Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Quality of life and adherence to inhaled corticosteroids and tiotropium in COPD are related
Authors Ter Huurne K, Kort S, van der Palen J , van Beurden W , Movig K, van der Valk P, Brusse-Keizer M
Received 26 February 2016
Accepted for publication 11 April 2016
Published 26 July 2016 Volume 2016:11(1) Pages 1679—1688
DOI https://doi.org/10.2147/COPD.S107303
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Kirsten Koehorst-ter Huurne,1 Sharina Kort,1 Job van der Palen,1,3 Wendy JC van Beurden,1 Kris LL Movig,2 Paul van der Valk,1 Marjolein Brusse-Keizer1
1Department of Pulmonary Medicine, 2Department of Clinical Pharmacy, Medisch Spectrum Twente, 3Department of Research Methodology, Measurement, and Data Analysis, University of Twente, Enschede, the Netherlands
Background: Poor adherence to inhaled medications in COPD patients seems to be associated with an increased risk of death and hospitalization. Knowing the determinants of nonadherence to inhaled medications is important for creating interventions to improve adherence.
Objectives: To identify disease-specific and health-related quality of life (HRQoL) factors, associated with adherence to inhaled corticosteroids (ICS) and tiotropium in COPD patients.
Methods: Adherence of 795 patients was recorded over 3 years and was deemed optimal at >75%–≤125%, suboptimal at ≥50%–<75%, and poor at <50% (underuse) or >125% (overuse). Health-related quality of life was measured with the Clinical COPD Questionnaire and the EuroQol-5D questionnaire.
Results: Patients with a higher forced expiratory volume in 1 second (FEV1)/vital capacity (VC) (odds ratio [OR] =1.03) and ≥1 hospitalizations in the year prior to inclusion in this study (OR =2.67) had an increased risk of suboptimal adherence to ICS instead of optimal adherence. An increased risk of underuse was predicted by a higher FEV1/VC (OR =1.05). Predictors for the risk of overuse were a lower FEV1 (OR =0.49), higher scores on Clinical COPD Questionnaire-question 3 (anxiety for dyspnea) (OR =1.26), and current smoking (OR =1.73). Regarding tiotropium, predictors for suboptimal use were a higher FEV1/VC (OR =1.03) and the inability to perform usual activities as asked by the EuroQol-5D questionnaire (OR =3.09). A higher FEV1/VC also was a predictor for the risk of underuse compared to optimal adherence (OR =1.03). The risk of overuse increased again with higher scores on Clinical COPD Questionnaire-question 3 (OR =1.46).
Conclusion: Several disease-specific and quality of life factors are related to ICS and tiotropium adherence, but a clear profile of a nonadherent patient cannot yet be outlined. Overusers of ICS and tiotropium experience more anxiety.
Keywords: chronic obstructive pulmonary disease, adherence, inhalation medication, quality of life
Background
COPD is a major global health problem, currently being the fifth leading cause of morbidity. It is expected to be the third leading cause of mortality in 2020.1 Treatment of COPD is supportive, aimed at relieving symptoms, decreasing the number of exacerbations, and improving the quality of life.2 Pharmacotherapy consists of inhaled medications, including short- and long-acting bronchodilators, such as tiotropium bromide, to relieve dyspnea symptoms and inhalation corticosteroids (ICS) to suppress the prominent pulmonary inflammation.2 Large randomized trials have demonstrated that long-term use of long-acting bronchodilators and ICS reduces symptoms, improves quality of life and exercise tolerance, reduces number and severity of exacerbations, and may decrease mortality.3–5
The effectiveness of inhaled medications is substantially influenced by a patient’s therapy adherence. Adherence is essential and seems to be associated with reduced mortality and hospitalization.6–8 In common with other chronic diseases, therapy adherence in COPD patients is generally poor, varying in studies from 18% to 40% for ICS, 17% to 29% for combination medication, and 13% to 80% for long-acting sympaticomimetics.9–13 Medication adherence is influenced by patient- and medication-related factors, such as disease- and treatment acceptance, knowledge about and faith in the treatment, effective patient–clinician relationship, routinization of the pharmacological therapy, and side effects.7,14,15 Medication-related factors, such as frequent daily use, multiple dosing, and side effects, all have a negative influence on adherence.16,17 COPD patients often have a medication regimen requiring multiple daily dosages during a prolonged period and frequently use more than one medication often in different devices simultaneously, making therapy adherence a difficult task. Next to the above mentioned factors, COPD-specific factors and perceived health-related quality of life (HRQoL) may also be associated with adherence to inhalation therapy.
Understanding of determinants of adherence to inhaled medications is important to help create interventions for improving medication adherence in COPD patients. We therefore conducted a study to identify disease-specific and HRQoL factors that are associated with adherence to ICS and tiotropium in COPD patients.
Methods
Study design
This study is part of the Cohort on Mortality and Inflammation in COPD study. It concerns a single center, prospective, cohort study. From December 2005 till April 2010, 795 patients were included with a follow-up period of 3 years. Patients were recruited at the Department of Pulmonology, Medisch Spectrum Twente Hospital, Enschede. The research protocol was approved by the hospital’s Medical Ethical Committee and all patients provided written informed consent.
To be eligible for the study, patients had to meet the following criteria: 1) a clinical diagnosis of COPD, as defined by the Global Initiative for Chronic Obstructive Lung Disease criteria; 2) current or exsmoker; 3) age ≥40 years; 4) no medical condition compromising survival within the follow-up period or serious psychiatric comorbidity; 5) absence of any other lung disease; 6) no maintenance therapy with antibiotics; and 7) the ability to speak Dutch. Patients were consecutively enrolled when hospitalized for an acute exacerbation of COPD or when visiting the outpatient clinic in a stable state.
Demographic characteristics were obtained at baseline. Smoking status was determined by the Vlagtwedde questionnaire.12 Patients were dichotomously categorized as frequent (≥2 exacerbations in the year prior to inclusion in this study) or infrequent (<2 exacerbations in the year prior to inclusion in this study) exacerbators. An exacerbation was defined as a worsening of respiratory symptoms that required treatment with a short course of oral corticosteroids with or without antibiotics. Data on exacerbations and number of hospitalizations 1 year prior to inclusion in this study were recorded from hospital records and dichotomized as ≥1 versus no hospitalizations. Data on the common comorbidities myocardial infarction, congestive heart failure, and diabetes mellitus were obtained from medical records. Lung function was measured by spirometry, performed according to standard guidelines.10
Furthermore, HRQoL was measured by means of the validated Dutch versions of the Clinical COPD Questionnaire (CCQ) and the EuroQol-5D questionnaire (EQ-5D). The CCQ is a disease-specific questionnaire consisting of 10 questions that can be combined in a function, mental, and symptom domain.18,19 It provides an overall score from 0 (very good control) to 6 (extremely poor control). The EQ-5D is a nondisease-specific questionnaire consisting of five domains (mobility, self-care, usual activities, anxiety/depression, and pain/discomfort) and a visual analogue scale.20 It is used to measure HRQoL in chronic diseases. The questions have three response options (no, some, and extreme problems). In both questionnaires, higher scores indicate a worse experience of health status.
The primary outcome, therapy adherence, was recorded from pharmacy records. The patients were not aware that their medication records were going to be used for monitoring their therapy adherence. Theoretical medication use was calculated using information on dispensing date, total supply, and dosage regimen. We computed the total number of days for which patients had collected medication during follow-up and divided this by the total number of days between the first and last collection during follow-up plus the day’s supply of the last refill.21
This was expressed as a percentage and was deemed good if it was between ≥75% and ≤125%, suboptimal between ≥50% and <75%, and poor if <50% (underuse) and >125% (overuse). We excluded medication when it was prescribed only once or when it was used less than 90 days.
Tiotropium was the only long-acting muscarinic agonist used. Furthermore, the ICS beclomethasone, ciclesonide, fluticasone, budesonide, and the combined preparations of fluticasone–salmeterol and budesonide–formoterol were included in the analyses.
Statistical analysis
Baseline characteristics are reported as mean with standard deviation when normally distributed or medians with corresponding interquartile ranges. Nominal variables are reported as numbers with corresponding percentages. To identify a subset of independent continuous variables that are associated with the different types of adherence, analysis of variance tests or Kruskal–Wallis tests were performed as appropriate, with the Tukey HSD and Holm–Bonferroni correction being applied to the significance criterion once pairwise comparisons were made among the study groups. For nominal variables, this association was tested by means of chi-square or Fisher’s exact tests. For both medication types, separate multivariate nominal regression models were made. Variables with a significance P≤0.05 were considered as candidate variables for the multivariate nominal regression analysis and were initially all entered. Subsequently, variables with the highest P-values were eliminated step by step, until the fit of the model decreased significantly (based on the likelihood-ratio test). In case of multicollinearity between variables, the variable that produced the best model fit was included in the model. All statistical calculations were carried out with the SPSS statistical package (version 22.0).
Results
Of the 795 included patients, 635 used ICS and 438 used tiotropium. A total of 385 patients used both ICS and tiotropium.
Inhaled corticosteroids
Smoking status, FEV1 in liters, and the FEV1/vital capacity (VC) ratio were univariately associated with adherence to ICS (Table 1). Current smoking was more often observed in patients with underuse and overuse. Patients with overuse showed the worst lung function, expressed as a low FEV1 in liters, while patients with underuse had the highest FEV1/VC ratio. The number of exacerbations in the year prior to inclusion in this study showed a trend in which underusers were more often infrequent exacerbators. Overall, ≥1 hospital admission in the year prior to inclusion in this study was associated with suboptimal use of medication.
Regarding the CCQ scores, there was a noticeable trend in which patients with optimal adherence scored best on all CCQ questions, indicating a higher quality of life. However, we observed that suboptimal users scored higher on questions 1 (shortness of breath) and 9 (limitations in daily activities) compared to optimal users (Table 2). We also noticed that overusers scored higher on question 3 (being anxious for increased dyspnea) compared to optimal users.
We found no association between adherence to ICS and any of the EQ-5D questions (Table 3).
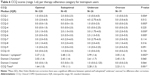
Multinominal regression analysis with ICS
The multivariate nominal regression model (with optimal adherence set as reference category, see Table 4) showed that an increase of 1 L in FEV1 was associated with a two-fold lower risk of overuse (odds ratio [OR] =0.49; 95% confidence interval [CI]: 0.25–0.95) compared to optimal use. An increase in 1% of the FEV1/VC ratio was associated with a 3% higher risk of suboptimal use (OR =1.03; 95% CI: 1.00–1.05) and a 5% higher risk of underuse (OR =1.05; 95% CI: 1.02–1.08) compared to optimal use. Each unit increase on CCQ-question 3 (being anxious for dyspnea) was associated with a 26% higher risk of overuse of ICS (OR =1.26; 95% CI: 1.02–2.91). Finally, patients who were admitted to the hospital 1 year prior to inclusion in this study had a 2.7-fold increased risk of suboptimal use (OR =2.67; 95% CI: 1.48–4.80), compared to optimal use.
Tiotropium
The tiotropium group showed similar baseline characteristics compared to patients in the ICS group, except for a prominent higher percentage of optimal adherence in this group (78%). Table 5 shows that only FEV1/VC ratio was univariately associated with adherence to tiotropium, with underusers having a higher FEV1/VC ratio compared to optimal users.
Regarding the CCQ scores, tiotropium showed the same trend as ICS in which patients with optimal adherence scored better on every question. Nevertheless, suboptimal users had significantly higher scores on question 1 (shortness of breath in rest) (Table 6). In contrast to ICS adherence, underusers instead of overusers scored significantly higher on question 3 (anxiety for increased dyspnea). The symptom domain and total CCQ scores were also associated with underuse of medication, but overuse was also related to higher scores on the symptom domain. Patients with a higher score on the EQ-5D questions concerning mobility and usual activities used tiotropium more often suboptimally and showed more underuse and overuse (Table 7). Anxiety and depression were associated with suboptimal use, underuse, and overuse.
Multinominal regression analysis tiotropium
The multivariate nominal regression model (Table 8) showed that an increase of 1% in FEV1/VC ratio was associated with a 3% higher risk of suboptimal use (OR =1.03; 95% CI: 1.01–1.06) and a 4% higher risk of underuse (OR =1.04; 95% CI: 1.01–1.07) compared to optimal use. Each unit increase in CCQ-question 3 score was associated with almost a 1.5-fold increased risk of overuse of tiotropium (OR =1.46; 95% CI: 1.07–2.00). Patients’ scoring being unable to perform usual activities had a 3.1-fold increased risk of showing suboptimal use (OR =3.09; 95% CI: 0.95–10.06) instead of optimal use.
Discussion
This analysis was designed to determine COPD-related factors that are associated with adherence to inhalation medication. Therapy adherence to both ICS and tiotropium showed to be related to various disease-specific and HRQoL factors.
In our study, 57% of the patients who use ICS and 78% of the patients who use tiotropium showed optimal adherence, which is higher than reported in literature. However, this is in line with a nationwide observational study that showed higher adherence levels in our region compared to other regions in the Netherlands.22 Lately, emphasis has been placed on enhancing therapy adherence because there seems to be an evident reduction in symptoms and future exacerbations.4,5 Whereas Cecere et al23 and Mehuys et al24 found demographic factors predictive for therapy adherence to long-acting beta-agonists, we did not find any demographic factors predictive for adherence to ICS and tiotropium.
Multivariately, the strongest predictors for suboptimal use of ICS were an increase in FEV1/VC ratio and ≥1 hospital admissions in the year prior to inclusion in this study. An important predictor for underuse of ICS was an increase in FEV1/VC ratio. Strong predictors for overuse of ICS were a lower absolute FEV1, a higher score on CCQ-question 3 concerning anxiety for dyspnea, and a current smoking status. These findings suggest that a better lung function predisposes patients to decreased use of their medication, whereas a worse lung function predisposes patients to overuse. However, predictors were measured at baseline, while overuse was determined over the 3-year follow-up period. Overuse could indeed be already present before the follow-up. Infrequent exacerbations were not significantly associated with adherence, but showed a trend toward underuse. This can possibly be explained by the fact that COPD patients who do not experience frequent exacerbations and/or have a better lung function experience less respiratory symptoms and therefore use less inhaled medications.
With regard to tiotropium, multivariately, strong predictors for suboptimal use were a better lung function and the inability to perform usual activities as asked by the EQ-5D whereas a higher FEV1/VC ratio also was a predictor for underuse. The association between therapy adherence and lung function corresponds with our findings in the ICS group. Overuse was again strongly associated with a higher score on CCQ question 3 concerning anxiety for dyspnea.
Our results demonstrate that in a large cohort of patients with COPD, adherence to inhaled medications is in fact class-dependent. This means that adherence to inhaled medications depends on the type of medication.25 However, in our study we only used ICS, merged into one group, and tiotropium. We did not include short-acting beta-2-agonists, such as salbutamol, which are frequently used among patients with COPD because therapy adherence with these medications is not possible to determine, being used as needed. Also, it is important to notice that adherence to one type of medication does not automatically mean adherence to another type of medication.
The relationship between adherence and HRQoL may be ambivalent. A better HRQoL may lead to nonadherence. Contrary, the effect of adherence on HRQoL might be a consequence of the negative effects that it can generate.26 With regard to quality of life and therapy adherence, we noticed that two questions concerning respiratory symptoms (shortness of breath in rest and anxiety for dyspnea) were associated with adherence to ICS and tiotropium. Patients experiencing more shortness of breath in rest were univariately more likely patients with suboptimal adherence to ICS and tiotropium. We cannot fully explain this association and wonder whether it concerns a chicken-and-egg situation. It is also possible that patients with suboptimal use do not optimally benefit from the therapy and therefore experience more shortness of breath in rest. The same explanation can be posed for the total CCQ score regarding tiotropium. It is possible that patients who show underuse experience more shortness of breath in rest, resulting in higher total CCQ scores, indicating a worse quality of life.
While depression and anxiety often coexist, they are separate conditions, but many COPD patients suffer from both.27 A remarkable finding in our study is the significantly increased scores on the question concerning anxiety for dyspnea in overusers of ICS and tiotropium. Several studies have already demonstrated the relation between depression and nonadherence.22 Turan et al28 found in 2014 that the presence of depressive symptoms led to decreased adherence in patients with COPD. However, they did not find a significant association between anxiety and adherence, which is in contrast with our study, nor did they include overuse in measuring adherence, so it is unknown whether the mentioned nonadherence is related to overuse. It is worth mentioning that we specifically looked at anxiety concerning respiratory symptoms, whereas Snaith et al29 looked at anxiety in general according to the Hospital Anxiety and Depression Scale (HADS) questionnaire. Detecting anxiety in COPD is important, since anxiety is a condition that can be effectively treated with pharmacological and nonpharmacological interventions and consequently might reduce overuse.
We observed no association between presence of one of the recorded comorbidities and therapy adherence. This is consistent with a study of Huetsch et al30 that also found these comorbidities to be poor predictors for adherence.31 Khdour et al31 found a relation between presence of comorbidities and adherence, but included more comorbidities than we did in our study and put these comorbidities together as a dichotomous variable.
Our study has several strengths. We defined subgroups of nonadherence, so we could see what type of nonadherence is related to our variables. Just as Krigsman et al32 did, we decided to choose an upper cut-off point as well, in order to study overuse. This subdivision shows that nonadherent patients differ in profile, which helps us to examine patterns of different medication use between patients. Furthermore, our use of pharmacy refill records for estimating adherence could be seen as a strength. This method allowed us to obtain objective data and avoid recall and social desirability biases. Also, this method of monitoring is an accurate measurement of adherence compared to self-report. A downside of this method is that it measures medication acquisition, but not actual medication consumption. It is likely that patients who regularly refill their medications are using them, but this cannot always be verified. In general, adherence is higher in clinical trial settings because patients are motivated to take their medication in correct doses at correct times. Since our patients were not in a clinical trial and since they were not aware that their medication records were going to be used for monitoring their therapy adherence, adherence in our study can be considered very high. Next to this, many adherence studies use data of 1-year follow-up. Since medication use in COPD is long-term, we followed our patients for 3 years, thus giving an estimate on long-term use. Finally, we applied a very comprehensive and complete database of 795 patients complemented with accurate completeness of associated pharmacy data.
Despite these advantages, some limitations of our study should be noted. The information available for our analyses was limited to the variables included in the database. The impact of other variables possibly associated with adherence, such as side effects from therapies, inconvenience in the form of frequent or complex medication dosing regimens, and patient’s beliefs, could not be assessed in this study.
Future studies can put more emphasis on these variables to explore them as predictors for nonadherence, possibly by means of in-depth interviews, where a closer look may be taken why patients do not adhere. Also, interventions that are developed to improve adherence may need to be adapted to incorporate different types of nonadherence in different types of medication.
Conclusion
This study confirms that several quality of life factors and disease-specific factors are related to ICS and tiotropium adherence, but a clear profile of the patient who shows underuse or overuse cannot yet be outlined. A better lung function, expressed as a higher FEV1/VC ratio, was in both groups associated with more suboptimal use and more underuse. Overusers of ICS and tiotropium experience more anxiety symptoms and more physical symptoms. Further research is needed to investigate more variables associated with the different types of nonadherence in different types of medication classes. Also, further research is required into the role of anxiety in adherence to inhalation medication.
Acknowledgment
This study was partly supported by an unrestricted research grant from GlaxoSmithKline.
Disclosure
The authors report no conflicts of interest in this work.
References
Anto JM, Vermeire P, Vestbo J, Sunyer J. Epidemiology of chronic obstructive pulmonary disease. Eur Respir J. 2001;17:982–994. | ||
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of COPD, global initiative for chornic obstructive pulmonary disease (GOLD) 2013. Available from: http://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016/. Accessed May 25, 2016. | ||
Calverley PM, Anderson JA, Celli B et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356:775–789. | ||
Ferguson GT. Recommendations for the management of COPD. Chest. 2000;117:23S–28S. | ||
Tashkin DP, Celli B, Senn S, et al; UPLIFT Study Investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359:1543–1554. | ||
Balkrishnan R, Christensen DB. Inhaled corticosteroid use and associated outcomes in elderly patients with moderate to severe chronic pulmonary disease. Clin Ther. 2000;22:452–469. | ||
Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax. 2008;63:831–838. | ||
Vestbo J, Anderson JA, Calverley PM, et al. Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax. 2009;64:939–943. | ||
Ingebrigtsen TS, Marott JL, Nordestgaard BG, et al. Low use and adherence to maintenance medication in chronic obstructive pulmonary disease in the general population. J Gen Intern Med. 2015;30:51–59. | ||
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. Report Working Party standardization of lung function tests, European Community for steel and coal. Official statement of the European Respiratory Society. Eur Respir J Suppl. 1993;16:5–40. | ||
Restrepo RD, Alvarez MT, Wittnebel LD et al. Medication adherence issues in patients treated for COPD. Int J Chron Obstruct Pulmon Dis. 2008;3:371–384. | ||
van der Lende R, Jansen-Koster EJ, Knijpstra S, Meinesz AF, Wever AM, Orie NG. [Prevalence of cold in Vlagtwedde and Vlaardingen (computer diagnosis versus doctors’ diagnosis)]. Ned Tijdschr Geneeskd. 1975;119:1988–1996. Dutch. | ||
van Grunsven PM, van Schayck CP, van DM, van Herwaarden CL, Akkermans RP, van WC. Compliance during long-term treatment with fluticasone propionate in subjects with early signs of asthma or chronic obstructive pulmonary disease (COPD): results of the Detection, Intervention, and Monitoring Program of COPD and Asthma (DIMCA) Study. J Asthma. 2000;37:225–234. | ||
Baiardini I, Braido F, Bonini M, Compalati E, Canonica GW. Why do doctors and patients not follow guidelines? Curr Opin Allergy Clin Immunol. 2009;9:228–233. | ||
George J, Kong DC, Thoman R, Stewart K. Factors associated with medication nonadherence in patients with COPD. Chest. 2005;128:3198–3204. | ||
Lareau SC, Yawn BP. Improving adherence with inhaler therapy in COPD. Int J Chron Obstruct Pulmon Dis. 2010;5:401–406. | ||
Tashkin DP. Multiple dose regimens. Impact on compliance. Chest. 1995;107:176S–182S. | ||
Stallberg B, Nokela M, Ehrs PO, Hjemdal P, Jonsson EW. Validation of the clinical COPD Questionnaire (CCQ) in primary care. Health Qual Life Outcomes. 2009;7:26. | ||
van der MT, Willemse BW, Schokker S, ten Hacken NH, Postma DS, Juniper EF. Development, validity and responsiveness of the Clinical COPD Questionnaire. Health Qual Life Outcomes. 2003;1:13. | ||
EuroQol Group. EuroQol – a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. | ||
Sikka R, Xia F, Aubert RE. Estimating medication persistency using administrative claims data. Am J Manag Care. 2005;11:449–457. | ||
DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. | ||
Cecere LM, Slatore CG, Uman JE, et al. Adherence to long-acting inhaled therapies among patients with chronic obstructive pulmonary disease (COPD). COPD. 2012;9:251–258. | ||
Mehuys E, Boussery K, Adriaens E, et al. COPD management in primary care: an observational, community pharmacy-based study. Ann Pharmacother. 2010;44:257–266. | ||
Huurne KK, Movig K, van der Valk P, van der Palen J, Brusse-Keizer M. Differences in Adherence to Common Inhaled Medications in COPD. COPD. 2015;12(6):643–648. | ||
Agh T, Domotor P, Bartfai Z, Inotai A, Fujsz E, Meszaros A. Relationship between medication adherence and health-related quality of life in subjects with COPD: A systematic review. Respir Care. 2015;60:297–303. | ||
Panagioti M, Scott C, Blakemore A, Coventry PA. Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;9:1289–1306. | ||
Turan O, Yemez B, Itil O. The effects of anxiety and depression symptoms on treatment adherence in COPD patients. Prim Health Care Res Dev. 2014;15:244–251. | ||
Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003;1:29. | ||
Huetsch JC, Uman JE, Udris EM, Au DH. Predictors of adherence to inhaled medications among Veterans with COPD. J Gen Intern Med. 2012;27:1506–1512. | ||
Khdour MR, Hawwa AF, Kidney JC, Smyth BM, McElnay JC. Potential risk factors for medication non-adherence in patients with chronic obstructive pulmonary disease (COPD). Eur J Clin Pharmacol. 2012;68:1365–1373. | ||
Krigsman K, Moen J, Nilsson JL, Ring L. Refill adherence by the elderly for asthma/chronic obstructive pulmonary disease drugs dispensed over a 10-year period. J Clin Pharm Ther. 2007;32:603–611. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.