Back to Journals » Psychology Research and Behavior Management » Volume 14
Psychometric Properties of the Multidimensional Scale of Perceived Social Support (MSPSS) Among Family Caregivers of People with Schizophrenia in China
Authors Wang D, Zhu F, Xi S, Niu L, Tebes JK, Xiao S , Yu Y
Received 18 May 2021
Accepted for publication 8 July 2021
Published 7 August 2021 Volume 2021:14 Pages 1201—1209
DOI https://doi.org/10.2147/PRBM.S320126
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Dan Wang,1 Feng Zhu,1 Shijun Xi,1 Lu Niu,1 Jacob Kraemer Tebes,2 Shuiyuan Xiao,1 Yu Yu1,2
1Department of Social Medicine and Health Management, Xiangya School of Public Health, Central South University, Changsha, Hunan, People’s Republic of China; 2Division of Prevention and Community Research, Department of Psychiatry, Yale School of Medicine, New Haven, CT, USA
Correspondence: Yu Yu
Department of Social Medicine and Health Management, Xiangya School of Public Health, Central South University, Upper Mayuanlin Road 238, Changsha, Hunan, 410008, People’s Republic of China
Tel +86-731-84805459
; +86 1 203-745-9531
Email [email protected]; [email protected]
Introduction: The Multidimensional Scale of Perceived Social Support (MSPSS) is one of the most widely used scales for social support. Although previous studies have shown good reliability and concurrent validity, conflicting evidence exists on its factor structures.
Aim: To validate the MSPSS among caregivers of people with schizophrenia in China and assess its factor structure.
Methods: A cross-sectional study was conducted of 449 family caregivers in 12 communities for psychometric testing, eg, internal consistency reliability, test–retest reliability, construct validity, exploratory factor analysis (EFA) and confirmatory factor analysis (CFA).
Results: The MSPSS showed good internal consistency with a Cronbach’s alpha of 0.95, good test–retest reliability with intraclass correlation coefficient (ICC) of 0.91, and kappa ranging from 0.62 to 0.71. Concurrent validity was supported by its negative correlations with perceived stress, and significant positive correlations with caregiving rewarding feelings, family functioning, and coping. EFA yielded a two-factor structure (family vs non-family), while CFA generally supported a three-factor structure (family, friends, and significant others).
Conclusion: Our findings show good psychometric properties of the MSPSS among caregivers of people with schizophrenia in China. EFA yields two-factor structure and CFA yields three factors consistent with the theory underlying the measure’s development.
Keywords: Multidimensional Scale of Perceived Social Support, reliability, validity, factor analysis, Chinese
Plain Language Summary
What is already known about the topic?
- Social support comes from three different sources: family, friends, and significant others.
- The MSPSS showed good reliability and factorial validity among diverse samples in the original psychometric study.
What this paper adds
- MSPSS shows good psychometric properties among caregivers of people with schizophrenia in China.
- This paper demonstrates that a two-factor structure of MSPSS is family and non-family support.
Introduction
Social support is a useful multidimensional resource to help people with positive strategies when confronting adversity and stress.1 Social support usually comes from various sources such as family, friends and other social relationships. Abundant evidence has shown positive impacts of social support upon self-efficacy, job commitment, marital satisfaction, coping style and family function.2,3 Additionally, social support has buffering effects against fatigue, depression, insomnia, suicidal intention.4,5
Given the relationship of social support to health, a psychometrically sound measurement tool is needed to guide interventions and evaluation. The Multidimensional Scale of Perceived Social Support (MSPSS) is one of the most widely used instruments to assess social support.6 It contains 12 items assessing support from three sources: family, friends and significant others. Since its development by Zimet et al in 1988,7 the MSPSS has been translated into various versions and validated among various populations.8–10 These studies generally reported high reliability of MSPSS, with Cronbach’s alpha≥0.90; as well as good concurrent validity, with significant associations with other health indicators such as coping,11 loneliness12 and stress.13
Although past studies consistently reported good reliability and validity of the MSPSS, conflicting evidence exists on its factor structure. While most studies using confirmatory factor analysis (CFA) generally supported the three-factor structure (family, friends and significant others);14–16 some studies using exploratory factor analysis (EFA) showing different factor structures. For instance, Tonsing et al13 validated the Urdu version of MSPSS among a sample of Pakistani and Nepalese respondents living in Hong Kong and found a two-factor structure. While the original Friends subscale was retained as one factor, the remaining items of the original domains of Family and Significant Others all loaded on to a single factor, suggesting a broader family factor. Similar two-factor structures were also reported with caregivers of patients with cancer in Zimbabwe,17 public secondary school teachers in Peninsular Malaysia18 and adult stroke survivors in Nigeria.19 A single-factor solution for the MSPSS has been found using principal components factor analysis of EFA among a South Asian population.20 This suggests that the factor structure may be both sample- and method-dependent.21
The MSPSS was first translated into Chinese by Huang et al in 1996 and has since been validated with various populations.22–24 However, the psychometric properties of MSPSS have not yet to be tested among caregivers of people living with schizophrenia.
Caring for a family member with schizophrenia imposes a significant burden on family caregivers,25 who have undergone a broad spectrum of problems including physical burnout, economic pressure and psychological distress.26 Numerous studies have demonstrated that caregivers of people with schizophrenia are socially isolated and lack social support,27–29 which further aggravates caregiver burden and psychological distress.30 It is thus important to validate the MSPSS among caregivers of people with schizophrenia in China to better understand and measure their social support and guide for subsequent interventions.
The current study was conducted to test the psychometric properties of MSPSS among caregivers of people with schizophrenia in China. Specifically, we used both EFA and CFA to examine the internal consistency reliability, concurrent validity, and factor structure.
Methods
Participants
The study was conducted in Changsha City which lies in the central southern part of China. As the capital of Hunan Province, Changsha city is also the most populous city in Hunan with a population constituting of 11.82% of Hunan Province. Changsha City is one of the most developed and prosperous major cities in China with fast growing in its commercial, manufacturing, transportation, education and innovation. Data was obtained from the baseline assessment for a large community intervention program to implement a WeChat-based integrative family intervention (WIFI) for people living with schizophrenia and their families.31 Family caregivers were recruited from 12 community health centers in Changsha city in Hunan Province through the “686 Program” – a community-based program to support the management and treatment of individuals with major mental disorders that is financed by the central government. The program provides free anti-psychotic medication for registered clients with a serious mental illness.32 The inclusion criteria for family caregivers are as follows: 1) caring for a family member registered in the “686 program” who meets criteria in the Chinese classification of Mental Disorders (CCMD-3) or the international classification of Schizophrenia (ICD-10) criteria for schizophrenia; 2) living with the care recipient for at least the last two years; 3) aged ≥18 years; and 4) able to read and communicate. Caregivers with obvious physical or mental illness and thus unable to communicate were excluded from the study sample. The sample size of 449 satisfies the factor analytic requirement of at least 10 respondents per item.33
Procedure and Ethical Considerations
This cross-sectional study was conducted among family caregivers of people with schizophrenia in China from May 2019 to September 2019. Family caregivers were invited to participate in the study by a member of the research team during the monthly free medication clinic at their family member’s community health center. The research team member explained the study purpose, procedures, potential risks and benefit of participation, prior to obtaining written informed consent. Upon receipt of written consent, each family caregiver participated in a face-to-face interview and also completed a survey questionnaire. Participants received the standard payment for research participation: 20 yuan (equivalent to $2.8) in cash. After 2 weeks, a random sample of 25 participants were retested using the same surveys to assess re-test reliability. The study was reviewed and approved by the Ethics Committee of the Xiangya School of Public Health, Central South University (No.: XYGW-2019-029).
Measures
Multidimensional Scale of Perceived Social Support (MSPSS)
MSPSS is a 12-item scale originally designed to assess social support from three different sources: family, friends, and significant others (ie, romantic, subordinate or other particularly close relationship).34 Each subscale has four items and the total score ranges from 12 to 84, with higher scores indicating more social support. Respondents are asked to choose whether they agree with each statement on a 7-point Likert scale from 1 = “strongly disagree” to 7 = “strongly agree”.35 In the current study, the MSPSS showed good internal consistency, with a Cronbach’s alpha of 0.95.
Perceived Stress Scale (PSS)
PSS is a 10-item scale used to assess the degree of perceived stress within the past month.36 It includes two domains: perceived distress (6 positive items) and perceived coping (4 negative items, reversely scored). Each item is rated on a 5-point Likert scale ranging from 0 (never) to 4 (very often). The total score ranges from 0 to 40, with higher scores indicative of greater perceived stress. In the current study, the PSS showed good internal consistency, with a Cronbach’s alpha of 0.79.
Adaptation, Partnership, Growth, Affection and Resolve (APGAR)
APGAR is a 5-item scale to assess perceived family functioning.37 Each item is scored on a 3-point Likert scale from 0 (hardly ever) to 2 (almost always). The total score ranges from 0 to 10 with higher scores indicating higher satisfaction with family functioning. In the current study, the APGAR showed good internal consistency, with a Cronbach’s alpha of 0.95.
Simple Coping Style Questionnaire (SCSQ)
SCSQ38 was first adapted from Folkman and Lazarus’s most widely used Coping Style Questionnaire (CSQ) to facilitate its application in a Chinese context.39 The 20-item scale covers two domains: active coping (12 items) and passive coping (8 items). Each item is scored on a 4-point Likert scale–from 0 (never) to 3 (always). The total score is calculated separately for positive and negative coping to assess coping tendencies and frequencies. In the current study, the SCSQ showed good internal consistency, with a Cronbach’s alpha of 0.88.
Caregiving Rewarding Feelings (CRF)
Positive feelings about caregiving were assessed using the Caregiving Rewarding Feelings (CRF) scale.40 It consists of 12 items asking about a range of possible rewarding feelings during caregiving, such as “a better person” and “have a stronger sense of responsibility”. Each item is rated on a 5-point Likert scale from 1 (“totally disagree”) to 5 (“strongly agree”) with higher total score indicating more positive feelings. In the current study, the CRF showed good reliability with a Cronbach’s alpha of 0.96.
Statistical Analyses
Data were analyzed using IBM SPSS Statistics 23.0 and Amos 22.0 software. Internal consistency reliability was assessed by the Cronbach’s alpha coefficient, with a recommended level of 0.70 or above indicating good internal consistency.41 Test–retest reliability was measured by the intraclass correlation coefficient (ICC) for the total score and kappa for each item, with a recommended level of ICC ≥0.70 and kappa ≥0.60, indicating good test–retest reliability.42 Pearson correlation or Spearman’s rank correlations was used to test the concurrent validity of the MSPSS depending on data normality distribution, with expected significant positive correlations with family functioning (measured by APGAR), positive coping style (measured by SCSQ) and positive feelings about caregiving (measured by CRF), as well as an expected negative correlation with perceived stress (measured by PSS).
Factor structure was tested first by EFA and then by CFA. EFA was employed to determine whether the MSPSS has a different factor structure than the a priori three-factor structure, while CFA was used to compare the new factor structure for the EFA (if any) and the a priori three-factor structure. Bartlett’s test of sphericity43 (measuring of sampling accuracy) and the Kaiser-Meyer-Olkin (KMO) test44 (measuring sampling adequacy) were used to examine the appropriateness of the factor analysis. The following model fit indices were used as criteria for CFA: root mean square error of approximation (RMSEA; desired value <0.06), comparative fit index (CFI; desired value ≥0.90), normed fit index (NFI; desired value >0.95),45 goodness-of-fit index (GFI; desired value ≥0.90), incremental fit index (IFI; desired value ≥0.90),46 Tucker–Lewis index (TLI; desired value ≥0.90) and parsimony goodness-of-fit index (PGFI; desired value >0.50)47. P value <0.01 (two-tailed) was considered as statistically significant.
Results
Sample Characteristics
A total of 449 family caregivers completed the survey. The sample size satisfies the factor analytic requirement of at least 10 respondents per item.33 Characteristics of participants are summarized in Table 1. Participants were 60.09 (SD:12.28) years old on average. Most were married or cohabiting (75.72%) and unemployed (85.52%). Over half were female (54.12%), parent caregivers (56.57%), and with some physical illnesses (59.24%). The total MSPSS score was moderately low with an average score of 50.35±18.95.
 |
Table 1 Characteristics of the Sample (N = 449) |
Internal Consistency Reliability
As shown in Table 2, Cronbach’s α coefficient was 0.95 for the total scale of MSPSS, 0.92 for the family subscale, 0.93 for the friend subscale, and 0.89 for the significant others subscale. ICC was 0.91 for the total scale of MSPSS, 0.85 for the family subscale, 0.93 for the friend subscale, and 0.80 for the significant others subscale. All these results indicate good internal consistency reliability.
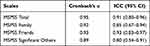 |
Table 2 Internal Consistency of the MSPSS and Its Three Subscales |
Test–Retest Reliability
The ICC for the total score was 0.91 (P < 0.001), exceeding the recommended standard of 0.70. Kappa for each item ranged from 0.62 for item 7 and 8 to 0.71 for item 9, exceeding the recommended standard of 0.60. All these results indicate good test–retest reliability.
Concurrent Validity
Spearman’s rank correlations were used for concurrent validity testing after normality testing showed non-normal distribution of MSPSS. Table 3 displays the correlations between MSPSS and PSS, CRF, APGAR, SCSQ. The total scale of the MSPSS was significantly negatively associated with the PSS (r =−0.221, P<0.01); and significantly positively associated with CRF (r = 0.535, P < 0.01), APGAR (r = 0.558, P < 0.01), and SCSQ (r =0.347, P < 0.01).
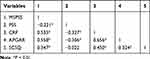 |
Table 3 Correlations of MSPSS and Its Three Subscales with Other Variables (N=435) |
Exploratory Factor Analysis
The Kaiser–Meyer–Olkin (KMO) measure for the 12 items was 0.924, which is considered acceptable The Bartlett’s test of sphericity had a significant level of p < 0.001, indicating a strong association among the variables. Therefore, the data were appropriate to proceed for EFA.
Although most earlier studies confirmed an a priori three-factor structure of the MSPSS, the EFA in this sample yielded only a two-factor solution. As shown in Table 4, factor 1 (eigenvalues = 7.71) accounted for 64.27% of the variance and included all items from the original subscales of significant others and friends. Factor 2 (eigenvalues = 1.17) accounted for 9.75% of the variance and included all items from the original family subscale. The combination of two factors accounted for 74.03% of the total variance.
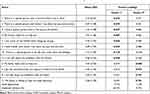 |
Table 4 Descriptive Statistics and Factor Loadings of the MSPSS (N=435)† |
Confirmatory Factor Analysis
A CFA was conducted to test the a priori three-factor structure for the MSPSS and then compared with the new two-factor structure just obtained using the EFA. Table 5 shows a comparison of the model fit indices for between the two- and three-factor analyses. As is evident, the CFA generally supported the a priori three-factor structure, with all model fit indexes meeting the criteria except for the RMSEA (=0.10, exceeding the required criteria of <0.06). Also, the CFA did not support the new two-factor structure, with RMSEA, GFI, TLI, NFI not meeting the necessary criteria. Thus, the CFA showed better model fit for the a priori three-factor structure of the MSPSS than the two-factor structure obtained using EFA.
 |
Table 5 Summary of Model Fit Statistics from Confirmatory Factor Analysis for the MSPSS Factorial Structure¶ |
Discussion
This study provides evidence of the reliability and validity of the Chinese version of the MSPSS among family caregivers of people with schizophrenia in China. Overall, the MSPSS shows good internal consistency and test–retest reliability. Concurrent validity was also supported by significant negative correlations with perceived stress, and significant positive correlations with caregiving rewarding feelings, family functioning, and coping. The EFA yielded a two-factor structure, but the CFA generally supported the a priori three-factor structure of the original scale.
Cronbach’s alpha coefficients for the total scale and its three subscales exceeded 0.89, indicating high internal consistency of the MSPSS. This finding is consistent with previous studies showing high Cronbach’s alpha coefficients.11,12,48 For instance, Wittenborn’s study among individuals in prison in the US reported a Cronbach’s alpha coefficient of 0.93 for the total MSPSS, and Zhou’s study among a Chinese population with methadone maintenance treatment reported a Cronbach’s alpha coefficient of 0.92. The ICC of the total score and the weighted kappa for each item were also above the recommended, showing high test–retest reliability. This finding is also consistent with other studies showing similar results.49–51 This finding indicates the stability of the MSPSS in assessing social support over time. However, future research should examine test–retest reliability with a larger sample.
The MSPSS also showed significant negative correlations with PSS, and significant positive correlations with CRF, APGAR, and CSCQ, demonstrating favorable concurrent validity. The results are in keeping with previous studies showing similar results. For instance, social support has been reported to be negatively associated with perceived stress with a correlation coefficient of 0.458 in Lohanan’s study,52 and positively associated with positive coping with a correlation coefficient of 0.21 in Lin, J’s study.53 This finding illustrates that the MSPSS aligns with the key functions of social support in buffering stress, facilitating positive coping, improving family functioning, and instilling positive feelings among caregivers. However, only mild correlation was found for PSS and SCSQ, and moderate correlation for CRF and APGAR with MSPSS, indicating that other factors may mediate such correlations, which warrants further study.
Different factor structures were supported by the use of different methods, with EFA yielding a two-factor structure and CFA a three-factor structure. In the EFA, the original family subscale was retained as one factor, while the original subscales of friends and significant others were combined into a single “non-family subscale.” This finding is consistent with some previous research that has found a “Significant Others” scale and “Friends” scale as one factor.13,48 The specific sample characteristics and socio-cultural factors of the study sample may have accounted for these effects. Most caregivers in this study were married and unemployed, thus likely engaged mostly in-home care with fewer social contacts outside of the home. In addition, because of the significant time and energy required to care for their family members with schizophrenia, caregivers may have had little time to obtain social support from individuals outside of their family, such as friends, neighbors, and co-workers (since most were unemployed). For these in-home family caregivers, social support sources may be more limited and can be thus more readily classified as family and non-family.
Another factor that could have accounted for these results may have been cultural. The Chinese culture is dominated by Confucian values that attach great importance to familism.54 Family constitutes the basic unit in the Chinese social structure and plays an essential role in every family member’s life. All social contacts outside the family are likely to be seen in a similar light as “not in the family.”
In contrast, the CFA showed better model fit for the three-factor structure, which is consistent with most previous studies with other samples also using CFA. Thus, the CFA supported the original theory underlying the creation of the MSPSS that there are three dimensions of social support.34 The discrepancy between EFA and CFA further suggests that the factors may be method-dependent, thereby recommending caution when choosing the appropriate analytic method to yield a factor structure that best fits the theoretical model of interest.21 This finding shows that there is a lack of agreement about the underlying factor structure of the MSPSS.
There were some limitations to note. First, the sample in the current study was recruited from 12 communities in Changsha city in China, and thus may not be completely generalizable to other families and countries. Second, except for the test–retest assessment, the study was cross-sectional and thus the sensitivity of the measures to change could not be ascertained. And finally, the test–retest reliability was based on a relatively small sample.
Conclusions
The MSPSS is a valid instrument with adequate psychometric properties and can be reliably used to assess perceived social support among family caregivers of people with schizophrenia. Its factors may be method-dependent, with EFA yielding a two-factor structure and CFA more consistent with the original scales a priori three-factor structure. Our study indicates that there is no unified standard on the dimensions of the MSPSS; thus, it is necessary to choose the factor structure that best fits the theoretical model at hand.
Ethical Approval
Ethical approval was obtained from the Institutional Review Committee of the Xiangya School of Public Health of Central South University (No.: XYGW-2019-029). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all individual participants included in the study.
Acknowledgments
The authors would like to thank all the families of individuals with schizophrenia for their participation in the WIFI program and for openly sharing their feelings and experiences. We would also like to thank the Changsha Psychiatric Hospital as well as the 12 community health centers for their collaboration and support. The MSPSS is free to use (Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment 1988;52:30-41).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was funded by a grant from the National Natural Science Foundation of China (Grant Number 71804197) and the China Scholarship Council (CSC) in support of the corresponding author Dr. Yu Yu.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Palacio GC, Krikorian A, Gomez-Romero MJ, Limonero JT. Resilience in caregivers: a systematic review. Am J Hosp Palliat Med. 2019;37(8):648–658.
2. Trask PC, Paterson AG, Trask CL, Bares CB, Birt J, Maan C. Parent and adolescent adjustment to pediatric cancer: associations with coping, social support, and family function. J Pediatr Oncol Nurs. 2003;20(1):36–47. doi:10.1053/jpon.2003.5
3. Maddy LM
4. Matel-Anderson DM, Bekhet AK, Garnier-Villarreal M. Mediating effects of positive thinking and social support on suicide resilience. West J Nurs Res. 2019;41(1):25–41. doi:10.1177/0193945918757988
5. Kim S, Suh S. Social support as a mediator between insomnia and depression in female undergraduate students. Behav Sleep Med. 2019;17(4):379–387. doi:10.1080/15402002.2017.1363043
6. Cruz Dantas MM, Carlos Alchieri J, Chaves Maia EM. Instruments employed in the evaluation of social support. Acta Psiquiatr Psicol Am Lat. 2015;61(4):305–313.
7. Zimet GDDN, Dahlem NW, Zimet SG, Farley,GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52(1):30–41. doi:10.1207/s15327752jpa5201_2
8. Pushkarev GS, Zimet GD, Kuznetsov VA, Yaroslavskaya EI. The Multidimensional Scale of Perceived Social Support (MSPSS): reliability and validity of Russian version. Clin Gerontol. 2020;43(3):331–339. doi:10.1080/07317115.2018.1558325
9. Nearchou F, Davies A, Hennessy E. Psychometric evaluation of the multi-dimensional scale of perceived social support in young adults with chronic health conditions. Ir J Psychol Med. 2019;1–5. doi:10.1017/ipm.2019.54
10. Aloba O, Opakunle T, Ogunrinu O. Psychometric characteristics and measurement invariance across genders of the Multidimensional Scale of Perceived Social Support (MSPSS) among Nigerian adolescents. Health Psychol Rep. 2019;7(1):69–80. doi:10.5114/hpr.2019.82629
11. Tsilika E, Galanos A, Polykandriotis T, Parpa E, Mystakidou K. Psychometric properties of the multidimensional scale of perceived social support in Greek nurses. Can J Nurs Res. 2019;51(1):23–30. doi:10.1177/0844562118799903
12. Wittenborn AK, Natamba BK, Rainey M, Zlotnick C, Johnson J. Suitability of the multidimensional scale of perceived social support as a measure of functional social support among incarcerated adults with major depressive disorder. J Community Psychol. 2020;48(3):960–976. doi:10.1002/jcop.22315
13. Tonsing K, Zimet GD, Tse S. Assessing social support among South Asians: the multidimensional scale of perceived social support. Asian J Psychiatr. 2012;5(2):164–168. doi:10.1016/j.ajp.2012.02.012
14. Laksmita OD, Chung M-H, Liao Y-M, Chang P-C. Multidimensional scale of perceived social support in Indonesian adolescent disaster survivors: a psychometric evaluation. PLoS One. 2020;15(3):e0229958–e0229958. doi:10.1371/journal.pone.0229958
15. Wongpakaran T, Wongpakaran N, Sirirak T, Arunpongpaisal S, Zimet G. Confirmatory factor analysis of the revised version of the Thai multidimensional scale of perceived social support among the elderly with depression. Aging Ment Health. 2018;22(9):1143–1148. doi:10.1080/13607863.2017.1339778
16. Wang Y, Wan Q, Huang Z, Huang L, Kong F. Psychometric properties of multi-dimensional scale of perceived social support in Chinese parents of children with cerebral palsy. Front Psychol. 2017;8:2020.
17. Dambi JM, Tapera L, Chiwaridzo M, Tadyanemhandu C, Nhunzvi C. Psychometric evaluation of the Shona version of the Multidimensional Scale of Perceived Social Support Scale (MSPSS-Shona) in adult informal caregivers of patients with cancer in Harare, Zimbabwe. Malawi Med J. 2017;29(2):89–96. doi:10.4314/mmj.v29i2.3
18. Lee SC, Moy FM, Hairi NN. Validity and reliability of the Malay version multidimensional scale of perceived social support (MSPSS-M) among teachers. Qual Life Res. 2017;26(1):221–227. doi:10.1007/s11136-016-1348-9
19. Mohammad AH, Al Sadat N, Yim LS, Chinna K. Validity and reliability of the Hausa version of multidimensional scale of perceived social support index. Iran Red Crescent Med J. 2015;17(2). doi:10.5812/ircmj.18776
20. Akhtar A, Rahman A, Husain M, Chaudhry IB, Duddu V, Husain N. Multidimensional scale of perceived social support: psychometric properties in a South Asian population. J Obstet Gynaecol Res. 2010;36(4):845–851. doi:10.1111/j.1447-0756.2010.01204.x
21. Yu Y, Shiu CS, Yang JP, et al. Factor analyses of a social support scale using two methods. Qual Life Res. 2015;24(4):787–794. doi:10.1007/s11136-014-0815-4
22. Ho SK, Chan ES. Modification and validation of the multidimensional scale of perceived social support for Chinese school teachers. Cogent Educ. 2017;4(1):1277824. doi:10.1080/2331186X.2016.1277824
23. Zhou K, Lie H, Wei X, et al. Reliability and validity of the multidimensional scale of perceived social support in Chinese mainland patients with methadone maintenance treatment. Compr Psychiatry. 2015;60:182–188. doi:10.1016/j.comppsych.2015.03.007
24. Huang LJQ, Ren WH. The correlation among coping mode, social support and psychosomatic symptoms in patients with cancer. Chin Ment Health J. 1996;10:160–161.
25. Ebrahimi H, Seyedfatemi N, Areshtanab HN, et al. Barriers to family caregivers’ coping with patients with severe mental illness in Iran. Qual Health Res. 2018;28(6):987–1001. doi:10.1177/1049732318758644
26. Madathumkovilakath NB, Kizhakkeppattu S, Thekekunnath S, Kazhungil F. Coping strategies of caregivers towards aggressive behaviors of persons with severe mental illness. Asian J Psychiatr. 2018;35:29–33. doi:10.1016/j.ajp.2018.04.032
27. Sun X, He J, Liu Y, Ge J, Zhang W, Liu D. The influence of social support, care burden, and depression on quality of life among caregivers of patients with severe mental illness: a cross-sectional survey in rural areas of Sichuan, China. Lancet. 2019;394:12.
28. Winahyu KM, Hemchayat M, Charoensuk S. Factors affecting quality of life among family caregivers of patients with schizophrenia in Indonesia. J Health Res. 2015;29:S77–S82.
29. Dyck DG, Short R, Vitaliano PP. Predictors of burden and infectious illness in schizophrenia caregivers. Psychosom Med. 1999;61(4):411–419. doi:10.1097/00006842-199907000-00001
30. Sintayehu M, Mulat H, Yohannis Z, Adera T, Fekade M. Prevalence of mental distress and associated factors among caregivers of patients with severe mental illness in the outpatient unit of Amanuel Hospital, Addis Ababa, Ethiopia, 2013: cross-sectional study. J Mol Pscyhiatr. 2015;3(1):9. doi:10.1186/s40303-015-0014-4
31. Yu Y, Li T, Xi S, et al. Assessing a WeChat-based Integrative Family Intervention (WIFI) for schizophrenia: protocol for a stepped-wedge cluster randomized trial. JMIR Res Protoc. 2020;9(8):e18538. doi:10.2196/18538
32. Good BJ, Good M-JD. Significance of the 686 Program for China and for global mental health. Shanghai Arch Psychiatry. 2012;24(3):175–177.
33. Sapnas KG, Zeller RA. Minimizing sample size when using exploratory factor analysis for measurement. J Nurs Meas. 2002;10(2):135–154. doi:10.1891/jnum.10.2.135.52552
34. Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990;55(3–4):610–617.
35. Aroian K, Templin TN, Ramaswamy V. Adaptation and psychometric evaluation of the multidimensional scale of perceived social support for Arab immigrant women. Health Care Women Int. 2010;31(2):153–169. doi:10.1080/07399330903052145
36. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. doi:10.2307/2136404
37. Smilkstein G, Ashworth C, Montano D. Validity and reliability of the family APGAR as a test of family function. J Fam Pract. 1982;15(2):303–311.
38. Xie Y. Simplified coping style questionnaire. Chin Ment Health J. 1999;13(Suppl):122–124.
39. Folkman S, Lazarus RS. Coping as a mediator of emotion. J Pers Soc Psychol. 1988;54(3):466–475. doi:10.1037/0022-3514.54.3.466
40. Yu Y, Tang BW, Liu ZW, Chen YM, Zhang XY, Xiao -SY*. Who Cares for The Schizophrenia Individuals in Rural China - A Profile of Primary Family Caregivers. Compr Psychiatry. 2018 Jul;84:47-53. doi:10.1016/j.comppsych.2018.04.002
41. Jc N. Psychometric Theory.
42. Campbell MK, Fayers PM, Grimshaw JM. Determinants of the intracluster correlation coefficient in cluster randomized trials: the case of implementation research. ClinTrials. 2005;2(2):99–107. doi:10.1191/1740774505cn071oa
43. Tobias S, Carlson JE. Brief report: Bartlett’s test of sphericity and chance findings in factor analysis. Multivariate Behav Res. 1969;4(3):375–377. doi:10.1207/s15327906mbr0403_8
44. Kaiser H. An index of factorial simplicity. Psychometrika. 1974;39(1):31–36. doi:10.1007/BF02291575
45. Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. doi:10.1080/10705519909540118
46. Bollen KA. Structural Equations with Latent Variables. New York: Wiley; 1989.
47. Ml W. Structural Equation Modeling: AMOS Operation and Application.
48. Teh WL, Shahwan S, Abdin E, et al. Confirmatory factor analysis and measurement invariance of the multidimensional scale of perceived social support in young psychiatric and non-psychiatric asians. Ann Acad Med Singapore. 2019;48(10):314–320.
49. Cartwright AV, Pione RD, Stoner CR, Spector A. Validation of the multidimensional scale of perceived social support (MSPSS) for family caregivers of people with dementia. Aging Ment Health. 2020;1–8. doi:10.1080/13607863.2020.1857699
50. Ekback M, Benzein E, Lindberg M, Arestedt K. The Swedish version of the multidimensional scale of perceived social support (MSPSS) - a psychometric evaluation study in women with hirsutism and nursing students. Health Qual Life Outcomes. 2013;11(1);1–9
51. Wongpakaran T, Wongpakaran N, Ruktrakul R. Reliability and validity of the Multidimensional Scale of Perceived Social Support (MSPSS): Thai Version. Clin Pract Epidemiology Ment Health. 2011;7(1):161–166. doi:10.2174/1745017901107010161
52. Lohanan T, Leesawat T, Wongpakaran T, et al. Development and validation of a screening instrument for borderline personality disorder (SI-Bord) for use among university students. Bmc Psychiatry. 2020;20(1). doi:10.1186/s12888-020-02807-6.
53. Lin J, Su Y, Lv X, et al. Perceived stressfulness mediates the effects of subjective social support and negative coping style on suicide risk in Chinese patients with major depressive disorder. J Affect Disord. 2020;265:32–38. doi:10.1016/j.jad.2020.01.026
54. Cheng ST, Chan ACM. The multidimensional scale of perceived social support: dimensionality and age and gender differences in adolescents. Pers Individ Dif. 2004;37(7):1359–1369. doi:10.1016/j.paid.2004.01.006
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
