Back to Journals » Transplant Research and Risk Management » Volume 8
Psychological rejection of the transplanted organ and graft dysfunction in kidney transplant patients
Authors Latos M, Lázár G, Horváth Z, Wittmann V, Szederkényi E, Hódi Z, Szenohradszky P, Csabai M
Received 13 January 2016
Accepted for publication 31 March 2016
Published 29 June 2016 Volume 2016:8 Pages 15—24
DOI https://doi.org/10.2147/TRRM.S104133
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Qing Yi
Melinda Látos,1 György Lázár,1 Zoltán Horváth,1 Victoria Wittmann,1 Edit Szederkényi,1 Zoltán Hódi,1 Pál Szenohradszky,1 Márta Csabai2
1Department of Surgery, Faculty of Medicine, 2Psychology Institute, University of Szeged, Szeged, Hungary
Abstract: Interdisciplinary studies suggest that the mental representations of the transplanted organ may have a significant effect on the healing process. The objective of this study was to examine the representations of the transplanted organ and their relationship with emotional and mood factors, illness perceptions, and the functioning of the transplanted organ. One hundred and sixty-four kidney transplant patients were assessed using the Spielberger Anxiety Inventory, the Beck’s Depression Scale, the Posttraumatic Growth Inventory, the Brief Illness Perception Questionnaire, and the Transplanted Organ Questionnaire. Medical parameters were collected from the routine clinical blood tests (serum creatinine and estimated glomerular filtration rate levels) and biopsy results. Our most outstanding results suggest that kidney-transplanted patients’ illness representations are associated with health outcomes. The Transplanted Organ Questionnaire “psychological rejection” subscale was connected with higher serum creatinine and estimated glomerular filtration rate levels. Logistic regression analysis showed that psychological rejection subscale, Brief Illness Perception Questionnaire, and Posttraumatic Growth Questionnaire total scores were associated with graft rejection. These results may serve as a basis for the development of complex treatment interventions, which could help patients to cope with the bio-psycho-social challenges of integrating the new organ as part of their body and self.
Keywords: anxiety, depression, illness representations, posttraumatic growth, psychological rejection, renal transplantation
Introduction
Interdisciplinary studies suggest that representations of the transplanted organ may have a significant effect on the healing process.1–3 According to research evidence and clinical experience, the transplanted kidney as a “foreign body” may call forth archaic beliefs and reactions, which in turn would cause intrapsychological conflicts about the new organ, and often obstruct the psychological acceptance of the graft.2,4–6 Psychological conflicts about the new kidney may lead to depression and treatment of noncompliance, and thus these are suggested as possible predictors of problems in recovery.7,8
According to the researches, psychotherapeutic intervention was an effective means of addressing emotional problems in recipients of kidney transplants.4,9,10 The most frequent psychological issues as expressed by the patients were fear of rejection, feelings of paradoxical loss posttransplant despite having received a successful transplant, and the psychological integration of the newly acquired kidney.9 Schlitt et al suggested that optimal integration of the graft was less frequent after kidney transplantation, compared with other types of transplantation.11 This might indicate that patients have psychological problems associated with the presence of an organ obtained from another individual. All these unsolved emotional problems can cause serious psychological disturbances or, in some cases, transplant rejection also.2,3,12
The growing awareness that psychological factors can predict posttransplant clinical outcomes (including graft rejection) need to be confirmed by systematic approaches. Some quantitative data are available since the subjective experience of transplanted organ recipients has been investigated.13
Corruble et al realized that no specific questionnaire dedicated to the measurement of the representations of the transplanted organ is available.1 But the foreign organ is a key element of the recipient’s daily life, and these representations are neither spontaneously expressed by patients. Focusing on the transplanted organ may give a complementary and different approach to the field of psychological aspects of transplantation, and this aspect could be relevant in the healing process. The questionnaire developed by Corruble et al aimed at assessing the positive and negative attitude regarding the transplanted organ, concerns about the donor (feelings of gratitude, guilt, and indebtedness), and the transplantation as both a saver and a potential negative phenomenon in the patient’s mind.1
Aims and research questions
The objective of this cross-sectional study is to provide a detailed picture about the representations of the transplanted organ in kidney recipients and their possible correlations with the healing process. The interactions of psychoimmunological mechanisms in these processes are extremely complex. We assumed circular causal connections between psychological variables and kidney functions.
Research questions of the study are the following
- What are the attitudes of patients about the healing process as related to the transplant experience and the representation of the organ?
- Are these representations associated with emotional and mood factors, posttraumatic growth, and illness perceptions? Are there associations between the transplant-related representations and the functioning of the transplant organ?
We hypothesized that the Transplanted Organ Questionnaire (TOQ) “psychological rejection” subscale would be associated with negative emotional and mood factors, lower posttraumatic growth, negative emotional and cognitive illness representations, higher serum creatinine level, and lower estimated glomerular filtration rate (eGFR).
Methods
Study design and population
All materials used in this study (NEP-PSZICH-001) were approved by the Scientific and Research Ethics Committee of the Medical Research Council. Data were collected over a 4-month period from April 2014 to July 2014. The study was conducted on patients who received a cadaver kidney transplant more than 1 year ago in the Department of Surgery. The mean of completion of questionnaires posttransplant was 5.48 years (standard deviation [SD]: 4.33). Each patient was provided with comprehensive information regarding the study and written informed consent was taken. The final sample comprised 164 patients. Ninety-four recipients were males, with a mean age of 50.61 years (SD: 18.54), and 70 were females, with a mean age of 53.84 years (SD: 12.57). Psychological assessments were conducted by a trained health psychologist, blinded to medical data.
Transplanted Organ Questionnaire
The TOQ aimed at assessing feelings of indebtedness, guilt, and gratitude from the recipient toward the donor, the transplantation as both a saver and a negative phenomenon, and the future transplant as both a foreign organ and as a positive element.1 The questionnaire addresses the following three dimensions: the “donor” subscale representing concerns about the donor, the “positive attitude toward the transplant” subscale representing a positive idealization regarding the transplanted organ, and the “psychological rejection” subscale, representing a negative attitude about the transplanted organ.
Spielberger State and Trait Anxiety Inventory
The Spielberger State and Trait Anxiety Inventory (STAIS and STAIT) was administered to measure the level of anxiety after transplantation.21
Beck’s Depression Inventory
Beck’s Depression Inventory (BDI) was used to assess the severity of depressive symptoms.22
Posttraumatic Growth Inventory
We applied the Posttraumatic Growth Inventory (PTGI), which was designed for assessing positive outcomes following a struggle with highly challenging life circumstances.23 The questionnaire comprised five subscales (relating to others, new possibilities, personal strength, spiritual change, and appreciation of life) and a total posttraumatic growth score.
Brief Illness Perception Questionnaire
The Brief Illness Perception Questionnaire (BIPQ) was used to assess the cognitive and emotional representations of illness.24 Five of the items assess cognitive illness representations: consequences, timeline, personal control, treatment control, and identity. Two of the items evaluate emotional representations: concern and emotions. One item assesses illness comprehensibility.
Sociodemographic factors
Sociodemographic background factors are age, sex, marital status, number of children, occupational characteristics, and educational level.
Outcome ascertainment of renal functioning
Medical parameters (serum creatinine level and eGFR) of patients were collected from the routine clinical blood tests after transplantation, at the required control follow-up medical examination to assess allograft outcomes. Serum creatinine (a blood measurement) is an important indicator of renal health because it is an easily measured by product of muscle metabolism that is excreted unchanged by the kidneys (normal range =70–120 μmol/L). The eGFR is used to screen for and detect kidney damage. A normal eGFR level is 60 or more. The lower eGFR number may suggest kidney disease. The eGFR equations are not valid for those who are 75 year of age or older.
Furthermore, we recorded acute rejection episodes after transplantation. Rejection is one of the most common complications, and a statistically significant indicator of poor outcome following a renal transplant.8,25 Graft rejection was diagnosed according to clinical and histopathological criteria.
Statistical analyses
Data were analyzed using IBM SPSS 20.0 for Windows (IBM Corporation, Armonk, NY, USA). Quantitative variables were described using mean and SDs. The Shapiro–Wilk tests were used to analyze for normal or abnormal distribution of the data. To reveal the pattern of relations among the variables, Spearman and Pearson correlation were used. Group comparisons were performed with independent t-test and Mann–Whitney test, one-way analysis of variance or Kruskal–Wallis test. TOQ subscale scores were compared in different subgroups of patients depending on sociodemographic, psychological, and medical variables. Linear regression was used to determine the relationship between graft function (eGFR), illness representations, and psychological rejection. Binary logistic regression analyses (forward method) of psychological variables were performed to detect possible predictors for graft rejection. Results were considered statistically significant when the P-value was <0.05.
Results
Sociodemographic characteristics
The 164 kidney-transplanted patients were 51.99 years old on an average (SD =16.32). Of them, 42.68% were females, 45.73% had a higher secondary or university qualification, and 59.75% became disability receivers.
Depressive and anxiety scores
The BDI score mean was 3.66 (minimum: 0 and maximum: 22). Fourteen (8.53%) patients reported higher depressive scores (BDI score of 10 or more). The median STAIS score was 26, and the mean was 28.54 (minimum: 20 and maximum: 71). The trait anxiety (STAIT) mean score was 30.54, and the median was 28. Seven (4.26%) patients reported anxiety symptoms (STAIT score of 48 or more).
BDI scores correlated with STAIS and STAIT (STAIS Spearman coefficient =0.54, P>0.001; STAIT Spearman coefficient =0.57, P>0.001). We found no differences between males and females on the BDI and STAI scores (BDI P=0.560, STAIS P=0.514; STAIT P=0.241). Low educational levels were significantly associated with state and trait anxiety (STAIS Spearman coefficient =−0.17, P=0.030; STAIT Spearman coefficient =−0.16, P=0.043). No significant association was found between anxiety and depression scales and marital status (P>0.05), age (P>0.05), or number of children (P>0.05) and education level (P>0.05).
TOQ and sociodemographic variables
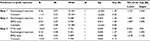
There was no significant difference between males and females on the “positive attitude” and “psychological rejection” subscales (Table 1). “Donor” subscale scores were higher among females (Mann–Whitney test Z=−2.09, P=0.036). “Positive attitude” (Pearson coefficient =0.19, P=0.013) and “donor” subscale (Spearman coefficient =0.24, P=0.001) were reported to correlate with age. No significant association was found between TOQ subscale scores and education level (“donor” P=0.080, “positive attitude” P=0.378, “psychological rejection” P=0.294) and marital status (“donor” P=0.108, “positive attitude” P=0.464, “psychological rejection” P=0.420). We found associations between occupational characteristics and TOQ subscales. Pensioners represented more positive idealization attitude regarding the transplanted organ (“positive attitude” mean: 24.07, SD: 9.34, N=15) than patients who get disability pension (“positive attitude” mean: 15.42, SD: 9.71, N=98) (F=3.77, df=4, P=0.012). Furthermore, pensioners had shown higher scores on the “donor” subscale (mean: 11.53, SD: 8.89), than others who became disability pension receivers (mean: 5.55, SD: 6.48) (C=9.34, df=3, P=0.025) (Table 1).
  | Table 1 Transplanted Organ Questionnaire and sociodemographic variables Abbreviation: df, degrees of freedom. |
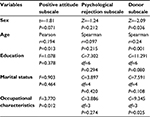
TOQ subscale scores and depressive symptoms, anxiety, illness representations, and posttraumatic growth
The “psychological rejection” subscale scores significantly correlated with the BDI scores and STAI scores (Table 2). The TOQ “positive attitude” subscale significantly correlated with the posttraumatic growth total score and subscales (P<0.005) (Table 2). The “donor” subscale correlated with PTGI total scores and “relating to others”, “personal strength”, “spiritual change”, and “appreciation of life” scales (P<0.005). No significant association was found between “psychological rejection” and PTGI scales (Table 2).
The “positive attitude toward the transplant” subscale was significantly associated with total BIPQ score, identity concern, and emotions scale (Table 3). The “donor” subscale correlated with BIPQ personal control and concern scales. The “psychological rejection” subscale correlated with the BIPQ total score, consequences, treatment control, identity, concern, and emotional representation scale.
  | Table 3 TOQ subscale scores and illness representations Abbreviations: BIPQ, Brief Illness Perception Questionnaire; TOQ, Transplanted Organ Questionnaire. |
TOQ subscale scores and graft functioning
Significant associations of the TOQ subscale scores were found with the medical variables. Patients with higher serum creatinine level (cut point =130 μmol/L − serum creatinine median) had higher scores on the “ psychological rejection” (Mann–Whitney test Z=−3.41, P=0.001) and “donor” subscales (Mann–Whitney test Z=−2.12, P=0.034). No significant association was found between serum creatinine level and “positive attitude” scale (t=−1.36, P=0.175) (Table 4).
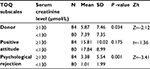  | Table 4 TOQ subscale scores and serum creatinine levels Abbreviations: SD, standard deviation; TOQ, Transplanted Organ Questionnaire. |
The lower level of eGFR (poor kidney function) was significantly associated with the “psychological rejection” subscale (Kruskal–Wallis test P=0.003, χ2 =11.95, df=2) (Table 5). No significant associations were found between eGFR level and “positive attitude” and “donor” scales.
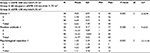  | Table 5 Transplanted Organ Questionnaire and eGFR levels Abbreviations: df, degrees of freedom; eGFR, estimated glomerular filtration rate; min, minimum; max, maximum; SD, standard deviation. |
Posttraumatic growth, mood factors, and graft functioning
Statistical analyses on BDI (C=0.39, df=2, P=0.820), STAIS (C=1.50, df=2, P=0.472), STAIT (C=3.24, df=2, P=0.198), and PTGI (C=3.28, df=2, P=0.257) variables did not reveal any significant effect associated with eGFR levels. However, the “spiritual change” (C=7.43, df=2, P=0.024) and “appreciation of life” scales (C=7.06, df=2, P=0.029) were significantly associated with eGFR levels, which means higher scores on these PTGI scales were associated with higher eGFR level, which indicates better graft functioning. There were no significant connections with the other PTGI scales.
Illness representation and graft functioning status
Analysis of variance revealed the brief IPQ total scores higher among patients showing poor graft functioning (eGFR <30 mL/min/1.73 m2, BIPQ =36.74, F=5.96, df=2, P=0.003) compared with those free of this complication (60 mL/perc > eGFR ≥30 mL/min/1.73 m2, BIPQ =30.07). The “consequences” (C=10.32, df=2, P=0.006) and “emotional representation” scales (C=9.89, df=2, P=0.007) were associated with lower eGFR level.
We expected that stronger personal control beliefs would also be associated with better kidney graft function. The statistical measures indicate that, as hypothesized, higher personal control measured by the brief IPQ was associated with lower serum creatinine level, which indicates better graft function (cut point: serum creatinine level 130 μmol/L, t=2,32, df=154, P=0.021).
Presumed predictors of graft function
To analyze the influence of medical and psychological factors on graft functioning, patients were separated into a “rejection group” (N=55) and a “nonrejection group” (N=109). In the “rejection group”, patients’ biopsy-proved rejection developed after transplantation and their average serum creatinine level value was <180 μmol/L. In the “nonrejection group”, patients did not show apparent signs of rejection and their average serum creatinine level was >180 μmol/L. We compared all measured variables between the two groups: average serum creatinine and eGFR levels, psychological rejection and depression scores, posttraumatic growth total score and three subscales (new possibilities, personal strength, and appreciation of life), BIPQ total score and three subscales (consequences, personal control, and emotional representation) which showed differences (Table 6).
For further investigation, a binary logistic regression analysis was used to identify psychological factors contributing to an increased risk of graft rejection (dependent variable) (Table 7). The logistic regression with forward method among psychological variables identified three main predictors of graft rejection in our sample. The resulting model was statistically significant (χ2=40.42, df=3, P<0.001). The “psychological rejection” subscale (OR=1.27, 95% CI=1.091–1.492, P=0.002), the PTGI total score (OR=0.98, 95% CI=0.964–0.994, P=0.005), and BIPQ total score (OR=1.06; 95% CI=1.018–1.103, P=0.005) were significant predictors of graft rejection episodes after transplantation. This model explained between 23% (Cox and Snell R square) and 32.1% (Nagelkerke R square) of the variance, and correctly classified 67.7 of cases. There were no other significant interactions with other psychological variables.
Discussion
The aim of our cross-sectional study was finding psychological risk factors, which were associated with lower graft function in kidney transplant patients by using quantitative assessment of anxiety, depression, posttraumatic growth, and illness representations. We assumed circular causal connections between psychological variables and kidney functions.
In our results, the TOQ’s “positive attitude” and “donor” subscale scores increased with age, showing more positive attitude toward the transplant and at the same time concern about the donor in older recipients. Females indicated more concerns about the donor than males. Numerous differences between the sexes in illness representations and communication about the illness have been seen in the past decades.26–28 Examination of the correlations between the patients’ education level, marital status, occupational characteristics, and their attitude toward the transplant revealed no significant results.
The TOQ “positive attitude toward the transplant” and “donor” subscales significantly correlated with the posttraumatic growth total score and PTGI subscales, which means positive idealization attitude regarding the transplanted organ and concerns about the donor associated with higher PTGI values. The “positive attitude” subscale was also associated with total BIPQ score, BIPQ identity, concern, and emotional representation scales. The “donor” subscale correlated with BIPQ personal control and concern scales. The “psychological rejection” subscale correlated with the BIPQ total score, consequences, treatment control, identity, concern, and emotional representation scales.
We hypothesized that the TOQ “psychological rejection” subscale would be associated with negative emotional and mood factors, lower posttraumatic growth, negative emotional and cognitive illness representations, higher serum creatinine level, and lower eGFR. In our sample, the “psychological rejection” subscale scores significantly correlated with the BDI scores and STAI scores. Psychological rejection of the transplanted organ was associated with negative illness representations. We expected that stronger personal control beliefs would be associated with higher kidney graft function. Based on a detailed analysis of results, we found that higher personal control (BIPQ score) was associated with lower serum creatinine level, which indicates better graft function, and in the “nonrejection group”, patients also had higher level of personal control.
To analyze the influence of medical and psychological factors on graft functioning, patients were separated into a “rejection group” and a “nonrejection group”. Between the two groups, serum creatinine and eGFR levels, psychological rejection and depression scores, posttraumatic growth total score and three subscales (new possibilities, personal strength, and appreciation of life), BIPQ total score, and three subscales (consequences, personal control, and emotional representation) showed differences. Previous research also suggests that negative mood factors may effect on biological processes and can influence physical health through the complex pathways connecting psychological factors and physical illness. Among kidney transplant patients, depression also appears to play an important role in terms of kidney graft survival and patient mortality.29–32 Dobbels et al found that depression was associated with a twofold increase in risk of graft failure, return to dialysis, and death with a functioning graft.32 Novak et al found that depressed patients were at greater risk of death over the study follow-up compared to nondepressed clients.29 The association between negative mood states and poor clinical outcomes in kidney transplant patients might be explained by several factors, for example, with nonadherence to treatment regimens.33–35 Furthermore, depression in kidney transplant patients is associated with unhealthy behaviors including sedentary lifestyles, lower activity levels, and higher alcohol use, which may be associated with transplant-related outcomes.30
Posttransplant patients must cope with several types of negative emotions, which, in some cases, remain persistent.4,36–38 Consequently, the transplanted organ is not inert at a psychological level; the process of “psychic transplantation” is not able to run its course properly.39 In our sample, the “psychological rejection” (negative attitude about the transplanted organ) was also associated with lower plasma-creatinine level and reduced eGFR value. The lower level of eGFR (poor kidney function) was also significantly associated with negative illness representations (BIPQ). No significant associations were found between eGFR level and “positive attitude” and “donor” subscales, depression, anxiety, and posttraumatic growth scores.
Logistic regression analysis showed that “psychological rejection” scale, BIPQ, and Posttraumatic Growth Questionnaire total scores were associated with graft rejection after transplantation. This result is coherent with our previous data showing that mental representation of the foreign organ could influence the kidney transplantation prognosis.40 These results might have remarkable clinical implications. If the graft is not integrated mentally in the self and body image, the representations of the “foreign body” can be associated with such psycho-neuro-immunological processes, which eventually may have an adverse effect on kidney function.2,5,11 According to Corruble et al, higher TOQ “psychological rejection” subscale was associated with increased risk of death among liver transplant recipients.1
We found that posttraumatic growth may be an important factor in the healing process among kidney-transplanted patients. Despite the growing knowledge of posttraumatic growth, only a minimal amount of research has been conducted on the relationship between posttraumatic growth and physical well-being. For example, heart attack victims who reported psychological growth from traumatic experiences were found to have lower rates of mortality than those who did not perceive any derived benefit.41 Females who reported deriving benefit from traumatic experiences in their lives had quicker cortisol habituation to stressors than those who did not report psychological growth.42 Qualitative analysis revealed that posttraumatic growth might provide additional perspectives for rehabilitation among stroke survivors.43 Researchers also suggested that health care providers might help the recovery of patients by facilitating posttraumatic growth.44,45
In our sample, the illness perceptions were associated with rejection episodes and lower graft functioning. When individuals develop a physical disease, they tend to generate a specific pattern of beliefs and opinions (mental representations) that have the main role of helping them to understand their illness.46 In many chronic diseases, patient’s perception of illness may influence both the susceptibility to complaints and the psychosocial state of health.47 Empirical studies showed that a negative perception of illness is associated with increased risk of death in patients with end-stage renal disease.48–50 A review showed that several domains of the IPQ were associated with higher depression symptoms and noncompliance to treatment.51
Finally, our study has several limitations (small sample size, single-center study). Furthermore, the interactions of psychoimmunological mechanisms in these processes are particularly multifarious. Nevertheless, despite these limitations, our results support the medical relevance of patients’ representations. To explore and correct these attitudes and representations, the use of such psychometric tools such as TOQ may be a useful clinical aid.
Besides the contribution to better understand the complex psychosomatic nature of the transplantation process, our study may also promote the development of supportive techniques, which can enhance recovery in kidney transplant patients.5,52–54 Such a psychosocial intervention could be an effective means of addressing emotional problems (fear of rejection), reduce emotional distress, and improve health behaviors among patients with kidney transplantation.
Acknowledgment
The authors wish to thank Rózsa Havancsák for her valuable help.
Author contributions
ML, MC, ES, and GL designed the protocol; ML, ZH, PS, and ZH collected and analyzed the data; ML, VW, and MC interpreted the data and wrote the article. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Corruble E, Barry C, Varescon I, Castaing D, Samuel D, Falissard B. The Transplanted Organ Questionnaire: a validation study. J Psychosom Res. 2012;73:319–324. | ||
Fukunishi I. Psychosomatic problems surrounding kidney transplantation. Psychother Psychosom. 1992;57:42–49. | ||
Mai FM, McKenzie FN, Kostuk WJ. Psychiatric aspects of heart transplantation: preoperative evaluation and postoperative sequelae. Br Med J. 1986;292(6516):311–313. | ||
Consoli E. Person-centered approach in the medicine of organ transplants; 2012. Available from: http://www.psicoanalisi.it/psicoanalisi/osservatorio/articoli/osservaing1132.htm. | ||
Ilić S, Avramović M. Psychological aspects of living donor kidney transplantation. Med Biol. 2002;9:195–200. | ||
Shimazono Y. Accommodating a “foreign” organ inside the body: post-transplant bodily experiences of Filipino kidney recipients. Ars Vivendi J. 2013;3:24–50. | ||
Achille MA, Ouellette A, Fournier S, Vachon M, Hébert MJ. Impact of stress, distress and feelings of indebtedness on adherence to immunosuppressants following kidney transplantation. Clin Transplant. 2006;20:301–306. | ||
Dickenmann MJ, Nickeleit V, Tsinalis D, Gürke L, Mihatsch MJ, Thiel G. Why do kidney grafts fail? A long-term single-center experience. Transpl Int. 2002;15:508–514. | ||
Baines LS, Joseph JT, Jindal RM. Emotional issues after kidney transplantation: a prospective psychotherapeutic study. Clin Transplant. 2002;16:455–460. | ||
Schulz K, Kroencke S. Psychosocial challenges before and after organ transplantation. Transpl Res Risk Manag. 2015:7:45–58. | ||
Schlitt HJ, Brunkhorst R, Schmidt HHJ, Nashan B, Haverich A, Raab R. Attitudes of patients before and after transplantation towards various allografts. Transplantation. 1999;68:510–514. | ||
Abram HS, Buchanan DC. The gift of life: a review of the psychological aspects of kidney transplantation. Int J Psychiatry Med. 1976;7:153–164. | ||
Grady KL, Jalowiec A. Predictors of compliance with diet 6 months after heart transplantation. Heart Lung. 1995;24(5):359–368. | ||
Lough ME, Lindsey AM, Shinn JA, Stotts NA. Impact of symptom frequency and symptom distress on self-reported quality of life in heart transplant recipients. Heart Lung. 1987;16:193–200. | ||
De Geest S, Borgermans L, Gemoets H, et al. Incidence, determinants, and consequences of subclinical non-compliance with immunosuppressive therapy in renal transplant recipients. Transplantation. 1995;59(3):340–347. | ||
Fife BL, Huster GA, Cornetta KG, Kennedy VN, Akard LP, Broun ER. Longitudinal study of adaptation to the stress of bone marrow transplantation. J Clin Oncol. 2000;18:1539–1549. | ||
Schlebusch L, Pillay BJ, Louw J. Body-image differences in live related and cadaver renal transplant recipients. S Afr J Psychol. 1992;22:70–75. | ||
Hayward MB, Kish JP Jr, Frey GM, Krichner M, Carr LS, Wolfe CM. An instrument to identify stressors in renal transplant recipients. Nephrol Nurs J. 1989;16(2):81–85. | ||
Wirth PH, Barton CF. An instrument to measure self-care principles of renal transplant recipients. Nephrol Nurs J. 1985;12(13–14):353–356. | ||
Ziegelmann JP, Griva K, Hankins M, et al. The Transplant Effects Questionnaire (TxEQ): The development of a questionnaire for assessing the multidimensional outcome of organ transplantation – example of end stage renal disease (ESRD). Br J Health Psychol 2002;7:393–340. | ||
Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. | ||
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4(6):561–571. | ||
Tedeschi R, Calhoun L. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress. 1996;9:455–471. | ||
Broadbent E, Petrie KJ, Main J, Weinman J. The Brief Illness Perception Questionnaire. J Psychosom Res. 2006;60:631–367. | ||
Nankivell BJ, Alexander SI. Rejection of the kidney allograft. N Engl J Med. 2010;363:1451–1462. | ||
Glynn LM, Christenfeld N, Gerin W. Gender, social support, and cardiovascular responses to stress. Psychosom Med. 1999;61(2):234–242. | ||
Grace SL, Krepostman S, Brooks D, et al. Illness perceptions among cardiac patients: relation to depressive symptomatology and sex. J Psychosom Res. 2005;59(3):153–160. | ||
Scholz U, Klaghofer R, Dux R, et al. Predicting intentions and adherence behavior in the context of organ transplantation: gender differences of provided social support. J Psychosom Res. 2012;72(3):214–219. | ||
Novak M, Molnar MZ, Szeifert L, et al. Depressive symptoms and mortality in patients after kidney transplantation: a prospective prevalent cohort study. Psychosom Med. 2010;72:527. | ||
Zelle DM, Dorland HF, Rosmalen JG, et al. Impact of depression on long-term outcome after renal transplantation: a prospective cohort study. Transplantation. 2012;94(10):1033. | ||
Rocha G, Poli de Figueiredo CE, d’Avila D, Saitovitch D. Depressive symptoms and kidney transplant outcome. Transplant Proc. 2001;33:3424. | ||
Dobbels F, Skeans MA, Snyder JJ, Tuomari AV, Maclean JR, Kasiske BL. Depressive disorder in renal transplantation: an analysis of Medicare claims. Am J Kidney Dis. 2008;51:819. | ||
Jindal RM, Joseph JT, Morris MC, Santella RN, Baines LS. Noncompliance after kidney transplantation: a systematic review. Transplant Proc. 2003;35:2868. | ||
Jindal RM, Neff RT, Abbott KC, et al. Association between depression and nonadherence in recipients of kidney transplants: analysis of the United States renal data system. Transplant Proc. 2009;41:3662. | ||
Gorevski E, Succop P, Sachdeva J, et al. Is there an association between immunosuppressant therapy medication adherence and depression, quality of life, and personality traits in the kidney and liver transplant population? Patient Prefer Adherence. 2013;7:301. | ||
Achille MA, Oullette A, Fournier S, Hebert MJ, Girardin C, Paquet M. Impact of transplant-related stressors and feelings of indebtedness on psychosocial adjustment following kidney transplantation. J Clin Psychol Med Settings. 2004;11:63–73. | ||
Kaba E, Thompson DR, Burnard P, Edwards D, Theodosopoulou E. Somebody else’s heart inside me: a descriptive study of psychological problems after a heart transplantation. Issues Ment Health Nurs. 2005;26:611–625. | ||
Pérez-San-Gregorio MA, Martín-Rodriquez A, Díaz-Dominiquez R, Pérez-Bernal J. The influence of posttransplant anxiety on the long-term health of patients. Transplant Proc. 2006;38:2406–2408. | ||
De Pasquale C, Pistorio ML, Sorbello M, et al. Body image in kidney transplantation. Transplant Proc. 2010;42:1123–1126. | ||
Látos M, Devecsery Á, Horváth Z, et al. The role of body image integrity and posttraumatic growth in successful organ transplantation: a 3-year longitudinal study of kidney transplant patients. Health Psychology Open. 2015;2(1):1–8. | ||
Epel ES, McEwen BS, Ickovics JR. Embodying psychological thriving: physical thriving in response to stress. J Soc Issues. 1998;54:301–322. | ||
Bower JE, Kemeny ME, Taylor SE, Fahey JL. Cognitive processing, discovery of meaning, CD4 decline, and AIDS-related mortality among bereaved HIV-seropositive men. J Consult Clin Psychol. 1998;66:979–986. | ||
Kauenemund A, Zwick S, Rief W, Exner C. (Re-)defining the self-enhanced posttraumatic growth and event centrality in stroke survivors: a mixed-method approach and control comparison study. J Health Psychol. 2014;21(5):679–689. | ||
Schmidt SD, Blank TO, Bellizzi KM, Park CL. The relationship of coping strategies, social support, and attachment style with posttraumatic growth in cancer survivors. J Health Psychol. 2014;17:1033–1040. | ||
Wang Y, Wang Y, Liu X. Posttraumatic growth of injured patients after motor vehicle accidents: an interpretative phenomenological analysis. J Health Psychol. 2012;17:297–308. | ||
Skelton JA, Croyle RT. Mental Representation in Health and Illness. New York: Springer-Verlag; 1991. | ||
Scharloo M, Kaptein AA, Weinman J, et al. Illness perceptions, coping and functioning in patients with rheumatoid arthritis, chronic obstructive pulmonary disease and psoriasis. J Psychosom Res. 1998;44(5):573–585. | ||
van Dijk S, Scharloo M, Kaptein AA, et al. Dekker for the NECOSAD Study Group. Patients’ representations of their end-stage renal disease: relation with mortality. Nephrol Dial Transplant. 2009;24(10):3183–3185. | ||
Kimmel PL, Peterson RA, Weihs KL, et al. Dyadic relationship conflict, gender, and mortality in urban hemodialysis patients. J Am Soc Nephrol. 2000;11(8):1518–1525. | ||
Chilcot J, Wellsted D, Farrington K. Illness perception predict survival in hemodialysis patients. Am J Nephrol. 2011;33(4):358–363. | ||
Chilcot J. The importance of illness perception in end-stage renal disease: associations with psychosocial and clinical outcomes. Semin Dial. 2012;25:59–64. | ||
García-Llana H, Barbero J, Olea T, et al. Incorporation of a psychologist into a nephrology service: criteria and process. Nefrologia. 2010;30(3):297–303. | ||
Nilsson M, Persson L, Forsberg A. Perceptions of experiences of graft rejection among organ transplant recipients striving to control the uncontrollable. J Clin Nurs. 2007;17:2408–2417. | ||
Rodrigue JR, Mandelbrot DA, Pavlakis M. A psychological intervention to improve quality of life and reduce psychological distress in adults awaiting kidney transplantation. Nephrol Dial Transplant. 2011;26:709–715. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.