Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
Proton pump inhibitors use is associated with a lower risk of acute exacerbation and mortality in patients with coexistent COPD and GERD
Authors Su VY , Liao HF, Perng DW, Chou YC, Hsu CC , Chou CL, Chang YL, Yen JC, Chen TJ , Chou TC
Received 22 November 2017
Accepted for publication 12 April 2018
Published 19 September 2018 Volume 2018:13 Pages 2907—2915
DOI https://doi.org/10.2147/COPD.S157761
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Chunxue Bai
Vincent Yi-Fong Su,1–3 Han-Fang Liao,4 Diahn-Warng Perng,3,5 Yueh-Ching Chou,4,6,7 Chia-Chen Hsu,6 Chia-Lin Chou,4,6 Yuh-Lih Chang,4,6 Jiin-Cherng Yen,4 Tzeng-Ji Chen,3,8,9 Ting-Chun Chou4,6
1Department of Internal Medicine, Taipei City Hospital, Taipei, Taiwan; 2Institute of Clinical Medicine, 3Faculty of Medicine, School of Medicine, National Yang-Ming University, Taipei, Taiwan; 4Department and Institute of Pharmacology, National Yang-Ming University, Taipei, Taiwan; 5Department of Chest Medicine, Taipei Veterans General Hospital, Taipei, Taiwan; 6Department of Pharmacy, Taipei Veterans General Hospital, Taipei, Taiwan; 7School of Pharmacy, Taipei Medical University, Taipei, Taiwan; 8Department of Family Medicine, Taipei Veterans General Hospital, Taipei, Taiwan; 9Institute of Hospital and Health Care Administration, National Yang-Ming University, Taipei, Taiwan
Objective: The effect of antacid therapy for patients with COPD and gastroesophageal reflux disease (GERD) remains unclear.
Patients and methods: This nationwide population-based study was conducted using data from Taiwan’s National Health Insurance Research Database, and enrolled COPD patients with or without GERD. Patients with COPD who were not prescribed COPD medications were excluded. Patients with GERD who underwent upper gastrointestinal endoscopy or 24-hour pH monitoring and received at least 1 antacid were enrolled as symptomatic GERD group. The primary endpoint was acute exacerbation and mortality.
Results: This study included 3,485 patients with COPD and symptomatic GERD, and 13,938 patients with COPD alone and covered 12,806.57 and 56,809.78 person-years, respectively, from 2000 to 2011. After multivariate adjustment, symptomatic GERD was associated with acute exacerbation (adjusted hazard ratio [HR]: 1.35, 95% CI: 1.23–1.48, p<0.0001) and mortality (HR: 1.42, 95% CI: 1.25–1.61, p<0.0001). In the COPD with symptomatic GERD group, use of proton pump inhibitors was associated with a lower risk of acute exacerbation and mortality (acute exacerbation, HR 0.31, 95% CI: 0.20–0.50, p<0.0001; mortality, HR 0.36, 95% CI: 0.20–0.65, p=0.0007), whereas no significant benefit was observed for histamine2-receptor antagonists.
Conclusion: Use of proton pump inhibitors was associated with a lower risk of acute exacerbation and mortality in the patients with COPD and symptomatic GERD.
Keywords: GERD, COPD, acute exacerbations, death
Introduction
COPD is one of the most common diseases worldwide, characterized by high morbidity and mortality, and poor quality of life.1 It is a major global health concern and has become a global epidemic. In 2015, 3.2 million people died from COPD worldwide,2 and it has been projected to become the third leading cause of death worldwide by 2030 according to estimates by the World Health Organization.3 Gastroesophageal reflux disease (GERD), also known as acid reflux, is a long-term condition where stomach acid or stomach contents come back up into the esophagus. Previous research4,5 has suggested that GERD is more common in patients with COPD than in those without COPD. In addition, several small studies6–9 have also suggested that an increase in the frequency of COPD exacerbations may be associated with the presence of GERD. GERD has been shown to worsen the control of COPD and to heighten bronchial reactivity and microaspiration.10 Furthermore, GERD has been reported to increase the risk of bacterial colonization in the lower respiratory tract and thereby increase the risk of acute exacerbations in COPD.11 A systematic review and meta-analysis12 of 7 observational studies found that GERD was an independent risk factor for acute exacerbation in patients with COPD.
One of the most important forms of pharmacologic management for GERD is antacid therapy, including histamine2-receptor antagonists (H2RAs) and proton pump inhibitors (PPIs). PPIs are the most effective acid-suppression medications available and are the cornerstone of therapy for GERD. PPI therapy improves both chronic cough and reflux symptoms in patients with GERD.13 However, few studies10 have addressed the role of acid inhibitory treatment in patients with COPD and GERD. The importance of GERD in patients with COPD has been highlighted in international guidelines for COPD.1 Importantly, the risk of acute exacerbation11,12 has been reported to be greater in patients with COPD + GERD than in those with COPD alone. The effect of co-medications on acute exacerbation of COPD in patients with GERD + COPD remains unclear. Thus, we conducted this study using data from a nationwide population-based database to analyze the distinct effects of PPIs and H2RAs on acute exacerbation of COPD in patients with coexisting COPD and GERD.
Methods
Data source
The National Health Insurance (NHI) program in Taiwan was initiated by the government in 1995 to provide comprehensive medical coverage to all residents in Taiwan.14 In 2010, 23 million individuals were enrolled in the NHI program nationwide, with a coverage rate of >99% of the entire population in Taiwan. The National Health Research Institute (NHRI) manages and publicly releases multiple NHI databases for research purposes. The NHI medical claims databases include patient characteristics, detailed claims data for examinations, management, and prescription drugs, and diagnoses for all hospital inpatients and outpatients. In this cohort study, we retrieved data for all patients with diagnoses of COPD and GERD from the National Health Insurance Research Database (NHIRD). The data used in this study were retrieved from the Longitudinal Health Insurance Database 2000 (LHID2000) and 2005 (LHID2005), comprising ~1,000,000 randomly sampled people who were alive in 2000 and 2005, respectively. All registration files and medical claims for reimbursements of these individuals were collected from 1995 to 2011. The released database has been validated by NHRI (http://nhird.nhri.org.tw/date_01.html) to be representative of the whole Taiwanese population. The accuracy of the diagnoses recorded in the NHIRD, such as sleep apnea,15 pneumonia,15 asthma,16 COPD,16 tuberculosis contact,17 and tuberculosis14 has been validated. The study was exempted from full review by the Institutional Review Board of Taipei Veterans General Hospital because the datasets consisted of de-identified secondary data.
Study design and population
We conducted a retrospective analysis to evaluate the effects of PPIs and H2RAs on acute exacerbation of COPD and mortality in patients with coexisting COPD and GERD. In this retrospective cohort study, we enrolled adult patients (≥40 years old) with newly-diagnosed COPD (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes 491, 492, 496) from 2000 to 2009 as the newly-diagnosed COPD cohort. We identified patients with a diagnosis of COPD according to these ICD-9-CM codes in at least 2 recorded outpatient visits or 2 emergency room visits or 1 hospitalization for COPD. Patients with a diagnosis of COPD who were not prescribed with COPD medications within 1 year were excluded. We also enrolled patients with a diagnosis of GERD using ICD-9-CM codes 530.11 or 530.81. Patients with a diagnosis of GERD who did not undergo upper gastrointestinal endoscopy or 24-hour pH monitoring or receive antacids (PPIs and H2RAs) within 180 days prior to diagnosis were enrolled as silent GERD. Newly-diagnosed COPD patients were identified and divided into 3 cohorts: COPD without GERD (COPD alone group), COPD with symptomatic GERD, and COPD with silent GERD. The date of enrollment was defined as the date on which GERD was initially diagnosed. Four age-, gender- and year of enrollment-matched groups of patients with COPD without GERD were randomly selected from the same datasets. All patients were followed until the date of death, withdrawal from the NHI program, or 31 December 2011, whichever occurred first. Data on H2RA and PPI prescriptions were extracted. The primary endpoint was acute exacerbation of COPD and mortality. Patients who were followed up for <28 days and those diagnosed with GERD before the study period were excluded.
Potential confounders and classification of severity
In the analysis of the effects of PPIs and H2RAs on the reduction of acute exacerbations, we controlled for age, sex, comorbidities, and COPD severity, and identified the following comorbidities diagnosed before enrollment that may have confounded the results: arrhythmia, heart failure, ischemic heart disease, peripheral vascular disease, stroke, asthma, psychiatric disorders, and lung cancer.
The severity of COPD was determined according to the annual frequency of emergency department visits (0 and ≥1) and hospitalizations (0 and ≥1) for acute exacerbation and COPD medications (0–2 and ≥3) in the 1 year before the index date. The Global Initiative for Chronic Obstructive Lung Disease guidelines suggest that the frequency of past exacerbation is an important factor when classifying COPD severity.18 COPD medications included long-acting β2-agonists, long-acting muscarinic antagonists, short-acting β2-agonists, short-acting muscarinic antagonists, inhaled corticosteroids, and xanthine.
Effect of exposure to PPIs and H2RAs
Information on PPIs and H2RAs was extracted to analyze their effects on developing acute exacerbation of COPD in the patients with COPD and symptomatic GERD. The patients who were prescribed with PPIs and H2RAs were assigned to PPIs and H2RAs groups, respectively. The PPIs included omeprazole, esomeprazole, lansoprazole, rabeprazole, and pantoprazole. The prescribed H2RAs included cimetidine, ranitidine, famotidine, nizatidine, and roxatidine. We used data on prescription of PPIs and H2RAs during the follow-up period and before the first acute exacerbation for each patient, and calculated the cumulative doses of PPIs and H2RAs in each 90-day period. Furthermore, we used the WHO defined daily dose (DDD) to determine whether a dose effect existed. PPI/H2RA doses of <1 and ≥1 DDD per day were categorized as low-dose and high-dose groups, respectively.
Statistical analysis
All data extraction, matching, and computations were performed using the SAS 9.4 software package (SAS Institute, Cary, NC, USA). Comparisons between the 2 groups were made using the independent Student’s t-test for continuous variables or Pearson’s χ2 test for categorical variables, as appropriate. The Kaplan–Meier method was used to analyze survival, with significance assessed by the log-rank test. Cox proportional hazard regression models were used to determine the effect of the use of PPIs and H2RAs (as a time-dependent covariate) during the follow-up period. The prescription of medication in each 90-day period served as time-dependent covariates. The hazard ratio (HR) for acute exacerbation and mortality in each period was calculated for each medication. Other baseline variables were analyzed as non-time-dependent covariates. Risk factors with a p-value <0.1 in the univariate analysis were entered into the multivariate analysis. All data are expressed as means ± SD or numbers and percentages unless otherwise stated. Two-tailed p-values <0.05 were considered to be significant. All analyses were conducted using SAS statistical software, version 9.4.
Results
Clinical characteristics of the study population
We identified 71,185 patients with newly-diagnosed COPD between 1 January 2000 and 31 December 2009, of whom 6,325 with a diagnosis of GERD before COPD and those with a follow-up period <28 days (n=5,470) were excluded. The COPD patients with GERD who did not receive PPIs/H2RAs or undergo endoscopy or 24-hour pH monitoring within 180 days (n=5,449) were enrolled as COPD with silent GERD, and the remaining 3,485 patients were classified with the COPD with symptomatic GERD (COPD + GERD) cohort. Another 13,938 age-, gender- and year of enrollment-matched COPD patients without GERD were randomly selected as the COPD alone cohort. Data for the COPD + GERD and COPD alone cohorts covered 12,806.57 and 56,809.78 person-years, respectively, from 2000 to 2011. Figure S1 shows the process of enrollment and follow-up.
The basic characteristics of the COPD with symptomatic GERD cohort and COPD alone cohort are shown in Table 1. The COPD with symptomatic GERD cohort had a shorter follow-up time (3.67 vs 4.08 years), higher rate of COPD-related emergency room visits (≥1 visit, 4.99% vs 2.20%), hospitalizations (≥1 hospitalization, 15.21% vs 6.12%), and more prescriptions of COPD medications (≥3 drugs, 21.75% vs 11.41%; all p<0.0001) compared with the COPD alone cohort. In addition, the COPD with symptomatic GERD cohort had higher prevalence rates of comorbidities. During the entire follow-up period, the COPD with symptomatic GERD group were prescribed with significantly more PPIs and H2RAs than the COPD alone group (PPIs, 86.89% vs 15.30%; H2RAs, 53.66% vs 23.83%; both p<0.0001). The basic characteristics of the COPD with silent GERD cohort is shown in Table S1.
The effect of GERD on acute exacerbation and mortality in COPD
Table 2 displays the exacerbation rates and drugs used to treat exacerbation in the COPD with symptomatic GERD and COPD alone cohorts. The exacerbation rates were higher in the COPD with symptomatic GERD cohort than in the COPD alone cohort. Compared to the COPD alone cohort, the COPD with symptomatic GERD cohort had more total exacerbations (rate ratio [RR], 1.78; 95% CI: 1.69–1.87, p<0.0001), more outpatient department visits (RR, 1.52; 95% CI: 1.43–1.62, p<0.0001), more emergency department visits (RR, 1.44; 95% CI: 1.16–1.76, p=0.0007), more hospitalizations (RR, 2.48; 95% CI: 2.28–2.69, p<0.0001), more intensive care unit admissions (RR, 2.70; 95% CI: 2.19–3.33, p<0.0001), and a longer hospital stay (RR, 2.63; 95% CI: 2.58–2.69, p<0.0001). Similarly, the COPD with symptomatic GERD group were prescribed with significantly more drugs for exacerbation than COPD alone group (steroids, 280.5 vs 217.8 mg, p<0.0001; antibiotics, 11 vs 9 days, p<0.0001).
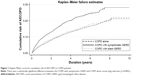
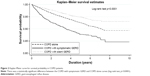
Of note, the COPD with symptomatic GERD cohort had a significantly greater risk of acute exacerbation than the COPD alone cohort in the Kaplan–Meier analysis (log-rank test, p<0.0001; Figure 1). After multivariate adjustment, symptomatic GERD was independently associated with acute exacerbation (adjusted HR: 1.35, 95% CI: 1.23–1.48, p<0.0001; Table S2). Similarly, the COPD with symptomatic GERD cohort had a significantly greater hazard of mortality than the COPD alone cohort (log-rank test, p<0.0001; Figure 2). Symptomatic GERD was independently associated with mortality (HR: 1.42, 95% CI: 1.25–1.61, p<0.0001; Table S3). In contrast, COPD with silent GERD cohort did not have a significantly greater hazard of acute exacerbation and mortality than the COPD alone cohort (Figures 1 and 2). We identified the following independent risk factors for both acute exacerbation and mortality in the COPD with symptomatic GERD cohort: old age, male sex, stroke, more frequent emergency department visits for COPD, more frequent hospitalization for COPD, and more medications for COPD (Tables S4 and S5).
Effects of PPIs/H2RAs on acute exacerbations and mortality
In the COPD with symptomatic GERD group, a high dose of PPIs (≥1 DDD per day) was associated with a significantly lower risk of acute exacerbation (HR 0.31, 95% CI: 0.20–0.50, p<0.0001) compared with a low dose of PPIs (<1 DDD per day). Furthermore, a high dose of PPIs was associated with a significantly lower risk of mortality (HR 0.36, 95% CI: 0.20–0.65, p=0.0007) compared with a low dose of PPIs. In contrast, a high dose of H2RAs (≥1 DDD per day) was associated with an insignificantly lower risk of acute exacerbation (HR 0.75, 95% CI: 0.47–1.21) and mortality (HR 0.80, 95% CI: 0.39–1.63) compared with a low dose of PPIs (<1 DDD per day; Table 3).
  | Table 3 Association between PPIs/H2RAs use and risk of acute exacerbation and mortality in COPD with symptomatic GERD |
Table 4 shows the results of the effects of PPIs/H2RAs on acute exacerbation and mortality in the patients with COPD. Compared with the COPD alone group, the patients in the COPD with symptomatic GERD group who were treated with low-dose PPIs or H2RAs were associated with a significantly higher risk of acute exacerbation (HR 1.75, 95% CI: 1.50–2.03, p<0.0001) and mortality (HR 1.97, 95% CI: 1.56–2.50, p<0.0001). Furthermore, the patients in the COPD with symptomatic GERD group who were treated with high-dose H2RAs were still associated with an insignificantly higher risk of acute exacerbation (HR 1.28; 95% CI: 0.91–1.80) and mortality (HR 1.33, 95% CI: 0.78–2.25) than those in the COPD alone group. In contrast, the patients in the COPD with symptomatic GERD group who were treated with high-dose PPIs were associated with a significantly lower risk of acute exacerbations (HR, 0.58, 95% CI: 0.38–0.90, p=0.0156) than those in the COPD alone group. Importantly, there was no significant difference in the risk of mortality between the COPD with symptomatic GERD group who were treated with high-dose PPIs and those in the COPD alone group (HR 0.95, 95% CI: 0.54–1.67; Table 4).
  | Table 4 Association between PPIs/H2RAs use and risk of acute exacerbations and mortality in patients with COPD |
Discussion
In this study, we demonstrated that COPD patients with symptomatic GERD had a greater burden of medical care than those without GERD. In addition, symptomatic GERD was an independent risk factor for death in the patients with COPD. We also demonstrated that the use of PPIs was associated with a significant reduction in acute exacerbation and mortality in the COPD patients with symptomatic GERD, but that the use of H2RAs was not. To the best of our knowledge, this is the largest cohort study to investigate the effect of acid suppressing medications on the risk of acute exacerbation and death among COPD patients with symptomatic GERD.
In this study, we enrolled 3,485 COPD patients with symptomatic GERD and 13,938 COPD patients without GERD from a real world setting instead of a professional study, which is of greater value because it more closely reflects real clinical practice. The COPD cohort was derived from a national database which minimized selection bias. Because participation in the NHI program is mandatory in Taiwan, and as all Taiwanese residents can use medical service with low copayments, follow-up in NHIRD involves minimal referral bias. In this study, the diagnosis of COPD required prescriptions with at least 1 COPD medication, and the diagnosis of symptomatic GERD required confirmation via upper gastrointestinal endoscopy or 24-hour pH monitoring. Therefore, the diagnoses of COPD and symptomatic GERD in our dataset were both thorough and reliable.
Following the GOLD guidelines for COPD,1 the severity of COPD was classified according to the average number of acute exacerbations per year. In this study, the severity of COPD was estimated, which helped to eliminate bias caused by the increased use of medications in patients with severe COPD. Furthermore, sensitivity analysis was performed to explore the dose-dependent effect of acid suppressing medications on acute exacerbation in the COPD with symptomatic GERD cohort.
Previous epidemiological studies6,7,9,11 have reported that COPD + GERD was associated with more acute exacerbations compared to COPD without GERD. One questionnaire-based, cross-sectional survey6 in the USA enrolled 86 patients with COPD and reported that the presence of GERD symptoms appeared to be associated with increased exacerbations of COPD. In addition, prospective cohort studies7,9,11 in Japan which enrolled 82, 67, and 221 COPD patients, respectively, found that GERD symptoms were an important factor associated with COPD exacerbations. Moreover, a large retrospective cohort study in Denmark that enrolled 1,259 COPD patients with GERD showed that GERD was associated with an increased risk of acute exacerbations of COPD (HR 2.7, 95% CI: 1.3–5.4). However, GERD has been defined using a self-reported questionnaire in almost all previous studies.6–9,11,12 In this study, the COPD + GERD cohort were prescribed significantly more COPD medications and had more acute exacerbations than the COPD without GERD cohort. These findings are consistent with those of previous studies conducted worldwide. Furthermore, the diagnosis of symptomatic GERD in our study required confirmation via upper gastrointestinal endoscopy or 24-hour pH monitoring. Importantly, this is the first study to demonstrate that symptomatic GERD was an independent risk factor for death in COPD patients.
Antacid medications including PPIs and H2RAs play an important role in the pharmacologic management of GERD. PPIs are a more effective treatment for acid reduction in GERD than H2RAs. In one small prospective cohort study from Turkey,19 13 COPD patients with GERD showed significant improvements in COPD symptoms after 2 months of treatment with PPIs. To the best of our knowledge, this study is the first to investigate the effect of PPIs and H2RAs on acute exacerbation and mortality in COPD patients with symptomatic GERD. We found that PPIs were more effective in reducing acute exacerbation of COPD and mortality than H2RAs in COPD patients with symptomatic GERD, and that H2RAs were not beneficial for acute exacerbations and mortality in COPD patients with symptomatic GERD. Importantly, our results showed that the use of PPIs was associated with a significantly lower dose-dependent risk of acute exacerbation and mortality in the COPD patients with symptomatic GERD. Additionally, stroke was an independent risk factor for both acute exacerbation and mortality in COPD patients with symptomatic GERD. Dysphagia is known to be a common and potentially serious complication of stroke. Patients with stroke may receive nasogastric tube feeding, which may increase the risk of gastric reflux. In a screening study,20 the prevalence of GERD is as high as 56% in patients with stroke and associated with aspiration pneumonia. Therefore, physicians should not postpone treatment for GERD in the hopes of a spontaneous recovery in COPD patients with stroke.
The results of our study have several implications. Increasing evidence suggests that PPIs are highly effective in treating GERD symptoms, and that GERD symptoms are an independent risk factor for acute exacerbation of COPD. Our findings strengthen the evidence for the benefits of PPIs in COPD patients with symptomatic GERD, which might improve the prescription of PPIs in clinical practice. Moreover, to the best of our knowledge, this study is the first to investigate the effect of H2RAs and PPIs on acute exacerbation and mortality in COPD patients with symptomatic GERD.
Nevertheless, this study has some limitations. First, the claims-based dataset lacked certain personal information such as data on smoking and obesity, although these factors appear to have no influence on the selection of PPIs and H2RAs. Second, the results of pulmonary function test and dyspnea scale were not available. In accordance with recent COPD guidelines,1 however, we used the annual frequency of admission for COPD to classify severity. Diagnoses of COPD and GERD that rely on administrative claims data recorded by physicians or hospitals may be less accurate than those made in a prospective clinical setting. However, the diagnosis of symptomatic GERD required upper gastrointestinal endoscopy or 24-hour pH monitoring confirmation and the diagnosis of COPD required the prescription of at least 1 COPD medication. Third, we could not assess drug adherence directly. However, this bias is toward the null hypothesis and would lead to an underestimation of the actual effects of medications. Finally, the external validity of our findings may be of concern because almost all enrollees were Chinese. The generalizability of our results to non-Chinese populations must be verified in further studies.
Conclusion
This study demonstrated a higher acute exacerbation rate and risk of mortality in patients with COPD and symptomatic GERD compared with those with COPD alone. The use of PPIs decreased the risk of future acute exacerbation and mortality in the patients with COPD and symptomatic GERD. Further well-designed studies of patients with COPD and symptomatic GERD are warranted and should focus on distinguishing the effects of different antacid medications.
Acknowledgments
This study was supported in part by grants from Taipei Veterans General Hospital (2015-12-005BC, and V105D10-003-MY2-2). This study is based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by the National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of the Bureau of National Health Insurance, Department of Health or National Health Research Institutes. The authors would like to thank the Biostatistics Task Force at Taipei Veterans General Hospital and the Institute of Public Health, National Yang-Ming University, for the comments and assistance in data analysis. The authors acknowledge the help of Hsin-Yi Huang and Chyong-Mei Chen in data collection and analysis.
Author contributions
VYS, HFL, DWP and YCC had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: VYS, HFL, DWP, YCC, CCH, CLC, YLC. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work. Study supervision: DWP, YCC, CCH, CLC, YLC, JCY, TJC.
Disclosure
The authors report no conflicts of interest in this work.
References
Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am J Respir Crit Care Med. 2017;195(5):557–582. | ||
GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5(9):691–706. | ||
World Health Organization. Burden of COPD. Available from: http://www.who.int/respiratory/copd/burden/en/. Accessed: March 21, 2016. | ||
Mokhlesi B, Morris AL, Huang CF, Curcio AJ, Barrett TA, Kamp DW. Increased prevalence of gastroesophageal reflux symptoms in patients with COPD. Chest. 2001;119(4):1043–1048. | ||
Casanova C, Baudet JS, del Valle Velasco M, et al. Increased gastro-oesophageal reflux disease in patients with severe COPD. Eur Respir J. 2004;23(6):841–845. | ||
Rascon-Aguilar IE, Pamer M, Wludyka P, et al. Role of gastroesophageal reflux symptoms in exacerbations of COPD. Chest. 2006;130(4):1096–1101. | ||
Takada K, Matsumoto S, Kojima E, et al. Prospective evaluation of the relationship between acute exacerbations of COPD and gastroesophageal reflux disease diagnosed by questionnaire. Respir Med. 2011;105(10):1531–1536. | ||
Ingebrigtsen TS, Marott JL, Vestbo J, Nordestgaard BG, Hallas J, Lange P. Gastro-esophageal reflux disease and exacerbations in chronic obstructive pulmonary disease. Respirology. 2015;20(1):101–107. | ||
Terada K, Muro S, Sato S, et al. Impact of gastro-oesophageal reflux disease symptoms on COPD exacerbation. Thorax. 2008;63(11):951–955. | ||
Lee AL, Goldstein RS. Gastroesophageal reflux disease in COPD: links and risks. Int J Chron Obstruct Pulmon Dis. 2015;10:1935–1949. | ||
Terada K, Muro S, Ohara T, et al. Abnormal swallowing reflex and COPD exacerbations. Chest. 2010;137(2):326–332. | ||
Sakae TM, Pizzichini MM, Teixeira PJ, Silva RM, Trevisol DJ, Pizzichini E. Exacerbations of COPD and symptoms of gastroesophageal reflux: a systematic review and meta-analysis. J Bras Pneumol. 2013;39(3):259–271. | ||
Labenz J, Nocon M, Lind T, et al. Prospective follow-up data from the ProGERD study suggest that GERD is not a categorial disease. Am J Gastroenterol. 2006;101(11):2457–2462. | ||
Su VY, Su WJ, Yen YF, et al. Statin use is associated with a lower risk of tuberculosis. Chest. 2017;152(3):598–606. | ||
Su VY, Liu CJ, Wang HK, et al. Sleep apnea and risk of pneumonia: a nationwide population-based study. CMAJ. 2014;186(6):415–421. | ||
Su VY, Yang KY, Yang YH, et al. Use of ICS/LABA combinations or LAMA is associated with a lower risk of acute exacerbation in patients with coexistent COPD and asthma. J Allergy Clin Immunol Pract. Epub 2018 Feb 10. | ||
Su VY, Yen YF, Pan SW, et al. Latent tuberculosis infection and the risk of subsequent cancer. Medicine (Baltimore). 2016;95(4):e2352. | ||
Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. | ||
Eryuksel E, Dogan M, Olgun S, Kocak I, Celikel T. Incidence and treatment results of laryngopharyngeal reflux in chronic obstructive pulmonary disease. Eur Arch Otorhinolaryngol. 2009;266(8):1267–1271. | ||
Satou Y, Oguro H, Murakami Y, et al. Gastroesophageal reflux during enteral feeding in stroke patients: a 24-hour esophageal pH-monitoring study. J Stroke Cerebrovasc Dis. 2013;22(3):185–189. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.