Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
Psychosocial Problems of Rural Indian Women Practising Breast Self-Examination – a Community-Based Study from Southern India
Authors Balaiah Mehanathan P, Arthur Edwards Dennison A, Vikramathithan Panchapooranam A, Kandasamy S, Subbiah P, Velappan L, Kalyanaraman S
Received 8 September 2022
Accepted for publication 14 December 2022
Published 17 April 2023 Volume 2023:15 Pages 263—270
DOI https://doi.org/10.2147/BCTT.S386421
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Pranela Rameshwar
Pabithadevi Balaiah Mehanathan,1 Alex Arthur Edwards Dennison,1 Amudha Vikramathithan Panchapooranam,2 Sunitha Kandasamy,3 Padmavathi Subbiah,4 Lakshmikandhan Velappan,4 Shantaraman Kalyanaraman5
1General Surgery, Tirunelveli Medical College, Tirunelveli, Tamil Nadu, India; 2Microbiology, Tirunelveli Medical College, Tirunelveli, Tamil Nadu, India; 3Community Medicine, Thoothukudi Medical College, Tuticorin, Tamil Nadu, India; 4MRHRU, Tirunelveli, Tamil Nadu, India; 5Pathology, Tirunelveli Medical College, Tirunelveli, Tamil Nadu, India
Correspondence: Shantaraman Kalyanaraman, Tirunelveli Medical College, 63, Ittamozhi Road, Tisaiyanvilai, Tirunelveli, 627657, India, Tel +91 9443133898, Email [email protected]
Introduction: Globally, breast cancer affects 2.5 million people annually. Younger women with advanced-stage cancers had a lower survival rate, but early detection enhanced survival chances by 27 to 47%. Breast self-examination (BSE) has led to early detection and higher rates of benign biopsies. Studies evaluating the psychosocial impact of BSE are few in India which has been attempted in the present study.
Methods: The community-based descriptive cross-sectional study was conducted among rural women aged 30 years and above, who have done BSE at least once without present or prior breast abnormalities in the field practice area of Model Rural Health Research Unit, Tirunelveli. The research questionnaire was developed based on the findings of focus group discussion (FGD) on the same objective in the study area.
Results: Among 379 participants, 146 (38.5%) felt confident in their BSE knowledge, 28.2% (n=107) and 5.5% (n=21) of the respondents experienced anxiety and depression while practising BSE, respectively. There is a significant difference between the mean anxiety levels (p-value=0.002) and depression (p-value=0.013) of individuals who have detected anomalies during BSE and those who have not.
Conclusion: Regular counselling has to improve knowledge about BSE, like the timing and method of examination, and decreases the anxiety and depression level.
Keywords: breast cancer, self-examination, screening, Hamilton scales, rural women
Introduction
Breast cancer is a global problem accounting for 2.5 million cases per year worldwide. Breast cancer has ranked number one cancer among Indian females with an age adjusted rate as high as 25.8 per 100,000 women and mortality of 12.7 per 100,000 women.1 The younger women have a reported lower survival rate with cancers being detected at an advanced stage, while earlier detection improves survival rates by 27% to 47%.2 Early detection is being performed using breast self-examination (BSE), clinical breast examination (CBE) and mammography, of which BSE is an easily available option for women in rural areas of India as a part of the National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) of the National Health Mission, Ministry of Health and Family Welfare, Govt of India. This method involves the woman herself looking at and feeling each breast for possible lumps, change in consistency, distortions or swelling.
Breast self-examination has resulted in the early detection of breast cancers. On the contrary, studies have reported that breast self-examination does not cause remarkable changes in mortality or stage of breast cancer, but results in higher rates of benign breast biopsies.2 It has also been reported that learning to do breast self-examination can result in depression, anxiety,3 fear, fatalism and higher levels of psychological distress, especially cancer-specific intrusive thoughts that can result in excessive and repeated examination.4,5 The WHO says that National Cancer Control programmes should not recommend mass screening by breast self-examination and physical examinations of the breast. Rather, programmes should encourage breast awareness and early diagnosis of breast cancer, especially for women aged 40–69 years attending primary health care centres or hospitals for other reasons, by offering them clinical breast examinations. According to the studies, the WHO and Canadian task force is not promoting BSE as a screening tool for early detection as BSE practice led to increased number of benign breast biopsies and the economic costs.2,8 The procedure has been supported by health education messages in which some women perceived the messages constructively and have performed the examination which has resulted in early detection, whereas in some others these messages were perceived as threatening to result in increased anxiety and avoidance.6,7
Most of such studies that evaluated the impact of breast self-examination and its psychological impact were from United States, Canada or Europe,2,8 while similar studies which assessed Indian populations were sparse. This study was implemented to make a community level assessment of the psychosocial problems of breast self-examination and barriers that could affect the objectives of the National Program.
Materials and Methods
The Institutional Ethics Committee at the Tirunelveli Medical College approved this community-based descriptive cross-sectional study in the field practice area of Model Rural Health Research Unit (MRHRU), Kalloor, Tirunelveli, between 2019 to 2020 and the study complies with the Declaration of Helsinki. The MRHRU field practice area comprising 14 clusters caters to the population of 36,663. The number of women in the reproductive age of 30 years and above is 11,818. We assume the prevalence as 50% and the calculated sample size was 373 with 95% confidence interval and with a design effect of 1. An initial survey was carried out to approach all women aged 30 years and above in the village to know whether they are aware of and practising BSE with their oral consent. The prevalence of the BSE in this area was 37% as reported from the routine field activities of the MRHRU (study setting). By using purposive sampling technique, the participants were included as per inclusion and exclusion criteria till the sample size was achieved. To explore the psychosocial impact of BSE on women and to assist the development of the study questionnaire, focus group discussion (FGD) was conducted. The principal investigator who was trained in qualitative research methodology conducted three FGDs till the point of saturation among those purposively selected women aged 30 years and above who have done BSE at least once. The FGD was audio recorded with the permission of the participant. The recording was transcribed, translated, back-translated and manual content analysis was done. Based on the findings of the qualitative analysis, a structured study questionnaire was prepared, pilot tested and validated. The questionnaire consists of socio-demographic variables, family history of breast cancer, knowledge and practice of BSE and Hamilton anxiety and depression scales. During focused group discussion, the participants mentioned about anxiety and depression while doing BSE. Hamilton anxiety and depression scales are most commonly used validated scales worldwide to assess the anxiety and depression levels. Those consented women aged 30 years and above irrespective of marital status who had done BSE at least once without any present or previous breast abnormalities have administered the study questionnaire after obtaining informed written consent. Privacy and confidentiality were assured as the data were collected by trained female field staff at the participant’s house, the place of convenience for the women. The data were randomly verified by the field coordinator, entered in a Microsoft Excel spreadsheet and analysed using the statistical software SPSS version 16.0. The descriptive statistics were summarized as mean, standard deviation and proportions. To establish the relationship between the psychosocial factors and the knowledge and practice of BSE, the chi-square test and Fisher’s exact test have been applied. The Kruskal–Wallis test was done to test the significance of scores of anxiety and depression among the women who did breast self-examination and the identification of breast abnormalities was calculated.
Results
Demographic Details and Breast Self-Examination
This community-based study documented the psychosocial problems of BSE of the 379 rural women. The mean age of the study participants was 38.20±5.17 (SD) years. Most of the participants who have practised BSE belong to the age group of 30 to 40 years. 62.7% (n=238) of the women who did BSE were homemakers. 57.2% (n=217) of women who did BSE have completed either primary or secondary school of education (Table 1).
 |
Table 1 Distribution of Socio-Demographic Details of the Participants (n=379) |
Knowledge and Practice of Breast Self-Examination
Out of 379 participants, 93.9% (n=356) knew about how to perform BSE and only 38.5% (n=146) of the participants were confident about their knowledge about BSE. Health care workers were the source of knowledge for 79.2% (n=300) of the participants. 33% (n=125) of the participants have known to do BSE after menses whereas 34% (n=129) have not responded to this question. 44.9% (n=170) of the women have responded that it was advisable to do BSE occasionally and 57% (n=216) have done BSE occasionally. Only 27.7% (n=105) of the women have done breast self-examination, once a month. Only 4.7% (n=18) of the women who did breast self-examination have detected some abnormality in the breast (Table 2).
 |
Table 2 Knowledge and Practice of Breast Self-Examination (n=379) |
Anxiety and Depression Score After BSE
Table 3 depicts that 28.2% (n=107) and 5.5% (n=21) of the participants had anxiety and depression while practising BSE. The association of educational and occupational status of the women with their anxiety and depression levels were statistically not significant (Table 4). There is no significant correlation between the factors such as age, number of children and their corresponding anxiety, depression score (age vs anxiety: correlation coefficient=0.036; p-value=0.713, age vs depression: correlation coefficient=−0.219; p-value=0.340, number of children vs anxiety: correlation coefficient=−0.068; p-value=0.487, number of children vs depression: correlation coefficient=0.116; p-value=0.616). 7.1% of women who did BSE repeatedly had increased anxiety level.
 |
Table 3 Distribution of the Level of Anxiety and Depression Among the Study Participants (n=379) |
 |
Table 4 Association Between Selected Variables and Anxiety and Depression |
There is significant difference between the mean anxiety scores of those who have found abnormalities while performing BSE and those who have not (p-value=0.002). There is significant difference between the mean depression scores of those who have found abnormalities while performing BSE and those who have not (p-value=0.013) (Table 5). There is no significant relationship between the frequency of BSE practice with the score of anxiety and depression (Table 6 and Table 7).
 |
Table 5 Mean Scores of Anxiety and Depression and Those Who Have Found Abnormalities While Performing BSE and Those Who Have Not |
 |
Table 6 Frequency of BSE Practice |
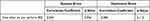 |
Table 7 Association of Frequency of BSE Practice and Anxiety and Depression Level |
Discussion
Breast self-examination, clinical breast examination and mammography are the common screening tools used to detect early breast cancer. Mammography is expensive and available in the cities only. So, BSE is the only readily available option to women living in rural areas9 and is largely promoted as a screening tool for the early detection of breast cancer. Screening or regular check-up for breast cancer is important for early detection and confirmation of diagnosis. As per the Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) in India, women who are 30 years of age and above should be screened by a trained health care provider at least once in five years. The health workers educate and motivate the women in her area about the steps in BSE. Women are also educated about the warning signs/symptoms of breast cancer and if they experience any of these, they are advised to visit the health facility. Screening of breast cancer with CBE is conducted at the village level or at the sub-centre level by any trained health worker – preferably lady physician, staff nurse or an auxiliary nurse and midwife. If there is any abnormal finding in CBE, the woman should be referred to a medical officer or surgeon at Community Health Centre/District Hospital/Government Hospital for further evaluation and management. The prevalence of the practice of BSE is still low in India.10–13 A study conducted in a rural hospital of South India reported the majority 354 (85.1%) of the women in the study had never heard of BSE. None had performed monthly BSE. Only 40 (9.6%) of the women actually performed BSE within the last 6 months.11 A study conducted in a teaching hospital in central India also stated that none of the study participants had knowledge about BSE or had previously done BSE.12 A systematic review of awareness among Indian women in community stated that knowledge of BSE varied from very poor (2%) to good (69.8%) in the community setting and the practice was similarly negligible (0%) to moderate (34.9%).13 The prevalence of BSE practice in our study area was found to be 37%. Level of education, socioeconomic factors and knowledge about BSE and availability of time are independent predictors in the performance of BSE. The women who practise BSE in our study mostly belong to the age group of 30 to 40 years. The cancer breast occurs in this age group is an early onset cancer breast and the early detection will improve the survival status of the individual.14,15 But, there are mixed findings on the influence of age on breast cancer screening practices. While Tafavian et al found a lack of association between age and BSE,16 Akhigbe and Omuemu and Park et al reported an association between increasing age and BSE, and found participants who practice BSE or those who undergo mammogram screening are typically 50 years and older.17,18 79.2% of them got their knowledge of breast self-examination from the health worker. The promotion of BSE by the health care worker has reached the community to a larger extent. But, only 38.5% of the participants were confident of their knowledge about BSE like the timing of examination and method of examination, which has to be improved by repeated counselling and demonstration. Confidence in the practice of BSE will improve the chances of doing BSE regularly.
Unemployed women are more in our study population, contributing 60.8%. This shows that women who are working are preoccupied with work at both workplaces and at the house. Women who are unemployed are more in the study suggesting that they have enough time to converse within the neighbourhood and gain knowledge on BSE and utilise their time to take care of their health and hence practise BSE. A community-based, cross-sectional study conducted among 200 rural women at the same state region of the study setting has reported that the mean age of the study group was 36.9±8.8 years. 50% of the women belonged to class IV socioeconomic class. Most of the women 178 (89%) were aware of breast cancer. Only 26% of the women were aware of BSE. Although BSE was practised by 18% women, only 5% of the total participants practised it regularly every month. Another study from South India also reported that positive family history was the important factor which sustained the practice of BSE. Women with higher level of education had better knowledge regarding breast cancer and BSE.10 The practice of BSE was significantly associated with higher education, being a housewife, higher socioeconomic status and a history of a breast lump in self or family.11,19
45.8% of women are doing BSE occasionally and have shown their self-concern towards early detection of breast cancer but improvement in the knowledge of BSE practices will help them to perform BSE often as recommended. When the intensity of the awareness programmes is increased, this 45.8% could be easily made to do BSE 6 times a year which is ideal as per the NCD programme. On the other hand, 7.1% of women who are doing BSE more than once a month had increased anxiety score comparatively, and they need counselling to alleviate the fear and anxiety of detecting any abnormality in the breast.
25.9% of women who practised BSE at least once developed mild anxiety, 1.6% developed mild to moderate anxiety and only 0.5% developed moderate to severe anxiety in our study which is in contrast to the Russian trial, Shanghai trial and UK trial. All of these studies proved that there is increased anxiety after doing BSE which resulted in an increased number of benign breast biopsies,7,8 which is not true in our study.
The mean depression score was 27.00±8.29 and the mean anxiety score was 12.33±8.72 among those who have detected an abnormality in the breast, in comparison to those who have not detected (depression score=13.50±8.35; p-value=0.013 and anxiety score=5.26±7.32; p-value=0.002) any abnormality in the breast while doing BSE. A healthy discussion about breast lumps and breast problems is needed to alleviate this anxiety. They must be told of the fact that all lumps are not cancers and early diagnosis of cancer has a good prognosis. Fear of developing cancer, fear of life, the emotional and financial burden of developing cancer and the lack of proper knowledge may be the reasons for the anxiety level in these women. The study was conducted in a rural population. Hence, it may not be applied to urban areas and a modernized city population.
Conclusion
In our set-up, breast self-examination can still be used as best screening tool for the early detection of breast cancer as only 1.6–0.5% of women who practice breast self-examination develop moderate to severe anxiety while doing BSE. Breast self-examination as an effective screening tool for early detection of cancer, more awareness programmes and counselling are needed regularly to alleviate this anxiety. Even though the knowledge of BSE is gained mostly from the health care worker, more campaigns and demonstrations of BSE at primary health centre level and community level are needed to improve the prevalence of BSE practice. More emphasis on BSE should be given during their clinical and NCD clinic visit.
Abbreviations
BSE, Breast Self-Examination; CBE, Clinical Breast Examination; FGD, Focus Group Discussion; MRHRU, Model Rural Health Research Unit; NPCDCS, National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke; SD, Standard Deviation.
Acknowledgments
I thank my postgraduates Dr Athisayamani and Dr Subhash Mehta who helped me in data collection. I thank the NIE scientist Dr Yuvaraj who helped me to conduct the study. I express my sincere gratitude to Dr P. Manickam, Scientist E, Mr T. Daniel Rajasekar, Senior Technical Officer, Mrs Gayathri K, Technician II, and Mr Balusamy M, Technician II for their valuable comments and support. I also thank Dr Muthu, Scientist C and Mrs Maryam Jamila. S Project Assistant-Statistics of MRHRU for this support.
Disclosure
The authors declare that there is no conflicts of interest in this work.
References
1. Malvia S, Bagadi SA, Dubey US, Saxena S. Epidemiology of breast cancer in Indian women. Asia Pac J Clin Oncol. 2017;13(4):289–295. doi:10.1111/ajco.12661
2. Houssami N, Ciatto S, Martinelli F, Bonardi R, Duffy SW. Early detection of second breast cancers improves prognosis in breast cancer survivors. Ann Oncol. 2009;20(9):1505–1510. doi:10.1093/annonc/mdp037
3. Baxter N; Canadian Task Force on Preventive Health Care. Preventive health care, 2001 update: should women be routinely taught breast self-examination to screen for breast cancer? CMAJ. 2001;164(13):1837–1846.
4. Erblich J, Bovbjerg DH, Valdimarsdottir HB. Psychological distress, health beliefs, and frequency of breast self-examination. J Behav Med. 2000;23(3):277–292. doi:10.1023/A:1005510109233
5. Ghahramanian A, Rahmani A, Aghazadeh AM, Mehr LE. Relationships of fear of breast cancer and fatalism with screening behavior in women referred to health centers of Tabriz in Iran. Asian Pac J Cancer Prev. 2016;17(9):4427–4432.
6. Block LG, Williams P. Undoing the effects of seizing and freezing: decreasing defensive processing of personally relevant messages. J Appl Soc Psychol. 2002;32(4):803–830. doi:10.1111/j.1559-1816.2002.tb00243.x
7. Millar MG, Millar K. Negative affective consequences of thinking about disease detection behaviors. Health Psychol. 1995;14(2):141–146. doi:10.1037/0278-6133.14.2.141
8. Nelson HD, Tyne K, Naik A, et al. Screening for breast cancer: an update for the U.S. preventive services task force. Ann Intern Med. 2009;151(10):727–W242. doi:10.7326/0003-4819-151-10-200911170-00009
9. Olaogun JG, Emmanuel EE, Dada SA, Odesanmi OM, Adesua OA. The prevalence of practicing breast self-examination and knowledge of breast cancer disease among women attending secondary health facility. Int Surg J. 2017;4(10):3211–3217. doi:10.18203/2349-2902.isj20174491
10. Kumarasamy H, Veerakumar AM, Subhathra S, Suga Y, Murugaraj R. Determinants of awareness and practice of breast self-examination among rural women in Trichy, Tamil Nadu. J Midlife Health. 2017;8(2):84–88. doi:10.4103/jmh.JMH_79_16
11. Baburajan C, Pushparani MS, Lawenya M, Lukose L, Johnson AR. Are rural women aware of breast cancer and do they practice breast self-examination? A cross-sectional study in a rural hospital in South India [published online ahead of print, 2021 Jan 27]. Indian J Cancer. 2021. doi:10.4103/ijc.IJC_799_19
12. Siddharth R, Gupta D, Narang R, Singh P. Knowledge, attitude and practice about breast cancer and breast self-examination among women seeking out-patient care in a teaching hospital in central India. Indian J Cancer. 2016;53(2):226–229. doi:10.4103/0019-509X.197710
13. Gupta R, Gupta S, Mehrotra R, Sodhani P. Risk factors of breast cancer and breast self-examination in early detection: systematic review of awareness among Indian women in community and health care professionals. J Public Health. 2020;42(1):118–131. doi:10.1093/pubmed/fdy228
14. Nyström L. How effective is screening for breast cancer? BMJ. 2000;321(7262):647–648. doi:10.1136/bmj.321.7262.647
15. Dündar PE, Ozmen D, Oztürk B, et al. The knowledge and attitudes of breast self-examination and mammography in a group of women in a rural area in western Turkey. BMC Cancer. 2006;6(1):43. doi:10.1186/1471-2407-6-43
16. Tavafian SS, Hasani L, Aghamolaei T, Zare S, Gregory D. Prediction of breast self-examination in a sample of Iranian women: an application of the health belief model. BMC Womens Health. 2009;9(1):37. doi:10.1186/1472-6874-9-37
17. Akhigbe AO, Omuemu VO. Knowledge, attitudes and practice of breast cancer screening among female health workers in a Nigerian urban city. BMC Cancer. 2009;9(1):203. doi:10.1186/1471-2407-9-203
18. Park MJ, Park EC, Choi KS, Jun JK, Lee HY. Sociodemographic gradients in breast and cervical cancer screening in Korea: the Korean National Cancer Screening Survey (KNCSS) 2005–2009. BMC Cancer. 2011;11:257. doi:10.1186/1471-2407-11-257
19. Sachdeva S, Mangalesh S, Dudani S. Knowledge, attitude and practices of breast self-examination amongst Indian women: a pan-India study. Asian Pac J Cancer Care. 2021;6(2):141–147. doi:10.31557/apjcc.2021.6.2.141-147
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
