Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
Rasagiline for sleep disorders in patients with Parkinson’s disease: a prospective observational study
Authors Schettino C, Dato C, Capaldo G, Sampaolo S, Di Iorio G, Melone MA
Received 5 July 2016
Accepted for publication 4 August 2016
Published 29 September 2016 Volume 2016:12 Pages 2497—2502
DOI https://doi.org/10.2147/NDT.S116476
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Carla Schettino,1,2,* Clemente Dato,1,2,* Guglielmo Capaldo,1,2 Simone Sampaolo,1,2 Giuseppe Di Iorio,1,2 Mariarosa AB Melone1,2
1Department of Medical, Surgical, Neurological, Metabolic Sciences, and Aging, 2Division of Neurology and InterUniversity Center for Research in Neurosciences, Second University of Naples, Naples, Italy
*These authors contributed equally to this work
Introduction: Rasagiline is a selective, irreversible monoamine oxidase B inhibitor that ameliorates the symptoms of Parkinson’s disease (PD) by inhibiting striatal dopamine metabolism. There is also evidence that monoamine oxidase B inhibitors increase melatonin levels in the pineal gland and may have a beneficial effect on sleep disorders, which are a common feature in patients with PD.
Methods: This single-center, prospective, observational, 12-week study compared the effect of combination therapy with levodopa 200–300 mg/d + rasagiline 1 mg/d (n=19) with levodopa 200–300 mg/d alone (n=19) in the treatment of sleep disorders in patients with idiopathic PD.
Results: After 12 weeks’ treatment, mean sleep latency was significantly (P<0.001) lower and the improvement in sleep latency from baseline was significantly (P=0.001) greater in patients receiving levodopa + rasagiline than in patients receiving levodopa alone. Similarly, at the end of the study, the mean total sleep time was significantly (P=0.002) longer and the improvement from baseline in mean total sleep time was significantly (P=0.026) greater in patients receiving levodopa + rasagiline than levodopa alone. There were no significant differences between treatment groups for the mean number of awakenings reported at week 12 nor the change from baseline to week 12 in mean number of awakenings.
Conclusion: Adding rasagiline to levodopa improved sleep outcomes and may be an appropriate option for patients with PD experiencing sleep disorders.
Keywords: Parkinson’s disease, rasagiline, sleep disorders, Parkinson’s disease sleep scale
Introduction
Idiopathic Parkinson’s disease (PD) is often associated with sleep disorders, the most common of which are insomnia, increased daytime sleepiness, restless legs syndrome, and rapid eye movement (REM) sleep behavior disorder.1 Polysomnographic studies have demonstrated that patients with PD experience increased sleep latency, reduced sleep efficiency, and reduced duration of REM sleep.2 Sleep disorders affect approximately two-thirds of patients with PD,3 and these patients are likely to experience a greater severity of nonmotor PD symptoms than those without sleep disorders.4 Unsurprisingly, sleep disorders in patients with PD have a negative impact on quality of life.2
Assessing sleep using traditional instruments (polysomnography) is both costly and time consuming and requires specialized hospital-based settings. Consequently, sleep scales are widely employed in clinical practice. In patients with PD, individual items of the Parkinson’s Disease Sleep Scale (PDSS) accurately distinguish patients from healthy controls, and items of the PDSS have been shown to correlate with polysomnography.5 The PDSS is also useful to assess the severity of sleep disorders in PD, and individual sleep scales can be used to evaluate response to treatment.
The most frequently used PD medications (eg, levodopa and dopamine agonists) show little efficacy in controlling sleep disturbances.6,7 In fact, dopaminergic medication appears to adversely affect sleep continuity; low-dose dopamine agonists are associated with insomnia while higher doses are associated with day-time sleepiness.1,6
Rasagiline is a selective, irreversible inhibitor of monoamine oxidase B (MAOB-I) that ameliorates the symptoms of PD by inhibiting striatal dopamine metabolism.8 MAOB-Is also increase melatonin levels in the pineal gland and may therefore contribute to modulation of wakefulness/sleep patterns and circadian rhythms.9 Rasagiline has been used for many years in the European Union and USA as a first-line treatment for early forms of PD, as well as in combination with levodopa and dopamine agonists in more advanced forms of the disease. Clinical studies with rasagiline have demonstrated that the drug has a good safety profile as monotherapy10 and in combination regimens.11
The aim of this observational study was to compare the efficacy of levodopa + rasagiline with that of levodopa alone in the treatment of sleep disorders in patients with PD.
Methods
Study design and patients
This single-center, prospective, observational study evaluated 38 outpatients with PD experiencing sleep disturbances. The study was performed over 12 weeks from January to June 2015 at the Clinic of Movement Disorders, II Division of Neurology, Second University of Naples, Italy. The study was approved by the Medical Ethical Committee of Second University of Naples and Security Board, and all participants provided written informed consent. Patient privacy was maintained and only the investigator was able to link data to an individual via the identification number assigned at enrollment.
Eligible patients were aged ≥18 years with a diagnosis of idiopathic mild-to-moderate PD (Hoehn and Yahr stage 1–2), according to the United Kingdom Parkinson’s Disease Society Brain Bank Diagnostic Criteria. Patients were also required to be experiencing sleep disturbances (including insomnia, hypersomnolence, vivid dreaming, restless legs, and other sleep-related movement disorders), as reported by the patient (PDSS mean score ≥100) and to be receiving treatment with levodopa (200–300 mg/d) with or without rasagiline (1 mg/d, administered in a single dose at 7 pm). Exclusion criteria included the presence of any primary sleep disorder; any neurodegenerative disease other than PD or any type of dementia (according to Diagnostic and Statistical Manual of Mental Disorders, 4th edition criteria), by physician assessment; pregnancy and/or breast-feeding; and comorbidities that could result in secondary sleep disorders, including congestive heart failure, other serious heart disease, severe liver disease/cirrhosis, severe renal failure/dialysis, severe respiratory failure, severe anemia, hypothyroidism, and diabetes. Cutoff values for comorbidity signs and symptoms were not defined; inclusion or exclusion of a given patient was at the investigator’s discretion.
Treatment and assessments
Patients were randomly assigned to 12 weeks’ treatment with levodopa (200–300 mg/d) or levodopa + rasagiline (1 mg/d).
Patient demographics and characteristics were collected at baseline and included family history, age of onset of PD, stage of disease (Hoehn and Yahr staging), motor symptoms (Unified Parkinson’s Disease Rating Scale III scores), cognitive function (Mini-Mental State Examination and Beck Depression Inventory scale scores) treatments received, and the presence of comorbidities.
The primary end point was improvement in sleep quality based on sleep latency (hours), number of awakenings, and total sleep time (hours) as recorded in autonomously compiled patient sleep diaries. Patients were required to record, within 30 minutes of waking, information on their sleep–wake cycle for the duration of the study. Clinical evaluations, performed at baseline and at the end of the 12-week study period, included the following: general physical, neurological and psychological examination, assessment of adherence to therapy, administration of the Hoehn and Yahr scale, and administration of the PDSS (a decrease in PDSS scores indicates improvement).
Statistical analysis
Given the observational nature of the study, an expected difference between the two treatment groups was not assumed a priori, and so sample size was not calculated.
Descriptive statistical analyses were performed using a general linear model (GLM) to correct for observed variation in baseline features. Data are expressed as means with standard deviation and mean standard error (SE) for the continuous variables. Normal distribution was tested and 95% confidence intervals (CIs) were calculated. Two-tailed t-tests were applied to evaluate statistical significance within groups and significance of between-group difference was based on analysis of variance models (P<0.05).
Results
All 38 patients completed the 12 weeks’ treatment, and key baseline demographics/clinical characteristics are described in the supplementary information (Table S1). Patients had a mean age of 70.3±10.6 years, 56.8% were male, and mean disease duration was 55.9±5.5 months. Baseline characteristics were similar between treatment groups. At baseline, almost all the patients reported difficulties in initiating and maintaining sleep, with correspondingly high PDSS (104.7±21.5 and 103.9±21.8 in the monotherapy and combination therapy groups, respectively). The mean levodopa dose was 267.41 mg/d in the combination group vs 281.7 mg/d in the monotherapy group.
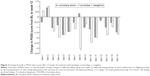
Sleep latency (Figure 1A), number of awakenings (Figure 1B), and total sleep time (Figure 1C) all improved significantly from baseline to week 12 in patients receiving levodopa + rasagiline. In contrast, sleep latency was the only measure to show a significant improvement from baseline to week 12 (Figure 1A) with levodopa alone. At 12 weeks and compared with levodopa alone, patients receiving levodopa + rasagiline had a significantly lower mean sleep latency time (Figure 1A), while the improvement from baseline was significantly greater with levodopa + rasagiline (−0.5474±0.69472 h vs −1.6789±1.20627 h; P=0.001). There was no significant difference between treatment groups for the mean number of awakenings reported at week 12 (Figure 1B) or change from baseline to week 12 (−0.2105±0.41885 vs −0.1579±0.50146; P=0.728). At week 12, mean total sleep time was significantly greater in patients receiving combination treatment than monotherapy (Figure 1C), and the improvement from baseline to week 12 was significantly greater with levodopa + rasagiline than levodopa alone (1.2642±1.62450 h vs 0.3211±0.69648 h; P=0.026).
Applying a GLM to correct for baseline features, the treatment received and the baseline value of each end point were significantly related to variation at week 12. The estimated marginal mean of delta sleep latency was −1.57 (SE: 0.166; 95% CI: −1.906, −1.225) in the levodopa + rasagiline group vs −0.58 (SE: 0.181; 95% CI: −0.954, −0.208) in the levodopa alone group (P=0.001); the estimated marginal mean of delta number of awakenings was −0.36 (SE: 0.086; 95% CI: −0.535, −0.182) and 0.004 (SE: 0.101; 95% CI: −0.203, 0.211), respectively (P=0.013), while the estimated marginal mean of delta total sleep hours was 1.35 (SE: 0.315; 95% CI: 0.701, 1.995) vs 0.30 (SE: 0.362; 95% CI: −0.449, 1.041), respectively (P=0.044).
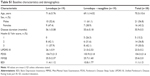
Improvements in PDSS at 12 weeks were greater with combination treatment compared with levodopa alone (Figure 2). A significant reduction in PDSS scores (ie, an improvement in sleep) from baseline to week 12 was observed in six of 15 items in the levodopa alone group (distressing dreams, urine incontinence, limb paresthesia, cramps, tremor, and feeling tired and sleepy) and ten of 15 items (restless limbs, fidgeting in bed, distressing dreams, distressing hallucinations, nycturia, urine incontinence, limb paresthesia, cramps, tremor, and feeling tired and sleepy) in the levodopa + rasagiline group. PDSS scores at 12 weeks were significantly lower with levodopa + rasagiline vs levodopa alone for nycturia (P=0.012) and limb paresthesia (P=0.032), while the change from baseline to week 12 significantly favored levodopa + rasagiline vs levodopa alone for nycturia (P=0.002). Applying a GLM to correct for baseline features, the baseline value of each item was significantly related with variation for 12 of 15 items at week 12.
Discussion
This observational study indicates that the addition of rasagiline to levodopa improves sleep quality in patients with PD experiencing sleep disorders. After 12 weeks’ treatment, sleep latency and total sleep time were significantly more improved in patients receiving combination therapy than in those receiving levodopa alone.
Our findings support those of the randomized, double-blind ACTOR study in patients with PD, which demonstrated that physician-assessed sleep disorders and daytime sleepiness decreased significantly more with rasagiline 1 mg/d than with pramipexole 1.5 mg/d.10
In animal models, it has been shown that inhibition of monoamine oxidase (MAO) also increases melatonin levels in the pineal gland,9 and it is hypothesized that this is how rasagiline may improve sleep disorders in patients with PD. Furthermore, rasagiline lacks amphetamine-like metabolites, and so may confer advantages over other MAOB-Is in the treatment sleep disorders in patients with PD.12
Although the study was prospective, it had a number of limitations including the relatively small number of patients recruited. Furthermore, we restricted our study to subjective symptoms and perception of restfulness using patient sleep diaries and PDSS scores. We accept that detailed assessment of the complex sleep architecture in patients with PD requires additional studies using instrumental techniques that currently are not in common clinical practice (eg, polysomnography), expanding our observations on REM behavior disorder, and periodic limb movement syndrome.
Conclusion
This small monocentric study suggests that rasagiline added to chronic levodopa therapy might provide relevant benefit to patients with PD experiencing sleep disorders. Given the high prevalence of sleep disorders in this population, prospective, randomized studies in more patients and over a longer time period are warranted.
Acknowledgments
We thank Valentina Mirisola (Medi Service, Genoa) for assistance with the statistical analyses and Simone Boniface and Matthew Weitz of Springer Healthcare Communications, for medical writing assistance in drafting and preparing the manuscript for submission. This medical writing assistance was funded by Lundbeck.
Author contributions
Mariarosa AB Melone conceived the various aspects of the work and the study as a whole. Giuseppe Di Iorio critically reviewed the study plan. All authors contributed to enroll the patients. Carla Schettino, Clemente Dato, Guglielmo Capaldo, and Simone Sampaolo were involved in the data acquisition and collectively vouch for the accuracy and integrity of the data. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
Mariarosa AB Melone has received a grant from the Ministry of Education, Universities and Research (MIUR) in Italy under PRIN contract #20109MXHMR_004, unrelated to this research. The authors report no other conflicts of interest in this work.
References
Schrempf W, Brandt MD, Storch A, Reichmann H. Sleep disorders in Parkinson’s disease. J Parkinsons Dis. 2014;4(2):211–221. | ||
Breen DP, Vuono R, Nawarathna U, et al. Sleep and circadian rhythm regulation in early Parkinson disease. JAMA Neurol. 2014;71(5):589–595. | ||
Tandberg E, Larsen JP, Karlsen K. A community-based study of sleep disorders in patients with Parkinson’s disease. Mov Disord. 1998;13(6):895–899. | ||
Neikrug AB, Maglione JE, Liu L, et al. Effects of sleep disorders on the non-motor symptoms of Parkinson disease. J Clin Sleep Med. 2013;9(11):1119–1129. | ||
Dhawan V, Dhoat S, Williams AJ, et al. The range and nature of sleep dysfunction in untreated Parkinson’s disease (PD). A comparative controlled clinical study using the Parkinson’s disease sleep scale and selective polysomnography. J Neurol Sci. 2006;248(1–2):158–162. | ||
Park A, Stacy M. Dopamine-induced nonmotor symptoms of Parkinson’s disease. Parkinson’s Dis. 2011;2011:485063. | ||
Trotti LM, Bliwise DL. Treatment of the sleep disorders associated with Parkinson’s disease. Neurotherapeutics. 2014;11(1):68–77. | ||
Lecht S, Haroutiunian S, Hoffman A, Lazarovici P. Rasagiline – a novel MAO B inhibitor in Parkinson’s disease therapy. Ther Clin Risk Manag. 2007;3(3):467–474. | ||
King TS, Richardson BA, Reiter RJ. Regulation of rat pineal melatonin synthesis: effect of monoamine oxidase inhibition. Mol Cell Endocrinol. 1982;25(3):327–338. | ||
Viallet F, Pitel S, Lancrenon S, Blin O. Evaluation of the safety and tolerability of rasagiline in the treatment of the early stages of Parkinson’s disease. Curr Med Res Opin. 2013;29(1):23–31. | ||
Parkinson Study Group. A randomized placebo-controlled trial of rasagiline in levodopa-treated patients with Parkinson disease and motor fluctuations: the PRESTO study. Arch Neurol. 2005;62(2):241–248. | ||
Youdim MB, Gross A, Finberg JP. Rasagiline [N-propargyl-1R(+)-aminoindan], a selective and potent inhibitor of mitochondrial monoamine oxidase B. Br J Pharmacol. 2001;132(2):500–506. |
Supplementary material
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.