Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
Quantitative and Qualitative Research on Management Strategies for Dyspnoea in Elderly Patients with Coronary Heart Disease Complicated with Chronic Heart Failure
Authors Niu YN, Li R, Zhao P, He P, Li YL, Wang Y
Received 13 June 2022
Accepted for publication 30 August 2022
Published 10 September 2022 Volume 2022:15 Pages 2007—2013
DOI https://doi.org/10.2147/JMDH.S378379
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ya-Nan Niu,1,* Rui Li,2,* Pei Zhao,1 Piao He,1 Yan-Ling Li,2 Yun Wang3
1Department of Spine Surgery, Affiliated Hospital of Hebei University, Baoding, People’s Republic of China; 2Department of Tuberculosis, Affiliated Hospital of Hebei University, Baoding, People’s Republic of China; 3Department of Nursing, Xingtai Medical College, Xingtai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yun Wang, Department of Nursing, Xingtai Medical College, No. 618 Iron and Steel North Road, Xindu District, Xingtai City, Hebei Province, 054000, People’s Republic of China, Tel +8613703120786, Email [email protected]
Objective: To investigate the most effective strategies for the management of dyspnoea in elderly patients with coronary atherosclerotic heart disease (CHD) complicated with chronic heart failure (CHF).
Methods: The best management plans for dyspnoea were evaluated using quantitative and qualitative research techniques for a total of 120 senior patients with CHD complicated with CHF. A self-made questionnaire on dyspnoea management strategies served as the survey instrument for the cross-sectional quantitative investigation. A phenomenological approach served as the framework for the qualitative study, which involved semi-structured interviews with 12 elderly patients who had CHD complicated by CHF. Data were gathered through audio recordings, and the Colaizzi method was used to analyse the data.
Results: A data analysis of the qualitative research results revealed the four strategies for dyspnoea management that were most effective: using drugs, inhaling oxygen, staying in a comfortable position and maintaining air circulation. These were consistent with the most effective strategies identified by the quantitative findings. There was no significant difference in the choice of dyspnoea management strategies for men and women (t = 0.968, P = 0.806); patients tended to use multiple integrated strategies to manage dyspnoea.
Conclusion: Health care providers should consider employing individualised combinations of dyspnoea management strategies to assist elders with CHD complicated with CHF during acute exacerbations of dyspnoea.
Keywords: elderly people, CHD complicated with CHF, dyspnoea, management strategies, quantitative research, qualitative research
Introduction
Coronary atherosclerotic heart disease (CHD), referred to as coronary heart disease, is a common cardiovascular disease in the elderly, mainly due to the imbalance of coronary blood flow and myocardial demand caused by organic coronary lesions.1 Chronic heart failure (CHF) is a critical end-complication and comorbidity of CHD in the elderly, and it is also the main cause of repeated hospitalisation and even death in the elderly aged 60 and above.2 The prominent clinical manifestations of CHF are dyspnoea, respiratory muscle weakness and decreased cardiopulmonary exercise tolerance, which seriously affects patients’ daily lives and causes a great waste of medical resources.2,3 Therefore, the management of dyspnoea is very important.
Traditionally, medical personnel have implemented health education interventions for patients with dyspnoea according to established medical guidelines. The drawback of these interventions include the possibility of ignoring the individual characteristics of patients, prolonging the duration of attacks and increasing the fear and helplessness of patients.4 Because individuals experience exacerbations of dyspnoea differently, the strategies for managing dyspnoea that are considered to be most effective vary from person to person. The purpose of this study was to understand the coping strategies of elderly patients with CHD and CHF when they had dyspnoea and to provide a reference for medical staff to assist patients in implementing an individualised management model.
Method
Study Population
A combination of objective sampling and convenience sampling was used to select as the research participants 120 elderly patients with CHD complicated with CHF who were hospitalised in the Department of Cardiovascular Medicine at a tertiary hospital in Baoding from January to December 2021. There were 48 males and 72 females aged 71.6 ± 7.4 years. Inclusion criteria: ① conformed to the clinical diagnosis of CHD,5 ② aged ≥ 60 years, ③ diagnosed with CHF,2 ④ had clear consciousness and were able to express their wishes and ⑤ provided informed consent and participated voluntarily. Exclusion criteria: ① cognitive impairment; ② serious liver, kidney, lung or other important organ dysfunctions; ③ combined malignant tumours; ④ chronic diseases such as severe hypertension, arrhythmia, diabetes or anaemia; and ⑤ pacing installation equipment, cardiopulmonary resuscitation or electrical defibrillation. This study has been reviewed by the hospital’s ethics committee. A total of 130 questionnaires were distributed, and 120 valid questionnaires were recovered (four cases refused to respond because of a physical inability to adapt, and six questionnaires were omitted because of missing items). The effective rate of questionnaire recovery was 92.3%. General information of the patients is presented in Table 1.
 |
Table 1 Demographic and Clinical Characteristics of Study Subjects (n=120) |
Quantitative Study
General Information of Research Subjects
The medical records of all subjects were examined, and clinical data was collected, including demographic and clinical characteristics such as age, gender, education, marital status, religious beliefs, monthly income, comorbidities, medication use, oxygen use and smoking history.
Dyspnoea Management Strategies Questionnaire
The “Dyspnoea Management Strategies Questionnaire” was self-compiled and prepared based on relevant domestic and international literature6,7 and consultations with experts in cardiology and respiratory departments to evaluate the preferred coping strategies of the research subjects when dyspnoea occurred. The questionnaire included 30 common dyspnoea management strategies and patients’ perceptions of the effectiveness of each strategy. The effectiveness of each patient’s selected management plan was evaluated on a scale from 0% to 100%; as the study’s main focus was perceived effectiveness rather than the total score, an average for each item was calculated rather than a total score. The questionnaire’s internal consistency measure, Cronbach’s value, was 0.832, its test-retest reliability coefficient was 0.811 and its content validity index (CVI) was 0.819.
Quality Control
(1) Before filling out the questionnaire, the requirements were explained in a unified guideline and filled out anonymously. (2) After the questionnaires were completed, researchers collected them and immediately checked if there were missing items and dealt with them accordingly. Any blank and missing items were eliminated to maintain validity. (3) For research subjects who had difficulty writing, the researcher read the questionnaire items and options one by one, assisted the subjects in filling them out and strictly avoided any subjective guidance. (4) The data were checked and entered by two people to ensure accuracy.
Data Analysis and Data Processing
SPSS 25.0 statistical software was used for statistical analysis of the data, and P < 0.05 was considered statistically significant. All continuous variables were described by means and standard deviations, and categorical variables were described by numbers and percentages. Group differences were analysed by two independent sample t-tests.
Qualitative Research
Research methods
The interpretive phenomenological research method8 was used to select 12 typical subjects from the quantitative research data for semi-structured, in-depth interviews. Prolonged verbal communication and activities tend to exacerbate dyspnoea, so written open-ended questions were used instead of lengthy face-to-face interviews. Respondents were given a limited time to write an answer to the open-ended question: “When you have sudden shortness of breath and increased difficulty breathing, what is the most effective way to relieve it?”
Quality Control
(1) Researchers created an interview outline, made an appointment with the interviewee for a time and place, and recorded the interview after obtaining the interviewee’s consent. (2) The interview was one-on-one, and the time was approximately 40–60 minutes. (3) During the interview, researchers did not interrupt the interviewee’s speech and did not express any opinions with personal emotions. (4) The interviews of each group were terminated when the information was saturated. All of the collected data were analysed using the Colaizzi method.9
Result
Quantitative Research Results
Study Subjects’ Chosen Management Strategies for Dyspnoea
The results in Table 2 show that among the 30 dyspnoea management strategies, the top three most selected by patients were inhaling oxygen (102 cases, 85.0%), maintaining air circulation (96 cases, 80.0%) and using drugs (94 cases, 78.3%). The top five most selected by male patients were inhaling oxygen (42 cases, 87.5%), maintaining air circulation, staying in a comfortable position, moving slowly and immediately slowing down activity (each mentioned in 40 cases, 83.3%). The top four options for female patients were inhaling oxygen (60 cases, 83.3%), maintaining air circulation (56 cases, 77.8%), using drugs and preparing for the event (52 cases each, 72.2%). Table 2 lists 11 dyspnoea management strategies. When dyspnoea attacks occurred, 50% or more of patients chose these strategies.
 |
Table 2 Study Subjects Selected Dyspnea Management Strategies and Perceived Effectiveness |
Average Number of Dyspnoea Management Strategies Used by Study Subjects
During an episode of dyspnoea, research subjects usually employed a combination of strategies. The average number of management strategies used by male patients to cope with dyspnoea was 9.85 ± 1.92, and the average number of management strategies used by female patients to cope with dyspnoea was 11.53 ± 1.65. The difference was not statistically significant (t = 1.765, P = 0.643). See Table 3.
 |
Table 3 Average Number of Study Subjects Choosing Dyspnea Management Strategies |
Average Number of Dyspnoea Management Strategies Considered Most Effective by Study Subjects
The average number of dyspnoea management strategies considered most effective by study subjects was 6.93 ± 4.85. The average number for male patients was 7.12 ± 4.64, and the average number for female patients was 6.86 ± 4.75. There was no significant gender difference in the selection of the most effective dyspnoea management strategy (t = 0.968, P = 0.806). See Table 4.
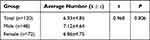 |
Table 4 Average Number of Dyspnea Management Strategies Considered Most Effective by Study Subjects |
Study Subjects’ Ranking of the Most Effective Dyspnoea Management Strategies
Table 5 shows patients’ ranking of dyspnoea management strategies. Pursed-lip breathing has always been regarded as an effective method for the treatment of worsening dyspnoea; it ranked seventh in this study.
 |
Table 5 Ranking of the Most Effective Dyspnea Management Strategies Considered by Research Subjects |
Qualitative Research Results
The data analysis shows four main strategies for dyspnoea management, which were extracted and summarised: using drugs, inhaling oxygen, staying in a comfortable position and changing breathing patterns. This was similar to the most effective strategies identified by the quantitative research results. Changing the breathing pattern refers to consciously changing the breathing pattern during an episode of dyspnoea, including “pursed lip breathing”, “deep breathing”, “concentrating on breathing through the nose for a few minutes” and “shortening the breathing time”. These strategies were determined from the observation of the patients’ long-term repeated experiences of dyspnoea from the nursing care process of the medical staff. Some patients reported that they were dependent on oxygen inhalation. For example, Patient A felt safe when inhaling oxygen. Once the oxygen was removed, the patient’s blood oxygen level dropped, which is life-threatening. Patient D wore an emerald Avalokitesvara Bodhisattva on his body. Although it was only for psychological effect, the patient said that the Bodhisattva gave him a sense of security when he was hospitalised, which has not been mentioned in other studies. Healthcare providers should try to understand the importance of each strategy being used by a patient and the implications behind it. Strategies for maintaining air circulation that were included in quantitative studies were not addressed in qualitative studies.
Discussion
Patients with CHF typically seek medical attention for dyspnoea. Dyspnoea is a prevalent symptom of CHF, as evidenced by the fact that 89.5% of patients with the condition have experienced it.10 The patient’s ability to tolerate activities gradually declines as a result of long-term dyspnoea, and the patient’s physical, psychological and social well-being are all severely impacted.11 For these reasons, dyspnoea self-management is crucial. The focus of medical staff should be on a thorough evaluation of the patient’s dyspnoea and assistance in implementing the necessary interventions to reduce the symptoms of dyspnoea and enhance the patient’s clinical condition.
During the onset of dyspnoea, all study subjects usually chose a combination of multiple coping strategies. Although the second-ranked management strategy in the quantitative study was oxygen inhalation, only 62 (51.7%) of the participants used oxygen at home. While pursed-lip breathing and relaxation techniques are generally considered the most clinically effective way to assist patients in managing dyspnoea, pursed-lip breathing was surprisingly ranked seventh out of the top 10 strategies. The results of one study showed that a diaphragmatic breathing retraining intervention showed preliminary results in increasing physical activity and functional status in patients with CHF but did not reduce dyspnoea as originally expected.12 Therefore, the collaboration between CHF patients and health professionals and the therapeutic effect of the individualised selection of dyspnoea management strategies need to be further explored.
Qualitative research on patients’ self-selected dyspnoea management techniques is scarce. In this study, patients’ preferred methods for managing their dyspnoea were drug use, oxygen inhalation, maintaining a fixed posture and altering breathing patterns. When patients experience dyspnoea, they feel it, relieve it and look for and employ different strategies to treat it in a problem-solving manner. In this qualitative study, all 12 patients used drugs and oxygen. They hoped that the nursing staff would provide drugs and oxygen treatment in time when they felt breathing difficulties, even if the nurse was very busy. This may be because when a patient has difficulty breathing, the most important thing is to solve their physical discomfort. For patients, the function of nursing staff is obviously not fully clear, so nursing staff should spend more time with patients, listen to their needs, understand their thoughts and feelings, provide more psychological support and truly implement patient-centred care. Hong et al13 carried out mindfulness-based decompression training combined with dyspnoea assessment by bending over in elderly patients with CHF, which improved the cardiac function and negative emotions of the patients; therefore, this strategy may be promoted in clinical practice.
Additionally, there were no gender difference in the management options for dyspnoea in this study, which contrasts with the findings of research in the international literature and may be explained by the study’s small sample size and hardly discernible male-female ratio. Gender variations in the selection of appropriate management options for dyspnoea and the rise in the number of female patients with CHF highlight the need for additional discussion.
Conclusion
When elderly patients with CHD complicated with CHF experience dyspnoea, using drugs, inhaling oxygen, staying in a comfortable position and maintaining air circulation may be effective coping strategies, but personalised measures also need to be considered.
Abbreviations
CHD, coronary atherosclerotic heart disease; CHF, chronic heart failure.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Affiliated Hospital of Hebei University.
Written informed consent was obtained from all participants.
Acknowledgments
Ya-Nan Niu and Rui Li are co-first authors for this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Fund Project and Number: S&T Program of Hebei (192777102D). The funding agency did not play a role in study design, data collection, analysis and interpretation, and manuscript writing.
Disclosure
All of the authors had no any personal, financial, commercial, or academic conflicts of interest in this work.
References
1. Jingjing M, Lichun Z, Ping L, et al. Application effect of exercise rehabilitation nursing in elderly patients with coronary heart disease and chronic heart failure. Integr Chin Western Med Nurs. 2018;4(5):130–133.
2. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18(8):891–975. doi:10.1002/ejhf.592
3. Tang Q, Wang Y, Li K. Zhenwu decoction for chronic heart failure: protocol for a systematic review and meta-analysis. Medicine. 2018;97(29):e11559. doi:10.1097/MD.0000000000011559
4. Lixia W, Haixia Z. Effects of specific nursing intervention based on health education on depression and serum cortisol levels in patients with coronary heart disease and heart failure during convalescence. China Prim Med. 2015;22(02):305–307.
5. Zheng Y, Yu B, Alexander D, et al. Associations between metabolomic compounds and incident heart failure among African Americans: the ARIC Study. Am J Epidemiol. 2013;178(4):534–542. doi:10.1093/aje/kwt004
6. Xunyu S. The Effect of Fast Breathing and Slow Breathing Qi Muscle Training on Exercise Tolerance in Patients with Chronic Heart Failure [master’s thesis]. Jiangsu, Suzhou: Soochow University; 2016.
7. Qianqian S. The Application of Symptom Management Education in the Core Symptom Cluster of Patients with Lung Cancer Chemotherapy [master’s thesis]. Henan, Zhengzhou: Zhengzhou University; 2019.
8. Minichiello V, Aroni R, Timewell E. In-Depth Interviewing. Mel-bourne: Longman; 1995:138–152.
9. Colaizzi PF. Psychological Research as the Phenomenologist Views It. Oxford: Oxford University Press; 1978.
10. Chaoqun W, Linfang Z. Research status of respiratory training in patients with chronic heart failure. Nurs Res. 2021;35(3):437–441.
11. Lin C, Guanghui C. The effect of nursing intervention on cardiac function in elderly patients with coronary heart disease and heart failure. Bethune Med J. 2016;14(4):516–518.
12. Seo Y, Yates B, Pozehl B, et al. Diaphragmatic breathing retraining intervention to improve dyspnea, physical activity, and functional status in heart failure patients. Circulation. 2014;130(12):A15524.
13. Hong X, Xiaosu N, Chenling S, et al. Effects of mindfulness-based stress reduction training combined with assessment of leaning over dyspnea on negative emotions and cardiac function in elderly patients with chronic heart failure. Qilu J Nurs. 2021;27(9):82–84.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
