Back to Journals » Nature and Science of Sleep » Volume 11
Psychometric Analysis Of The Sleep Hygiene Index And Correlation With Stress And Anxiety Among Saudi University Students
Authors Anwer S , Alghadir A, Manzar MD , Noohu MM , Salahuddin M , Li H
Received 8 July 2019
Accepted for publication 20 September 2019
Published 8 November 2019 Volume 2019:11 Pages 325—332
DOI https://doi.org/10.2147/NSS.S222440
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sutapa Mukherjee
Shahnawaz Anwer,1,2 Ahmad Alghadir,1 Md Dilshad Manzar,3 Majumi M Noohu,4 Mohammed Salahuddin,5 Heng Li2
1Rehabilitation Research Chair, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia; 2Department of Building and Real Estate, Hong Kong Polytechnic University, Kowloon, Hong Kong Special Administrative Region; 3Department of Nursing, College of Applied Medical Sciences, Majmaah University, Al Majmaah 11952, Saudi Arabia; 4Centre for Physiotherapy and Rehabilitation Sciences, Jamia Milia Islamia, New Delhi, India; 5Department of Pharmacy, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan-Aman 260, Ethiopia
Correspondence: Shahnawaz Anwer
Rehabilitation Research Chair, College of Applied Medical Sciences, King Saud University, P.O. Box-10219, Riyadh 11433, Saudi Arabia
Email [email protected]
Aims: This study aimed to assess the psychometric properties of the Sleep Hygiene Index (SHI) instrument in screening poor sleep hygiene practices among Saudi university students. As a secondary goal, the association of sleep hygiene practices with stress and anxiety scores were assessed.
Methods: Two-hundred and four healthy college and university students aged 18 to 25 years participated in this cross-sectional questionnaire-based survey. Participants were asked to complete the English version of the SHI instrument, the Perceived Stress Scale (PSS-10), the Generalized Anxiety Disorder (GAD-7) scale, and to provide demographic details.
Results: The average scores for the SHI, the GAD-7, and the PSS-10 were 6.6, 5.3, and 16.2, respectively. The internal consistency of the SHI was adequate (McDonald’s Omega 0.76). The corrected item-total correlations for all the items were fair (range, 0.31–0.50). A statistically significant positive correlation/association of the SHI scores with the PSS score, GAD-7, and self-reported poor sleep were obtained in this sample of Saudi university students. Factor analysis favored a 4-factor model of the SHI in the study sample.
Conclusion: The SHI scale demonstrated an adequate level of internal consistency as a self-reported instrument in the assessment of sleep hygiene among Saudi university students. In addition, poor sleep hygiene was correlated with stress and anxiety scores.
Keywords: sleep hygiene, stress, anxiety, mood, university student, adolescent
Introduction
Inadequate sleep at night causes day-time sleepiness in approximately half to three-quarters of college students.1 In addition, family histories of anxiety or depression and individuals who manifest lifelong anxiety and depression from early childhood onwards are at greater risk for insomnia in later life.2 Furthermore, previous studies reported a high prevalence of inadequate sleep among youth who exhibit clinical anxiety3,4 as well as high levels of stress and anxiety in university students.5 Similarly, many studies suggested that anxiety is one of the risk factors for future insomnia,6,7 while others reported a bidirectional association of anxiety and depression with insomnia.8,9 Moreover, another study reported highest comorbidity of insomnia among individuals with generalized anxiety disorder (GAD).10
College and university students often reduce their sleep time to provide additional hours for school work and studying.1 As a consequence, students are more likely to develop poor sleeping patterns, especially during examination periods.11 About 59% and 51% of medical students reported inadequate sleep quality in the Europe and Western countries, respectively.12,13 A high prevalence of poor sleep and sleep disturbances have been reported in Afro-Asian university students,14,15 which has often been found to have an association with mental health conditions like anxiety and depression.16 Previous studies have been conducted among Saudi medical students to assess their sleep qualities and their results indicated that about 37% of students reported a poor sleep quality.17,18
Sleep plays a vital role in maintaining mental and physical well-being as well as the cognitive processes.19,20 Lack of sleep can negatively influence the academic performance of college/university students11 and several previous studies have reported reduced academic performance in students with poor sleep hygiene compared to those who had good sleep hygiene.21–23 Another study conducted in China has reported that about 19% of the students had poor sleep hygiene.24 Similarly, more than 90% of undergraduate medical students in Chinese university reported excessive sleepiness during day-time, with women being more affected than men.25
Clinical scales are important tools for evaluating various human behaviors,26 and quality of sleep is commonly evaluated by various scales.27–29 Poor sleep habits are also referred to as poor sleep hygiene.30 Sleep hygiene includes environmental factors, habits, and daily practices that are necessary for good quality of night-time sleep.31 There are three scales that have been developed to assess sleep hygiene: the Sleep Hygiene Index (SHI),32 the Sleep Hygiene Self-Test (SHST),33 and the Sleep Hygiene Awareness and Practice Scale (SHAPS).34
The SHI has demonstrated relatively higher internal consistency (Chronbach’s alpha=0.66)32 compared to the SHST (Chronbach’s alpha=0.54)33 and SHAPS (Chronbach’s alpha=0.47)34 in assessing sleep hygiene. In addition to moderate internal consistency, the SHI has shown good test–retest reliability (r=0.71, p<0.001) and was significantly correlated with sleep quality and sleepiness in day among nonclinical subjects.32 However, despite the importance of sleep hygiene, there is a dearth of studies assessing sleep hygiene practices among college/university students in Saudi Arabia. Further, no previous studies have validated the use of the SHI to assess sleep hygiene practices among Saudi university students.
Given the seriousness of sleep problems and psychological issues (e.g., stress and anxiety) and their negative impact on the professional and academic life of university students, the current study aimed to assess the psychometric properties (including internal consistency and factor analysis) of the SHI instrument in assessing sleep hygiene practices among Saudi university students. Secondarily, the relationship between sleep hygiene practices and stress and anxiety scores were assessed.
Methods
Participants
A pool of healthy college and university students who were potential participants in this study were invited using a simple random sampling design. Inclusion criteria were that the students were aged 18 years and older and were willing to participate in the study. Participants with the presence of chronic disease, current or past history of schizophrenia, bipolar, or other psychotic disorders, memory problems, and the use of neuro-psychotic medications were excluded. Study aims and procedures were explained to each participant. Participants were asked to complete the English version of the SHI, the Perceived Stress Scale (PSS-10), the Generalized anxiety disorder (GAD-7), and to provide demographic details. Since potential participants were students of an English education system, the original English version of the questionnaire was used in this study. The current study was approved by the institutional Ethical committee, Rehabilitation Research chair, King Saud University, Saudi Arabia. The required sample size was estimated according to published criteria regarding the subject-to-item ratio (2–20 subjects per item).35 Therefore, we enrolled more than 15 participants for each item of the SHI (n=204). We hypothesized that the SHI would be a reliable tool for assessing sleep hygiene practices among Saudi university students. Additionally, we expected that there would be a positive correlation/association of the SHI scores with PSS, GAD, and self-reported poor sleep.
Measures
SHI Instrument
The SHI is a self-administered 13-item instrument designed to assess sleep hygiene behavioral during day-to-day life.32 Items in the SHI were adopted from the diagnostic criteria for poor sleep hygiene in the International Classification of Sleep Disorders.36 Participants were requested to indicate if they engaged in certain sleep hygiene behaviors. In this study, a dichotomized scoring system for each of the 13-items was employed with 0=no and 1=yes. The items were summed to obtain a global SHI score ranging from 0 to 13. A higher SHI score signifies poorer sleep hygiene. Previous research has shown adequate reliability and validity of the SHI.32
PSS-10
The PSS is a 10-item instrument designed to evaluate the self-perceived amount of stress of the participants. Each item is scored on a 6-point Likert scale ranging from 0 (never) to 5 (very often). The items are added to obtain a total PSS score ranging from 0 to 40. Higher score indicates higher levels of stress.37
GAD-7
The GAD scale is a self-administered 7-item instrument designed to evaluate the level of anxiety over a period of 2 weeks. Each item is scored on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). The items are added to obtain a total GAD score ranging from 0 to 21. Higher scores indicate higher levels of anxiety. The items were designed to evaluate symptoms of anxiety according to the Diagnostic and Statistical Manual of Mental Disorders-IV-TR.38
Self-Reported Poor Sleep
Self-reported sleep was assessed on dichotomous scale indicating normal or disturbed sleep.
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS 22.0) software (SPSS Inc., Chicago, USA) and Factor 10.8.04 were used for the statistical analyses. Descriptive statistics were calculated to present mean, percentages, frequencies, and indexes of skewness and kurtosis. Internal consistency was assessed using the McDonald’s Omega and Cronbach’s alpha tests. The correlation of the SHI scores with the PSS and GAD-7 scores was evaluated using the Spearman correlation test. Binary logistic regression was employed to assess relationship between the dichotomous measures of self-reported poor sleep with the SHI total score. Factor 10.8.04 was used for factor analyses: an exploratory factor analysis followed by a semi-confirmatory factor analysis.39 Sample suitability and sample size adequacy for the factor analysis of the SHI scores were assessed using the Kaiser-Meyer-Olkin Test of Sampling Adequacy (KMO; 0.66), determinant (0.29), Bartlett’s test of sphericity (χ2 (78)=248.8, p<0.00001),40 and the communalities for all items were above the minimum criteria of 0.2.41 Robust factor analysis for bias-corrected and accelerated solution using tetrachoric correlation dispersion matrix with bootstrapping for 500 samples was performed. Robust diagonally weighted least square methods for factor extraction with promin rotation were used in the EFA. Factor loadings in the EFA were estimated for linear models. Kaiser’s criteria (Eigenvalue ≥1),42 the cumulative variance rule (>40%), and parallel analysis were used for the factor extraction in the EFA.43 Model fit was evaluated using the weighted root mean square residual (WRMR), goodness of fit index (GFI), comparative fit index (CFI), root mean square error of approximation (RMSEA), and robust mean and variance-adjusted chi square. The values indicating acceptable and/or excellent fit were determined by the previously published guidelines.44,45 These values included a p-value >0.05 for χ2, the χ2/df <2, the GFI>0.95, the CFI>0.95, RMSEA and WRMR<0.05.44,45 The statistical level of significance was set at p<0.05. A receiver operating curve (ROC) analysis with self-reported poor sleep as the state variable and SHI total score as the test variable was performed.
Results
Participants’ Characteristics And Item Distribution
Table 1 presents the participants’ demographic characteristics. Approximately 50% of the participants were in the 3rd, 4th, and 5th year of university education and about 40% of the participants were enrolled in nursing and allied healthcare courses; however, approximately 50% of the participants did not report about their courses. The average scores for the SHI, the GAD-7, and the PSS-10 were 6.6, 5.3, and 16.2, respectively. Seven SHI item scores had univariate asymmetry, with the absolute value of skewness greater than 1, while 10 items had kurtosis issues (Table 2). However, no major issues of multivariate asymmetry skewness and kurtosis were found as determined by a non-significant value of Mardia’s coefficient of skewness and kurtosis.
 |
Table 1 Participant Characteristics Of Saudi University Students |
 |
Table 2 Internal Consistency And Univariate Distribution Characteristics Of The Sleep Hygiene Index (SHI) In Saudi University Students |
Internal Consistency
The internal consistency of the SHI is presented in Table 2. The internal consistency of the SHI was adequate as determined by the McDonald’s Omega (0.76), though Cronbach’s alpha (0.59) indicated a moderate level. The corrected item-total correlations for all the items were fair (range=0.31–0.50). The Cronbach’s alpha values did not increase above 0.61 if individual items were deleted.
Association/Correlation With Related Measures
Statistically significant positive correlations of the SHI scores with the PSS score (r=0.29), GAD-7 (r =0.36), and self-reported poor sleep (odds ratio: 1.20 95% Confidence interval (1.01–1.43), p<0.05) were obtained.
Factor Analysis
Measures Of Sample Suitability And Adequacy For Factor Analysis
The Kaiser-Meyer-Olkin Test of Sampling Adequacy (KMO) (0.66) indicates that the sample size is adequate.46 The Bartlett’s test of Sphericity (<0.001) ruled out the issue of singularity in the SHI item scores.46 Further, the determinant score (0.29) indicates that there was no problem of multicollinearity in the SHI item scores.46
Exploratory Factor Analysis
Table 3 and Figure 1 detail the factor extraction measures used in the exploratory factor analyses of the SHI scores in our sample of Saudi university students. The three tests showed heterogenous findings, that is, the cumulative variance rule (>40%), the Kaiser’s criteria (Eigenvalue >1), and the parallel analysis based on principal component analysis (Figure 1A) and parallel analysis based on minimum rank factor analysis (Figure 1B) indicated disparate models; 2-factor, 4-factor, 4-factor model and 1-Factor solution for the SHI (Table 4).
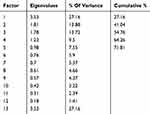 |
Table 3 Exploratory Factor Analysis: Eigenvalues And Total Variance Explained Of The Sleep Hygiene Index (SHI) In Saudi University Students |
 |
Table 4 Exploratory Factor Analysis: Factor Loadings And Communality Of The Sleep Hygiene Index (SHI) In Saudi University Students |
Model Fit
Table 5 indicates that the 4-factor model had the best fit with lowest values for RMSEA, WRMR, χ2 and χ2/df, and optimal value for CFI, non-significant χ2 and highest value for GFI.
 |
Table 5 Fit Statistics Of The Sleep Hygiene Index Models In Saudi University Students |
Screening For Self-Reported Poor Sleep
A ROC analysis found that a cutoff total score of 7.5 for the SHI total score showed the highest accuracy (sensitivity: 57.6% and specificity: 67.6%) for classifying cases with self-reported poor sleep among the sample of Saudi university students in this study (area under the curve=0.62, 95% confidence interval=0.52–0.73).
Discussion
The present study supports the evidence for the psychometric analysis of the SHI in Saudi university students. We found that the SHI scale had an acceptable level of internal consistency in our sample. Given that SHI with dichotomous scoring for individual items was used in this study, McDonald’s Omega is better suited to assess internal consistency. However, Cronbach’s alpha was also presented for inter-study comparisons. A recent study reported a moderate level of internal consistency of SHI among Nigerian university students.43 However, previous studies reported higher values of the Cronbach’s alpha (ranges, 0.66–0.89). Ozdemir et al47 reported a Cronbach’s alpha value of 0.70–0.71 in a Turkish sample, while Cho et al48 identified a Cronbach’s alpha value of 0.75 in a Korean sample. Further, Chehri et al49 and Mastin et al32 noted Cronbach’s alpha values of 0.89 and 0.66 in Persian and United States samples, respectively. However, a direct comparison between previous studies and the current study is difficult since the previous studies were carried on the non-clinical and clinical patients,47 chronic pain,48 and the general population.49 In the present study, there were minor variations in the Cronbach’s alpha value if items were deleted, especially for items 2, 6, and 8, suggesting the importance and relevance of each item for the structural validity of the SHI among Saudi university students.
The expected relationship between poor sleep and stress-related anxiety is supported in the present study by the significant correlations between the SHI total score and the PSS score, GAD-7 score, and self-reported poor sleep score. Previous studies have reported a bidirectional association of anxiety and depression with insomnia.8,9 Additionally, another study reported poor sleep hygiene and sleep problems among individuals with GAD.10
The results of the exploratory factor analysis indicated three different factor structures for the SHI among Saudi university students. The model fit indices employed favored the 4-factor model for the SHI in the study population. These findings are different from those reported in some of the previous studies. Cho el al48 reported a 3-factor model for the SHI in chronic pain patients. However, it is noteworthy that the findings are based only on the EFA.48 Seun-Fadipe et al43 reported that a 2-factor model of the SHI was optimal in a Nigerian university student population. Chehri et al49 also found a 3-factor model for the SHI in a Persian male population. It is therefore recommended that future studies with large sample sizes and multi-centre data collection should explore the dimensionality of the SHI using EFA, CFA, and measurement invariance across socio-demographic characteristics for a better understanding on this topic. The SHI was found to have adequate validity for screening students with self-reported poor sleep. The results are slightly better than those reported by Seun-Fadipe et al43 for-screening Nigerian undergraduate students with poor sleep quality based on the subjective evaluation by a questionnaire. In that study, sub-optimal specificity (below 50%) was reported for screening students with poor sleep quality using the SHI.
Conclusion
The SHI had adequate levels of internal consistency as a self-reported instrument in the assessment of sleep hygiene practices among Saudi university students. In addition, poor sleep hygiene was associated with stress, anxiety, and self-reported poor sleep in Saudi university students. Further research is needed to explore the effects of lifestyle behaviors such as problematic use of internet, mobile devices, and online games on sleep hygiene practices.
Acknowledgments
The authors are grateful to the Deanship of Scientific Research, King Saud University, for funding through Vice Deanship of Scientific Research Chairs.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hershner SD, Chervin RD. Causes and consequences of sleepiness among college students. Nat Sci Sleep. 2014;6:73–84. doi:10.2147/NSS.S62907
2. Goldman-Mellor S, Gregory AM, Caspi A, et al. Mental health antecedents of early midlife insomnia: evidence from a four-decade longitudinal study. Sleep. 2014;37(11):1767–1775. doi:10.5665/sleep.4168
3. Forbes EE, Bertocci MA, Gregory AM, et al. Objective sleep in pediatric anxiety disorders and major depressive disorder. J Am Acad Child Adolesc Psychiatry. 2008;47(2):148–155. doi:10.1097/chi.0b013e31815cd9bc
4. Storch EA, Murphy TK, Lack CW, Geffken GR, Jacob ML, Goodman WK. Sleep-related problems in pediatric obsessive-compulsive disorder. J Anxiety Disord. 2008;22(5):877–885. doi:10.1016/j.janxdis.2007.09.003
5. Royal college of psychiatrists, Mental health of students in higher education. London; 2011. Available from: https://www.rcpsych.ac.uk/mental-health/parents-and-young-people/young-people/worries-and-anxieties.
6. Jansson M, Linton SJ. The development of insomnia within the first year: a focus on worry. Br J Health Psychol. 2006;11(Pt 3):501–511. doi:10.1348/135910705X57412
7. Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30(3):274–280. doi:10.1093/sleep/30.3.274
8. Jansson-Frojmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64(4):443–449. doi:10.1016/j.jpsychores.2007.10.016
9. Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40(8):700–708. doi:10.1016/j.jpsychires.2006.07.008
10. Monti JM, Monti D. Sleep in schizophrenia patients and the effects of antipsychotic drugs. Sleep Med Rev. 2004;8(2):133–148. doi:10.1016/S1087-0792(02)00158-2
11. Ahrberg K, Dresler M, Niedermaier S, Steiger A, Genzel L. The interaction between sleep quality and academic performance. J Psychiatr Res. 2012;46:1618–1622. doi:10.1016/j.jpsychires.2012.09.008
12. Preišegolavičiūtė E, Leskauskas D, Adomaitienė V. Associations of quality of sleep with lifestyle factors and profile of studies among Lithuanian students. Medicine. 2010;46:482–489. doi:10.3390/medicina46070070
13. Brick CA, Seely DL, Palermo TM. Association between sleep hygiene and sleep quality in medical students. Behav Sleep Med. 2010;8:113–121. doi:10.1080/15402001003622925
14. Manzar MD, Zannat W, Kaur M, Hussain ME. Sleep in university students across years of university education and gender influences. Int J Adolesc Med Health. 2015;27(3):341–348. doi:10.1515/ijamh-2014-0037
15. Manzar MD, Bekele BB, Noohu MM, et al. Prevalence of poor sleep quality in the Ethiopian population: a systematic review and meta-analysis. Sleep Breath. 2019;10:1–8. doi:10.1007/s11325-019-01871-x
16. Ghrouz AK, Noohu MM, Manzar MD, Spence DW, BaHammam AS, Pandi-Perumal SR. Physical activity and sleep quality in relation to mental health among college students. Sleep Breath. 2019;23(2):627–634. doi:10.1007/s11325-019-01780-z
17. Abdulghani HM, Alrowais NA, Bin-Saad NS, Al-Subaie NM, Haji AM, Alhaqwi AI. Sleep disorder among medical students: relationship to their academic performance. Med Teach. 2012;34(Suppl 1):S37–41. doi:10.3109/0142159X.2012.656749
18. Bahammam AS, Alaseem AM, Alzakri AA, Almeneessier AS, Sharif MM. The relationship between sleep and wake habits and academic performance in medical students: a cross-sectional study. BMC Med Educ. 2012;12:61. doi:10.1186/1472-6920-12-61
19. Ratcliff R, Van Dongen HP. Sleep deprivation affects multiple distinct cognitive processes. Psychon Bull Rev. 2009;16:742–751. doi:10.3758/PBR.16.4.742
20. Giri P, Baviskar M, Phalke D. Study of sleep habits and sleep problems among medical students of Pravara institute of medical sciences, Loni, Western Maharashtra, India. Ann Med Heal Sci Res. 2013;3:51–54. doi:10.4103/2141-9248.109488
21. Vanderlind WM, Beevers CG, Sherman SM, et al. Sleep and sadness: exploring the relation among sleep, cognitive control, and depressive symptoms in young adults. Sleep Med. 2014;15:144–149. doi:10.1016/j.sleep.2013.10.006
22. Short MA, Gradisar M, Lack LC, Wright HR. The impact of sleep on adolescent depressed mood, alertness and academic performance. J Adolesc. 2013;36:1025–1033. doi:10.1016/j.adolescence.2013.08.007
23. Menon B, Karishma HP, Mamatha IV. Sleep quality and health complaints among nursing students. Ann Indian Acad Neurol. 2015;18:363–364. doi:10.4103/0972-2327.157252
24. Feng G, Chen J, Yang X. Study on the status and quality of sleep-related influencing factors in medical college students. Zhonghua Liu Xing Bing Xue Za Zhi. 2005;26:328–331.
25. Lu J, Fang GE, Shen SJ, Wang Y, Sun Q. A questionnaire survey on sleeping in class phenomenon among Chinese medical undergraduates. Med Teach. 2011;33:508.
26. Fernández-Cruz KA, Jiménez-Correa U, Marín-Agudelo HA, Castro-López C, Poblano A. Proposing the clinical inventory of sleep quality. Sleep Sci. 2016;9(3):216–220. doi:10.1016/j.slsci.2016.10.002
27. Buysse DJ, Reynolds CHF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi:10.1016/0165-1781(89)90047-4
28. Akerstedt T, Hume K, Minors D, Waterhouse J. The subjective meaning of good sleep, in intra individual approach using the Karolinska Sleep Diary. Percept Mot Skills. 1994;79:287–296. doi:10.2466/pms.1994.79.1.287
29. Zammit GK. Subjective ratings of the characteristics and sequelae of good and poor sleep in normals. J Clin Psychol. 1988;44:123–130. doi:10.1002/1097-4679(198803)44:2<123::AID-JCLP2270440206>3.0.CO;2-D
30. Currie SR, Wilson KG, Pontefract AJ, deLaplante L. Cognitive–behavioral treatment of insomnia secondary to chronic pain. J Consult Clin Psychol. 2000;68:407–416. doi:10.1037/0022-006X.68.3.407
31. Riedel BW. Sleep hygiene. In: Lichstein KL, Morin CM, editors. Treatment of Of Late-Life Insomnia. Thousand Oaks, CA: Sage; 2000.
32. Mastin DF, Bryson J, Corwyn R. Assessment of sleep hygiene using the sleep hygiene index. J Behav Med. 2006;29:223–227. doi:10.1007/s10865-006-9047-6
33. Blake DD, Gomez MH. A scale for assessing sleep hygiene: preliminary data. Psychol Rep. 1998;83:1175–1178. doi:10.2466/pr0.1998.83.3f.1175
34. Lacks P, Rotert M. Knowledge and practice of sleep hygiene techniques in insomniacs and good sleepers. Behav Res Ther. 1986;24:365–368. doi:10.1016/0005-7967(86)90197-X
35. Anthoine E, Moret L, Regnault A, Sébille V, Hardouin J-B. Sample size used to validate a scale: a review of publications on newly-developed patient reported outcomes measures. Health Qual Life Outcomes. 2014;12:176. doi:10.1186/s12955-014-0176-2
36. Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–1394. doi:10.1378/chest.14-0970
37. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. doi:10.2307/2136404
38. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
39. Ferrando PJ, Lorenzo-Seva U. Program FACTOR at 10: origins, development and future directions. Psicothema. 2017;29(2):236–240. doi:10.7334/psicothema2016.304
40. Kaiser HF. A second generation little jiffy. Psychometrika. 1970;35:401–416. doi:10.1007/BF02291817
41. Child D. The Essentials of Factor Analysis.
42. Williams B, Onsman A, Brown T. Exploratory factor analysis: A five-step guide for novices. Australas J Paramed. 2010;8(3):1–13. doi:10.33151/ajp.8.3.93
43. Seun-Fadipe CT, Aloba OO, Oginni OA, Mosaku KS. Sleep hygiene index: psychometric characteristics and usefulness as a screening tool in a sample of Nigerian undergraduate students. J Clin Sleep Med. 2018;14(8):1285–1292. doi:10.5664/jcsm.7256
44. Manzar MD, BaHammam AS, Hameed UA, et al. Dimensionality of the Pittsburgh sleep quality index: a systematic review. Health Qual Life Outcomes. 2018;16(1):89. doi:10.1186/s12955-018-0915-x
45. Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. doi:10.1080/10705519909540118
46. Field AP. Discovering Statistics Using SPSS for Windows: Advanced Techniques for Beginners. London, UK: Sage Publications; 2000.
47. Ozdemir PG, Boysan M, Selvi Y, Yildirim A, Yilmaz E. Psychometric properties of the Turkish version of the sleep hygiene index in clinical and non-clinical samples. Compr Psychiatry. 2015;59:135–140. doi:10.1016/j.comppsych.2015.02.001
48. Cho S, Kim GS, Lee JH. Psychometric evaluation of the sleep hygiene index: a sample of patients with chronic pain. Health Qual Life Outcomes. 2013;11:213. doi:10.1186/1477-7525-11-213
49. Chehri A, Kiamanesh A, Ahadi H, Khazaie H. Psychometric properties of the persian version of sleep hygiene index in the general population. Iran J Psychiatry Behav Sci. 2016;10(3):e5268. doi:10.17795/ijpbs-5268
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

