Back to Journals » Open Access Journal of Contraception » Volume 11
Quality of Long-acting Reversible Contraception Provision in Lomé, Togo
Authors Weidert K, Tekou KB , Prata N
Received 17 April 2020
Accepted for publication 2 August 2020
Published 23 September 2020 Volume 2020:11 Pages 135—145
DOI https://doi.org/10.2147/OAJC.S257385
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Igal Wolman
Karen Weidert,1 Koffi B Tekou,2 Ndola Prata1
1Bixby Center for Population, Health and Sustainability, School of Public Health, University of California at Berkeley, Berkeley, CA, USA; 2Centre d’Evaluation et de Suivi du Groupe de Recherche et d’Appui en Santé et Education de la Population, Lomé, Togo
Correspondence: Ndola Prata
School of Public Health, University of California at Berkeley, 6142 Berkeley Way West, Berkeley, CA 94720-6390, USA
Tel +1510643-4284
Email [email protected]
Context: Provision of high-quality contraceptive counseling and services is essential to ensure family planning (FP) programs are rights-based and voluntary. Togo’s modern contraceptive use has steadily increased with almost a quarter of the method mix attributed to long-acting reversible contraceptives (LARC). The purpose of this study is to assess the quality of LARC provision in Togo.
Methods: Data for this study were collected in 2016 as part of a larger research study conducted in Lomé, Togo to assess the effectiveness of the ongoing FP service delivery model. Quality of FP service was assessed in terms of program capacity and program performance. Program capacity was measured with five individual variables and program performance was measured with the Method Information Index (MII). Descriptive statistics and mixed effects models were used to assess likelihood of LARC uptake.
Results: Of the 669 clients included in the study, 19.4% received a LARC method. Multivariable results show that LARC uptake is significantly associated with supervisory visit at the facility in the last three months (program capacity indicator) (OR 1.44; 95%CI 1.48– 2.39) and is twice as likely for those with a positive MII score, even after controlling for provider and client characteristics (OR 2.1; 95%CI 1.61– 2.51).
Conclusion: This study identified supervisory visits and comprehensive contraceptive counseling as the key quality factors positively associated with uptake of LARC. Continued focus on quality of care and provider–client information exchange is necessary to ensure women’s FP needs are met.
Keywords: LARC, Togo, method information index, FP services, quality
Background
Concerted investments in family planning (FP) programs over the last decade have resulted in substantial progress in meeting women’s and men’s reproductive needs in Sub-Saharan Africa (SSA), including Francophone West Africa. The creation of the Ouagadougou Partnership in 2011, unifying nine member countries (Benin, Burkina Faso, Côte d’Ivoire, Guinea, Mali, Mauritania, Niger, Senegal and Togo) under a shared vision and common goal of reducing the high percentage of women dying during pregnancy and childbirth, has been a large driver of success in the member countries.1,2 This renewed regional focus on FP was critical given that Francophone West African countries have some of the highest fertility rates in the world, with an average of 5.5 births per women when the Ouagadougou Partnership was created.2
However, despite impressive gains in new contraceptive users in the West Africa region since 2011, increased contraceptive access and acceptance requires more effort on both the demand and supply sides to ensure the specific FP needs of women and men, including adolescents, are met.3 Between 2015 and 2018, the number of women using modern contraceptive methods grew by 1.4 million in the Ouagadougou Partnership countries. However, another 817,000 women must elect to take up modern methods to reach the Ouagadougou Partnership 2020 target of 2.2 million additional users set by Ministers of Health of the member countries in December 2015. Even if that goal is met, at least eight million women will still have an unmet need for modern contraception in the nine countries.4
In Togo, 35% of pregnancies are unintended5 and the total fertility rate (TFR) is 4.8, with large differences between rural and urban communities: TFR of 3.5 in Lomé compared to 6.0 in the Savanna region.6 In the 2017–2018 FP 2020 progress report, the modern contraceptive prevalence rate (mCPR) was 24.7% among all women, and unmet need was 33.7% among married women in Togo.6 The modern method mix is comprised of the following: male condom (32.3%); injectable (30.5%); implants (20.4%); pill (11.4%); intrauterine device (IUD) (3.6%); female sterilization (1.2%); and other modern methods (0.6%).6 Yet due to higher demand and more common use of contraception, Togo is considered to be entering a period where rapid growth in mCPR is possible with heightened focus on ensuring contraceptive availability, high-quality services, and continued demand generation.7
To capitalize on the opportunity for rapid growth in mCPR while also safeguarding reproductive autonomy, Togolese women should receive counseling on the full range of contraceptive methods and side effects to allow them to make informed choices about which methods best meet their reproductive health needs. For some women and couples who want to limit or space for at least two years, the method of choice would be long-acting reversible contraceptives (LARCs), such as IUD and subdermal implants, which offer the highest level of reversible protection against pregnancy.8,9 They are safe and effective for a longer period of time (3–12 years) than more commonly used methods, such as pills and injectables.8,10,11 It is important to note that although LARC methods are highly effective, overemphasis on LARC may reduce women’s reproductive autonomy; and therefore, the focus should be on comprehensive contraceptive counseling.12
Despite the popularity of short-acting methods such as hormonal injections and pills among FP users in SSA, several studies have also demonstrated that when women are able to choose among a wide range of contraceptive options, significant proportions choose LARC methods.13–17 In Togo, demand for LARC at mobile outreach events in rural communities was found to be very high, with many women receiving services choosing a LARC method when the full range of contraceptive options were available. Additionally, 20% of mobile service clients had previously used, but discontinued, a short-acting method.18 By offering a wider range of FP methods to rural women, they opted to choose a LARC method, which better suited their needs.
Providing women with a choice of contraceptive methods and high-quality counseling are essential components of rights-based FP19 and two key elements in Bruce’s Quality of Care Framework.20 When she first presented her framework in 1990, Bruce made a case for more attention to quality of FP services.20 Two decades later, there is growing evidence on the association between quality of FP services and method uptake and continuation to substantiate Bruce’s framework,21–24 yet there is limited recent data to understand the specific aspects of quality associated with uptake and continuation, especially in low and middle-income countries (LMICs).22,25 A systematic review of the evidence on factors determining the quality of care in FP services in Africa concluded that there was no strong evidence from which to make recommendations and called for future studies in this area.26
The purpose of this paper is to assess whether quality of FP service provision affects LARC uptake among urban and peri-urban FP clients in Lomé, Togo. Since the provision of LARC methods requires more interaction with facilities and clinical providers, we hypothesize that quality of services might be related to LARC uptake. A recent study found that though contraceptive use is increasing in many parts of SSA, LARC is still underutilized and lagging behind short-term methods, especially in West and Central Africa.27 Their findings underscored the need to address various barriers to the uptake of LARC methods in SSA and the authors suggested that programmatic intervention for expansion of LARC methods, particularly across West and Central Africa, may be a promising way to support the achievement of the goals of FP 2020. Insights from assessing quality of services and LARC uptake in this study may highlight key modifications needed to support better LARC access for women and couples. The findings of this study will provide evidence on the quality of FP programs and how it relates to LARC adoption in Togo, as well as identify the most important factors associated with quality of services, with broader implications for Francophone West Africa.
Methods
Study Design
This study is part of a larger operations research that was conducted in Lomé, Togo to assess the effectiveness of the FP service delivery model of the Agir pour la Planification Familiale (AgirPF) program implemented by EngenderHealth and its partners and funded by the US Agency for International Development (USAID)/West Africa.28 AgirPF was a five-year program (2013–2018) designed to expand women’s access to and use of FP services in five West African countries, including Burkina Faso, Cote d’Ivoire, Mauritania, Niger, and Togo. AgirPF aimed to enable individuals and couples to make, and act on, voluntary informed decisions about FP. It was implemented in selected urban and peri-urban areas across the five countries with intervention activities that aimed to address gaps in FP providers’ training, inconsistent availability of contraceptive supplies, and structural flaws in existing health care systems.29 The operations research employed a quasi-experimental design with a nonequivalent control group to assess the relative effectiveness of the AgirPF service delivery model, comparing intervention sites and controls (nonintervention areas). As illustrated in Figure 1, both intervention and nonintervention areas registered increases in contraceptive prevalence from baseline data collection conducted between March and June 2014 and operations research in August 2016 (data from households surveys). The difference-in-difference analysis is statistically significant (p=0.005) suggesting that the AgirPF model was more effective in increasing overall contraceptive prevalence as compared to nonintervention areas. Figure 2 also shows a varied contraceptive method mix between intervention and nonintervention areas (data from household surveys).
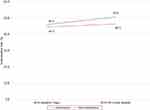 |
Figure 1 Trends in contraceptive use in intervention and nonintervention areas between baseline household data collection in 2014 and operations research in 2016 in Lomé, Togo. |
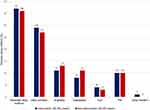 |
Figure 2 Contraceptive method mix in intervention and nonintervention areas based on household data collected during operations research in August 2016 in Lomé, Togo. |
Data Collection
For the operations research, 11 intervention health facilities and five control health facilities were randomly selected from the baseline study conducted prior to implementation of AgirPF in Togo. The sites selected comprise 50% of the baseline sites.28,29 Across the 16 facilities, the following data were collected: 16 facility audits, 47 provider interviews, 1094 nonparticipatory observations of client–provider interactions and 1089 client exit interviews. Facility audits were used to capture facility infrastructure, availability of contraceptives, and frequency of stock outs; observations of client–provider interactions provided data on technical competence of provider, and the availability and correct use of equipment and materials required for the consultation; client exit interviews provided information on perceptions related to respectful treatment, quality of counseling, choice of methods, satisfaction with services, as well as sociodemographic characteristics of the clients; provider surveys collected data on provider characteristics, qualifications, training received, confidence in training, service delivery environment, perceived challenges, and recommendations for improvements.
This study is a secondary data analysis using facility data (only women attending facilities in intervention and nonintervention areas) collected during operations research when the modern contraceptive prevalence was not statistically significantly different between intervention and nonintervention clinics (modern CPR 62.2% vs 56% respectively p=0.285). The focus is on women receiving modern contraceptive method and not any method, as women visiting a facility for FP tend to seek modern methods. A study from Lomé found that women’s preferences for contraceptive methods were as follows in descending order: progestin injections, IUDs, Norplant (levonorgestrel), pills and spermicides.30
Study Sample
Our initial analytic sample included a total of 1089 women who participated in FP consultation/services and completed a client exit interview. From that sample, we excluded 420 women who either reported a reason for the visit which was not related to wanting a contraceptive method to prevent pregnancy or did not receive a contraceptive method that day (mostly due to referrals). Thus, the final sample included a total of 669 women who visited the study clinic sites to obtain a contraceptive method, received a modern method that day, and consented to the client exit interview.
Variable Definitions
Quality of care is measured through diverse indicators, which often interact with other factors to affect a range of program outcomes. For this study, we were specifically interested in uptake of LARC as an outcome variable. The independent variable, quality of FP services, was assessed in terms of (1) program capacity; and (2) program performance. Program capacity was measured using the following five variables: availability of contraceptive methods at the facility; provider participation in an in-service training two years prior to the survey; provider reported restrictions in providing contraceptive methods based on client characteristics (ie, parity, age, marital status); facility-level reports of supported supervision three months prior to survey; and availability of equipment necessary for FP service provision.
Program performance was assessed using the Method Information Index (MII), which is calculated from contraceptive users’ responses to three questions on information given to them by their provider about their chosen method of contraception: (1) were you informed about other methods? (2) Were you informed about side effects? (3) Were you told what to do if you experienced side effects?22,31 The index, ranging from 0–3, was used as a binary variable (three or less than three). These data were collected from the client exit interviews that were administered directly after the FP consultation by trained enumerators in a private location at the facility.
Table 1 provides more detailed information for each of the variables used to construct the quality measures. Client characteristics (age, marital status, number of living children, education, and wealth terciles) and provider characteristics (age and professional category—midwife vs other mid-level clinical providers, such as nurse and physician assistant) were also identified as covariates of interest.
 |
Table 1 Description and Source of Data for Study Outcome and Independent Quality of Service Variables |
Data Analysis
All analyses were run in StataIC, version 15.32 For this analysis, we focus on clients who received a modern method during an FP consultation on days when survey data collection took place. Descriptive statistics explored the associations between covariates of the sample population and providers and the primary outcome. A bivariate analysis to assess clients’ key sociodemographic variables and LARC uptake was conducted with Pearson chi-squared p-values estimated. Bivariate associations between all service quality indicators and LARC uptake were also conducted, those with Pearson chi-squared p<0.02 were used to model quality and LARC uptake. While program performance was assessed using one single index indicator, MII, program capacity had multiple indicators, as attempts to develop an index were not successful. Mixed effects models were used to assess associations between quality indicators and uptake of LARC with health facility as a random intercept. We adjusted the models both for provider and client characteristics. Results are presented with odds ratios and 95% confidence intervals. Statistical significance was established at p<0.05, with marginal significance at p values between 0.05 and 0.09.
Ethical Approval
Ethical approval was provided by the Togolese Comité de Bioéthique pour la Recherche en Santé of the Togolese Ministry of Health and Social Protection (Avis no. 017/2016/CBRS du 30 Juin 2016). Approval was also provided by the University of California, Berkeley Center for Protection of Human Subjects (CPHS #2016-04-8614). All participants in the study provided verbal informed consent and participants under the age of 18 years were approved to provide informed consent on their own behalf. These conditions were approved by both ethics committees. This sub-analysis of the previously collected data was exempted from review by the University of California, Berkeley Center for Protection of Human Subjects.
Results
Of the 669 clients included in the sample, over half (55.6%) were 25–34 years of age and most (94.8%) were married with one to three living children (77.1%). The sample was evenly distributed between the education and wealth categories. Almost two-thirds of the clients (64.7%) received FP counseling from midwives vs other clinical staff and over half (55.2%) were seen by providers aged 20–39 years.
Within the sample, 19.4% (n=130) received a LARC method. Table 2 highlights the bivariate analysis of factors associated with uptake of LARC. Only the age of provider was found to be significantly associated with uptake of LARC (p=0.01), such that younger providers (aged 20–39 years) were more likely to provide LARC than providers 40 years and older. Though the age of the client was not significant at p=0.09 level, clients 25–34 years more likely to receive a LARC method, than women in the younger and older age categories.
 |
Table 2 Characteristics of Study Sample and Their Association with LARC Uptake Among Study Sample |
Figure 3 shows the percentage of LARC adopters (n=130) who received quality services as assessed by six measures. For all of the FP quality assessment measures, the vast majority of LARC adopters received services at facilities with supervisory visits in the past three months. The only two quality measures that did not benefit at least 50% of women adopting LARC were provider in-service training (42.3%) and provider reporting minimum restrictions (37.7%).
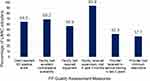 |
Figure 3 Percent of LARC adopters receiving quality FP services among LARC adopters in study sites in Lomé, Togo. |
Table 3 shows the results from the mixed effects models. We present results from three models: a model with unadjusted quality indicators; a model adjusted for all quality indicators that were statistically significantly associated with LARC uptake in the unadjusted model with p-values <0.05; and quality indicators adjusted for client and provider characteristics associated at bivariate level with a p value <0.02.
 |
Table 3 Percent of Clients Exposed to Quality FP and Unadjusted and Adjusted Mixed Effects Model Results for LARC Uptake, with Facility as a Random Intercept in Lomé, Togo |
Results from the first panel show that supervisory visits and MII score were the only two quality measures positively and significantly associated with LARC uptake in the sample population. Women visiting facilities with supervisory visits in the last three months were four times more likely to adopt LARC methods (OR 4.1; 95%CI 1.49–11.33); while women with positive MII score were almost eight times more likely to adopt LARC (OR 7.9; 95%CI 5.05–12.51).
The second panel shows the results from a combined model which includes the two quality indicators statistically significantly associated with LARC uptake at p<0.05. Supervisory visits decreased the odds ratio from 4.1 to 1.5 and maintained significance. Similarly, the MII score decreased from 7.9 to 2.1 odds ratio and remained significant. When the quality indicators were adjusted for client and provider characteristics, both MII and supervisory visits maintained the odds ratios and significance levels.
Discussion
There is a growing body of evidence to support the notion that improving the quality of care of FP services is key to increasing use and continuation of FP services, particularly in resource limited settings.22,26,33 However, evidence on which factors are most important in determining quality of FP services is still sparse.26 In this study, we set out to assess if the quality of FP service provision, both of program performance and program capacity, influenced LARC adoption in Lomé, Togo. As noted prior, we were interested in LARC, as recent studies have suggested it is lagging in West Africa and women still face barriers to access.27
We found that factors related to the quality of FP service provision were statistically significantly associated with LARC uptake, even when controlling for client and provider characteristics. Program performance was measured using MII, as this indicator is increasingly being used to measure the quality of information given to clients during FP counseling and is a FP 2020 core indicator. The highly significant association between a positive MII score and LARC adoption suggests the importance of information for decision-making and method use. Another recent study found a similar positive relationship between quality of information exchanged as measured by MII and method continuation;22 however, the research using MII is still limited.
It should also be noted that only 28% of women interviewed for this study answered “yes” to all three questions in the MII, suggesting more progress is needed in providing adequate information to women adopting a contraceptive method in Lomé. However, among LARC adopters, 64.6% of women reported “yes” to all three MII indicators. In addition, more evidence is still needed to understand the value of MII in predicting future contraceptive use and fertility. In a study of MII over time using DHS data from 25 developing countries, MII and mCPR were not correlated, suggesting the two indicators capture different aspects of FP programs.33 Moreover, the ability of the MII to adequately predict contraceptive continuation was recently questioned and study authors recommended including a fourth question in future applications of MII which would ask women about the possibility of switching to another FP method.34
Recognizing that using MII alone would not fully reflect all key aspects of quality of care, we also assessed program capacity. Results showed that among the five indicators used to assess program capacity; only a supervisory visit at the facility in the last three months was significantly associated with uptake of LARC in the study population. The association held, even after adjusting for program performance, as well as client and provider characteristics. In fact, after all adjustments, women visiting a facility which had a recent supervisory visit had a 44% likelihood of adopting a LARC method. This finding suggests the importance of supervision in positively influencing provider morale and performance in clinical settings. We do not know who conducted the supervisory visit and this information was not collected as part of the study. The facility staff were just asked if they received a supervisory visit in the last three months. We do know that the expectation of the supervision was to follow standard protocol for supportive supervision with guidance on assessing stock, ensuring technical capacity of clinical staff by observing clinic visits, discussing difficult cases and going over challenges, and verifying a reporting system is in place. However, we did not collect data on whether these measures were implemented, but given the positive correlation with supervisory visits, we feel confident that the supportive supervision was implemented as expected. It is well established in the literature that supportive or facilitative supervision, which incorporates coaching and mentoring, is more effective in motivating providers than cursory inspections and harsh discipline.21,26,35,36 In an experiment in Kenya to test a cascade training package in which providers were trained and asked to update their untrained colleagues with instructional materials afterwards, the training package showed less impact on adherence to clinical FP guidelines than when supportive supervision was also offered as part of the intervention.35 A more recent study in Kenya, which assessed a quality management intervention, found that while providers reported mixed opinions about the effectiveness of the intervention, the majority reported that the supervisory visits helped them improve the quality of their services.37
The other four measures of program capacity (provider attitudes, method availability, equipment availability, and provider training) did not have a significant association with LARC uptake, even in the unadjusted model. In another analysis utilizing this same dataset, the authors found that though provider restrictions were widespread, they did not affect women’s ability to receive the method they wanted among women who had a desired method prior to their FP consultation.38 Though there could be different explanations for this finding, the one that seems most plausible is that a woman’s demand for a specific method overrides the provider’s restrictions. Potentially, women who arrive at the clinic with a desired method in mind are able to negotiate receipt of this method, even in cases where the provider reported a restriction. Thus, this speaks to the importance and need for more demand generating activities to accompany supply side interventions. Additionally, the sample was comprised largely (94%) of married women with nearly three-quarters older than 24 years. Meanwhile, most provider-imposed restrictions are related to age and marital status.38–40
We hypothesized that provider training would be associated with LARC uptake, since other studies in SSA have found providers to be a barrier based on biases based on sociodemographics, misconceptions about safety or lack of training in provision.41 However, we did not find a significant association between provider training and LARC uptake, which could be due to several reasons. The indicator measured whether a provider received in-service training in the last two years, but did not account for how recently the training took place or the quality of that training. Quality provider training was a component of the AgirPF program, but this study combined both AgirPF intervention and control facilities. In addition, provider training should include values clarification and support the provision of FP counseling and services free of bias or restrictions, yet as already noted, a previous study using these data found provider-reported restrictions based on age, parity, and marital status were widespread. This suggests that the training was potentially more successful in improving skills, but not attitudes.38 Knowledge transfer during training is important, but the implementation of knowledge acquired as demonstrated by the provider’s practice after the training is even more important. This finding provides additional evidence on the critical role of supervisory visits. Investing in provider competency should be combined with measures to ensure providers are supported to deliver best practices in FP care.26 Similar to provider training, availability of equipment and contraceptive methods were not significantly associated with LARC uptake. This finding indicates that if women are not given full information through comprehensive FP counseling, then the effect of the other supply side factors is diminished. Thus, the information provided to prospective users is most crucial. Furthermore, while this study has focused on the quality of service delivery, MII is not only a supply side measure. In this sense, it can also be thought of as a point of encounter with the “demand” side (ie, whether the woman is provided with enough information to believe that use of LARC will be safe, effective and that she can come to be seen as soon as/if there are any side effects).
Nonetheless, quality is multidimensional, and though this study highlighted factors of quality significantly associated with LARC uptake, all quality-related factors should be addressed in developing FP service delivery. For example, systematic review of factors determining quality of care in Africa found that structural factors, such as cost of services, wait time, clinic hours, and privacy were determinants of quality and require strategies to reduce these barriers.26
Limitations
Despite the significant findings of the study, there are several limitations to note. The study took place in urban and peri-urban facilities in Lomé and therefore the findings are not representative of the country as a whole. Moreover, the study sample was comprised of older and married women, and therefore, may not reflect the experiences of younger and unmarried women, who may face more challenges in accessing LARC. Women in the study setting are likely to also receive information on LARC outside of the clinic setting, given information, education, and communication campaigns that are common in urban communities.
While the multifaceted measurement of quality strengthened this study design, certain measurement aspects had limitations. We utilized client exit interviews for the MII. However, a recent study found that compared to observation data in the facility survey, exit interview data overestimated the level of side effects counseling substantially, and its reporting had poor predictive value.42 While the larger operations research in which this study was nested did include observation data, we chose to use client exit reports for this study, as we were more interested in the information exchange as perceived by the client and the comparability to other surveys offered by MII; the results from the observation data were also not very different from client exit interview results.
The client exit interview data may be affected by recall and courtesy bias. We tried to minimize the recall bias inherent in self-reporting by having the client exit interview take place immediately after the FP consultation, rather than retrospective surveys as in applications of MII in DHS or FP 2020. Courtesy bias that can result when clients feel uncomfortable reporting negative aspects of care43 could only be minimized by providing a private location for the interviews and ensuring the interviewers were trained in building rapport and trust. We feel that this bias was limited, considering only 28% of women answered “yes” to all three questions in the MII.
The provider survey also had limitations. As noted already, the variable on in-service provider training might have been too broad in that it included all training from the last two years and did not include specific questions related to the type and quality of training. In addition, provider interviews may reflect a social response bias or desire of the provider to report perceived best practices rather than actual practices.43 However, given the high prevalence of restrictions reported by providers, we think this bias was also minimized in the study.
Conclusion
This study highlighted the importance of two service delivery quality factors in LARC uptake: comprehensive counseling and supervisory visits. More research is needed to understand the impact of the layered dimensions of quality on reproductive health outcomes. Continued focus on quality of care and comprehensive counseling is necessary to ensure women’s FP needs are met within a rights-based framework. In addition, given the importance of provider–client information exchange highlighted in this study, more effort is needed to ensure women are given comprehensive information on the full range of methods and their side effects in Lomé and beyond.
Acknowledgments
This study was conducted with data collected through the Evidence for Development Project funded by the United States Agency for International Development, West Africa. Special thanks to Kokou Kpeglo and Adjoko Mensah of Cabinet of Recherche et d’Évaluation (CERA) in Lomé, Togo for their role in supervising fieldwork related to the data collection for this study and Alfredo Fort of International Technical and Business Consultants for his detailed review of the final draft of the manuscript. The points of view in this study are solely those of the authors and do not necessarily reflect the views of the United States Agency for International Development.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ouagadougou Partnership. Report to the 4th Annual Meeting of the Ouagadougou Partnership. Cotonou, Benin. December 9–11, 2015. Dakar, Senegal: Ouagadougou Partnership; 2016.
2. Ouagadougou Partnership. Family Planning: Francophone West Africa on the Move. Dakar, Senegal: Ouagadougou Partnership; 2012.
3. Mbacké C. The persistence of high fertility in sub-Saharan Africa: a comment. Popul Dev Rev. 2017;43:330–337. doi:10.1111/padr.12052
4. Guttmacher Institute. Adding It Up: Investing in Contraception and Maternal and Newborn Health in the Ouagadougoug Partership Countries (Fact Sheet). New York: Guttmacher Institute; 2018.
5. Ameyaw EK, Budu E, Sambah F, et al. Prevalence and determinants of unintended pregnancy in sub-Saharan Africa: a multi-country analysis of demographic and health surveys. PLoS One. 2019;14(8):e0220970. doi:10.1371/journal.pone.0220970
6. Family Planning 2020. FP2020 Core Indicator Estimates Togo. Washington, DC: Family Planning 2020; 2016.
7. Scoggins S, Bremner J. FP2020 Momentum at the Midpoint 2015–2016. Washington DC: FP2020; 2016.
8. Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366(21):1998–2007. doi:10.1056/NEJMoa1110855
9. Hatcher RA. Contraceptive Technology. Ardent Media; 2007.
10. Kaneshiro B, Aeby T. Long-term safety, efficacy, and patient acceptability of the intrauterine Copper T-380A contraceptive device. Int J Womens Health. 2010;2:211–220. doi:10.2147/IJWH.S6914
11. McNicholas C, Maddipati R, Zhao Q, Swor E, Peipert JF. Use of the etonogestrel implant and levonorgestrel intrauterine device beyond the U.S. Food and Drug Administration-approved duration. Obstet Gynecol. 2015;125(3):599–604. doi:10.1097/AOG.0000000000000690
12. Gomez AM, Fuentes L, Allina A. Women or LARC first? Reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Perspect Sex Reprod Health. 2014;46(3):171–175. doi:10.1363/46e1614
13. Curry DW, Rattan J, Huang S, Noznesky E. Delivering high-quality family planning services in crisis-affected settings II: results. Glob Health Sci Pract. 2015;3(1):25–33.
14. Jacobstein R, Stanley H. Contraceptive implants: providing better choice to meet growing family planning demand. Glob Health Sci Pract. 2013;1(1):11–17.
15. Jacobstein R, Curtis C, Spieler J, Radloff S. Meeting the need for modern contraception: effective solutions to a pressing global challenge. Int J Gynecol Obstet. 2013;121:S9–S15. doi:10.1016/j.ijgo.2013.02.005
16. Dassah ET, Odoi AT, Owusu-Asubonteng G. Prevalence and factors predictive of long-acting reversible contraceptive use in a tertiary hospital in urban Ghana. Eur J Contracept Reprod Health Care. 2013;18(4):293–299. doi:10.3109/13625187.2013.790951
17. Jarvis L, Wickstrom J, Shannon C. Client Perceptions of quality and choice at static, mobile outreach, and special family planning day services in 3 African countries. Glob Health Sci Pract. 2018;6(3):439–455.
18. Corker J. Taking Family Planning to the Village. Using Mobile Outreach Services to Increase Voluntary Family Planning in Togo. Washington DC: Population Services International; 2015.
19. Hardee K, Kumar J, Newman K, et al. Voluntary, human rights–based family planning: a conceptual framework. Stud Fam Plann. 2014;45(1):1–18. doi:10.1111/j.1728-4465.2014.00373.x
20. Bruce J. Fundamental elements of the quality of care: a simple framework. Stud Fam Plann. 1990;21(2):61–91. doi:10.2307/1966669
21. RamaRao S, Lacuesta M, Costello M, Pangolibay B, Jones H. The link between quality of care and contraceptive use. Int Fam Plan Perspect. 2003;29(2):76–83. doi:10.2307/3181061
22. Chakraborty NM, Chang K, Bellows B, et al. Association between the quality of contraceptive counseling and method continuation: findings from a prospective cohort study in social franchise clinics in Pakistan and Uganda. Glob Health Sci Pract. 2019;7(1):87–102.
23. Mensch B, Arends-Kuenning M, Jain A. The impact of the quality of family planning services on contraceptive use in Peru. Stud Fam Plann. 1996;27(2):59–76. doi:10.2307/2138134
24. Koenig MA, Hossain MB, Whittaker M. The influence of quality of care upon contraceptive use in rural Bangladesh. Stud Fam Plann. 1997;28(4):278–289. doi:10.2307/2137859
25. Hancock NL, Stuart GS, Tang JH, Chibwesha CJ, Stringer JS, Chi BH. Renewing focus on family planning service quality globally. Contracept Reprod Med. 2016;1(1):10. doi:10.1186/s40834-016-0021-6
26. Tessema GA, Gomersall JS, Mahmood MA, Laurence CO, Mortimer K. Factors determining quality of care in family planning services in Africa: a systematic review of mixed evidence. PLoS One. 2016;11(11):e0165627. doi:10.1371/journal.pone.0165627
27. Adedini SA, Omisakin OA, Somefun OD, Kabir R. Trends, patterns and determinants of long-acting reversible methods of contraception among women in sub-Saharan Africa. PLoS One. 2019;14(6):e0217574. doi:10.1371/journal.pone.0217574
28. Agir pour la Planification Familiale (AgirPF). Using Baseline Data to Develop an In-Country Strategy for Improving Family Planning Use and Service Delivery in Togo. New York: EngenderHealth (AgirPF); 2017.
29. Agir pour la Planification Familiale (AgirPF). Assessment of Facility-, Provider- and Household-Related Aspects of Family Planning Service Delivery and Utilization in Four West African Countries. New York: EngenderHealth (AgirPF); 2015.
30. Adama-Hondégla AB, Aboubakari A-S, Fiagnon K, Bassowa A, Badabadi EJ, Akpadza K. Women’s preferential contraceptive methods in publics’ family planning centers in Lomé (Togo, West Africa): a prospective study of 734 cases. Open J Obstet Gynecol. 2015;5(10):564. doi:10.4236/ojog.2015.510080
31. Chang KT, Mukanu M, Bellows B, et al. Evaluating quality of contraceptive counseling: an analysis of the method information index. Stud Fam Plann. 2019;50(1):25–42. doi:10.1111/sifp.12081
32. StataCorp LLC. 2019. Available from: https://www.stata.com/company/.
33. Jain AK. Examining progress and equity in information received by women using a modern method in 25 developing countries. Int Perspect Sex Reprod Health. 2016;42(3):131–140. doi:10.1363/42e1616
34. Jain A, Aruldas K, Tobey E, Mozumdar A, Acharya R. Adding a question about method switching to the method information index is a better predictor of contraceptive continuation. Glob Health Sci Pract. 2019;7(2):289–299.
35. Stanback J, Griffey S, Lynam P, Ruto C, Cummings S. Improving adherence to family planning guidelines in Kenya: an experiment. Int J Qual Health Care. 2007;19(2):68–73. doi:10.1093/intqhc/mzl072
36. Dohlie M-B, Mielke E, Mumba FK, Wambwa GE, Rukonge A, Mongo W. Using practical quality improvement approaches and tools in reproductive health services in East Africa. Jt Comm J Qual Improv. 1999;25(11):574–587. doi:10.1016/S1070-3241(16)30471-0
37. Wendot S, Scott RH, Nafula I, Theuri I, Ikiugu E, Footman K. Evaluating the impact of a quality management intervention on post-abortion contraceptive uptake in private sector clinics in western Kenya: a pre-and post-intervention study. Reprod Health. 2018;15(1):10. doi:10.1186/s12978-018-0452-4
38. Pleasants E, Koffi T, Weidert K, McCoy S, Prata N. Are women in lome getting their desired methods of contraception? Understanding provider bias from restrictions to choice. Open Access J Contracept. 2019;10:79–88. doi:10.2147/OAJC.S226481
39. Tumlinson K, Okigbo CC, Speizer IS. Provider barriers to family planning access in urban Kenya. Contraception. 2015;92(2):143–151. doi:10.1016/j.contraception.2015.04.002
40. Calhoun LM, Speizer IS, Rimal R, et al. Provider imposed restrictions to clients’ access to family planning in urban Uttar Pradesh, India: a mixed methods study. BMC Health Serv Res. 2013;13(1):532. doi:10.1186/1472-6963-13-532
41. Mazzei A, Ingabire R, Mukamuyango J, et al. Community health worker promotions increase uptake of long-acting reversible contraception in Rwanda. Reprod Health. 2019;16(1):75. doi:10.1186/s12978-019-0739-0
42. Choi Y. Estimates of side effects counseling in family planning using three data sources: implications for monitoring and survey design. Stud Fam Plann. 2018;49(1):23–39. doi:10.1111/sifp.12044
43. Tumlinson K, Speizer IS, Curtis SL, Pence BW. Accuracy of standard measures of family planning service quality: findings from the simulated client method. Stud Fam Plann. 2014;45(4):443–470. doi:10.1111/j.1728-4465.2014.00007.x
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
