie, trauma), high myopia, bilateral FTMH on presentation, previous retinal surgery, retinal breaks, or intraocular inflammation were excluded. Demographics, medical and ocular history, refractive error, phakic status, best corrected visual acuity, follow-up duration, surgical technique, single operation anatomic success, and reoperations were recorded.
Results: The rate of fellow eye FTMH was 2.6% (2/77) at 1 year, 5.2% (4/77) at 3 years, 9.1% (6/66) at 6 years, and 9.1% (7/77) as of final follow up. There were 2 cases by year 1, 2 additional cases by year 3, 2 additional cases by year 6, and 1 additional case reported thereafter. The average follow up was 11.1 ± 4.5 years. There was no significant difference in visual outcomes between primary eyes and fellow eyes. There was no significant difference in gender, age, ocular comorbidities, refractive error, phakic status, and visual acuity between the unilateral and bilateral groups.
Conclusion: The rate of FTMH in the fellow eye was low but significant, increased during long-term follow up, and may stabilize after 6 years.
Keywords: macular hole, fellow eye, surgical outcomes, counseling
Introduction
Idiopathic full-thickness macular holes (FTMH) impair central vision and quality of life. Previous studies have shown that individuals with FTMH are at increased risk for subsequent FTMH in the fellow eye compared to the general population.1–5 Depending on the length of follow-up, the rate of FTMH in the fellow eye ranges from 2.8% to 15.6%.1,3,4,6–8
Some reported risk factors for developing FTMH include older age, female gender, myopia, trauma, inflammation, as well as lack of posterior vitreous detachment (PVD), and optical coherence tomography (OCT) features such as outer foveal defect, inner foveal cyst, and vitreomacular adhesion or traction.1,3–5
The incidence of FTMH development in the fellow eye has been reviewed in the literature, but most studies have relatively short follow-up or report long-term rates based on estimates from curve-fit analysis. The current study aims to determine the actual, rather than projected, rate of fellow eye FTMH in a cohort of patients with long-term follow-up data. Secondarily, the cohort was studied for potential risk factors for fellow eye involvement.
Materials and Methods
A retrospective chart review of patients who underwent pars plana vitrectomy for unilateral idiopathic full thickness macular hole by a single provider at a single surgical site was conducted. The University of Miami Miller School of Medicine Institutional Review Board (IRB)/Ethics Committee approval was obtained, and waiver of informed consent was granted as it was not applicable in this retrospective study. The described research adhered to the tenets of the Declaration of Helsinki. The data accessed complied with all relevant data protection and privacy regulations. Patients were identified by searching the electronic medical record (in use since May 1, 2014) for follow-up examination visits on eyes that appeared on the surgical logs from January 2003 through April 2014 with at least 5 years of follow-up. Best corrected visual acuity (BCVA) was recorded pre-operatively, post-operative year 1 (POY1), and POY5. For the purposes of BCVA, a visit within 6 months of the 1-year anniversary of the surgical date was tabulated as POY1; a visit within 1 year of the 5-year anniversary of the surgical date was tabulated as POY5. For the calculation of rate and incidence, the population at different time points was determined by their last known follow up, key exclusion criteria included patients with secondary causes of FTMH (ie, trauma), follow-up less than 5 years, bilateral MH on presentation, lamellar holes or pseudoholes, previous vitreoretinal surgery, retinal tears or detachment, and intraocular inflammation. A FTMH was confirmed by dilated slit lamp biomicroscopy or optical coherence tomography (OCT) (Zeiss, Germany; Heidelberg Engineering Inc., MA, USA). Surgical intervention was conducted by a single provider and included pars plana vitrectomy, inner limiting membrane peel, gas tamponade, and face down positioning for 1 week.
The study population was stratified into two groups: unilateral and bilateral. The unilateral group included patients whose fellow eye did not develop FTMH and the bilateral group included patients whose fellow eye did develop FTMH. These groups were then divided into 2 subgroups: primary eye and fellow eye.
Age, gender, history of diabetes or hypertension, laterality (right or left), past ocular history, refractive error (hyperopia, low myope, high myope), lens status (phakic, pseudophakic, aphakic), single operation anatomic success, tamponade agent (SF6, C3F8), number of reoperations for recurrent or persistent FTMH, preoperative best corrected visual acuity (BCVA), post-operative year (POY) 1 BCVA, POY5 BCVA, final BCVA, and total follow-up were recorded from chart review. In cases of fellow eye involvement, the time from primary eye diagnosis until fellow eye diagnosis was recorded.
Fisher's exact test was used to compare categorical variables, and Mann–Whitney-Wilcoxon test was used to compare groups of quantitative variables. Statistical significance was defined as p < 0.05. Statistical analysis was conducted using R (R Core Team, 2021).
Results
There were 614 FTMHs operated in the study interval. A total of 79 patients were identified as meeting inclusion criteria and having at least 5 years of follow-up information in the EMR. Two patients were then excluded due to ocular trauma (n = 1) or previous vitreoretinal surgery (n = 1), leaving 77 patients included in the study cohort for analysis.
The average age of patients at the time of primary FTMH surgery was 65.9 ± 6.7 years. Females constituted 77% (59/77) of the study cohort. Ocular comorbidities (such as primary open-angle glaucoma, normal tension glaucoma, pseudoexfoliation glaucoma, angle closure glaucoma, ocular hypertension, dry or wet age-related macular degeneration, drusen, epiretinal membrane, non-proliferative diabetic retinopathy, diabetic macular edema, cystoid macular edema, LASIK, strabismus, and amblyopia) were noted in 42.9% (33/77). Only two patients (2.6%, 2/77) had history of LASIK. Neither developed a fellow eye FTMH. Pre-LASIK refractive error was unknown and was therefore omitted. One hundred percent (77/77) of patients were followed up at 1 year, 100% (77/77) at 3 years, and 86% (66/77) at 6 years. There was an average follow-up of 11.1 ± 4.5 years.
The rate of fellow eye FTMH was calculated after one year (2.6%, 2/77), three years (5.2%, 4/77), and six years (9.1%, 6/66) (Table 1). In total, a fellow eye FTMH was identified in seven patients (9.1%, 7/77). There were 2 cases by year 1, 2 additional cases by year 3, 2 additional cases by year 6, and 1 additional case reported thereafter. Figure 1 shows this information in graphical form as a survival curve.
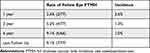 |
Table 1 Rate and Incidence of Fellow Eye FTMH |
 |
Figure 1 Kaplan-Meier Survival Curve of Fellow Eye Involvement Over Time. Probability axis represents the percentage chance of not developing fellow eye involvement. Time axis is depicted in years. |
There were no differences in demographic and past medical history of the unilateral and bilateral group patients in gender, age, or history of hypertension, but diabetes mellitus was less common in the unilateral (14%) than in the bilateral group (67%) (p = 0.047) (Table 2).
 |
Table 2 Demographic and Past Medical History |
There were no statistically significant differences in eye laterality, presence of past ocular history, refractive error, lens status, pre-operative and post-operative BCVA (post-operative year 1 [POY1], POY5), tamponade agent, and follow up (Table 3). There was an increased average number of reoperations for recurrent or persistent FTMH in the primary eye of the bilateral group compared to the primary eye of the unilateral group (0.67 vs 0.31, p = 0.019). There were no differences in past ocular history or refractive status between the unilateral group and the bilateral group.
 |
Table 3 Comparison of the Primary Eyes of the Unilateral and Bilateral Groups |
There were no differences in BCVA comparing the primary eye and fellow eye of bilateral patients at pre-operation, POY1, and POY5 (Table 4). Potential differences were observed in single operation anatomic success in the fellow eye (100%, 7/7) compared to the primary eye (67% 4/6). There was also a potential difference in the number of reoperations for recurrent or persistent FTMH in the fellow eye (0) compared to the primary eye (0.67). However, these differences were not statistically significant (p = 0.19, p = 0.14, respectively).
 |
Table 4 Comparison Between the Primary Eye and Fellow Eye of Patients Who Developed a Fellow Eye FTMH |
Discussion
The current study tabulated the rate of developing a FTMH in the fellow eye as 9.1%, which is much greater than the 0.33% rate of development for a unilateral FTMH in the general population.7 The increased risk observed aligns with previous reports that had similar inclusion and exclusion criteria, but shorter follow-up intervals, with incidences from 2.8% to 15.6%.1,2,4,6–10 A strength of the current study is the average follow-up of 11.1 years while previous reports have follow-up of fewer than 6 years.1–8 For example, Lewis et al previously examined 365 patients with FTMH at our institution and found a 13% rate (n=4/32) of fellow eye involvement at 48 months, but the average follow-up was only 2.6 years.4 This rate was slightly greater than reported in the current study, however this variance could be explained by the smaller patient population.
Papers that reported rates of fellow eye FTMH greater than 20% either conducted a curve-fit analysis to estimate the presumably higher rates at 20–30 years of follow-up5 or included partial thickness holes (ie, macular cysts and lamellar holes) in their analysis.7 The current study does not rely on curve-fit analysis and only included full thickness macular holes.
The other consideration of long-term follow-up is what happens if no surgical action is taken. Casuso et al reviewed 65 cases of non-operated FTMH over a 5-year follow-up. While staging on presentation was split fairly equal (24% stage 2; 37% stage 3; 40% stage 4) most progressed to stage 4 (84%) at final follow-up with vision ranging from 20/200 to 20/400.11 The current study was not designed to evaluate this natural history question. Although spontaneous closure of small MHs has been demonstrated,12 and some providers recommend observation of early, small MHs, this was not the usual practice of the current investigators.
Females constituting most cases of macular holes and possessing a higher rate of fellow eye FTMH development, has been a nearly universal finding in previous reports, possibly due to higher longevity among females.1–4,7,8 The higher rate of fellow eye FTMH in diabetes has not been previously reported but, independently, macular hole surgery presents some unique features in the diabetic eye.13
OCT data, an important element in studying fellow eye pathology, was not included in our study design, largely due to how long ago the study extended (2003–2014). Other, more recently ascertained series have reported strictly on OCT risk factors and found that lack of posterior vitreous detachment (PVD), outer foveal defect, inner foveal cyst, and vitreomacular adhesion or traction can indicate increased risk of fellow eye FTMH.3,14–16 Most of these studies were conducted within the last decade, and so their results are confined to relatively short-term follow up. Examining the influence of OCT-associated risk factors with long term (10 to 20 years) fellow eye FTMH development is an important next step in this research.
The main limitation of the current study is the high rate of patients that did not meet the inclusion criteria (only 77 out of 614 potential cases were included) of having an electronic medical record and at least 5 years of follow up. This could have been due to many patients pre-dating the adoption of EMR, the inability of a patient to return especially if coming from a distance, and the survival rate of an older population.
Conclusion
This single site, single provider, consecutive case series identified the rate of FTMH in the fellow eye to be 9.1% over an average follow-up of 11.1 years. The rate may stabilize after post-operative year 6. These results provide important prognostic and surveillance information to patients and providers.
Funding
This work was partially supported by the Heed Fellowship. The sponsor or funding organization had no role in the design or conduct of this research.
Disclosure
Dr Harry W Flynn Jr reports grants from NIH Center, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Ezra E, Wells JA, Gray RH, et al. Incidence of idiopathic full-thickness macular holes in fellow eyes. Ophthalmology. 1998;105(2):353–359. doi:10.1016/S0161-6420(98)93562-X
2. Bronstein MA, Trempe CL, Mackenzie Freeman H. Fellow eyes of eyes with macular holes. Am J Ophthalmol. 1981;92(6):757–761. doi:10.1016/S0002-9394(14)75625-9
3. Choi JH, Kim KT, Kang SW, Bae K, Lee SE, Kim AY. Development of idiopathic macular hole in fellow eyes: spectral domain optical coherence tomography features. Retina. 2020;40(4):765–772. doi:10.1097/IAE.0000000000002439
4. Lewis ML, Cohen SM, Smiddy WE, Gass JDM. Bilaterality of idiopathic macular holes. Graefes Arch Clin Exp Ophthalmol. 1996;234(4):241–245. doi:10.1007/BF00430416
5. Kumagai K. Percentage of fellow eyes that develop full-thickness macular hole in patients with unilateral macular hole. Arch Ophthalmol. 2012;130(3):393. doi:10.1001/archopthalmol.2011.1427
6. Philippakis E, Astroz P, Tadayoni R, Gaudric A. Incidence of macular holes in the fellow eye without vitreomacular detachment at baseline. Ophthalmologica. 2018;240(3):135–142. doi:10.1159/000488956
7. McDonnell PJ, Fine SL, Hillis AI. Clinical features of idiopathic macular cysts and holes. Am J Ophthalmol. 1982;93(6):777–786. doi:10.1016/0002-9394(82)90474-3
8. Fisher YL, Slakter JS, Yannuzzi LA, Guyer DR. A prospective natural history study and kinetic ultrasound evaluation of idiopathic macular holes. Ophthalmology. 1994;101(1):5–11. doi:10.1016/S0161-6420(94)31356-X
9. James M, Feman SS. Macular Holes. Albrecht Von Graefes Arch Clin Exp Ophthalmol. 1980;215(1):59–63. doi:10.1007/BF00413397
10. Gass JDM. Idiopathic senile macular hole: its early stages and pathogenesis. Arch Ophthalmol. 1988;106(5):629. doi:10.1001/archopht.1988.01060130683026
11. Casuso LA, Scott IU, Flynn HW Jr, et al. Long-term follow-up of unoperated macular holes. Ophthalmol. 2001;108(6):1150–1155. doi:10.1016/S0161-6420(01)00581-4
12. Elhusseiny AM, Smiddy WE, Flynn HW Jr, Schwartz SG. Case series of recurring spontaneous closure of macular hole. Case Rep Ophthalmol Med. 2019;16:2398342.
13. Flynn HW
14. Furashova O, Matthé E. Foveal crack sign as a predictive biomarker for development of macular hole in fellow eyes of patients with full-thickness macular holes. Sci Rep. 2020;10:19932. doi:10.1038/s41598-020-77078-y
15. Lindtjørn B, Krohn J, Forsaa VA. Optical coherence tomography features and risk of macular hole formation in the fellow eye. BMC Ophthalmol. 2021;21(1):351. doi:10.1186/s12886-021-02111-1
16. Chhablani J, Kumar K, Ali TR, Narayanan R. Spectral-domain optical coherence tomography features in fellow eyes of patients with idiopathic macular hole. Eur J Ophthalmol. 2014;24(3):382–386. doi:10.5301/ejo.5000386
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
