Back to Journals » Clinical Ophthalmology » Volume 16
Pseudophakia and Lens Opacities in 70-Year-Olds in Gothenburg, Sweden; Gender Differences, Impact on Self-Reported Visual Function and Validation of Self-Reported Cataract and Pseudophakia
Authors Nordström M , Holm M, Havstam Johansson L, Rydberg Sterner T, Ahlner F, Falk Erhag H , Skoog I, Zetterberg M
Received 21 March 2022
Accepted for publication 15 July 2022
Published 10 October 2022 Volume 2022:16 Pages 3269—3281
DOI https://doi.org/10.2147/OPTH.S366897
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 8
Editor who approved publication: Dr Scott Fraser
Moa Nordström,1,2 Mathias Holm,3 Lena Havstam Johansson,1,2 Therese Rydberg Sterner,4 Felicia Ahlner,4 Hanna Falk Erhag,4 Ingmar Skoog,4,5 Madeleine Zetterberg1,2
1Department of Clinical Neuroscience, Institute of Neuroscience and Physiology, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 2Department of Ophthalmology, Sahlgrenska University Hospital, Mölndal, Sweden; 3Department of Occupational and Environmental Medicine, School of Public Health and Community Medicine, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 4Department of Psychiatry and Neurochemistry, Institute of Neuroscience and Physiology, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 5Department of Psychiatry Cognition and Old Age Psychiatry, Sahlgrenska University Hospital, Mölndal, Sweden
Correspondence: Moa Nordström, Department of Ophthalmology, Sahlgrenska University Hospital, Mölndal, SE-431 80, Sweden, Tel +46 31 342 10 00, Fax +46 31 41 29 04, Email [email protected]
Purpose: The study aimed at determining the prevalence and sex differences in cataract, pseudophakia, lens opacities and self-reported cataract in 70-year-old people in Gothenburg, Sweden. The purpose was also to identify correlations between lens opacities, visual acuity and subjective visual function, and to validate self-reported cataract and cataract surgery.
Patients and Methods: Population-based cross-sectional study where participants (n=1182) answered questions about self-reported diagnosis of cataract and cataract surgery. A total of 1139 subjects completed the National Eye Institute Visual Functioning Questionnaire‐25 (NEI VFQ‐25), 560 subjects underwent ophthalmic examination including visual acuity and lens photography. t-test, Pearson chi-square and Mann–Whitney U-test were used for obtaining p-values. ANOVA (analysis of variances, Kruskal–Wallis, one-way) was used to compare VFQ-25 between 3 groups; no cataract, cataract and pseudophakia. To clarify the differences between specific pairs of groups post-hoc test (Bonferroni) was used after ANOVA.
Results: Self-reported cataract was more common in women than in men (27.2% vs 19.1%, p=0.001, chi-square). Cataract surgery was reported by 16.3% of women and 12.6% of men (p=0.072). Upon eye examination, the prevalence of pseudophakia was 16.9% in women compared to 10.2% in men (p=0.020). The prevalence of cataract, including pseudophakia, was 31.9% in women versus 23.8% in men (p=0.033). Significant correlations (Spearman’s rho) were found between lens opacities and visual acuity. Self-reported cataract surgery showed a very high specificity and high sensitivity. The composite score from NEI VFQ‐25 was lower in people with pseudophakia than in people with/without cataract (p=0.012, Kruskal–Wallis).
Conclusion: The prevalence of cataract including pseudophakia in 70-year-olds in Gothenburg is higher compared to previous studies in similar geographical areas. Also, it is more common in women than in men. The lack of significant sex differences in lens opacities may be due to cataract surgery at an earlier stage. Validation showed very good agreement between pseudophakia and self-reported cataract surgery.
Keywords: cataract, cataract surgery, cross-sectional study, gender differences, lens opacities, vision-related quality of life
Introduction
Globally, cataract is the major cause of blindness. Out of the 36 million who are blind worldwide, 35% is caused by cataract.1 In Sweden, the annual number of cataract extractions have steadily increased from 2014 until 2019, when the number of cataract surgeries were 139,665 according to the Swedish National Cataract register.2 In 2020, the number of cataract extractions decreased to 121 310, most likely due to the Covid-19 pandemic.3 For many years now, cataract extraction has been the most common surgical procedure in Sweden. More women than men have cataract surgery, but the proportion of women going through cataract extractions have gradually decreased since 2000, and the percentage in 2020 was 56%.3 Mean age at the time of surgery has decreased since 1999, resulting in a mean age of 73 years in 2020, and visual acuity at the time of surgery has gradually increased.
Epidemiological studies in ophthalmology are important for future planning of health care, for the comparison of disease burden and number of cataract extractions over time, as well as for further investigations of risk factors for the development of cataract. Updated information will provide increased knowledge within health care and society, for care recipients and care providers. Local studies are valuable because the prevalence may vary due to different risk factors in different populations thus affecting the prevalence of cataract and cataract surgery. Studies from several countries, including Sweden, have shown that the prevalence of lens opacities is higher in women than in men.4–7 Our study aimed to investigate if this is still the case, and to relate the results to the decreasing proportion of women undergoing cataract extractions, and to explore if there is inequality in access to health care.
The objective of this study was to determine updated sex-specific prevalence of cataract based on assessment of pseudophakia and lens opacities in 70-year-old people in the Gothenburg area in Sweden and relate these results to self-reported cataract. The study also aimed at exploring correlations between lens opacities, visual acuity and self-reported visual function using the National Eye Institute Visual Function Questionnaire (NEI VFQ-25) and the Rasch-based scoring algorithm National Eye Institute Visual Functioning Questionnaire 28 (NEI-VFQ-28R). Furthermore, the study aimed at investigating if there is conformity between self-reported cataract or pseudophakia, and diagnosis of cataract or pseudophakia as evaluated through examination, which is relevant for future studies exploring self-reported cataract and self-reported cataract surgery.
Materials and Methods
Participants
The Gothenburg H70 Birth Cohort Study is a population-based cross-sectional study, which started in 1971, investigating normal and pathological aging in older populations.8 In the Gothenburg H70 Birth Cohort Study of 2014–2016, 70-year-olds born in 1944 on specific dates (dates ending with 0, 2, 5 or 8) were selected from the Swedish Population Register.9 Inclusion criteria were living in the urban area of Gothenburg and being able to communicate in Swedish. A total of 1182 individuals (633 women, 549 men) answered questions on cataract surgery, cataract diagnosed by an ophthalmologist or optician, age-related macular degeneration or diabetic eye disease diagnosed by an ophthalmologist, previous laser surgery for diabetic eye disease and present or previous treatment for glaucoma. A total of 1139 individuals (614 women, 525 men) completed the National Eye Institute Visual Function Questionnaire (NEI VFQ-25).9,10
From the cohort of 1203, a subsample of 631 participants, born on days ending with 0, 2, 5 and 8 (born in January–April), and 5 and 8 (born in May–December), were invited for an ophthalmic examination conducted at Sahlgrenska University Hospital, Mölndal. Of those invited, 560 completed the ophthalmological examination; 295 were women (52.7%), and 265 were men (47.3%). Further details on the recruitment of participants can be found in a study by Havstam Johansson et al.9 The ophthalmological examination was conducted in 2014–2015 by specially trained ophthalmologic nurses and included, among other things, best corrected visual acuity (BCVA) using the Early Treatment Diabetic Retinopathy Study Chart (ETDRS),11 lens and fundus photographs taken after pupil dilatation with eyedrops containing cyclopentolate 0.85% and phenylephrine 1.5%. Lens photographs were slit-lamp images for grading nuclear color and nuclear opacities, and retroillumination images for grading cortical cataract and posterior subcapsular cataract. The fundus photograph comprised the posterior pole.
Ethics Approval and Consent to Participate
The study was approved by the Regional Ethical Review Board (Dnr 869–13, 127–14). The study was performed in accordance with the tenets of the Declaration of Helsinki and written informed consent was obtained from all participants. All participants gave consent for publication of data.
Procedure
Lens opacities were graded in the right eye, independently from the lens photographs by two ophthalmologists, using Lens Opacities Classification System (LOCS) III, which is an established and wide-spread method for grading lens opacities. LOCS II was updated to LOCS III in 199312 and consists of six slit-lamp images for grading nuclear color (NC) and nuclear opalescence (NO) and five retroillumination images for grading cortical cataract (CC) and posterior subcapsular cataract (PSC). NO and NC were graded from 0.1–6.9 with 0.1-unit intervals and CC and PSC were graded from 0.1–5.9 with 0.1-unit intervals. One resident in ophthalmology and one professor of ophthalmology assessed the LOCS grading independently. In cases where the difference in grading was more than one unit, the resident re-assessed the cases, and an average was calculated. Not all photographs could be assessed regarding lens opacities because of the quality of the photographs; 0.7–1.1% of the photographs depending on type of lens opacity. If data was missing according to either of the observers the other observer’s data was used.
In the Skövde Cataract study,6 which was implemented in a geographical area close to the Gothenburg area, the definition of cataract was converted from a definition according to LOCS II in the Eye Diseases Prevalence Research group13 into LOCS III, and the definition of cataract was one or more of the following in either eye: PSC>1, CC>3 and/or NO≥4. This definition was also used in the present study. In some analyses, pseudophakia was included in the definition of cataract. To determine interrater reliability, the degree of agreement among raters, Cohen’s κ was calculated. Sensitivity, specificity, positive predictive values and negative predictive values of self-reported cataract and self-reported cataract surgery were calculated by comparing the questions “Have you ever been diagnosed with cataract by an ophthalmologist or optician?” and “Have you ever had cataract surgery?” with cataract and pseudophakia as diagnosed from the lens photographs. Smoking was defined as self-reported ever smoker, diabetes as self-reported type 1 or type 2.
NEI VFQ-25 has been widely used in ophthalmological research and consists of 25 questions which are grouped into 12 subscales: general vision, ocular pain, near vision, distance vision, social functioning, role limitations, dependency, mental health, driving, peripheral vision, color vision and a single general health question. Its purpose is to assess influence of visual impairment on health-related quality of life.14 Each subscale is scored from 0–100 where 0 represent the worst possible and 100 is the best possible self-reported vision-targeted quality of life.15
Rasch measurement theory analysis has been used for transformation of questionnaire data to a continuous scale, thus enabling parametric statistical analysis. Rasch analyses of VFQ-25 have resulted in the Rasch-based scoring algorithm for the National Eye Institute Visual Functioning Questionnaire 28 (NEI-VFQ-28-R). In NEI-VFQ-28-R, the items are grouped into two broad domains; Activity Limitations (AL) with 19 items where 7 are additional, and Socio-Emotional Functioning (SEF) with 9 items, and a total score. 1139 participants answered VFQ-25 and the answers were converted into a Rasch-based score, according to the manual by Petrillo.16 The additional questions were not used. VFQ-25 and NEI-VFQ-28-R scores were assessed for participants with no cataract, cataract and pseudophakia based on findings from the eye examination. The group with no cataract included bilaterally phakic people with no significant lens opacities. The group with cataract included people with lens opacities in either eye according to the definition of cataract. The pseudophakic group included people with pseudophakia in both eyes or pseudophakia in one eye but no significant lens opacities in the fellow eye. If pseudophakia in one eye and significant lens opacities in the other eye the participant was included in the cataract group. If data was missing in one eye, the lens status of the other eye was used.
Statistics
A power-analysis was performed based on gender differences in self-reported cataract. Using an effect size of 10% between genders, an a-error probability of 5% and a power (1-b-error) of 80%, a desired total sample size of 622 subjects was obtained. Thus, the actual total sample size of 1182 participants was judged as sufficient. t-test, Pearson Chi-square and Mann–Whitney U-test were used for obtaining p-values. Results from LOCS gradings and vision-related quality of life are presented as median with interquartile range (IQR) and mean with standard deviation (SD). Cohen’s κ was calculated in order to determine interrater reliability. According to Landis and Koch, κ-values of 0.41–0.60 constitute moderate agreement and 0.61–0.80 is referred to as substantial agreement.17 Logistic regression, using a backwards stepwise approach, was used for analyzing the impact of sex, diabetes and smoking, on cataract and cataract extraction. ANOVA (Analysis of Variances) (Kruskal–Wallis, One-way) was used comparing VFQ-25 and Rasch analysis between 3 groups; no cataract, cataract and pseudophakia. To clarify the differences between specific pairs of groups, the post-hoc test Bonferroni was used after the ANOVA-test. All statistical analysis were performed using version 25.0 of IBM SPSS Statistics for Macintosh (IBM Corp, Armonk, NY, USA) except for power-analysis for which the free-to use software G*power (Heinrich Heine Universität Düsseldorf, Version 3.1.9.6) was used. P-values of <0.05 were considered statistically significant.
Results
The prevalence of self-reported cataract as diagnosed by an ophthalmologist or optician was 23.4%; 27.2% in women compared to 19.1% in men (p=0.001, chi-square), see Table 1. The prevalence of self-reported cataract surgery was 14.6%; 16.3% in women versus 12.6% in men (p=0.072). When excluding participants stating cataract surgery from participants stating cataract diagnosis, the number decreased to 9.0%; 11.1% in women compared to 6.6% in men (p=0.007). All, except one, who stated having had cataract surgery also stated having cataract diagnosed by an ophthalmologist or optician.
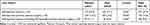 |
Table 1 Prevalence of Self-Reported Diagnosis of Cataract and Previous Cataract Surgery 1182 70-Year Old People in Sweden Answered Questions About Cataract Diagnosis and Previous Cataract Surgery |
Out of the 560 examined subjects, 13.8% were pseudophakic in at least one eye; 16.9% of the women vs 10.2% of the men, p=0.020, see Table 2. Among women, 31.9% had cataract including pseudophakia in at least one eye, compared to 23.8% in men (p=0.033, chi-square). The prevalence of cataract, excluding pseudophakia, was 14.9% in women and 13.6% in men.
 |
Table 2 Pseudophakia and Lens Opacities in Swedish 70-Year Olds; Gender Differences |
The odds-ratio for women compared to men for pseudophakia was 1.91 (95% confidence interval [CI] 1.15–3.16; p=0.012). The odds-ratio for women having cataract in either eye (including pseudophakia) was 1.46 (95% CI 1.00–2.12; p=0.051).
Logistic regression showed that even after adjustment for smoking and diabetes, female gender was still a significant risk factor for cataract and cataract surgery, see Table 3.
 |
Table 3 Logistic Regression of Possible Predictors for Cataract and Cataract Surgery in 70-Year Old People |
Grading lens opacities in the right eye showed that the mean of NO was 2.22 (SD 0.67), NC 1.97 (0.69), CC 1.17 (0.96) and PSC 0.25 (0.41). There were no significant sex differences in type of lens opacities. Grading of lens opacities had an inter-rater reliability (κ value) of 0.60 for NO ≥2, 0.62 for NC≥2, 0.56 for CC ≥2 and 0.64 for PSC ≥1.
When comparing self-reported cataract surgery with lens photographs, self-reported cataract surgery had a sensitivity of 90.7% (95% CI 82.0–95.4%), a specificity of 99.2% (95% CI 97.9–99.7%), a positive predictive value (PPV) of 0.944 (95% CI 0.866–0.978) and a negative predictive value (NPV) of 0.986 (95% CI 0.970–0.993). Self-reported cataract, as diagnosed by an ophthalmologist or optician, had a sensitivity of 52.9% (95% CI 45.1–60.7%), a specificity of 92.3% (95% CI 89.2–94.5%), a PPV of 0.730 (95% CI 0.641–0.804) and an NPV of 0.832 (95% CI 0.794–0.865). The prevalence of self-reported cataract and cataract surgery in the group who had eye examination was approximate to the prevalence in the whole group; 20.9% versus 23.4% and 13.0% versus 14.6%.
Best-corrected visual acuity (BCVA) was lower in participants with cataract, defined as lens opacities according to the definition of cataract, than without cataract. In the right eye, median ETDRS score was 83.00 letters (IQR 79.00–87.50) compared to 87.00 letters (83.00–90.00) (p<0.001 Mann–Whitney U-test), see Table 4.
 |
Table 4 Best Corrected Visual Acuity (BCVA) in Participants with and without Cataract |
The pseudophakic group had significantly lower self-reported vision-related quality of life according to VFQ-25 and NEI-VFQ-28-R compared to the groups without cataract (bilateral phakia and no cataract), or with lens opacities defined as cataract, in the following subscales: general health, general vision, ocular pain, distance vision, composite overall score, Rasch activity limitations, Rasch total, see Table 5.
Post-hoc test (Bonferroni) showed that the differences in general health (p=0.013), general vision (p=0.035), distance activities (p=0.046), ocular pain (p=0.055) and composite overall score (p=0.084) were between the groups with no cataract and pseudophakia. When the participants with self-reported other eye disease were excluded the significant differences between the groups with different lens status disappeared, see Supplemental Table 1. 19.5% of people with pseudophakia had self-reported other eye-diseases compared to 8.8% (p= 0.053, chi-square) of people with cataract, and 6.2% (p<0.001) in people without cataract or pseudophakia.
There were significant correlations (Spearman’s rho) between visual acuity and NO, NC, CC and PSC (Figures 1–4), where higher lens gradings were correlated with lower visual acuity. For men, there was a significant correlation between NO, NC and PSC and BCVA but for women there was only a significant correlation between CC and BCVA.
There were significant correlations between NC and impaired peripheral vision (Spearman’s rho −0.154 p=0.01), distance vision (−0.137, p=0.002), social functioning (−0.090, p= 0.046), role limitations (−0.127, p=0.005), composite overall score (−0.107, p=0.018), Rasch activity limitations (−0.094, p=0.038), Rasch socio-emotional functioning (−0.108, p=0.016), Rasch total (−0.107, p=0.018), and between NO and distance vision (−0.111, p=0.014). There were borderline significant correlations between NO and peripheral vision (Spearman’s rho −0.088, p=0.051).
Discussion
There is no global definition of cataract and in various epidemiological studies diverse lens grading scales and cut-offs have been used, often including pseudophakia and aphakia, and occasionally including visual acuity.5–7,18 This diversity can affect the accuracy when comparing the prevalence of cataract between different epidemiological studies.
LOCS III is one of the most common lens grading scales, and has been evaluated using objective methods of measuring lens opacities. Correlations between objective scatter index and nuclear, cortical and posterior subcapsular cataract have been found, using the double-pass Optical Quality Analysis System.19 A linear increase between lens density as measured with the Pentacam Scheimpflug system and LOCS III score has been ascertained,20 and the correlations between nuclear opalescence and objective scatter index and lens density have been confirmed in another study.21 These analyses, using objective methods to quantify lens opacities and correlating them to LOCS-III, justify the use of a parametric statistical approach when analyzing LOCS-data.
In the Beaver Dam Eye Study, conducted in 1988–1990, the prevalence of cataract at the age of 65–74 years was 23.5% in women and 14.3% in men, and the prevalence of pseudophakia was 3.6%.22 In the Blue Mountains Eye Study,5 conducted in 1992–1994, the prevalence of cataract in age 65–74 years was 23.6% in women and 19.1% in men, and the prevalence of pseudophakia was 5.8% in women and 6.3% in men. The prevalence of cataract in the same age group in a Finnish study in 2000–2001 was 22.1%, more common in women than men, and unoperated cataract was more common in women than men.23 These studies showed a lower prevalence of pseudophakia and cataract than in the present study, which can be explained by the increase in cataract surgeries in recent years.
Since increasing age is the most important factor for the development of cataract the comparisons of prevalence of cataract need to match the age of the participants.
In the Skövde Cataract study, the prevalence of cataract, including pseudophakia, at the age 70–74 years, was 23% in women and 21.5% in men.6 The prevalence of pseudophakia was 9% in women and 9.5% in men, and women had significantly higher levels of NO, NC and CC in all age groups. Among people aged 75–79 years and for the total group of 70–84 years, women had significantly higher prevalence of cataract. When including pseudophakia women had significantly higher prevalence in the group aged 75–79 years, 80–84 years and in the total group. In our study, the prevalence of cataract, including pseudophakia, was higher than in the Skövde Cataract study, especially in women, which can be due to a higher prevalence of pseudophakia in our study. The lens opacities were more severe in the Skövde Cataract Study in all cataract types, except for CC in men, which can be due to higher age in the participants. The increase in number of cataract surgeries, from 72´568 in 2006,24 to 114´598 in 201425 combined with surgery at an earlier stage, when the visual acuity is higher and the lens opacities are less severe may explain the lower grade of lens opacities, and the higher prevalence of pseudophakia in our study, compared to the Skövde Cataract Study.
To use several assessors for the estimation of lens opacities is likely to increase the quality of the outcome. Interrater reliability in our study was in the moderate-substantial range. In the Beaver Dam Eye study, κ values were in the substantial range (0.65–0.75) for all cataract types.26 In a study in Singapore, κ values between three observers were in the moderate range (0.41–0.60) initially and increased to substantial (0.61–0.80) after a standardization process.27
Self-reported cataract surgery has a high sensitivity and very high specificity in our study, matching numbers from the Los Angeles Latino Study.28 Since cataract surgery in Sweden in recent years has been performed at earlier stages, cataract surgery could perhaps be used as a surrogate marker for clinically relevant cataract, particularly since the access to cataract surgery is good. The disadvantage of this approach is that the type of lens opacity is not diagnosed.
In the current study, self-reported diagnosis of cataract had a sensitivity of only 53% and a specificity of 92%. Other studies have shown similar or lower sensitivity and specificity,28–30 including a study by Bowie which concluded that cataract surgery can be estimated with a questionnaire, but it is less accurate concerning cataract status, matching our conclusion.
The present study confirms that cataract, including pseudophakia, is more common in women than in men which confirms the findings in other studies.7,31 Earlier studies have shown a higher level of cortical and nuclear opacities in women than in men4,5,7 whereas in our cohort women had only slightly higher gradings in NO and NC than men.
The difference in pseudophakia between men and women is in accordance with previous studies, where the prevalence of cataract and pseudophakia is higher in women than men.7,31,32 Logistic regression confirmed that female gender is a predictor for cataract and cataract surgery.
With an increasing number of cataract extractions in Sweden, from a number of 73´513 in 2001 to 139´665 in 2019, an increase in pre-operative visual acuity from 0.3 (decimal) in 2001 to 0.5 in 2019 was seen, paralleled by a decrease in the proportion of women from 66.1% in 2001 to 58.4 in 2019.2,33 The gender differences in lens opacities that were previously seen have disappeared, whereas the prevalence of pseudophakia in women have increased. That the proportion of women going through cataract extractions have decreased in recent years may be explained by the dramatic increase in the total number of cataract extractions. The improvement in access to surgery have increased substantially for the majority of patients, in which the majority are women, who in earlier years had to wait longer for surgery.
That women have a higher prevalence of cataract than men can have different possible explanations: estrogens are thought to have anti-oxidative properties and protective effects against cataract, but when estrogen levels are dramatically reduced at menopause, the risk of developing cataract increases, i.e a withdrawal-effect.34,35
The participants showed good BCVA and high scores at VFQ-25 which may reflect good access to health care and surgery, also demonstrated by the high prevalence of pseudophakia. There have been concerns whether NEI VFQ-25 measures what it is intended to measure, and concerns that the questionnaire is multidimensional, meaning that not all questions included in a single score contributes to the measurement of a single construct.36 Rasch analysis was therefore developed and, in our study, the Rasch analysis confirms the results from VFQ-25.
Lens opacities resulted in lower visual acuity but only slightly lower scores in VFQ-25. Other studies, when validating VFQ-25, showed lower scores and visual acuity in participants with cataract37,38 which can be due to higher levels of lens opacities.
The pseudophakic group showed inferior results at VFQ-25 and a higher prevalence of other eye diseases. Since the differences in VFQ-25 disappear when excluding participants with other eye disease, the presumed reason for the inferior results could be comorbidity. For example, diabetic eye disease has been found to be a risk-factor for cataract26 and diabetic patients might benefit less from cataract surgery.39 Earlier studies have shown that the most frequent reason for “no-benefit” outcome after cataract surgery is a co-existing eye disease.40 The higher prevalence of pseudophakia in people with other eye disease can also be due to obtaining a diagnosis of cataract at an earlier stage.
The study has some limitations: the subjective nature of diagnosing cataract and grading lens opacities, which could be made more objective using an objective method such as the Pentacam Scheimpflug system and the double-pass Optical Quality Analysis System. In a larger cohort, and possibly older participants, more participants would have cataract, which probably would result in greater distribution in VFQ-25 and NEI-VFQ-28-R. Possibly questioning about contrast acuity could detect subjective ailments in participants with cataract.
Conclusion
The prevalence of cataract including pseudophakia in 70-year old people in the Gothenburg area is higher compared to a previous study in a similar geographical area,6 and more common in women than in men. This could be due to the increasing number of cataract surgeries, that are performed at an earlier stage.3 Validation showed very good agreement between pseudophakia assessed by lens photography and self-reported cataract surgery, whereas validation between diagnosis of cataract through examination and self-report showed high specificity but lower sensitivity. The results of BCVA and VFQ-25 are generally good. The results of this study are a good foundation for future studies about risk factors and cataract.
Abbreviations
AL, activity limitations; ANOVA, analysis of variances; BCVA, best corrected visual acuity; CC, cortical cataract; CI, confidence interval; ETDRS, Early Treatment Diabetic Retinopathy Study Chart; IQR, interquartile range; LOCS, lens opacities classification system; NC, nuclear color; NEI VFQ‐25, National Eye Institute Visual Functioning Questionnaire 25; NEI-VFQ-28R, National Eye Institute Visual Functioning Questionnaire 28; NO, nuclear opalescence; NPV, negative predictive value; PPV, positive predictive value; PSC, posterior subcapsular cataract; SD, standard deviation; SEF, socio-emotional functioning.
Data Sharing Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Author Contributions
LHJ performed the ophthalmic examination of 560 participants including visual acuity and lens photographs. MZ and MN analysed the lens photographs. MH did the Cohen’s κ analysis and the sensitivity and specificity analyses. MN did the other statistical analyses and wrote the manuscript with contribution from MZ and MH. TRS, FA and HFE collected data in the H70 study including NEI VFQ‐25 and information on cataract diagnosis and surgery from 1139 participants. IS is initiator and principal investigator of the H70 study. All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This work was supported by grants from the Swedish state under the agreement between the Swedish government and the county councils, the ALF-agreement (ALF-GBG-725041), Göteborg Medical Society, Dr Reinhard Marcuses Foundation, Konung Gustaf V:s och Drottning Victorias Frimurarestiftelse, Hjalmar Svensson Foundation, Greta Andersson Foundation, Marianne and Marcus Wallenberg Foundation, Herman Svensson Foundation, De Blindas Vänner, Agneta Prytz-Folkes och Gösta Folkes stiftelse and Kronprinsessan Margaretas Arbetsnämnd för Synskadade. The H70 study was financed by grants from the Swedish state under the agreement between the Swedish government and the county councils, the ALF-agreement (ALF 716681), the Swedish Research Council (2012-5041, 2015-02830, 2019-01096, 2013-8717, 2017-00639), Swedish Research Council for Health, Working Life and Welfare (2013-1202, 2018-00471, AGECAP 2013-2300, 2013-2496), Konung Gustaf V:s och Drottning Victorias Frimurarestiftelse, Hjärnfonden (FO2014-0207, FO2016-0214, FO2018-0214, FO2019-0163, FO2020-0235), Alzheimerfonden (AF-554461, AF-647651, AF-743701, AF-844671, AF-930868), Eivind och Elsa K:son Sylvans stiftelse. The sponsor or funding organization had no role in the design or conduct of this research.
Disclosure
Prof. Dr. Ingmar Skoog reports grants from Swedish Research Council, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Bourne RRA, Flaxman SR, Braithwaite T, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Global Health. 2017;5(9):e888–e897. doi:10.1016/S2214-109X(17)30293-0
2. Behndig A, Lundstrom M, Serring I, et al. The Swedish National Cataract Register – Annual; 2019. Available from: https://rcsyd.se/kataraktreg/publikationer/arsrapporter.
3. Behndig A, Lundström M, Montan P, et al. The Swedish National Cataract Register – Annual; 2020. Available from: https://rcsyd.se/kataraktreg/publikationer/arsrapporter.
4. Leske MC, Connell AM, Wu SY, Hyman L, Schachat A. Prevalence of lens opacities in the Barbados Eye Study. Archiv Ophthalmol. 1997;115(1):105–111. doi:10.1001/archopht.1997.01100150107018
5. Mitchell P, Cumming RG, Attebo K, Panchapakesan J. Prevalence of cataract in Australia: the Blue Mountains eye study. Ophthalmology. 1997;104(4):581–588. doi:10.1016/S0161-6420(97)30266-8
6. Ostberg A, Loth A, Gustafson D, Lindblom B. Skovde cataract study: i. Prevalence of lens opacities in a Swedish community. Ophthalmology. 2006;113(6):970–975. doi:10.1016/j.ophtha.2006.01.067
7. Koo E, Chang JR, Agron E, et al. Ten-year incidence rates of age-related cataract in the Age-Related Eye Disease Study (AREDS): AREDS report no. 33. Ophthalmic Epidemiol. 2013;20(2):71–81. doi:10.3109/09286586.2012.759598
8. Skoog I. Psychiatric epidemiology of old age: the H70 study–the NAPE lecture 2003. Acta Psychiatr Scand. 2004;109(1):4–18. doi:10.1046/j.1600-0447.2003.00260.x
9. Havstam Johansson L, Škiljić D, Falk Erhag H, et al. Vision-related quality of life and visual function in a 70-year-old Swedish population. Acta Ophthalmol. 2020;98(5):521–529. doi:10.1111/aos.14341
10. Rydberg Sterner T, Ahlner F, Blennow K, et al. The Gothenburg H70 Birth cohort study 2014–16: design, methods and study population. Eur J Epidemiol. 2019;34(2):191–209. doi:10.1007/s10654-018-0459-8
11. Ferris FL 3rd, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94(1):91–96. doi:10.1016/0002-9394(82)90197-0
12. Chylack LT
13. Congdon N, Vingerling JR, Klein BE, et al. Prevalence of cataract and pseudophakia/aphakia among adults in the United States. Archiv Ophthalmol. 2004;122(4):487–494. doi:10.1001/archopht.122.4.487
14. Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-item National Eye Institute Visual Function Questionnaire. Archiv Ophthalmol. 2001;119(7):1050–1058. doi:10.1001/archopht.119.7.1050
15. Mangione C. The National Eye institute 25-Item Visual Function Questionnaire. Available from: https://www.nei.nih.gov/sites/default/files/2019-06/manual_cm2000.pdf.
16. Petrillo J, Bressler NM, Lamoureux E, Ferreira A, Cano S. Development of a new Rasch-based scoring algorithm for the National Eye Institute Visual Functioning Questionnaire to improve its interpretability. Health Qual Life Outcomes. 2017;15(1):157. doi:10.1186/s12955-017-0726-5
17. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi:10.2307/2529310
18. Klein BE, Klein R, Linton KL. Prevalence of age-related lens opacities in a population. The Beaver Dam Eye Study. Ophthalmology. 1992;99(4):546–552. doi:10.1016/S0161-6420(92)31934-7
19. Cabot F, Saad A, McAlinden C, Haddad NM, Grise-Dulac A, Gatinel D. Objective assessment of crystalline lens opacity level by measuring ocular light scattering with a double-pass system. Am J Ophthalmol. 2013;155(4):629–635, 635.e1–2. doi: 10.1016/j.ajo.2012.11.005
20. Pei X, Bao Y, Chen Y, Li X. Correlation of lens density measured using the Pentacam Scheimpflug system with the Lens Opacities Classification System III grading score and visual acuity in age-related nuclear cataract. Br J Ophthalmol. 2008;92(11):1471–1475. doi:10.1136/bjo.2007.136978
21. Pan AP, Wang QM, Huang F, Huang JH, Bao FJ, Yu AY. Correlation among lens opacities classification system III grading, visual function index-14, pentacam nucleus staging, and objective scatter index for cataract assessment. Am J Ophthalmol. 2015;159(2):241–7.e2. doi:10.1016/j.ajo.2014.10.025
22. Klein BE, Klein R, Linton KL, Magli YL, Neider MW. Assessment of cataracts from photographs in the Beaver Dam Eye Study. Ophthalmology. 1990;97(11):1428–1433.
23. Laitinen A, Laatikainen L, Harkanen T, Koskinen S, Reunanen A, Aromaa A. Prevalence of major eye diseases and causes of visual impairment in the adult Finnish population: a nationwide population-based survey. Acta Ophthalmol. 2010;88(4):463–471. doi:10.1111/j.1755-3768.2009.01566.x
24. Lundstrom M, Stenevi U, Thorburn W, Montan P. Swedish National Cataract Register – Annual; 2006. Available from: https://rcsyd.se/kataraktreg/publikationer/arsrapporter.
25. Zetterstrom C, Lundstrom M, Serring I, Montan P, Behndig A, Kugelberg M. The Swedish National Cataract Register - Annual 2014; 2014.
26. Klein BE, Klein R, Lee KE. Incidence of age-related cataract: the Beaver Dam Eye Study. Archiv Ophthalmol. 1998;116(2):219–225. doi:10.1001/archopht.116.2.219
27. Tan AC, Loon SC, Choi H, Thean L. Lens Opacities Classification System III: cataract grading variability between junior and senior staff at a Singapore hospital. J Cataract Refract Surg. 2008;34(11):1948–1952. doi:10.1016/j.jcrs.2008.06.037
28. Patty L, Wu C, Torres M, Azen S, Varma R. Validity of self-reported eye disease and treatment in a population-based study: the Los Angeles Latino Eye Study. Ophthalmology. 2012;119(9):1725–1730. doi:10.1016/j.ophtha.2012.02.029
29. Linton KL, Klein BE, Klein R. The validity of self-reported and surrogate-reported cataract and age-related macular degeneration in the Beaver Dam Eye Study. Am J Epidemiol. 1991;134(12):1438–1446. doi:10.1093/oxfordjournals.aje.a116049
30. Bowie H, Congdon NG, Lai H, West SK. Validity of a personal and family history of cataract and cataract surgery in genetic studies. Invest Ophthalmol Vis Sci. 2003;44(7):2905–2908. doi:10.1167/iovs.02-1055
31. Lundstrom M, Stenevi U, Thorburn W. Gender and cataract surgery in Sweden 1992–1997. A retrospective observational study based on the Swedish National Cataract Register. Acta Ophthalmologica Scandinavica. 1999;77(2):204–208. doi:10.1034/j.1600-0420.1999.770218.x
32. Zhang JS, Xu L, Wang YX, You QS, Wang JD, Jonas JB. Five-year incidence of age-related cataract and cataract surgery in the adult population of greater Beijing: the Beijing Eye Study. Ophthalmology. 2011;118(4):711–718. doi:10.1016/j.ophtha.2010.08.021
33. Lundstrom M, Stenevi U, Thorburn W. The Swedish National Cataract Register - Annual 2001. Available from: https://rcsyd.se/kataraktreg/publikationer/arsrapporter.
34. Zetterberg M, Celojevic D. Gender and cataract–the role of estrogen. Curr Eye Res. 2015;40(2):176–190. doi:10.3109/02713683.2014.898774
35. Zetterberg M. Age-related eye disease and gender. Maturitas. 2016;83:19–26. doi:10.1016/j.maturitas.2015.10.005
36. Pesudovs K, Gothwal VK, Wright T, Lamoureux EL. Remediating serious flaws in the National Eye Institute Visual Function Questionnaire. J Cataract Refract Surg. 2010;36(5):718–732. doi:10.1016/j.jcrs.2009.11.019
37. Labiris G, Katsanos A, Fanariotis M, et al. Psychometric properties of the Greek version of the NEI-VFQ 25. BMC Ophthalmol. 2008;8:4. doi:10.1186/1471-2415-8-4
38. Kovac B, Vukosavljevic M, Djokic Kovac J, et al. Validation and cross-cultural adaptation of the National Eye Institute Visual Function Questionnaire (NEI VFQ-25) in Serbian patients. Health Qual Life Outcomes. 2015;13:142. doi:10.1186/s12955-015-0330-5
39. Olafsdottir E, Andersson DK, Stefansson E. The prevalence of cataract in a population with and without type 2 diabetes mellitus. Acta Ophthalmol. 2012;90(4):334–340. doi:10.1111/j.1755-3768.2011.02326.x
40. Lundstrom M, Stenevi U, Thorburn W. The Swedish National Cataract Register: a 9-year review. Acta Ophthalmologica Scandinavica. 2002;80(3):248–257. doi:10.1034/j.1600-0420.2002.800304.x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.