Back to Journals » Psychology Research and Behavior Management » Volume 15
Psychological Status and Job Burnout of Nurses Working in the Frontline of the Novel Coronavirus in China During the Delta Variant Outbreak: A Cross-Sectional Survey
Authors Hou J, Xu B, Zhang J , Luo L, Pen X, Chen S, Ma G, Hu Z, Kong X
Received 21 October 2021
Accepted for publication 18 February 2022
Published 5 March 2022 Volume 2022:15 Pages 533—546
DOI https://doi.org/10.2147/PRBM.S343749
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Igor Elman
Jianmei Hou,1,2 Binbin Xu,1 Jinghui Zhang,1,3,4 Lingxia Luo,1,5 Xiaobei Pen,1,6 Shujie Chen,1,4 Guiyuan Ma,1,4 Zixing Hu,1,4 Xiaoya Kong1,4
1Teaching and Research Section of Clinical Nursing, Xiangya Hospital, Central South University, Changsha, Hunan, 410008, People’s Republic of China; 2Department of Thoracic Surgery, Xiangya Hospital, Central South University, Changsha, Hunan, 410008, People’s Republic of China; 3National Clinical Research Center for Geriatric Disorders, Xiangya Hospital, Changsha, Hunan, 410008, People’s Republic of China; 4Xiangya Nursing School, Central South University, Changsha, Hunan, People’s Republic of China; 5Emergency Department, Xiangya Hospital, Central South University, Changsha, Hunan, 410008, People’s Republic of China; 6Intensive Care Unit, Xiangya Hospital, Central South University, Changsha, Hunan, 410008, People’s Republic of China
Correspondence: Jinghui Zhang, Tel +86 15874032339, Email [email protected]
Purpose: Investigating psychological status and job burnout of nurses working in the frontline of the novel coronavirus in Zhangjiajie city in China during the Delta variant outbreak, comparing differences and analyzing factors of these two variables between the nurses from different nucleic acid testing (NAT) sites.
Patients and methods: This survey was conducted from August 1 to 31, 2021. The participants were 512 nurses, 198 nurses of whom were from temporary NAT sites in communities/towns in Zhangjiajie city, and the rest were from NAT sites inside hospitals. The psychological status and the job burnout were measured by the Symptom Checklist-90 (SCL-90) and the Maslach Burnout Inventory-General Scale (MBI-GS).
Results: The prevalence of the SCL-90 positive result and job burnout were 49.4% and 61.1%, respectively. The factors influencing the psychological status of nurses included the contact with COVID-19 patients or their body fluids and specimens, working seniority and the duration of working in the frontline of the novel coronavirus. The independent risk factors of nurses’ job burnout included the following four factors. Firstly, the contact with COVID-19 patients or their body fluids and specimens (OR=150.95, 95% CI=(44.87,507.77), P< 0.001). Secondly, five to nine years of working seniority (OR=8.91, 95% CI=(3.59,22.14), P< 0.001). Thirdly, 10 to 19 days (OR=2.63, 95% CI=(1.19,5.82), P=0.017), 20 to 29 days (OR=161.31, 95% CI=(49.48,525.9), P< 0.001). Lastly, more than 30 days (OR=92.05, 95% CI=(33.88,250.14), P< 0.001) of working in the frontline of the novel coronavirus.
Conclusion: The prevalence of psychological problems and job burnout were at a high level among nurses working in the frontline of the novel coronavirus in different NAT sites. The nurses from NAT sites inside hospitals and temporary NAT sites in communities/towns in Zhangjiajie city had an equal risk of developing psychological problems and job burnout. Interventions need to be immediately implemented to promote psychological well-being and decrease job burnout of nurses.
Keywords: psychological status, job burnout, specimen collection, nucleic acid testing, the novel coronavirus, the Delta variant
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), has ravaged the world.1 Globally, as of 4:14pmCET, 29 December 2021, 281,808,270 confirmed cases of COVID-19 have been reported by the World Health Organization (WHO), including 5,411,759 confirmed deaths, with a mortality of 1.92%.2 The Delta variant, has the characteristics of a short incubation period, a quick velocity of propagation, and a high virus load.3 It was first reported in India in December 2020, and began to spread to many provinces and regions in China in May 2021.4 On November 26, 2021, WHO identified the Omicron variant as a variant of concern, which may result in a higher transmission rate and considerable impact when compared to the Delta variant.5
The confirmed cases of the novel coronavirus in Dalian city were found to have an activity track in Zhangjiajie city from July 17 to July 23, and on July 29, the confirmed case of the novel coronavirus in Zhangjiajie city was found.6 And then the novel coronavirus began to outbreak in Zhangjiajie city.6 To quickly screen the people infected by the Delta variant in Zhangjiajie city, universal nucleic acid testing (NAT) was conducted urgently, and besides the NAT sites inside hospitals, many NAT sites were temporarily set up in the communities and the towns of Zhangjiajie city.
Previous studies have reported that psychological problems such as anxiety and depression were found in frontline nurses fighting against the COVID-19.7–12 Poor sleep quality and stress are common during the COVID-19 crisis.13 Approximately, 60% of both frontline healthcare workers and non-frontline healthcare workers have poor sleep quality combined with moderate-severe stress.13 A multivariable logistic regression analysis showed that the depression in healthcare workers was significantly associated with the profession.14 The anxiety in healthcare workers was significantly associated with their age, profession, and residence.14 The stress in healthcare workers was significantly associated with their age.14
The job burnout of this population was also reported.15 The nurses working in the frontline of the novel coronavirus from NAT sites inside hospitals and temporary NAT sites in communities/towns in Zhangjiajie city during the Delta variant outbreak may also have these problems. Because they faced the high risk of being infected by the Delta variant and the fear of infection and death. These factors might make them suffer from huge psychological stress and even cause a sense of job burnout. In addition, compared with the nurses from NAT sites inside hospitals in Zhangjiajie city, those from temporary NAT sites in communities/towns in Zhangjiajie city were exposed to more stress and their psychological problems might be more serious since they not only bear the high risk of infection but also suffer from the open-air and high-temperature environment. However, little is known about the differences in the psychological state and job burnout between these two groups of nurses.
Therefore, the present cross-sectional study aimed to investigate the psychological status and job burnout of nurses working in the frontline of the novel coronavirus in China during the Delta variant outbreak and compare the differences in these two variables between the nurses from NAT sites inside hospitals and temporary NAT sites in communities/towns in Zhangjiajie city We also aimed to characterize and identify some factors influencing the psychological status and job burnout of nurses, which may provide information for nursing managers to make strategies to improve the psychological health of nurses and their work efficiency.
Methods
Study Design and Participants
This cross-sectional survey was conducted from August 1, 2021, to August 31, 2021, following approval by the Ethics Committee of Xiangya Hospital (ethics approval number: 202005402) and participants’ informed consent. The participants were nurses working in the frontline of the novel coronavirus from NAT sites inside hospitals and temporary NAT sites in communities/towns in Zhangjiajie city during the Delta variant outbreak. We went to the hospitals in Zhangjiajie city and selected nurses working in the frontline of the novel coronavirus from August 1, 2021, to August 31, 2021 by the snowball sampling method. There are some eligibility criteria about our participants: firstly, they were nurses working in the frontline of the novel coronavirus from NAT sites inside hospitals and temporary NAT sites in communities/towns in Zhangjiajie city from August 1, 2021, to August 31; secondly, they had all passed the training of NAT of the novel coronavirus and had more than 2 years of working experience; thirdly, they gave full informed consent prior to their participation. There are 105 items in the two questionnaires we used (MBI-GS and SCL-90), so our sample size should be at least 5 times of the number of items, that is, 525 participants. We received 554 questionnaires in total and excluded 42 ineligible responses. The valid response rate of the present study was 94.1% (512 out of 544).
The data was collected via Wen Juan Xing which is a professional online platform used for survey, voting, online registration, information collection, and online examination. Compared with the traditional survey method, it is fast, easy to use, cost-effective, and more suitable for the investigation during the outbreak of the Delta variant. The questionnaires were uploaded to Wen Juan Xing on August 1, 2021, and then the questionnaire link was pushed by WeChat Moments and WeChat groups for 31 days. To ensure the scientificity and integrity of data, before pushing the link, we explained the purpose of this survey and the precautions for filling in the questionnaire to all participants by Tencent Video Conferencing. We also set that each WeChat ID could only answer the questionnaire once and all questions required to be answered before submission.
Measurements
Sociodemographic data were collected by a self-designed questionnaire, including gender, age, marital status, educational attainment, professional title, working seniority, and the duration of working in the frontline of the novel coronavirus. Participants were also asked whether they had direct contact with COVID-19 patients or patients’ body fluids and specimens.
The psychological status of nurses was measured by the Symptom Checklist-90 (SCL-90), a 90-item self-report scale. The SCL-90 was developed by LR Derogatis in 1973 and was translated into the Chinese version by Wang Zhengyi in 1984.16,17 It contains 10 dimensions, including Somatization (12 items), Obsessive-Compulsive (10 items), Interpersonal Sensitivity (9 items), Depression (13 items), Anxiety (10 items), Hostility (6 items), Phobic anxiety (7 items), Paranoid Ideation (6 items), Psychoticism (10 items), and seven additional items to assess disturbances in appetite and sleep. Each item was assigned a score ranging from 1 (no symptom) to 5 (serious symptom). The items with a score of 2 and above were deemed positive items. The higher the score, the worse the psychological status.
In the present study, we calculated and analyzed the total score of 90 items, the dimension scores, the Global Severity Index (GSI),18 and the number of positive items of the SCL-90. The dimension score was calculated according to the formula: dimension score=the total score of the dimension/ the number of the dimension. The GSI equaled the total score divided by 90. The result was positive and further examination was required when the total score was more than 160, or any dimension score was more than 2, or the number of positive items was more than 43.11
The job burnout of nurses was measured by the Maslach Burnout Inventory-General Scale (MBI-GS),19 which was one of the versions of MBI and could be used in any occupational population. It was translated into Chinese version by Li Chaoping in 2003,20 with 15 items in total covering three dimensions: emotional exhaustion (5 items), cynicism (4 items), reduced personal accomplishment (6 items). It has good internal consistency reliability, whose Cronbach’s alpha coefficient for emotional exhaustion, cynicism, reduced personal accomplishment is 0.88, 0.83, 0.82 respectively.20 Each item consists of a 7-point Likert scale ranging from 0 (never) to 6 (every day). The scores of six items of reduced personal accomplishment were reversed. The higher the score, the higher the job burnout level.
In the present study, we calculated the dimension score and weighted sum score of job burnout. The former refers to the total score of each dimension, the latter was calculated according to the formula: Burnout= 0.4* emotional exhaustion+0.3* cynicism+0.3* reduced personal accomplishment.21 The participants could be divided into three groups according to the weighted sum score of job burnout: no burnout (weighted sum score ranging from 0–1.49), moderate burnout (weighted sum score ranging from 1.50–3,49), and severe burnout (weighted sum score ranging from 3.50–6.00).22 Participants with moderate or severe burnout were deemed to be a burnout case.
Statistical Analysis
Descriptive statistics were used to summarize participant characteristics. The SCL-90 scores, weighted sum score of job burnout, and the prevalence of job burnout. The One-sample t-test was used to compare the SCL-90 dimension scores of the subjects in the present study and these of Chinese nurses.23 The Spearman correlation analysis was used to explore the correlation between SCL-90 scores and job burnout when the data is not normally distributed. The GSI in different populations was compared using the Wilcoxon rank-sum test for the two-group comparison and the Kruskal–Wallis H-test was used for multiple comparisons when the data is not normally distributed. The Chi-squared test was used to compare the prevalence of job burnout in different populations. The generalized linear model was used for multivariate analysis to identify the influencing factors of psychological status since the dependent variable (GSI) was not normally distributed. The gamma distribution was selected as the distribution of the dependent variable and the logarithmic function was selected as the link function. Backward: LR binary logistic regression was used to identify the risk factors of job burnout. All analyses were performed using SPSS V.22.0.
Results
Participant Characteristics
We received 554 questionnaires in total and excluded 42 ineligible responses. The valid response rate of the present study was 94.1% (512 out of 544). Among 512 respondents, 38.7% were nurses from temporary NAT sites in communities/towns in Zhangjiajie city, the rest were from NAT sites inside hospitals in Zhangjiajie city. The majority were women (86.1%) and had a bachelor’s degree or above (82.8%). About half of the subjects were aged under 30 (48.8%) and got married (55.5%). 62.7% exhibited a junior professional title, and the largest working seniority group ranged between five to nine years (40.6%). 30.7% of the respondents reported having been working in the frontline of the novel coronavirus for more than 30 days, and the majority (88.7%) had direct contact with COVID-19 patients or their body fluids and specimens (Table 1).
 |
Table 1. Demographic Characteristics of the Participant Nurses (n=512) |
Psychological Status, Job Burnout and the Correlation Between the Two Variables
In the present study, 49.4% of the subjects exhibited positive results of SCL-90. The GSI of the SCL-90 among 512 nurses working in the frontline of the novel coronavirus was (1.59 ± 0.43). Table 2 indicated the dimension scores of current samples and the comparison with the Chinese nurse. The difference in interpersonal sensitivity, depression, anxiety, hostility, and phobic anxiety was statistically significant (all P<0.01). Table 3 demonstrated the prevalence of three degrees of job burnout among respondents, and the proportion of the burnout case was 61.1%. Pearson correlation analysis illustrated that the GSI of SCL-90 and the dimension scores (except hostility score) were positively correlated with the weighted sum score and the dimension scores of burnout (all P <0.05) (Table 4).
 |
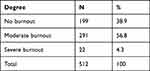 |
Table 3. Prevalence of Job Burnout Among the Nurses |
 |
Table 4. Correlations Between SCL-90 Scores and Job Burnout (Spearman Correlation Coefficient) |
GSI and the Prevalence of Job Burnout Among Nurses with Different Characteristics
As shown in Tables 5 and 6, The differences in GSI and the prevalence of job burnout were statistically significant between nurses working in the frontline of the novel coronavirus in different sites (both P<0.001). Statistical differences were found in GSI and the prevalence of job burnout among nurses with different educational attainment, professional title, working seniority, and the duration of working in the frontline of the novel coronavirus (all P<0.05). Statistical differences were also noted in GSI and the prevalence of job burnout between subjects who had direct contact with COVID-19 patients or their body fluids and specimens and those without contacts (P<0.001). Besides, statistical differences were found in the prevalence of job burnout among nurses of different ages (P<0.001). Given the positive correlation between GSI and the weighted sum score of burnout, we compared GSI among nurses with different job burnout results and found a statistical difference (P<0.001). The difference was also observed in the prevalence of job burnout among subjects with different SCL-90 results (P <0.001).
 |
Table 5. Comparison of GSI in Different Populations (n=512) |
 |
Table 6. Comparison of the Prevalence of Job Burnout in Different Populations (n=512) |
Influencing Factors of Psychological Status
Table 7 demonstrated the generalized linear model indicated the factors influencing the psychological status of nurses working in the frontline of the novel coronavirus included the history of direct contact with COVID-19 patients or their body fluids and specimens, working seniority, and the duration of working in the frontline of the novel coronavirus. A higher GSI (a worse psychological status) was observed for nurses who had direct contact with COVID-19 patients or their body fluids and specimens (B=0.133, 95% CI=(0.067, 0.199), P<0.001) and those with less than five years of working seniority (B=0.133, 95% CI=(0.039, 0.227), P=0.006) or with five to nine years of working seniority (B=0.096, 95% CI=(0.008, 0.184), P=0.033) compared with the nurses without contacts and those with more than 20 years of working seniority, respectively.
A lower GSI (a better psychological status) was noted for nurses working in the frontline of the novel coronavirus for less than 10 days (B=−0.199, 95% CI=(−0.268, −0.0130), P<0.001), 10 to 19 days (B=−0.251, 95% CI=(−0.305, −0.198), P<0.001), or 20 to 29 days (B=−0.202, 95% CI=(−0.253, −0.150), P<0.001) compared with those for more than 30 days.
Risk Factors of Job Burnout
Table 8 demonstrated the risk factors associated with job burnout among nurses working in the frontline of the novel coronavirus. A higher prevalence of job burnout was observed for nurses who had direct contact with COVID-19 patients or their body fluids and specimens (OR=150.95, 95% CI=(44.87,507.77), P<0.001), those with five to nine years of working seniority (OR=8.91, 95% CI=(3.59,22.14), P<0.001), and those working in the frontline of the novel coronavirus for 10 to 19 days (OR=2.63, 95% CI=(1.19,5.82), P=0.017), 20 to 29 days (OR=161.31, 95% CI=(49.48,525.9), P<0.001), or more than 30 days (OR=92.05, 95% CI=(33.88,250.14), P<0.001) compared with the nurses without contacts, those with more than 20 years of working seniority, and those working in the frontline of the novel coronavirus for less than 10 days, respectively.
 |
Table 7. Generalized Linear Model of the Factors Influencing GSI |
 |
Table 8. Risk Factors of Job Burnout by Binary Logistic Regression |
Discussion
In the present study, the prevalence of positive results of SCL-90 among 512 nurses working in the frontline of the novel coronavirus was 49.9%, which was much higher than that (14.1%) reported by Cai et al,11 indicating a bad psychological status. The difference may result from the difference in the research sample. The sample in the study by Cai consisted of health care workers fighting against the COVID-19 in Jiangsu province, including doctors, nurses, technicians, pharmacists, logistical personnel, and social workers, while the subjects of the present study were all nurses working in the frontline of the novel coronavirus in different NAT sites, some of who were from temporary NAT sites in communities/towns in Zhangjiajie city. Working in the frontline of the novel coronavirus in an open-air and high-temperature environment of communities and towns is more painful than working in hospitals.10 The dimension scores in depression, anxiety, hostility, and phobic anxiety among 512 nurses were higher compare with those among Chinese nurses,23 indicating psychological problems of depression, anxiety, hostility, and phobic anxiety. Nursing managers should pay attention to the psychological problems of nurses working in the frontline of the novel coronavirus and take appropriate strategies to improve nurses’ psychological health.
The proportion of the burnout case was 61.1%, which was higher than that (54%) reported by a meta-analysis of 7, 996 nurses working in different health care departments covering 21 epidemiological studies.24 This may be due to the pressure from the risk to be infected with COVID-19. Job burnout would affect work morale, quality of care, patient safety, and health care costs,25 and it is even linked to suicide.26,27 Besides, we found a positive correlation between the physiological status and burnout among nurses, indicating the effect of burnout on psychological health. Thus, interventions need to be implemented immediately to decrease the prevalence of burnout and improve work efficiency among nurses.
We observed a higher GSI for nurses who had direct contact with COVID-19 patients or their body fluids and specimens (B=0.133, 95% CI=(0.067.0.199), P<0.001) compared with those without contacts, which was consistent with that reported by Zhang et al and Deng.12,28 This is not surprising as direct contact with the COVID-19 patients would increase the risk of being infected. The sense of uncertainty and out-of-control caused by the COVID-19 might increase the risk of developing psychological problems. Besides, direct contact with COVID-19 patients or their body fluids and specimens was an independent risk factor of job burnout for nurses (OR=150.95, 95% CI=(44.87,507.77), P<0.001). We did not find similar findings in other studies. Job burnout positively correlated with psychological status, thus, the effect of contact with COVID-19 on job burnout is likely mediated through its impact on the psychological status.
The present study demonstrated that compared with nurses with more than 20 years of working seniority, those with less than five years of working seniority (B=0.133, 95% CI=(0.039, 0.227), P=0.006) and with five to nine years of working seniority (B=0.096, 95% CI=(0.008, 0.184), P-0.033) exhibited a higher GSI, those with five to nine years of working seniority (OR=8.91, 95% CI=(3.59,22.14), P<0.001) showed a higher prevalence of job burnout. The nurses with more than 20 years of working seniority exhibited better psychological status and low lower job burnout, which may be due to the possibility of having rich experience in coping with public health emergencies and high job accomplishment. Cai et al indicated that health care workers with public health emergency experience showed better performance in mental health during the COVID-19.11 Nurses with more than 20 years of work experience are usually mainstays or leaders of the department. This enabled them to have high self-esteem and a sense of accomplishment and low job burnout.
The most significant finding of the present study was that the psychological status and job burnout of nurses were also influenced by the duration of working in the frontline of the novel coronavirus. Compared with nurses who had been working in the frontline of the novel coronavirus for more than 30 days, those who had been working in the frontline of the novel coronavirus for less than 10 days (B=−0.199, 95% CI=(−0.268, −0.130), P<0.001), 10 to 19 days (B=−0.251, 95% CI=(−0.305, −0.198), P<0.001), or 20 to 29 days (B=−0.202, 95% CI=(−0.253, −0.150), P<0.001) exhibited a better psychological status. A higher prevalence of job burnout was observed for nurses who had been working in the frontline of the novel coronavirus for 10 to 19 days (OR=2.63, 95% CI=(1.19,5.82), P=0.017), 20 to 29 days (OR=161.31, 95% CI=(49.48,525.9), P<0.001), or more than 30 days (OR=92.05, 95% CI=(33.88,250.14), P<0.001) compared with those who had been working in the frontline of the novel coronavirus for less than 10 days. These suggest that the risk of psychological problems and job burnout of nurses is increasing with the extension of time spent on working in the frontline of the novel coronavirus. According to the Areas of Worklife (AW) model,29 which explains job burnout in terms of person-job imbalances, job burnout occurs when the imbalances take place in workload, control, reward, community, fairness, and values. In the present study, the continued high workload might be the most relevant factor to explain that the prevalence of job burnout among nurses increased over time.
We initially hypothesized that the nurses from temporary NAT sites in communities/towns in Zhangjiajie city might exhibit a worse psychological status and a lower prevalence of job burnout than those from NAT sites inside hospitals in Zhangjiajie city. The reasons for this hypothesis were as follows: The nurses from temporary NAT sites in communities/towns in Zhangjiajie city were faced with higher workloads and harsh work environment, which may cause more psychological problems and increase job burnout. But we did not find the difference in the psychological status and job burnout between the two groups. The reasons may be that they had a greater sense of control of the situation and higher personal accomplishment. Besides, the public and social media spoke highly of these heroes who put themselves in harm’s way. They were regarded as the most admirable people in the new era. In a word, this finding suggests that the psychological status and job burnout of the two groups of nurses need equal attention.
The present study has some limitations. First, it was limited in scope. All participants were from the NAT sites in Zhangjiajie city, limiting the generalization of our findings to other regions. Besides, a cross-sectional design was applied although the longitudinal research is more conducive to exploring the changes of psychological status and job burnout of nurses. Finally, although the quality control procedure was used throughout the data collection and entry, potential information bias may have occurred given the survey based on self-reported data.
Conclusion
In conclusion, the prevalence of psychological problems (depression, anxiety, hostility, and phobic anxiety) and job burnout were at a high level among nurses working in the frontline of the novel coronavirus. The nurses from temporary NAT sites in communities/towns in Zhangjiajie city and those from NAT sites inside hospitals in Zhangjiajie city had an equal risk of developing psychological problems and job burnout. The factors associated with nurses’ psychological status and job burnout included working seniority, the history of direct contact with COVID-19 patients or their body fluids and specimens, and the duration of working in the frontline of the novel coronavirus. Interventions need to be immediately implemented to promote psychological well-being and decrease job burnout of nurses. Equal attention should be provided to nurses who put themselves in harm’s way to support the temporary NAT sites in communities/towns and those who worked in the frontline of the novel coronavirus inside hospitals in Zhangjiajie city. Besides, special attention should be given to nurses with less than 10 years of working seniority, those who have worked in the frontline of the novel coronavirus continuously for more than 30 days, and those who had direct contact with COVID-19 patients or their body fluids and specimens.
Acknowledgments
We thank all participants. This study was conducted in accordance with the Declaration of Helsinki.
Funding
This study was funded by the Changsha Municipal Natural Science Foundation in Hunan Province, China (grant no: kq2014298), Hunan Provincial Health Commission, China (grant no: 202114050134) and 2021 Xiangya Nursing Discipline High level Scientific Research Project Cultivation Plan (Grant No: 2021xyhlpyjh004).
Disclosure
The authors report no conflicts of interest in this work.
References
1. To KK, Sridhar S, Chiu KH, et al. Lessons learned 1 year after SARS-CoV-2 emergence leading to COVID-19 pandemic. Emerg Microbes Infect. 2021;10(1):507–535. doi:10.1080/22221751.2021.1898291
2. World Health Organization [homepage on the Internet]. WHO Coronavirus (COVID-19) dashboard; 2021. Available from: https://covid19.who.int/.
3. Tianli H, Gan Q, Huang D, et al. The first CT manifestation of patients infected with variant strain Delta of COVID-19. Guangdong Med J. 2021.
4. Aleem A, Akbar Samad AB, Slenker AK. Emerging variants of SARS-CoV-2 and novel therapeutics against coronavirus (COVID-19). In: StatPearls. FL: Treasure Island; 2022.
5. Kumar S, Thambiraja TS, Karuppanan K, et al. Omicron and Delta variant of SARS-CoV-2: a comparative computational study of spike protein. J Med Virol. 2021;94:1641–1649.
6. People’s Network - Hunan channel [homepage on the Internet]. The whole staff of Zhangjiajie city completed nucleic acid detection, sampled 226014 samples, and confirmed 1 local case; 2022. Available from: https://baijiahao.baidu.com/s?id=1706634208250204229&wfr=spider&for=pc.
7. Zhang SX, Liu J, Afshar Jahanshahi A, et al. At the height of the storm: healthcare staff’s health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain Behav Immun. 2020;87:144–146. doi:10.1016/j.bbi.2020.05.010
8. Shen X, Zou X, Zhong X, et al. Psychological stress of ICU nurses in the time of COVID-19. Crit Care. 2020;24(1):200. doi:10.1186/s13054-020-02926-2
9. Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):15–16. doi:10.1016/S2215-0366(20)30078-X
10. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):203976. doi:10.1001/jamanetworkopen.2020.3976
11. Cai W, Lian B, Song X, et al. A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian J Psychiatr. 2020;51:102111. doi:10.1016/j.ajp.2020.102111
12. Zhang WR, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89(4):242–250. doi:10.1159/000507639
13. Jahrami H, BaHammam AS, AlGahtani H, et al. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath. 2021;25(1):503–511. doi:10.1007/s11325-020-02135-9
14. Arshad MS, Hussain I, Nafees M, et al. Assessing the impact of COVID-19 on the mental health of healthcare workers in three metropolitan cities of Pakistan. Psychol Res Behav Manag. 2020;13:1047–1055. doi:10.2147/PRBM.S282069
15. Wu Y, Wang J, Luo C, et al. A comparison of burnout frequency among oncology physicians and nurses working on the front lines and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manage. 2020;60(1):60–65. doi:10.1016/j.jpainsymman.2020.04.008
16. Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale–preliminary report. Psychopharmacol Bull. 1973;9(1):13–28.
17. Wang Z. Symptom Checklist-90. Shanghai Arch Psychiatry. 1984;12(2):68–70.
18. Monteiro F, Canavarro MC, Pereira M. Prevalence and correlates of psychological distress of middle-aged and older women living with HIV. Psychol Health Med. 2017;22(9):1105–1117. doi:10.1080/13548506.2017.1281972
19. Choi YG, Choi BJ, Park TH, et al. A study on the characteristics of Maslach Burnout Inventory-General Survey (MBI-GS) of workers in one electronics company. Ann Occup Environ Med. 2019;31:29. doi:10.35371/aoem.2019.31.e29
20. Li C, Shi K. The impact of distribution equity and procedural fairness on job burnout. Acta Psychol Sin. 2003;35(5):677–684.
21. Xu W, Pan Z, Li Z, et al. Job burnout among primary healthcare workers in rural China: a multilevel analysis. Int J Environ Res Public Health. 2020;17(3):727. doi:10.3390/ijerph17030727
22. Wen J, Cheng Y, Hu X, et al. Workload, burnout, and medical mistakes among physicians in China: a cross-sectional study. Biosci Trends. 2016;10(1):27–33. doi:10.5582/bst.2015.01175
23. Zhang P, Chen L, Song X, et al. Meta-analysis on mental health status of 31294 nurses in mainland china evaluated by SCL- 90 and construction of norm. China J Health Psychol. 2011;19(3):297–300.
24. Zhang YY, Han WL, Qin W, et al. Extent of compassion satisfaction, compassion fatigue and burnout in nursing: a meta-analysis. J Nurs Manag. 2018;26(7):810–819. doi:10.1111/jonm.12589
25. Noseworthy J, Madara J, Cosgrove D, et al. Physician burnout is a public health crisis: a message to our fellow health care CEOs. Health Aff Blog. 2017; 10. doi:10.1377/forefront.20170328.059397.
26. Kuhn CM, Flanagan EM. Self-care as a professional imperative: physician burnout, depression, and suicide. Can J Anaesth. 2017;64:158–168. doi:10.1007/s12630-016-0781-0
27. Stehman CR, Testo Z, Gershaw RS, et al. Burnout, drop out, suicide: physician loss in emergency medicine, part I. West J Emerg Med. 2019;20:485–494. doi:10.5811/westjem.2019.4.40970
28. Deng S. A survey on psychological status of healthcare providers in Yongchuan hospital affiliated to Chongqing Medical University, one of the designated hospitals for novel coronavirus pneumonia. Basic Clin Med. 2020;40(5):601–603.
29. Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15:103–111. doi:10.1002/wps.20311
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

