Back to Journals » Clinical Ophthalmology » Volume 14
Quality of Life in Patients with Unresolved Facial Nerve Palsy and Exposure Keratopathy Treated by Upper Eyelid Gold Weight Loading
Authors Nowak-Gospodarowicz I, Różycki R, Rękas M
Received 19 March 2020
Accepted for publication 6 July 2020
Published 5 August 2020 Volume 2020:14 Pages 2211—2222
DOI https://doi.org/10.2147/OPTH.S254533
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Izabela Nowak-Gospodarowicz, Radosław Różycki, Marek Rękas
Department of Ophthalmology, Military Institute of Medicine, Warsaw 04-141, Poland
Correspondence: Izabela Nowak-Gospodarowicz
Department of Ophthalmology, Military Institute of Medicine, 128 Szaserow St, Warsaw 04-141, Poland
Tel +48 261 816 575
Fax +48 22 515 05 08
Email [email protected]
Background: Loading of the upper eyelid with gold weights is a well-established procedure for the correction of paralytic lagophthalmos. There is no reliable research evaluating the results of this treatment from the patients’ viewpoint.
Aim: The aim of this research was to evaluate quality of life (QOL) domains through two standardized questionnaires (SF-36 and NEI-VFQ39) in patients treated by upper eyelid gold weight loading compared to healthy individuals (the “healthy” group) as well as patients with other ophthalmologic conditions (the “sick” group).
Patients and Methods: This prospective comparative clinical study of 416 surveys was conducted in 2012– 2018. The study group includes 59 people: 40 women, 19 men aged 55.5 ± 17.4 treated with gold weights for corneal complications due to unresolved facial nerve palsy. General QOL was assessed using the SF-36 questionnaire. Eye-related QOL was assessed through the NEI-VFQ39 questionnaire. The results were compared with those obtained in 2 control groups: the “healthy” and the “sick,” 53 individuals each.
Results: A statistically significant increase in QOL domains was noted in patients with facial nerve palsy after treatment (p< 0.001). No statistically significant differences were found in categories defining the Physical Component Score in these patients as compared to those from the “sick” control group (p = 0.95). After surgery, the results of the Mental Component Score were comparable to those in the “healthy” control group (p = 0.51). The eye-related health scores changed significantly after surgery and differed significantly compared to the “sick” control group (p < 0.05); however, they did not reach the level of the “healthy” control group (p < 0.001).
Conclusion: Patients with untreated facial nerve palsy had the lowest QOL levels among all individuals involved in this study. Treatment of lagophthalmos by gold weights significantly improved their QOL, with the greatest impact on mental aspects of health.
Keywords: facial nerve palsy, quality of life, QOL, gold weights, lid-loading, SF-36, NEI-VFQ25/39
Introduction
Paralysis of the facial nerve (cranial nerve VII) affects people all over the world regardless of age, gender or race. Function of the facial nerve is necessary for speech, smiling and the expression of emotions, which is why its damage greatly affects the functioning of individuals in society.1–5
Lack of innervation of the orbicularis oculi muscle makes it impossible to close the eye. In time, as a result of constant exposure, the cornea becomes resistant to the treatment of ulcers and perforations. This condition may even result in the loss of the eye.6,7 Usually, an obturation is needed or a partial medial or lateral tarsorrhaphy is performed to enable the regeneration of the cornea. Unfortunately, this form of treatment is associated with a reduced field of vision and cosmetic defects, which pleases neither patient nor surgeon.
Loading the upper eyelid with a gold weight seems to be an alternative method of treatment in such patients. This method was first described by K. Illig in 1958.8 Since then, both surgical techniques and the implants used have been continuously improved.9–11
The standard weights are made of 99.99% gold and are specially rounded, which allows an exact match to the curvature of the upper eyelid.
The weights allow for complete closure of the eye in most cases and effectively reduce the severity of inflammation or ulceration of the cornea, without limiting field of vision. An ideal weight allows the patient to close and open their eyes without inducing eyelid ptosis. The procedure is performed under local anesthesia. In the case of accompanying ectropion of the lower eyelid, surgical correction of the paralytic ectropion may also be performed.
Gold weights have many advantages: they are well tolerated as gold is a biologically inert material that does not affect magnetic resonance imaging and properly placed implants remain invisible to the environment. If necessary, they can be removed from the tissue of the upper eyelid without visible scarring.
Loading of the upper eyelid with gold weights is a well-established procedure for the correction of paralytic lagophthalmos,11–16 however there are no reliable studies assessing the results of the surgery from the perspective of patients.
Previous papers are based only on the visual analog scale (VAS)16–18 or were only partially related to the eye.5,19-21
To our knowledge, this is the first controlled study conducted with the use of 2 standardized questionnaires with proven accuracy and reliability to assess quality of life (QOL) domains in patients after upper eyelid loading with gold weights.
Therefore, the aim of this study is:
- To assess if and how impairment of the eye influences the general QOL in patients with facial nerve palsy through the use of 2 questionnaires: SF-36 and NEI VFQ39;
- To assess the influence of the applied treatment on QOL in patients with unresolved facial nerve palsy in relation to healthy people and patients affected with other ophthalmic conditions.
Patients and Methods
This prospective study was conducted in years 2012–2018 in accordance with the principles of good medical practice, in accordance with the Declaration of Helsinki and after obtaining approval from the Bioethical Commission at the Military Institute of Medicine in Warsaw (Poland). All patients provided written informed consent to participate in this study.
Characteristics of the Study Group
The study group included 59 patients: 40 women (67.8%) and 19 men (32.2%) with an average age of 55.5 ± 17.4 years. In 37 patients (62.7%), persistent paralysis affected the left facial nerve, while in 22 (37.2%) the paralysis was right-sided. Etiologies of the facial nerve palsy in the study group were as follows: cerebellopontine angle tumor surgery in 46 (78%) patients, salivary gland tumor surgery in 5 (8.5%); trauma in 4 (6.8%), congenital facial nerve palsy in 2 (3.4%) and idiopathic unresolved facial nerve palsy in 2 (3.4%). All patients presented with at least grade 4 disfunction of the facial nerve according to the House Brackman scale.22 The average Sunnybrook score was 28.6 ± 12.2.23
Twenty one patients (35.6%) had no surgical history of treatment prior to study enrollment. In another 21 of this group, tarsorrhaphy was performed one or more times to allow corneal healing, of which 5 (8.5%) patients were additionally treated with an amniotic membrane transplant to the cornea elsewhere. In 8 patients (13.5%), facial nerve/sublingual nerve anastomosis was previously applied with no satisfactory results. In 7 patients (11.8%) correction of the paralytic ectropion of the lower eyelid was performed at another hospital. Two other patients (3.4%) had a history of upper eyelid gold weight loading, which was then removed elsewhere due to complications.
The average duration of facial nerve palsy was 116 ± 202 months.
Criteria for participation in this study included:
(1) Unresolved paralysis of the facial nerve and lagophthalmos for at least 3 months despite intensive rehabilitation, (2) ocular symptoms reported by the patient due to exposure keratopathy not responding to conservative treatment, (3) at least good function (>8mm) of the levator muscle of the upper eyelid, and (4) condition of both the skin of the eyelid and ocular muscle of the eye allowed for surgery.
Patients were excluded (1) if they were younger than 18 years and (2) were unable or disagreed to independently complete questionnaires. Patients who did not have demographic or psychometric data were excluded from the analysis. Patients were not compensated for participation.
Preoperative best corrected visual acuity (BCVA) measured on the Snellen chart was 0.4 ± 0.3 and 0.6 ± 0.3 after upper eyelid gold weight loading (p<0.05). Despite at least 3 months of conservative treatment, all patients reported ocular surface disorders. Epitheliopathy was present in 31 patients (52.5%). Pathology within the deeper layers of the cornea (ie, interstitial changes) was noted in 14 patients (23.7%). The remaining 14 patients (23.7%) presented with deep corneal ulcers threatening perforation.
Corneal sensation was assessed with the use of a cotton swab and was normal (evident reaction after touching with a swab) in only in 22 patients (37.3%), weakened (patient reported that the touch was felt, but reaction might not be evident) in 23 (39%), and absent (no reaction and no perception reported after touching) in 14 patients (23.7%). The Schirmer Test, performed after applying anesthetic drops, was abnormal (below 10 mm) in 12 cases (20.3%).
Lagophthalmos, measured by caliper when attempting eyelid closure, was on average 7 ± 3 mm preoperatively and 0.1±0.5mm after upper eyelid gold weight loading (p<0.001). The preoperative marginal reflex index 1 (MRD1, the distance between the upper eyelid margin and corneal reflex) averaged 3.9 ± 1.6 mm in the affected eye and 3.8 ± 0.9 mm in the contralateral eye (p>0.1). The preoperative marginal reflex index 2 (MRD2, the distance between the lower eyelid margin and corneal reflex) averaged 6.8 ± 1.4 mm in the affected eye and 5.0 ± 0.8 mm in the contralateral eye (p<0.05). Postoperative MRD1 and MRD2 in the affected eye were 3.5 ± 1mm (p>0.05) and 5.4 ± 1.2 mm (p<0.05) respectively.
Patients used an average of 9±5 drops of moisturizing drugs per day preoperatively and 2±2 after surgery (p<0.05).
Estimation of the desired implant weight was performed before surgery individually for each patient while in a sitting position by fastening weight samples to the upper eyelid with double-sided tape in increments of 0.2 g – from 0.6 to 1.8 g, total. The lightest implant, which after 15 minutes ensured complete closing and opening of the eye without induction of eyelid ptosis above 2 mm, was considered to be proper (Supplementary materials).
Upper eyelid gold weight loading involved high pretarsal fixation with levator recession as previously described24 was performed under an operating microscope by one of 2 surgeons (IN-G and RR) in every patient.
The average weight of the implant was 1.5 ± 0.3 g.
Correction of paralytic ectropion was performed concomitantly, if necessary. Depending on clinical condition, medial spindle, lateral tarsal strip or a combination of both techniques was performed25–27 in 31 out of 59 patients (61%).
Follow-ups for evaluation of objective results of treatment, cosmetic effects of the surgery and complications were done on the following time schedule: day 1, 10, months 1, 3, 6, 12, 24, 36, and once a year thereafter. All patients from the study group remain under the care of our outpatient clinic.
Complications after upper eyelid gold weight lid loading were rare and included: 3 weight extrusions (5%), 4 weight migrations (6.8%), contouring in 2 cases (3.4%), unsatisfactory cosmesis in 2 patients (3.4%), and deterioration of BCVA in 3 (5%).28
Control Groups for the Assessment of QOL
Two control groups were created as reference points in order to compare the QOL results of patients with facial nerve palsy – extremely good (the “healthy” control group) and extremely poor QOL results (the “sick” control group). A control group of healthy people (53 of 72 people, 24M, 27F aged 42 ± 14 years) was recruited among adults between January 2013 and December 2014. After asking the question: “Have you ever had any eye disease?” and obtaining a negative answer, a questionnaire was distributed among indoor staff, as well as random people in one of Warsaw’s city parks and in the center of the city of Warsaw. Only people who completed both questionnaires were included in the study.
A second group – “the sick” control group – was defined after a literature search in order to find ophthalmic patients with proven extremely poor quality of life.29,30 The “sick“ controls were recruited in the same period and consisted of patients surgically treated for glaucoma or age-related macular degeneration (AMD) in one eye at our Ophthalmology Clinic.
There were 25 of 33 AMD patients (10M, 15F, aged 72 ± 9 years), and 28 of 38 glaucoma patients (12M, 17F, aged 63 ± 12 years who completed both questionnaires.
To check the validity of the selected control groups for the assessment of the quality of life, statistical analysis was performed.
Assessment of Quality of Life
Two questionnaires were used to evaluate QOL: SF-36v.2 (Medical Outcomes Study 36-items Short Form Health Survey in original Polish second version) and NEI VFQ3931 (the questionnaire for the assessment of vision function according to the National Eye study Institute Visual Function Questionnaire). Fully completed questionnaires were obtained from 157 individuals and results were analyzed as a part of this study. The license number QM022281/QM023605 was obtained from Quality Metric Inc. for the use of the SF-36 questionnaire.
The final version in Polish of the NEI-VFQ39 questionnaire was obtained after confirmation of the translation by two independent English translators using a forward-backward translation method.32,33 The internal coherence and reliability of the tests was calculated for each category by determining the α - Cronbach coefficient. A coefficient value above 0.8 was considered to be very good, above 0.7 as satisfactory.34
NEI-VFQ 39 consists of 25 questions or alternatively 39 questions in version VFQ 39. It takes about 10 minutes to complete the questionnaire.
In the VFQ 39 questionnaire, 12 categories of health are distinguished:
- General health – questions: 1, A1;
- General vision – questions: 2, A2;
- Ocular pain – questions: 4.19;
- Near activities – questions: 5,6,7, A3, A4, A5;
- Distance activities – questions: 8,9,14, A6, A7, A8;
- Social functioning – questions: 11.13, A9;
- Mental health – questions: 3,21,22,25, A12;
- Role difficulties – questions: 17.18, A11a, A11b;
- Dependency – questions: 20,23,24, A13;
- Driving – questions: 15c, 16.16 a;
- Color vision – question 12;
- Peripheral vision – question 10.
First, data were recoded to a value of 0–100 according to the key given,35 so that the range of obtained results ranged from 0 to 100 points, where 0 means the inability to perform the given activities due to sight, and 100 means a lack of any restrictions in the performance of activities.
Descriptive analysis for the general value of the NEI-VFQ39 questionnaire and individual health categories consisted of the calculation of mean values with standard deviation, median, threshold values of minimum and maximum.
The average was calculated according to the formula:
The sum of points for questions about a particular health category (without missing answers and answers to question 6, which should be treated as missing)/number of questions without missing answers.
The SF-36 questionnaire assesses eight homogeneous and two cumulative categories of health. Detailed categories include:
- Physical functioning (PF) – the range of typical physical activities performed on a daily basis – measurement of the limitation of physical activity caused by health restrictions (this domain contains 10 questions with multilevel answers)
- The importance of physical limitations (physical roles – RP) – the effect that physical health has on daily activity allows the measurement of the limitations of a physical activity specific to a patient caused by health problems (4 questions with yes/no answers)
- Pain complaints (bodily pain – BP) – intensity of physical pain and its impact on daily activity (evaluated with two questions about multilevel answers)
- General health (GH) – self-assessment of the general state of health of the patient in relation to their expectations and health (multilevel answers to 5 questions)
- Vitality (VT) – classified quantitatively as nervousness, irritability, depression, happiness, ie, energy level and fatigue measurement (3 questions with yes/no answers)
- Social functioning (SF) – the impact of emotional problems on functioning in everyday life (two questions with multilevel answers)
- The importance of emotional limitations (emotional role – RE) domain evaluated by 3 questions with yes/no answers
- Mental health (MH) defines the level of psychological stress and well-being (5 questions with multilevel answers)
Individual parameters can be combined into groups, summing up to four parameters concerning the assessment of the physical sphere of quality of life and four parameters of the mental aspect of the health.
Combined categories:
PF + RP + BP + GH = Physical Component Summary (PCS)
VT + SF + RE + MH = Mental Component Summary (MCS)
Point surveys are summed to a value between 0 and 100. Interpretation of normalized results is relatively easy because results for all 8 subscales greater than 50 exceed the norm, while results lower than 50 are classified as below the norm. A low numerical value reflects an unfavorable, subjective assessment of a patient’s health as a result of pain or disability. A high point value indicates a favorable health assessment without pain or a significant deficiency in the physical fitness of the body.36
The SF-36 scores obtained for individual health categories in the study group before and after surgery and in both control groups were compared.
Additionally, patients were asked to assess their quality of life level on a 0–10 VAS scale, where “0” meant the worst imaginable condition and “10” the best imaginable condition. Patients were also asked for a subjective assessment of the nuisance of the eye surface, symptoms and the number of necessary instillations of moisturizing preparations into the conjunctival sac during the day.
Statistical analysis was performed using SPSS software. For measurable features, the normality of the distribution of analyzed parameters was evaluated using the Shapiro–Wilk test. The Wilcoxon pair order test was used to compare the two dependent groups. For the two independent groups, the Mann–Whitney U-test was used. The Kruskal–Wallis test was used to compare more than two independent groups. A significance level of p <0.05 was assumed indicating the existence of statistically significant differences or dependencies.
Results
Four hundred and sixteen questionnaires were completed by participants and analyzed by researchers in this study: 208 SF-36 and 208 NEI VFQ39 questionnaires for the assessment of QOL domains in 157 individuals.
Fifty-one SF-36 and 51 NEI-VFQ-39 completed questionnaires from 51 patients out of 59 undergoing surgical treatment due to exposure keratopathy in 2012–2018 were obtained from the study group. The average QOL level in the study group on a VAS scale was 9.2 ± 1.2 six months after surgery. The reduction of used moisturizing drugs was reported in 57 of 59 patients (96.6%) six months after surgery.
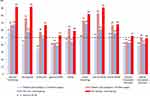
A summary of the results of the SF-36 questionnaire in individual health categories in the study group before and after surgery and in both control groups is presented in Figure 1.
Statistical dependencies between all groups are given in Table 1.
Statistically significant differences in all 8 examined areas of health on the basis of the SF-36 questionnaire were obtained in patients with 7thCN paralysis before and after surgery (p <0.001) (Table 1). The lowest scores were obtained in the group of patients with 7thCN paralysis before the procedure, most significantly in young women younger than 23 years of age. These results did not differ significantly in comparison to those obtained in the “sick” control group in categories defining the combined component of mental health (Mental Component Score – MCS) (p = 0.23). Results for the mental health category changed significantly in patients with 7thCN paralysis after the procedure (p <0.001) and were comparable to those obtained in the control group of healthy individuals (p = 0.51). Despite surgery, no statistically significant differences were found in the categories determining physical health (PCS) in patients with 7thCN paralysis compared to those in the “sick” control group (p=0.95) (Table 1).
Results were consistent with those obtained from the NEI-VFQ 39 questionnaire.
The measured categories of health depending on eyesight were similar in patients with facial nerve palsy before surgery compared to people in the “sick” control group (Figure 2, Table 2). Values changed significantly after surgery (p <0.001) and differed significantly in all categories compared to those obtained from the “sick” control group (p <0.05); however, they did not reach the level estimated for healthy individuals (p <0.001) (Table 2).
All the scores of the NEI-VFQ 39 questionnaire are presented in Figure 2.
Statistical dependencies between all groups for the NEI-VFQ 39 questionnaire are listed in Table 2.
Discussion
There is a lack of reliable research regarding the results of upper eyelid loading with gold weights in the treatment of exposure keratopathy due to unresolved facial nerve palsy from the patient’s perspective. In the study carried out by Schrom et al17 the overall QOL level on the VAS scale was evaluated retrospectively. Twelve of 16 (75%) patients were very satisfied with the operation’s effectiveness with the cosmesis rated at 3.8, where 1 was the best and 10 the worst, result. Sonmez et al18 divided the questionnaires of 30 patients into questions regarding: dry eye symptoms, tearing, redness of the eye, visual acuity, closing of the eye during the day, closing of the eye at night, cosmesis, use of moisturizing preparations and comfort “outdoors.” Each part was also rated on a 1–10-VAS scale, but here 1 meant the worst and 10 the best score. Patients in this group rated eye closure the best during the day (on average 8.8 ± 1.9), followed by at night (7.7 ± 3.0), cosmesis (7.6 ± 2.7), and using moisturizing drugs (7 1 ± 2.2). The lowest score was obtained for visual acuity.
Kelley and Sharpe16 note, on the basis of post-surgery surveys, that 72% of patients felt more comfortable after implantation of gold weights and subjectively note that assessed tearing decreased in this group by 50% after surgery. In our patients with facial nerve palsy, a general reduction of applied moisturizing drugs was recorded in 57 of 59 patients (96.6%) six months after surgery. Average QOL level on the 1–10-point VAS scale, where 1 means the worst and 10 the best condition, was 9.2 ± 1.2, and thus exceeded the level of satisfaction of patients from the aforementioned studies. However, different criteria and grading systems used by researchers make it impossible to reliably compare the data.
Aware of the impossibility of reliable measurement and comparison of such results, researchers in this study examined the quality of life domains in patients with unresolved facial nerve palsy and also in two control groups using two standardized questionnaires.
Questionnaire-based surveys focusing on health-related responses provide a relatively quick and simple way to obtain a number of reliable data. Repeating examination on the same people after a certain time allows researchers to assess changes in health. In this way, a statistically measurable natural course of disease or recovery can be ascertained. In the same way, an assessment of the outcome of medical intervention, in terms of improving QOL related to health, may be measured. For the “sick” control group, patients treated for glaucoma (28 people) or AMD (25 people) were selected. Glaucoma and AMD patients are characterized by the lowest subjective assessment of their quality of life compared to patients with other ophthalmic conditions.29,30 Such patients, given that they reflect an extremely low reference point, were included in the “sick” control group and served as a comparison to patients who underwent upper eyelid gold weight lid loading with regard to QOL domains. The extremely high reference point was in turn represented by the selected group of “healthy” individuals. Due to the fact that facial nerve paralysis was unilateral in patients from the study group, only patients treated invasively in one eye were involved in the study. However, while the differences in clinical presentation of glaucoma, AMD and paralytic lagophthalmos are obvious, from the patient’s point of view there are some similarities. Both patients treated for glaucoma and those with exposure keratopathy often experience discomfort and report ocular surface disorders.37–39 In the case of glaucoma, this is often the result of the use of topical eyedrops that lower intraocular pressure. In patients with lagophthalmos, discomfort is primarily the effect of the drying of the cornea which is permanently exposed. In both cases, the treatment of choice is moisturizing drugs in the form of drops or ointments applied topically to the conjunctival sac.
Another important ophthalmic problem in patients with facial nerve palsy is deterioration of visual acuity. In particular, near distance activities (ie, reading, writing, cooking or even looking at a watch) are impaired. This is not only due to corneal damage in the lower part of the cornea, which typically results from exposure, but also due to accumulation of excessive tears in the conjunctival sac due to paralytic ectropion and tear pump failure.40 Poor face perception resulting from AMD has been shown to impair social interactions and quality of life.41,42 Therefore, the “sick” control group also included patients treated for an exudative form of AMD, whose main problem is loss of central vision, which negatively impacts near and social activities.
The NEI-VFQ 39 questionnaire is a free of charge, recognized tool for subjective assessment of visual function, available only in English, which requires Polish translation.
The SF-36 questionnaire has been translated into more than 60 languages. In Poland, it was first used to assess the quality of life of patients suffering from schizophrenia at the Institute of Psychiatry and Neurology in Warsaw in 1997. As part of the translation of the survey into Polish, reliability and validity of scales were determined and standards for the Polish population were developed.43 Psychometric characteristics of the Polish version of SF-36v2 showed reliability comparable to the American scale.44
Statistically significant differences in all 8 examined QOL areas based on the SF-36 questionnaire were obtained in patients with facial nerve palsy before and after surgery (Figure 1, Table 1). Similar differences were obtained between the “healthy” and the “sick” control groups and between the “healthy” group and patients with facial nerve palsy before surgery (Figure 1, Table 1). These results were consistent with those obtained from the VFQ NEI 39 questionnaire in analogous groups (Figure 2, Table 2), although in patients with facial nerve palsy after surgery in NEI VFQ 39 there was no statistically significant difference between the study groups for driving categories (driving). This could be due to the fact that among patients undergoing surgical treatment (implantation of the gold weight) only 5 patients indicated they drove and in the control group only 7, and therefore this score was based on a very small number of people.
These results did not differ significantly compared to those obtained from the “sick” control group in terms of the Mental Component Summary (MCS): vitality (VT), role emotional (RE), mental health (MH) and general health (GH) categories (Table 1), which indicates a similar mental condition in patients suffering from AMD or glaucoma and patients with facial nerve palsy before surgery.
Interestingly, results related to the mental health QOL category changed significantly in the group of patients with 7thCN paralysis after surgery (Figure 1) and were comparable to those in the “healthy” control group (Table 1).
Differences in general health were still significant in patients with facial nerve palsy after surgery in comparison to the results obtained from the “healthy” control group. However, there were no differences in these groups in the pain category (bodily pain – BP) (Table 1, Figure 1).
This can be interpreted to mean that the correction of lagophthalmos resulted in the improvement of patients’ mental condition (above other areas) and relieves them from pain, but that the surgical intervention did not cure the illness.
Patients with facial nerve palsy who underwent surgery did not show differences in physical functioning (PF), social activity (SF) and the combined component of physical health (PCS) in comparison to the patients from the “sick” control group, which indicates that the surgery may have a small impact on physical aspects of health (Table 1). Similar observations were made by Coulson et al.19 Analyzing the quality of life of patients with long-term facial nerve palsy based on the SF-36 questionnaire, they found that the reduced quality of life was related primarily to social functioning and the mental sphere of health, and to a lesser extent physical functioning.
Tylka et al45 in their commentary on the validity and reliability of the SF-36v2 questionnaire draw attention to the characteristic tendency of Poles to complain more in comparison to the American population, which may explain the results in the “healthy” control group, specifically the value below 50 in the collective category defining the total level of mental health (MCS) (Figure 1).
In the NEI-VFQ-39 questionnaire, similar to the results of the analysis of the SF-36 questionnaire, no significant differences were found in any category except ocular pain and vision-dependent social functioning between patients with facial nerve palsy before treatment and patients from the “sick” control group (Table 2).
Results changed significantly after surgery, where differences in comparison to the “sick” control group were notable with the exception of two categories: color vision and driving (Table 2). The parameters assessed by the NFQ-NEI 39 questionnaire, similar to the results of the SF-36 questionnaire, significantly improved in the group of patients with facial nerve paralysis after surgery. However, there were still significant differences in QOL domains dependent on the eye assessed by these patients in comparison to people from the “healthy” control group (Table 2, Figure 2). This can be interpreted to mean that the correction of lagophthalmos by upper eyelid lid loading significantly improved visual acuity in patients with 7thCN palsy but did not let the eye restore completely, which is consistent with the objective results of treatment in this group of patients.46
In response to growing interest in quality of life of patients undergoing various medical procedures due to facial nerve dysfunctions, in 2011 Hernstrom et al47 published their study, which used the Facial Clinimertic Evaluation questionnaire (FaCE). Of the 15 questions of the FaCE questionnaire completed by 49 patients who received a platinum weight for the treatment of lagophthalmos, only 3 concerned the eye and included the assessment of dryness and irritation of the eye, use of topical moisturizers and tearing. In this case study, the authors showed statistically significant differences in QOL parameters in comparison to values from before surgical intervention (from 44.1 before to 52.7 after the surgery [P <0.001]) and reduction of eye dryness and the number of moisturizing drugs used, but did not find differences in the degree of tearing before and after surgery.
Patients with facial nerve palsy from our study before treatment achieved the lowest results in almost all QOL health categories as evaluated by the use of the SF-36 and the NEI VFQ-39 questionnaires (Figures 1 and 2). This can be explained by the fact that, in addition to eye symptoms, patients must cope with a cosmetic defect visible as facial asymmetry, smoothed mimic wrinkles, a drooping corner of the mouth and the inability to express emotions, which largely affects their life activities.48,49 This can explain why the lowest QOL scores were obtained in young women (<23 years old) with facial nerve palsy before upper eyelid gold weight lid loading procedure.
The results of this study let us conclude that patients with unresolved facial nerve palsy have the lowest QOL levels among all individuals involved in this study and that these decreased QOL levels were strictly related to ocular symptoms.
Implantation of gold weights led to a significant improvement in all QOL domains in patients with facial nerve palsy after surgery.
Improvement of QOL is primarily observed in the mental sphere of the health, where obtained values were similar to those estimated in the control group of “healthy” individuals.
Acknowledgments
Many thanks to Professor Jan Tylka – Professor at the Cardinal Stefan Wyszyński University in Warsaw in the Department of Clinical Psychology and Personality, Head of Clinical Psychology and Sociotherapy, and the Chairman of the National Team of Clinical Psychology Specialists for all the comments regarding this study. Source of support: Young Scientist Dotation from the Polish Ministry of Science and Higher Education (No. 200/2012).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mc Grounther DA. Facial disfigurement: the last bastion of discrimination. BMJ. 1997;314(7086):991. doi:10.1136/bmj.314.7086.991
2. Macgregor FC. Facial disfigurement: problems and management of social interaction and implications for mental health. Aesthetic Plast Surg. 1990;14(4):249–257. doi:10.1007/BF01578358
3. Valente SM. Visual disfigurement and depression. Plast Surg Nurs. 2004;24(4):140–146. doi:10.1097/00006527-200410000-00003
4. Bradbury E. Meeting the psychological needs of patients with facial disfigurement. Br J Oral Maxillofac Surg. 2012;50(3):193–196. doi:10.1016/j.bjoms.2010.11.022
5. Nellis JC, Ishii M, Byrne PJ, Boahene KD, Dey JK, Ishii LE. Association among facial paralysis, depression and quality of life in facial plastic surgery patients. JAMA Facial Plast Surg. 2017;19(3):190–196. doi:10.1001/jamafacial.2016.1462
6. Seiff RS, Chang JS. The staged management of ophthalmic complications of facial nerve palsy. Ophthalmic Plast and Reconstructive Surg. 1993;9(4):241–249. doi:10.1097/00002341-199312000-00003
7. Lee VZ, Currie V, Collin JRO. Ophthalmic management of facial nerve palsy. Eye. 2004;18(12):1225–1234. doi:10.1038/sj.eye.6701383
8. Illig KM. Eine neue Operationsmethode gegen Lagophthalmus. Klin Monatsbl Augenheilkd. 1958;32:410–411.
9. Smellie GD. Restoration of the blinking reflex in facial palsy by a simple lid-load operation. Brit J Plast Surg. 1966;19:279–283. doi:10.1016/S0007-1226(66)80056-5
10. Seiff SR, Sullivan JH, Freeman LN, Ahn J. Pretarsal fixation of gold weights in facial nerve palsy. Ophthalmic Plast Reconstr Surg. 1989;5(2):104–109. doi:10.1097/00002341-198906000-00005
11. Schrom T, Habermann K, Wernecke K, Scherer H. Implantation von Lidgewichten zur Therapie des Lagophthalmus. Ophthalmologe. 2005;102:1186–1192. doi:10.1007/s00347-005-1228-0
12. Mueller-Jensen K, Jansen M. Behandlung des fehlenden Lidschlusses. Dt Arztebl. 1997;94:2920–2921.
13. Hossam M, Foda T. Surgical management of lagophthalmos in patients with facial palsy. Am J Otol. 1999;20(6):391–395. doi:10.1016/S0196-0709(99)90079-0
14. Kinney S, Seeley B, Seeley M, Foster J. Oculoplastic surgical techniques for protection of the eye in facial nerve paralysis. Am J Otol. 2000;21:275–283. doi:10.1016/S0196-0709(00)80022-8
15. Tan S, Staiano J, Itinteang T, McIntyre B, McKinnon C. Gold weight implantation and lateral tarsorrhaphy for upper eyelid paralysis. J Cranio-Maxillo-Facial Surg. 2013;41:49–53. doi:10.1016/j.jcms.2012.07.015
16. Kelley SA, Sharpe DT. Gold eyelid weights in patients with facial palsy: a patient review. Plast Reconstr Surg. 1992;89:436–440. doi:10.1097/00006534-199203000-00006
17. Schrom T, Buchal A, Ganswindt S, Knippping S. Patient satisfaction after lid loading in facial palsy. Eur Arch Otorhinolaryngol. 2009;266:1727–1731. doi:10.1007/s00405-009-0981-0
18. Sonmez A, Ozturk N, Durmus N, Bayramici M, Numanoglu A. Patient’s perspectives on the ocular symptoms of facial paralysis after gold weight implantation. J Plast Reconstr Aesthet Surg. 2008;61:1065–1068. doi:10.1016/j.bjps.2007.06.019
19. Coulson SE, O’Dwyer NJ, Adams RD, Croxson GR. Expression of emotion and quality of life after facial nerve paralysis. Otol Neurol. 2004;25:1014–1019.
20. Vickery LE, Latchford G, Hevison J, Bellew M, Feber T. The impact of head and neck cancer and facial disfigurement on the quality of life of patients and their partners. Head Neck. 2003;25:289–296. doi:10.1002/hed.10206
21. Ryzenman JM, Pensak ML, Tew JM. Facial paralysis and surgical rehabilitation: a quality of life analysis in a cohort of 1595 patients after acoustic neuroma surgery. Otol Neurotol. 2005;26:516–521. doi:10.1097/01.mao.0000169786.22707.12
22. House JW, Brackman DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93(2):146–147. doi:10.1177/019459988509300202
23. Ross BG, Fradet G, Nedzelski JM. Development of a sensitive clinical facial grading system. Otolaryngol Head Neck Surg. 1996;114(3):380–386. doi:10.1016/S0194-5998(96)70206-1
24. Mavrikakis I, Malhotra R. Techniques for upper eyelid loading. Ophthal Plast Reconstr Surg. 2006;22:325–330. doi:10.1097/01.iop.0000235817.78695.6f
25. Nowinski TS, Anderson RL. The medial spindle procedure for involutional medial ectropion. Arch Ophthalmol. 1985;103:1750–1753. doi:10.1001/archopht.1985.01050110146045
26. Anderson RL, Gordy DD. The tarsal strip procedure. Arch Ophthalmol. 1979;97(11):2192–2196. doi:10.1001/archopht.1979.01020020510021
27. Tyers AG. Paralytic lagophthalmos. In: Tyers AG, Collin JRO, editors. Colour Atlas of Ophthalmic Plastic Surgery.
28. Nowak-Gospodarowicz I, Rozycki R, Koktysz R, Rękas M. Complications associated with the surgical techniques of upper eyelid loading: a clinicopathologic study of 7 explanted gold weight lid loads. Int J Ophthalmic Pathol. 2017;6:3.
29. Parrish RK, Gedde SJ, Scott IU, et al. Vision function and quality of life among patients with glaucoma. Arch Ophthalmol. 1997;115:1447–1455. doi:10.1001/archopht.1997.01100160617016
30. Scott IU, Smiddy WE, Schiffman J, Feuer WJ, Pappas CJ. Quality of life of low-vision patients and the impact of low-vision services. Am J Ophthalmol. 1999;128:54–62. doi:10.1016/S0002-9394(99)00108-7
31. Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-list-item national eye institute visual function questionnaire. Arch Ophthalmol. 2001;119(7):1050–1058. doi:10.1001/archopht.119.7.1050
32. Bullinger M, Alonso J, Apolone G, et al. Translating health status questionnaires and evaluating their quality: the IQOL project approach. International quality of life assessment. J Clin Epidemiol. 1998;51:913–923. doi:10.1016/S0895-4356(98)00082-1
33. Koller M, Aaronson NK, Blazeby J, et al. Translation procedures for standardised quality of life questionnaires: The European Organisation for Research and Treatment of Cancer (EORTC) approach. Eur J Cancer. 2007;43:1810–1820. doi:10.1016/j.ejca.2007.05.029
34. Cronbach LJ (1970). Essentials of psychological testing (3rd ed.). New York: Harper & Row. Available from: http://www.naukowiec.org/wiedza/metodologia/alfa-cronbacha_668.html.
35. Mangione CM, Berry S, Spritzer K, et al. Identifying the content area for the 51-item national eye institute visual function questionnaire: results from focus groups with visually impaired persons. Arch Ophthalmol. 1998;116:227–238. doi:10.1001/archopht.116.2.227
36. Ware J, Kosiński M, Dewey JE, Gandek B. SF-36 Health Survey: Manual & Interpretation Guide. Vol. 3. Lincoln, RI: QualityMetric Inc; 2000:5.
37. Leung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma. 2008;17(5):350–355. doi:10.1097/IJG.0b013e31815c5f4f
38. Skalicky SE, Goldberg I, McCluskey P. Ocular surface disease and quality of life in patients with glaucoma. Am J Ophthalmol. 2012;153(1):1–9.e2. doi:10.1016/j.ajo.2011.05.033
39. Quaranta L, Riva I, Gerardi C, Oddone F, Floriano I, Konstas AG. Quality of life in glaucoma: a review of the literature. Adv Ther. 2016;33:959–981. doi:10.1007/s12325-016-0333-6
40. Mc Laughlin CR. Epiphora in facial paralysis. Brit J Plast Surg. 1950;3:87–95. doi:10.1016/S0007-1226(50)80014-0
41. Mitchell J, Bradley C. Quality of life in age-related macular degeneration: a review of the literature. Health Qual Life Outcomes. 2006;4:97. doi:10.1186/1477-7525-4-97
42. Lane J, Rohan EMF, Sabeti F, et al. Impacts of impaired face perception on social interactions and quality of life in age-related macular degeneration: a qualitative study and new community resources. PLoS One. 2018;13(12):e0209218. doi:10.1371/journal.pone.0209218
43. Keller SD, Ware JE, Bentler PM, et al. Use of structural equation modeling to test the construct validity of the SF-36 health survey in ten countries: results from the IQOLA project. International quality of life assessment. J Clin Epidemiol. 1998;51(11):1179–1788. doi:10.1016/S0895-4356(98)00110-3
44. Brazier JE. The SF-36 health survey and its use in pharmacoeconomic evaluation. PharmacoEconomics. 1995;7(5):403–415. doi:10.2165/00019053-199507050-00005
45. Tylka J, Piotrowicz R. Kwestionariusz oceny jakości życia SF-36 – wersja polska. Kardiol Pol. 2009;67:1166–1169.
46. Nowak-Gospodarowicz I, Różycki R, Rękas M. Ocena leczenia keratopatii u chorych z niedomykalnością powiek operowanych poprzez dociążenie powieki górnej implantem ze złota - 7 letnie doświadczenia. Klinika Oczna (Acta Ophthalmologica Polonica). 2017;119(1):29–33.
47. Hernstrom DK, Lindsay RW, Cheney ML, Handlock TA. Surgical treatment of the periocular complex and improvement of quality of life in patients with facial nerve paralysis. Arch Facial Plast Surg. 2011;13(2):125–128. doi:10.1001/archfacial.2011.9
48. Hirschenfang S, Goldberg MJ, Benton JG. Psychological aspects of patients with facial paralysis. Dis Nerv Syst. 1969;30:257–261.
49. Smith IM, Mountain RE, Murray JA. An outpatient review of facial palsy in the community. Clin Otolaryngol. 1994;19:198–200. doi:10.1111/j.1365-2273.1994.tb01214.x
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.