Back to Journals » International Journal of Women's Health » Volume 14
Quality of Life During Pregnancy from 2011 to 2021: Systematic Review
Authors Boutib A, Chergaoui S, Marfak A , Hilali A, Youlyouz-Marfak I
Received 8 February 2022
Accepted for publication 24 May 2022
Published 2 August 2022 Volume 2022:14 Pages 975—1005
DOI https://doi.org/10.2147/IJWH.S361643
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Amal Boutib,1 Samia Chergaoui,1 Abdelghafour Marfak,1,2 Abderraouf Hilali,1 Ibtissam Youlyouz-Marfak1
1Laboratory of Health Sciences and Technologies, Higher Institute of Health Sciences, Hassan First University of Settat, Settat, Morocco; 2National School of Public Health, Rabat, Morocco
Correspondence: Ibtissam Youlyouz-Marfak, Hassan First University of Settat, Higher Institute of Health Sciences, Laboratory of Health Sciences and Technologies, Settat, 26000, Morocco, Tel +212 6 61 60 43 58, Fax +212 5 23 40 01 87, Email [email protected]
Purpose: Health-related quality of life (HRQoL) has emerged as a key concern in patient care. It has become one of the major objectives of clinical trials. Our study aims to describe the quality of life (QoL) during uncomplicated pregnancy and to assess its associated factors.
Patients and Methods: The search of articles was carried out using the online database of PUBMED and Web of Science with a limit of time between 2011 and 2021. Data were retrieved by two independent reviewers.
Results: 721 publications responding to keywords were identified, of which 73 articles on the topic were selected. The main countries that have published on this subject are Australia (n = 10) and China (n = 7). Twenty-three articles deal with QoL for pathological pregnancies. All the pathologies studied have a negative impact on the HRQoL of pregnant women, and its improvement depends on the type of treatment. Obesity, low back, and pelvic girdle pain, and hyperemesis gravidarum were the frequent pathologies during pregnancy. Socio-demographic characteristics related to improved well-being (favorable economic status, social support). Similarly, better sleep quality and moderate physical exercise were linked to an increased QoL. Physical and psychological factors were associated with a lower QoL.
Conclusion: The HRQoL refers to patients’ subjective evaluation of physical, mental, and social components of well-being. Optimizing the QoL during pregnancy necessitates a deeper understanding of their issues as well as counseling which provides support wherever needed.
Keywords: quality of life, health-related quality of life, uncomplicated pregnancy, pregnant women
Introduction
Most women have, to a greater or lesser extent, concerns about their well-being and that of their fetus during pregnancy, which is a specific condition that is not a disease or a normal state of a woman’s health. During pregnancy, women’s bodies undergo numerous biochemical, physiological, and anatomical changes. These are the first changes that make them vulnerable, both physically and mentally, and they are beyond their control. Also, hormonal changes can affect women’s emotions, leading to psychological issues like anxiety and depression. Even during a normal pregnancy, these changes can impair any woman’s ability to carry out her usual responsibilities. Changes occur in the physical, spiritual, and social dimensions as well as in the quality of life (QoL) of pregnant women at various gestational ages.1
In recent years, there has been an increase in the number of studies on QoL in worldwide literature, and it has become a popular topic in today’s society.2 It is defined by the World Health Organization as an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns.3 In the field of health, the term Health-Related Quality of Life (HRQoL) is frequently used, which considers aspects such as illnesses, disorders, and the need for therapeutic interventions.4
Women’s perceived QoL is essential to the concept of perinatal health, which encompasses physical, psychological, and social domains and is influenced by clinical and non-clinical events that are significant for women during pregnancy.5 The HRQoL is an important determinant of healthcare utilization and can be used to track medical outcomes.6 It has long been regarded as a significant outcome of nursing and medical interventions and research, to ameliorate the quality of life.7 Moreover, measuring HRQoL during the prenatal period gives valuable insight into this important phase and can help anticipate the mother’s early postnatal adjustment.8
Furthermore, the efficiency of nursing interventions to ameliorate women’s HRQoL during pregnancy has been documented in international research and systematic reviews.9 Hence, studying the scientific literature on the HRQoL in pregnancy might impact positively on the pregnant women’s well-being, and perhaps promote health interventions that can provide holistic and humanized care to the woman. To our knowledge, there is no review of the literature to describe the quality of life of pregnant women in primary care over the past ten years. The objectives of this study were to describe the quality of life during uncomplicated pregnancy and to assess its associated factors.
Quality of Life (QoL): Definition and Theory
Quality of life was defined by the WHO in 1993 as “the perception that an individual has of his place in life, in the context of the culture and of the value system in which he lives, in relation to his goals, expectations, standards, and concerns. It is a very broad concept that can be influenced in complex ways by the subject’s physical health, psychological state, level of independence, social relationships, and relationship to essential elements of their environment”. This definition describes QoL as satisfaction within different areas of existence. It is an individual notion: everyone, healthy or sick, has his perception of the QoL with his desires, wishes, satisfaction and a goal to be achieved.
Researchers have increasingly used the concept of QoL in the last five decades, particularly in the field of health care.10 As one of life’s most important aspects, health is a factor that has a significant impact on general QoL. It is then considered synonymous with “perceptual health” or “subjective health”. The HRQoL remains multi-dimensional and takes into account the physical, psychological, relational, symptomatic areas as well as sexuality and self-image.11
The factors that go into determining the indicators of QoL are material living conditions, which are divided into degraded housing conditions and financial constraints, psychosocial risks at work or ill-being at work, lack of confidence in society, weak social ties, economic and physical insecurities, as well as health which presents itself by two factors; the first is emotional discomfort or stress in everyday life due to the existence of mood disorders, lack of energy, lack of calm and tranquility or fatigue at the time of awakening. And the second is the poor physical health which is explained by the perception of the individual of his state of health, the existence of chronic disease, or discomfort to perform daily activities such as pregnancy for example, which is the case studied in our research.12
Health-Related Quality of Life (HRQoL): Measurement Instruments
The subjective HRQoL measure has been established as a legitimate dimension for evaluating the benefits of health interventions, in addition to clinically objective measures, to assess the impact of a disease or a health intervention from the patient’s perspective.13 The HRQoL is measured through the use of a questionnaire administered to patients. These questionnaires are multidimensional, and each dimension is indirectly measured by a set of items to respond to the characteristics of the measured concept.14 The method of assessment varies depending on the study: the scale can be self-administered by giving the participant a questionnaire to fill out so that he can complete each item without assistance, or administered by a researcher who asks questions about the patient’s entire life.
Many instruments for measuring the QoL have been developed to aid in the assessment of a patient’s health. In this regard, there are two types of instruments to assess the HRQoL: generic instruments (Table 1) and specific instruments. Generic instruments provide data on health status and QoL, regardless of pathology or even in the absence of pathology and can be used in general population. Also, their broader nature makes them preferable when the goal of measurement is to compare groups or individuals who have different health conditions. Specific QoL measurements focus on providing data that is specific to a disease. Patients cannot be compared to others suffering from other pathologies. These specific instruments are dedicated to a specific population of patients suffering from a specific pathology.
 |
Table 1 The Most Used Generic Questionnaires to Assess the Quality of Life of Pregnant Women Between 2011 and 2021 |
Materials and Methods
The focus of this bibliography review is on the evaluation of articles about the QoL related to pregnant women`s health. The search of articles was carried out using the online database of PUBMED and Web of Science with a limit of time between June 18, 2011 to July 17, 2021.
The keywords “Quality of life”, “pregnancy” and “pregnant” were searched in the titles or/and the abstracts in the articles written in English or French. The exclusion criteria were: 1) Literature reviews, meta-analysis, case reports, case series, and conference abstracts; 2) Pre-pregnancy, miscarriages, voluntary interruptions of pregnancy, childbirth, post-partum, and specific HRQoL questionnaires.
As shown in the flow chart (Figure 1), seven hundred twenty-one (721) articles were selected for initial abstract review (330 from PUBMED database and 391 from Web of Science) using advanced search provided by the two websites for the exclusion criteria (1). 97 abstracts were identified for the full article review after the title and abstract screening, of which 19 did not meet the inclusion criteria (2) and 20 articles were duplicated. Finally, 73 articles were included in the bibliography review.
 |
Figure 1 Flow chart showing the methodology for selecting articles on the quality of life in pregnant women. |
The articles are listed with details about the first author and the year of publication, country/continent, the aim of the study and the participants, the instrument used for the evaluation of the QoL and the number of assessment points, and finally the findings. The articles are grouped into 4 categories: Physiological pregnancy, pregnancy with pre-existing pathology, pregnancy with gestational pathology, and pregnancy with IVF.
Results
Article Selection
As mentioned before, 721 publications responding to keywords were identified and 73 articles on the QoL in pregnant women were selected (Table 2).
 |  |  |  |  |  |  |  |  |  |  |  |  |  |  |  |
Table 2 The Summary of Studies Assessing the Quality of Life of Pregnant Women Between 2011 and 2021 |
Since 18th June 2011 there was a slight decrease in interest in research on the QoL during pregnancy, passing from 6 publications in 2011–2012 to 4 publications in 2012–2013 and 2013–2014, then increased to 11 articles published in 2015–2016. Afterward, the number of publications dropped to 5 and 6 in 2016–2017 and 2017–2018 respectively and rose to 12 publications in 2018–2019. The next year the number declined to 7 publications but increased again to 12 publications in 2020–2021 (Figure 2). The geographical distribution of publications by continents showed that Europe and Asia are more interested in this subject (39% and 35% respectively) (Figure 3).
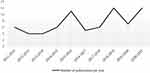 |
Figure 2 Distribution of number of articles published per year from 18/06/2011 to 17/06/2021. |
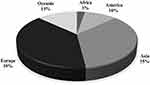 |
Figure 3 Geographical distribution by continent of publications dealing with the quality of life of pregnant women between 18/06/2011 and 17/06/2021. |
The main countries that have published on this subject between 32 countries are Australia (n = 10), China (n = 7), Iran (n = 7) and Turkey (n = 7) (Table 3). Looking closer in Africa, there were just 2 articles published from Egypt and Tunisia representing the North Africa. There was no publication from Morocco during the 10 years.
 |
Table 3 Geographical Distribution by Country of Publications Dealing with the Quality of Life of Pregnant Women Between 18/06/2011 and 17/06/2021 |
The articles that were selected were classified into four categories of obstetrics. 44 articles concern physiological pregnancies (60.27%), 16 articles concern pregnancies with gestational pathology (21.91%), 7 articles for pregnancies with pre-existing pathology (9.6%) and 6 articles are dealing with In Vitro Fertilization pregnancies (8.22%) (Figure 4).
 |
Figure 4 Number of articles evaluating the quality of life in pregnancy by the category of obstetrics from 18/06/2011 to 17/06/2021. |
Among the articles on the QoL during pregnancy related to pathology, a variety of pathologies have been explored namely the obesity, low back and pelvic girdle pain, and hyperemesis gravidarum (Table 4).
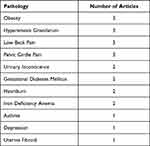 |
Table 4 Pathologies Studied in Relation to Quality of Life During Pregnancy |
17 different questionnaires were used in the articles of our review, the most used are The Short Form 36 Health Survey Questionnaire (SF-36) in 23 studies, The Short Form 12 Health Survey Questionnaire (SF-12) in 15 studies, and The World Health Organization Quality-of-Life Scale (WHOQOL-BREF) was used in 11 studies (Table 5).
 |
Table 5 Distribution of the Instruments of Quality of Life Used in the Review |
From the 73 articles studied, 54 are based on no more than 2 points of measurements of QoL during pregnancy, 31 of which are based on just one point of measurement (Figure 5).
 |
Figure 5 Number of points of measurement used to assess the quality of life during pregnancy. |
After reviewing the publications of our bibliography, we can summarize the results of the QoL in pregnant women in the physiological, pathological, and assisted pregnancies, also the factors impacting the QoL during pregnancy.
The Quality of Life of Pregnant Women
Physiological Pregnancies
For the physiological pregnancies, the QoL has proven to be good and excellent.15 However, Emmanuel et al found that the mean scores for the mental and physical domains of the QoL were lower than population norms.16 During the stages of pregnancy, general health increased from the 1st to the 2nd trimester17 and then the HRQoL decreased over time at the 2nd and the 3rd trimesters,18 mainly in the physical health,17–22 the mental health18,21,23 and the social functioning.17,19,24 The perceived health status was lower at the 9th month than the 3rd month of gestation18 and it was in the domains of “role limitations due to emotional problems”, “general health perception”, and “general health change”.25 On the contrary, Vachkova et al and Alzbon et al highlighted in their study that there was no difference in QoL between women in different trimesters of pregnancy.23,26
Pathological Pregnancies
Passing to publications with pathological pregnancies, eleven pathologies affecting the QoL were studied (Table 2).
Heartburn and regurgitation are common pregnancy symptoms, affecting up to 80% of women in their late pregnancy. This symptom is caused by increased reflux of gastric contents into the esophagus, which is facilitated by pregnancy-related hormonal changes.27 Dal Alba et al found that heartburn and regurgitation affect physical health, emotional health, and the social functioning of pregnant women and decrease their QoL.28 In contrast, the treatment of heartburn in pregnancy by receiving an alginate-based reflux suppressant or magnesium-aluminum antacid gel showed an improvement in the QoL of pregnant women.29 Hyperemesis gravidarum (HG) is characterized by severe nausea and excessive vomiting starting before the end of the 22nd week of gestation.30 For the treatment, there was no difference in QoL between rapid intravenous rehydration and routine care in pregnant women suffering from Nausea and Vomiting (NV) and/or HG.31 Also, using the Hyperemesis Impact of Symptoms questionnaire to tailor a care plan to address women’s individual needs was not associated with any significant improvements in the QoL,32 also the early enteral tube feeding in addition to standard care with intravenous rehydration and antiemetic treatment did not affect the QoL in women with Hyperemesis gravidarum.33
Low back pain (LBP) has a negative impact on pregnant women’s QoL, whereas Progressive Muscle Relaxation exercises accompanied by music improve their QoL.34 This is also true for the QoL of women receiving telephone-supported ergonomic education on pregnancy-related low back pain, except for physical functioning35 which can be increased by receiving ear acupuncture for pregnancy‐related LBP and/or posterior pelvic girdle pain (PGP).36 Also, the lumbopelvic belt helps increasing the overall QoL in pregnant women with PGP,37 but no significant difference in QoL between pregnant women receiving craniosacral therapy and those with standard treatment.38
The most frequent benign tumors in women are uterine fibroids (UFs). They are likely to cause numerous clinical symptoms in pregnant women, including pain, menorrhagia, and other obstetric problems. And impacts their QoL in physical health (mobility, pain and discomfort) and mental health (anxiety and depression) especially in pregnant women with less parity.39 Stress urinary incontinence (SUI) is the involuntary loss of urine on effort or physical exertion, sneezing, or coughing. And the most frequent type of urinary incontinence (UI) in pregnant women. Lin et al showed that women with SUI during pregnancy featured worse mental component summary scores.40 In addition, leakage in pregnant women with UI affects their physical, mental and social HRQoL domains.41
One of the most common chronic medical disorders that might make pregnancy more difficult is asthma. Its severity and exacerbations have both been associated with worse perinatal outcomes. However, in the study of Powell et al pregnant women with asthma reported good QoL.42
In obstetrics and perinatal care, anemia is a common issue. True anemia is defined as a hemoglobin level of less than 10.5 g/dL, regardless of gestational age. Nutritional deficits, parasite and bacterial infections, and inborn red blood cell disorders are the most common causes of anemia during pregnancy.43 For the HRQoL of life outcomes, Khalfallah et al found that pregnant women with Iron Deficiency Anemia receiving intravenous iron had significant improvement in QoL than those receiving oral treatment.44 Additionally, intravenous ferric carboxymaltose treatment improves vitality and social functioning.45
During pregnancy, both maternal obesity and gestational diabetes mellitus (GDM) are frequent. Both of these diseases have been linked to adverse pregnancy outcomes.46 GDM is a condition in which pregnant women who have never had diabetes have high blood glucose levels. Although all women have some insulin resistance during pregnancy, only a small percentage develop GDM.47 In 2019, a study found that there was no significant difference in HRQoL between the group of women receiving lifestyle counseling and the control group despite their GDM status.48 For obese pregnant women, in 2014 Claesson et al reported that physical activity among obese pregnant women provides better psychological well-being and improved QoL.49 Contrastingly, Seneviratne et al found that the antenatal exercise in overweight/obese women does not improve QoL in pregnancy.50 Also, there was no difference in QoL in obese pregnant women receiving serial weighing and dietary advice and women receiving standard antenatal care.51
Like obesity, depression is also one of the most common complications in pregnancy and it`s associated with severe health risks for both the mother and the child. For the HRQoL, a study evaluated the effectiveness of listening visits (LV) delivered at a woman’s usual point-of-care, including home visits or an ob-gyn office, and there was a greater improvement in QoL in depressed pregnant women receiving LV compared to women receiving standard social/health services.52
Assisted Pregnancies
For pregnant women with assisted conception or in vitro fertilization (IVF), the QoL decreases gradually with the progress of pregnancy,53 and they may report lower physical and better mental health during pregnancy than women with spontaneous conception.54 In the couple’s life, the existence of conflicts from pregnancy to the postpartum period and how to solve them was associated with a decrease in psychological QoL, whereas an increase in satisfaction with the marital relationship was associated with increases in all QoL domains.55 Additionally, the QoL significantly increases in women subjected to their first IVF treatment after receiving a mindfulness-based intervention (MBI),56 and among women having an assisted conception without gonadotropin stimulation.57
Factors Influencing the QoL in Pregnancy
Factors Decreasing the QoL in Pregnancy
Adolescent motherhood,58 advanced maternal age,59 high parity women,26,60,61 low educational level, the perception of fiscal situation,60 physical changes causing limitations, physical activity limitations, fear of managing labor,15 the preparedness for parenthood,60 place of receiving prenatal care,62 inadequate antenatal care consultations and living in a poor household,58 partner satisfaction,15 poor sleep quality,63 headache or migraine,64 anxiety and depression,61 fear of COVID-19,65 adherence to behavioral restrictions,66 the perception of health condition,60 higher overall gestational weight gain,67 gestational diabetes mellitus,59 the severity of nausea and vomiting,68 heart burn and regurgitation,28 low back pain,34 urinary incontinence,40,41 pathological pregnancies18 and hospitalization69 were factors frequently indicating a poor QoL during pregnancy.
Factors Increasing the QoL in Pregnancy
The following factors were strongly associated with a better quality of life: Exercise,70 moderate physical activity in water,71 high exercise adherence,70 adopting low-to-moderate intensity resistance training,72 Higher Energy Expenditures,73 clinical pilates exercises,74 having a body mass index BMI ≥ 25,75 better sleep quality,76 increase of sexual satisfaction,45 receiving a lifestyle advice,22 social support16,61 and receiving the solution-focused counselling in terms of violence.77
In contrast, planned pregnancies and history of depression were not associated with low mental or physical QoL,78 and offering an exercise program during pregnancy does not seem to influence healthy pregnant women’s psychological wellbeing and self-perceived general health.79
Discussion
Summary of Results
Quality of life is increasingly a prominent consideration in patient care. It was demonstrated by the 261% growth in the number of scientific publications related to this topic over the previous 10 years. Such tendency has reached the realm of obstetrics as well. As shown in our results, the number of articles studying the HRQoL in pregnant women increased over the past ten years, illustrating the current interest of the prenatal care. The publications were classified into four categories (physiological pregnancy, pathological pregnancy, assisted pregnancy and pregnancy with gestational pathology) to simplify the processing of articles from homogenous populations. The studies focusing on the physiological pregnancies are on the rise. Morin et al found in their research a low number of articles focusing on QoL in physiological pregnancies (21 articles from 2005 to 2015), in contrast, we found 44 articles in the same category at the last ten years.80
The specific HRQoL instruments were not included in our study because they are more focused on specific problems in pregnancy. We used the generic HRQoL questionnaires only in the inclusion criteria to focus on women`s overall well-being and their QoL. The most HRQoL instruments used are the SF-36, the SF-12 and the WHOQOL-BREF in 23, 15 and 11 articles respectively, since their time of administration is short (2–15 min), and the questions occupy multiple dimensions. Moreover, our detailed analysis reveals that the authors relied on only few points of measurement to estimate the QoL of pregnant women in most of cases. 31 articles used 1 point of measurement, 23 articles used 2 and 13 articles used 3. However, the pregnant woman`s physiological state changes frequently, which might modify her QoL on various occasions.
The HRQoL has been found to be good and excellent in physiological pregnancies. In spite of that, the mean mental and physical domain scores, were lower than population norms. During pregnancy, the QoL increased from the 1st to the 2nd trimester, then decreased in the 2nd and 3rd trimesters, notably in physical health, mental health, and social functioning. The 9th month of pregnancy had a lower perceived health status than the 3rd month. On the other hand, other researchers, found no variation in QoL among women in different trimesters of pregnancy in their trials. In our review we found that all the pathologies studied have a negative impact on the HRQoL of pregnant women, and its improvement depends on the type of the treatment. Obesity, low back and pelvic girdle pain, and hyperemesis gravidarum were the frequent pathologies during pregnancy.
Strengths and Limitations of the Study
To the best of our knowledge, this is the only systematic review of literature aiming at synthesizing data on pregnant women’s quality of life during the past 10 years. Many factors influencing the QoL during pregnancy have been studied. Our work also has its limitations: Only articles written in English or French were included in the study. As a result, the question of generalizability should be addressed. Specific HRQOL instruments were not included since they focus more on specific pregnancy issues than on women’s general well-being and QoL. Thus, the absence of a longitudinal QoL study and the unavailability of coverage of the full gestational period in terms of QoL, would very certainly cause us to reconsider the conclusions reached in most of the studies in our review.
Recommendations
Europe was the first continent interested in QoL during pregnancy, which can be explained as a result of the European strategic approach for making pregnancy safer, developed by WHO/Europe in 2008.81 While in some countries, the QoL in pregnancy has been little studied. In Morocco, there is no information provided on pregnant women`s QoL.
It should be emphasized that in many of the studies selected, the time of data collection on QoL does not span the whole pregnancy. Knowing that a woman’s physiological condition varies regularly during pregnancy, which might affect her QoL on several times, and to try to develop a standard of QoL in pregnant women in the most complete way possible, it is important to evaluate QoL with a significant number of points of measurement, encompassing the whole duration of pregnancy. This would allow the identification of critical phases of pregnancy that necessitate a change in prenatal care and would serve as a reference for assessing the impact of a specific pregnancy-related disease on QoL during this period.
Many factors were linked to pregnant women’s QoL. Socio-demographic characteristics related to improved well-being (favorable economic status, social support). Similarly, better sleep quality and moderate physical exercise were linked to an increased QoL. Physical and psychological factors were associated with a lower QoL. Noting that there are more factors reducing the QoL than those that improve it in pregnant women, and given the variety of elements influencing the QoL, the medical and paramedical professions must collaborate with social agencies, networks, and associations.
Conclusion
The most significant findings in our study were the variety of factors associated with poor quality of life in pregnant women. These include socio-demographic, economic, and obstetrical characteristics, as well as in vitro fertilization and the presence of pathologies during pregnancy. Another important finding is the lack of studies assessing the HRQoL with a significant number of points of measurement, encompassing the whole duration of pregnancy.
To conclude, even though the evaluation of the health-related quality of life in pregnancy is a growingly universal issue, it would be fascinating to develop a standardized curve for the change in the quality of life in pregnant women and to investigate the factors that might affect their quality of life. This would allow us to emphasize important phases of pregnancy and try to repair or remove issues impacting the quality of life, or even go so far as to question the influence of poor quality of life during pregnancy has on women`s childbirth, the postpartum, and the mother-child attachment in general.
Abbreviations
BMI, body mass index; COVID-19, coronavirus disease of 2019; EE, energy expenditures; GDM, gestational diabetes mellitus; HG, Hyperemesis Gravidarum; HRQoL, Health-related Quality of Life; IVF, in vitro fertilization; LBP, low back pain; LV, listening visits; MBI, mindfulness-based intervention; MCS, mental component summary; NV, nausea and vomiting; NVP, nausea and vomiting of pregnancy; PCS, physical component summary; PGP, pelvic girdle pain; PP, post-partum; QoL, quality of life; SF-12, the short form 12 health survey questionnaire; SF-36, the short form 36 health survey questionnaire; SUI, stress urinary incontinence; UFs, uterine fibroids; UI, urinary incontinence; WHO, world health organization; WHOQOL-BREF, the world health organization quality-of-life scale.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Abbaszadeh F, Baghery A, Mehran N. Quality of life among pregnant women. Hayat. 2009;15(1):41–48.
2. Casarin S, Barboza M, Siqueira H. Quality of life in pregnancy: literature systematic review. Revista de Enfermagem UFPE. 2010;4. doi:10.5205/reuol.892-7739-3-LE.0403esp201015
3. Whoqol Group. The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41(10):1403–1409. doi:10.1016/0277-9536(95)00112-k
4. Nicolussi AC, Sawada NO. Factors that influence the quality of life of patients with colon and rectal cancer. Acta paul enferm. 2010;23(1):125–130. doi:10.1590/S0103-21002010000100020
5. Jomeen J, Martin C. Perinatal quality of life: is it important for childbearing women? Pract Midwife. 2012;15(4):30–34.
6. Gerhardt CA, Britto MT, Mills L, Biro FM, Rosenthal SL. Stability and predictors of health-related quality of life of inner-city girls. J Dev Behav Pediatr. 2003;24(3):189–194. doi:10.1097/00004703-200306000-00010
7. Kyle SD, Morgan K, Espie CA. Insomnia and health-related quality of life. Sleep Med Rev. 2010;14(1):69–82. doi:10.1016/j.smrv.2009.07.004
8. Ngai FW, Chan SWC. Psychosocial factors and maternal wellbeing: an exploratory path analysis. Int J Nurs Stud. 2011;48(6):725–731. doi:10.1016/j.ijnurstu.2010.11.002
9. Armstrong KL, Fraser JA, Dadds MR, Morris J. Promoting secure attachment, maternal mood and child health in a vulnerable population: a randomized controlled trial. J Paediatr Child Health. 2000;36(6):555–562. doi:10.1046/j.1440-1754.2000.00591.x
10. Taillefer MC, Dupuis G, Roberge MA, Le May S. Health-related quality of life models: systematic review of the literature. Soc Indic Res. 2003;64(2):293–323. doi:10.1023/A:1024740307643
11. Mercier M, Schraub S. Quality of life: what are the assessment instruments?; 2005. Available from: http://hdl.handle.net/2042/9760.
12. Amiel M-H, Godefroy P, Lollivier S. Quality of life and well-being often go hand in hand. Institut National de la statistique et des études économiques. NO. 1428 - February 2013. Available from: www.insee.fr.
13. Haute Autorité de Santé. Evaluation of health technologies at HAS: Place of quality of life. Saint-Denis La Plaine: High Authority for Health; 2018.
14. Emrani L, Senhaji M, Bendriss A. Measuring health-related quality of life in the population of Tetouan, Morocco, by the SF-36: normative data and the influence of gender and age. East Mediterran Health J. 2016;22:133–141.
15. Mazúchová L, Kelčíková S, Dubovická Z. Measuring women’s quality of life during pregnancy. Kontakt. 2018;20(1):e31–e36. doi:10.1016/j.kontakt.2017.11.004
16. Emmanuel E, St John W, Sun J. Relationship between social support and quality of life in childbearing women during the perinatal period. J Obstetr Gynecol Neonatal Nurs. 2012;41(6):E62–E70. doi:10.1111/j.1552-6909.2012.01400.x
17. Chang SR, Chen KH, Lin MI, Lin HH, Huang LH, Lin WA. A repeated measures study of changes in health-related quality of life during pregnancy and the relationship with obstetric factors. J Adv Nurs. 2014;70(10):2245–2256. doi:10.1111/jan.12374
18. Morin M, Claris O, Dussart C, et al. Health‐related quality of life during pregnancy: a repeated measures study of changes from the first trimester to birth. Acta Obstet Gynecol Scand. 2019;98(10):1282–1291. doi:10.1111/aogs.13624
19. Nascimento SL, Surita FG, Parpinelli MÂ, Siani S, Pinto e Silva JL. The effect of an antenatal physical exercise programme on maternal/perinatal outcomes and quality of life in overweight and obese pregnant women: a randomised clinical trial. BJOG. 2011;118(12):1455–1463. doi:10.1111/j.1471-0528.2011.03084.x
20. Moccellin AS, Driusso P. Adjustments in static and dynamic postural control during pregnancy and their relationship with quality of life: a descriptive study. Fisioterapia. 2012;34(5):196–202. doi:10.1016/j.ft.2012.03.004
21. Lau Y. The effect of maternal stress and health-related quality of life on birth outcomes among Macao Chinese pregnant women. J Perinat Neonatal Nurs. 2013;27(1):14–24. doi:10.1097/JPN.0b013e31824473b9
22. Dodd JM, Newman A, Moran LJ, et al. The effect of antenatal dietary and lifestyle advice for women who are overweight or obese on emotional well-being: the LIMIT randomized trial. Acta Obstet Gynecol Scand. 2016;95(3):309–318. doi:10.1111/aogs.12832
23. Vachkova E, Jezek S, Mares J, Moravcova M. The evaluation of the psychometric properties of a specific quality of life questionnaire for physiological pregnancy. Health Qual Life Outcomes. 2013;11(1):214. doi:10.1186/1477-7525-11-214
24. Chen YH, Huang JP, Au HK, Chen YH. High risk of depression, anxiety, and poor quality of life among experienced fathers, but not mothers: a prospective longitudinal study. J Affect Disord. 2019;242:39–47. doi:10.1016/j.jad.2018.08.042
25. van den Bosch AS, Goossens M, Bonouvrié K, et al. Maternal quality of life in routine labor epidural analgesia versus labor analgesia on request: results of a randomized trial. Qual Life Res. 2018;27(8):2027–2033. doi:10.1007/s11136-018-1838-z
26. Alzboon G, Vural G. Factors influencing the quality of life of healthy pregnant women in North Jordan. Medicina. 2019;55(6):278. doi:10.3390/medicina55060278
27. Dall’Alba V, Fornari F, Krahe C, Callegari-Jacques SM, Silva de Barros SG. Heartburn and regurgitation in pregnancy: the effect of fat ingestion. Dig Dis Sci. 2010;55(6):1610–1614. doi:10.1007/s10620-009-0932-z
28. Dall’alba V, Callegari-Jacques SM, Krahe C, et al. Health-related quality of life of pregnant women with heartburn and regurgitation. Arq Gastroenterol. 2015;52(2):100–104. doi:10.1590/S0004-28032015000200005
29. Meteerattanapipat P, Phupong V. Efficacy of alginate-based reflux suppressant and magnesium-aluminium antacid gel for treatment of heartburn in pregnancy: a randomized double-blind controlled trial. Sci Rep. 2017;7:44830. doi:10.1038/srep44830
30. World Health Organization. International statistical classification of diseases and related health problems. World Health Organization; 2015. Available from: https://apps.who.int/iris/handle/10665/246208.
31. McParlin C, Carrick-Sen D, Steen IN, Robson SC. Hyperemesis in Pregnancy Study: a pilot randomised controlled trial of midwife-led outpatient care. Eur J Obstetr Gynecol Reprod Biol. 2016;200:6–10. doi:10.1016/j.ejogrb.2016.02.016
32. Fletcher SJ, Waterman H, Nelson L, et al. Holistic assessment of women with hyperemesis gravidarum: a randomised controlled trial. Int J Nurs Stud. 2015;52(11):1669–1677. doi:10.1016/j.ijnurstu.2015.06.007
33. Grooten IJ, Koot MH, van der Post JA, et al. Early enteral tube feeding in optimizing treatment of hyperemesis gravidarum: the Maternal and Offspring outcomes after Treatment of HyperEmesis by Refeeding (MOTHER) randomized controlled trial. Am J Clin Nutr. 2017;106(3):812–820. doi:10.3945/ajcn.117.158931
34. Akmeşe ZB, Oran NT. Effects of progressive muscle relaxation exercises accompanied by music on low back pain and quality of life during pregnancy. J Midwifery Womens Health. 2014;59(5):503–509. doi:10.1111/jmwh.12176
35. Pekçetin S, Özdinç S, Ata H, Can HB, Elter K. Effect of telephone-supported ergonomic education on pregnancy-related low back pain. Women Health. 2019;59(3):294–304. doi:10.1080/03630242.2018.1478364
36. Vas J, Cintado MC, Aranda-Regules JM, Aguilar I, Rivas Ruiz F. Effect of ear acupuncture on pregnancy-related pain in the lower back and posterior pelvic girdle: a multicenter randomized clinical trial. Acta Obstet Gynecol Scand. 2019;98(10):1307–1317. doi:10.1111/aogs.13635
37. Kordi R, Abolhasani M, Rostami M, Hantoushzadeh S, Mansournia MA, Vasheghani-Farahani F. Comparison between the effect of lumbopelvic belt and home based pelvic stabilizing exercise on pregnant women with pelvic girdle pain; a randomized controlled trial. J Back Musculoskelet Rehabil. 2013;26(2):133–139. doi:10.3233/BMR-2012-00357
38. Elden H, Östgaard HC, Glantz A, Marciniak P, Linnér AC, Olsén MF. Effects of craniosacral therapy as adjunct to standard treatment for pelvic girdle pain in pregnant women: a multicenter, single blind, randomized controlled trial. Acta Obstet Gynecol Scand. 2013;92(7):775–782. doi:10.1111/aogs.12096
39. Ming WK, Wu H, Wu Y, et al. Health-related quality of life in pregnancy with uterine fibroid: a cross-sectional study in China. Health Qual Life Outcomes. 2019;17(1):89. doi:10.1186/s12955-019-1153-6
40. Lin YH, Chang SD, Hsieh WC, et al. Persistent stress urinary incontinence during pregnancy and one year after delivery; its prevalence, risk factors and impact on quality of life in Taiwanese women: an observational cohort study. Taiwan J Obstet Gynecol. 2018;57(3):340–345. doi:10.1016/j.tjog.2018.04.003
41. Martínez Franco E, Parés D, Lorente Colomé N, Méndez Paredes JR, Amat Tardiu L. Urinary incontinence during pregnancy. Is there a difference between first and third trimester? Eur J Obstetr Gynecol Reprod Biol. 2014;182:86–90. doi:10.1016/j.ejogrb.2014.08.035
42. Powell H, McCaffery K, Murphy VE, et al. Psychosocial outcomes are related to asthma control and quality of life in pregnant women with asthma. J Asthma. 2011;48(10):1032–1040. doi:10.3109/02770903.2011.631239
43. Breymann C. Iron deficiency anemia in pregnancy. Semin Hematol. 2015;52(4):339–347. doi:10.1053/j.seminhematol.2015.07.003
44. Khalafallah AA, Hyppa A, Chuang A, et al. A prospective randomised controlled trial of a single intravenous infusion of ferric carboxymaltose vs single intravenous iron polymaltose or daily oral ferrous sulphate in the treatment of iron deficiency anaemia in pregnancy. Semin Hematol. 2018;55(4):223–234. doi:10.1053/j.seminhematol.2018.04.006
45. Breymann C, Milman N, Mezzacasa A, Bernard R, Dudenhausen J; FER-ASAP Investigators. Ferric carboxymaltose vs. oral iron in the treatment of pregnant women with iron deficiency anemia: an international, open-label, randomized controlled trial (FER-ASAP). J Perinat Med. 2017;45(4):443–453. doi:10.1515/jpm-2016-0050
46. Alfadhli EM. Maternal obesity influences birth weight more than gestational diabetes. BMC Pregnancy Childbirth. 2021;21(1):111. doi:10.1186/s12884-021-03571-5
47. Daci A, Elshani B, Giangiacomo B. Gestational diabetes mellitus (GDM) in the Republic of Kosovo: a retrospective pilot study. Med Arch. 2013;67(2):88–90. doi:10.5455/medarh.2013.67.88-90
48. Sahrakorpi N, Rönö K, Koivusalo SB, Stach-Lempinen B, Eriksson JG, Roine RP. Effect of lifestyle counselling on health-related quality of life in women at high risk for gestational diabetes. Eur J Public Health. 2019;29(3):408–412. doi:10.1093/eurpub/cky248
49. Claesson IM, Klein S, Sydsjö G, Josefsson A. Physical activity and psychological well-being in obese pregnant and postpartum women attending a weight-gain restriction programme. Midwifery. 2014;30(1):11–16. doi:10.1016/j.midw.2012.11.006
50. Seneviratne SN, Jiang Y, Derraik J, et al. Effects of antenatal exercise in overweight and obese pregnant women on maternal and perinatal outcomes: a randomised controlled trial. BJOG. 2016;123(4):588–597. doi:10.1111/1471-0528.13738
51. McCarthy EA, Walker SP, Ugoni A, Lappas M, Leong O, Shub A. Self-weighing and simple dietary advice for overweight and obese pregnant women to reduce obstetric complications without impact on quality of life: a randomised controlled trial. BJOG. 2016;123(6):965–973. doi:10.1111/1471-0528.13919
52. Segre LS, Brock RL, O’Hara MW. Depression treatment for impoverished mothers by point-of-care providers: a randomized controlled trial. J Consult Clin Psychol. 2015;83(2):314–324. doi:10.1037/a0038495
53. De Pascalis L, Agostini F, Monti F, Paterlini M, Fagandini P, La Sala GB. A comparison of quality of life following spontaneous conception and assisted reproduction. Int J Gynaecol Obstet. 2012;118(3):216–219. doi:10.1016/j.ijgo.2012.04.020
54. Vinturache A, Stephenson N, McDonald S, Wu M, Bayrampour H, Tough S. Health-related quality of life in pregnancy and postpartum among women with assisted conception in Canada. Fertil Steril. 2015;104(1):188–195.e1. doi:10.1016/j.fertnstert.2015.04.012
55. Gameiro S, Nazaré B, Fonseca A, Moura-Ramos M, Canavarro MC. Changes in marital congruence and quality of life across the transition to parenthood in couples who conceived spontaneously or with assisted reproductive technologies. Fertil Steril. 2011;96(6):1457–1462. doi:10.1016/j.fertnstert.2011.09.003
56. Li J, Long L, Liu Y, He W, Li M. Effects of a mindfulness-based intervention on fertility quality of life and pregnancy rates among women subjected to first in vitro fertilization treatment. Behav Res Ther. 2016;77:96–104. doi:10.1016/j.brat.2015.12.010
57. Haemmerli Keller K, Alder G, Loewer L, Faeh M, Rohner S, von Wolff M. Treatment-related psychological stress in different in vitro fertilization therapies with and without gonadotropin stimulation. Acta Obstet Gynecol Scand. 2018;97(3):269–276. doi:10.1111/aogs.13281
58. Ali N, Sheikh N, Akram R, et al. Measuring perinatal and postpartum quality of life of women and associated factors in semi-urban Bangladesh. Qual Life Res. 2019;28(11):2989–3004. doi:10.1007/s11136-019-02247-0
59. Liu J, Wang S, Leng J, et al. Impacts of gestational diabetes on quality of life in Chinese pregnant women in urban Tianjin, China. Prim Care Diabetes. 2020;14(5):425–430. doi:10.1016/j.pcd.2019.12.004
60. Dağlar G, Bilgic D, Özkan SA. Factors affecting the quality of life among pregnant women during third trimester of pregnancy. Cukurova Med J. 2019;44(3):772–781. doi:10.17826/cumj.482553
61. Moghaddam Hosseini V, Gyuró M, Makai A, Varga K, Hashemian M, Várnagy Á. Prenatal health-related quality of life assessment among Hungarian pregnant women using PROMIS-43. Clin Epidemiol Glob Health. 2021;9:237–244. doi:10.1016/j.cegh.2020.09.005
62. Zarei S, Mirghafourvand M, Mohammad-Alizadeh-Charandabi S, Effati- Daryani F, Shiri-Sarand F. Predictors of quality of life in pregnant women visiting health centers of Tabriz, Iran. JMRH. 2018. doi:10.22038/jmrh.2018.10378
63. Du M, Liu J, Han N, et al. Maternal sleep quality during early pregnancy, risk factors and its impact on pregnancy outcomes: a prospective cohort study. Sleep Med. 2021;79:11–18. doi:10.1016/j.sleep.2020.12.040
64. Peng W, Lauche R, Frawley J, Sibbritt D, Adams J. Utilization of complementary and alternative medicine and conventional medicine for headache or migraine during pregnancy: a cross-sectional survey of 1835 pregnant women. Complement Ther Med. 2018;41:192–195. doi:10.1016/j.ctim.2018.09.027
65. Naghizadeh S, Mirghafourvand M. Relationship of fear of COVID-19 and pregnancy-related quality of life during the COVID-19 pandemic. Arch Psychiatr Nurs. 2021;35(4):364–368. doi:10.1016/j.apnu.2021.05.006
66. Lau Y. Traditional Chinese pregnancy restrictions, health-related quality of life and perceived stress among pregnant women in Macao, China. Asian Nurs Res. 2012;6(1):27–34. doi:10.1016/j.anr.2012.02.005
67. Altazan AD, Redman LM, Burton JH, et al. Mood and quality of life changes in pregnancy and postpartum and the effect of a behavioral intervention targeting excess gestational weight gain in women with overweight and obesity: a parallel-arm randomized controlled pilot trial. BMC Pregnancy Childbirth. 2019;19(1):50. doi:10.1186/s12884-019-2196-8
68. Hirose M, Tamakoshi K, Takahashi Y, Mizuno T, Yamada A, Kato N. The effects of nausea, vomiting, and social support on health-related quality of life during early pregnancy: a prospective cohort study. J Psychosom Res. 2020;136:110168. doi:10.1016/j.jpsychores.2020.110168
69. Nakamura Y, Takeishi Y, Atogami F, Yoshizawa T. Assessment of quality of life in pregnant Japanese women: comparison of hospitalized, outpatient, and non-pregnant women. Nurs Health Sci. 2012;14(2):182–188. doi:10.1111/j.1442-2018.2011.00676.x
70. Haakstad LAH, Torset B, Bø K. What is the effect of regular group exercise on maternal psychological outcomes and common pregnancy complaints? An assessor blinded RCT. Midwifery. 2016;32:81–86. doi:10.1016/j.midw.2015.10.008
71. Rodríguez-Blanque R, Aguilar-Cordero MJ, Marín-Jiménez AE, Menor-Rodríguez MJ, Montiel-Troya M, Sánchez-García JC. Water exercise and quality of life in pregnancy: a randomised clinical trial. Int J Environ Res Public Health. 2020;17(4):E1288. doi:10.3390/ijerph17041288
72. O’Connor PJ, Poudevigne MS, Johnson KE, Brito de Araujo J, Ward-Ritacco CL. Effects of resistance training on fatigue-related domains of quality of life and mood during pregnancy: a randomized trial in pregnant women with increased risk of back pain. Psychosom Med. 2018;80(3):327–332. doi:10.1097/PSY.0000000000000559
73. Krzepota J, Sadowska D, Biernat E. Relationships between physical activity and quality of life in pregnant women in the second and third trimester. IJERPH. 2018;15(12):2745. doi:10.3390/ijerph15122745
74. Sonmezer E, Özköslü MA, Yosmaoğlu HB. The effects of clinical pilates exercises on functional disability, pain, quality of life and lumbopelvic stabilization in pregnant women with low back pain: a randomized controlled study. J Back Musculoskelet Rehabil. 2021;34(1):69–76. doi:10.3233/BMR-191810
75. Liang CC, Chao M, Chang SD, Chiu SYH. Impact of prepregnancy body mass index on pregnancy outcomes, incidence of urinary incontinence and quality of life during pregnancy - An observational cohort study. Biomed J. 2020;43(6):476–483. doi:10.1016/j.bj.2019.11.001
76. Tsai SY, Lee PL, Lin JW, Lee CN. Cross-sectional and longitudinal associations between sleep and health-related quality of life in pregnant women: a prospective observational study. Int J Nurs Stud. 2016;56:45–53. doi:10.1016/j.ijnurstu.2016.01.001
77. Dinmohammadi S, Dadashi M, Ahmadnia E, Janani L, Kharaghani R. The effect of solution-focused counseling on violence rate and quality of life of pregnant women at risk of domestic violence: a randomized controlled trial. BMC Pregnancy Childbirth. 2021;21(1):221. doi:10.1186/s12884-021-03674-z
78. Gariepy A, Lundsberg LS, Vilardo N, Stanwood N, Yonkers K, Schwarz EB. Pregnancy context and women’s health-related quality of life. Contraception. 2017;95(5):491–499. doi:10.1016/j.contraception.2017.02.001
79. Gustafsson MK, Stafne SN, Romundstad PR, Mørkved S, Salvesen K, Helvik AS. The effects of an exercise programme during pregnancy on health-related quality of life in pregnant women: a Norwegian randomised controlled trial. BJOG. 2016;123(7):1152–1160. doi:10.1111/1471-0528.13570
80. Morin M, Vayssiere C, Claris O, et al. Evaluation of the quality of life of pregnant women from 2005 to 2015. Eur J Obstetr Gynecol Reprod Biol. 2017;214:115–130. doi:10.1016/j.ejogrb.2017.04.045
81. World Health Organization. European Strategic Approach for Making Pregnancy Safer: Improving Maternal and Perinatal Health. World Health Organization; 2008:41.
82. Khalifa E, Mohammad H, Abdullah A, Abdel-Rasheed M, Khairy M, Hosni M. Role of suppression of endometriosis with progestins before IVF-ET: a non-inferiority randomized controlled trial. BMC Pregnancy Childbirth. 2021;21(1):264. doi:10.1186/s12884-021-03736-2
83. Keulen JKJ, Nieuwkerk PT, Kortekaas JC, et al. What women want and why. Women’s preferences for induction of labour or expectant management in late-term pregnancy. Women Birth. 2021;34(3):250–256. doi:10.1016/j.wombi.2020.03.010
84. Alizadeh S, Riazi H, Majd HA, Ozgoli G. The effect of sexual health education on sexual activity, sexual quality of life, and sexual violence in pregnancy: a prospective randomized controlled trial. BMC Pregnancy Childbirth. 2021;21(1):334. doi:10.1186/s12884-021-03803-8
85. Yikar SK, Nazik E. Effects of prenatal education on complaints during pregnancy and on quality of life. Patient Educ Couns. 2019;102(1):119–125. doi:10.1016/j.pec.2018.08.023
86. Noorbala AA, Afzali HM, Abedinia N, Akhbari M, Moravveji SA, Shariat M. Investigation of the effectiveness of psychiatric interventions on the mental health of pregnant women in Kashan City – Iran: a clinical trial study. Asian J Psychiatr. 2019;46:79–86. doi:10.1016/j.ajp.2019.09.036
87. Loughnan SA, Sie A, Hobbs MJ, et al. A randomized controlled trial of “MUMentum Pregnancy”: internet-delivered cognitive behavioral therapy program for antenatal anxiety and depression. J Affect Disord. 2019;243:381–390. doi:10.1016/j.jad.2018.09.057
88. Dodd JM, Louise J, Deussen AR, et al. Effect of metformin in addition to dietary and lifestyle advice for pregnant women who are overweight or obese: the GRoW randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2019;7(1):15–24. doi:10.1016/S2213-8587(18
89. Turkstra E, Mihala G, Scuffham PA, et al. An economic evaluation alongside a randomised controlled trial on psycho-education counselling intervention offered by midwives to address women’s fear of childbirth in Australia. Sex Reprod Healthc. 2017;11:1–6. doi:10.1016/j.srhc.2016.08.003
90. Ellouze F, Bouzouita I, Chaari I, et al. Relations entre sexualité, dépression et qualité de vie chez la femme Tunisienne enceinte. Sexologies. 2017;26(4):222–227. doi:10.1016/j.sexol.2017.06.002
91. Zare F, Aghamolaei T, Ghanbarnejad A, Zarei H, Asadian A, Dadipoor S. Quality of life of pregnant women in Bandar Abbas. Hormozgan Med J. 2016;19:8.
92. Petrov Fieril K, Glantz A, Fagevik Olsen M. The efficacy of moderate-to-vigorous resistance exercise during pregnancy: a randomized controlled trial. Acta Obstet Gynecol Scand. 2015;94(1):35–42. doi:10.1111/aogs.12525
93. Lau Y, Yin L. Maternal, obstetric variables, perceived stress and health-related quality of life among pregnant women in Macao, China. Midwifery. 2011;27(5):668–673. doi:10.1016/j.midw.2010.02.008
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
