Back to Journals » ClinicoEconomics and Outcomes Research » Volume 9
Propofol or benzodiazepines for short- and long-term sedation in intensive care units? An economic evaluation based on meta-analytic results
Authors Pradelli L , Povero M, Bürkle H, Kampmeier T, Della-Rocca G, Feuersenger A, Baron J, Westphal M
Received 11 March 2017
Accepted for publication 4 July 2017
Published 9 November 2017 Volume 2017:9 Pages 685—698
DOI https://doi.org/10.2147/CEOR.S136720
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Lorenzo Pradelli,1 Massimiliano Povero,1 Hartmut Bürkle,2 Tim-Gerald Kampmeier,3 Giorgio Della-Rocca,4 Astrid Feuersenger,5 Jean-Francois Baron,6 Martin Westphal5
1AdRes HE&OR, Torino, Italy; 2Department of Anaesthesiology and Critical Care Medicine, Medical Center – University of Freiburg, Faculty of Medicine, University of Freiburg, Freiburg, 3Clinic for Anesthesiology and Surgical Intensive Care Medicine, University Hospital Münster, Münster, Germany; 4Department of Anaesthesia and Intensive Care Medicine, Medical School of the University of Udine, Udine, Italy; 5Fresenius Kabi Deutschland GmbH, Bad Homburg, Germany; 6Fresenius Kabi ELAMA, Paris Cedex, France
Purpose: This evaluation compares propofol and benzodiazepine sedation for mechanically ventilated patients in intensive care units (ICUs) in order to identify the potential economic benefits from different payers’ perspectives.
Methods: The patient-level simulation model incorporated efficacy estimates from a structured meta-analysis and ICU-related costs from Italy, Germany, France, UK, and the USA. Efficacy outcomes were ICU length of stay (LOS), mechanical ventilation duration, and weaning time. We calculated ICU costs from mechanical ventilation duration and ICU LOS based on national average ICU costs with and without mechanical ventilation. Three scenarios were investigated: 1) long-term sedation >24 hours based on results from randomized controlled trials (RCTs); 2) long-term sedation based on RCT plus non-RCT results; and 3) short-term sedation <24 hours based on RCT results. We tested the model’s robustness for input uncertainties by deterministic (DSA) and probabilistic sensitivity analyses (PSA).
Results: In the base case, mean savings with propofol versus benzodiazepines in long-term sedation ranged from €406 (95% confidence interval [CI]: 646 to 164) in Italy to 1,632 € (95% CI: 2,362 to 880) in the USA. Inclusion of non-RCT data corroborated these results. Savings in short-term sedation ranged from €148 (95% CI: 291 to 2) in Italy to €502 (95% CI: 936 to 57) in the USA. Parameters related to ICU and mechanical ventilation had a stronger influence in the DSA than drug-related parameters. In PSA, propofol reduced costs and ICU LOS compared to benzodiazepines in 94%–100% of simulations. The largest savings may be possible in the UK and the USA due to higher ICU costs.
Conclusion: Current ICU sedation guidelines recommend propofol rather than midazolam for mechanically ventilated patients. This evaluation endorses the recommendation as it may lead to better outcomes and savings for health care systems, especially in countries with higher ICU-related costs.
Keywords: critically ill patients, mechanical ventilation, anesthetics, length of stay, costs, health care system
Plain language summary
Why was the study done? Very sick patients in the intensive care unit (ICU) often need breathing assistance by a ventilator machine. To ease the distress of breathing assistance, these patients often receive sedative drugs. Some sedatives may, however, make it more difficult for the patients to restart breathing without the breathing assistance. We did this study to find out how long it takes for patients to restart breathing and to leave the ICU when receiving different sedatives. We also wanted to find out if the costs for health care systems in Italy, Germany, France, UK, and the USA are lower if patients receive sedatives that allow an early return to breathing.
What did the researchers do and find? We searched scientific literature for studies comparing the effect of different sedatives on the time patients spend with breathing assistance and in the ICU. Thirty five studies with such data were identified and the results comprehensively analyzed. Patients receiving the sedative propofol needed breathing assistance for a shorter time and left the ICU earlier than patients who received benzodiazepines. Next, we calculated if using propofol instead of benzodiazepines would lower the costs for health care systems. Propofol would indeed lower the health care costs: in Italy, a country with relatively low costs for ICUs, the savings would be ~€406 per patient. In the USA, where costs for intensive care are higher, savings would be ~€1,632 per patient.
What do these results mean? These results strengthen the current guideline recommendations that propofol should be used for sedation in patients receiving breathing assistance. Patients treated with propofol need breathing assistance for a shorter time and may leave the ICU earlier. Propofol also allows cost savings for health care systems, especially in countries with high costs for ICUs.
Introduction
Acute pain and discomfort have deleterious effects on different physiological responses such as pulmonary and cardiovascular function and impede recovery after surgery.1 Therefore, relieving pain and anxiety to improve patient comfort in the intensive care unit (ICU) is strategic.2 Sedatives play a central role in amending physiological stress responses for better outcomes.2 Sedatives do, however, have side effects which have the potential to prolong mechanical ventilation and the time spent in the ICU.3 Extended mechanical ventilation is associated with increased morbidity and mortality in ICU patients4,5 and the specialized care necessary for ventilated patients increases the already considerable daily ICU costs.6,7 Consequently, a sedative agent that facilitates early recovery from mechanical ventilation and timely discharge from the ICU may contribute to optimize limited ICU resources and save money for our stressed health care systems.
We conducted this study to answer the following questions. First, which of the sedatives commonly used in critical care facilitates an early return to spontaneous breathing and timely ICU discharge? And second, do these effects translate into cost savings compared to the other sedatives?
Propofol and benzodiazepines such as midazolam and lorazepam are commonly used for ICU sedation. Midazolam is an imidazobenzodiazepine with moderate sedative potency and hypnotic, anxiolytic, amnestic, and anticonvulsant properties.8 Lorazepam has a longer duration of action compared to midazolam, yet all benzodiazepines may accumulate in the body after prolonged use.9 Propofol on the other hand is a potent sedative and hypnotic agent with anxiolytic, amnestic, antiemetic, and anticonvulsant properties, without a significant analgesic effect.10,11 It rapidly passes the blood–brain barrier, leading to a fast onset and offset of action3 and is quickly eliminated from the central compartment without significant accumulation in the body.12 In the current guidelines, non-benzodiazepine sedatives are recommended over benzodiazepines for mechanically ventilated ICU patients.13,14 Propofol is endorsed for moderate and deep sedation due to shorter weaning times associated with its use.14
In an earlier meta-analysis, propofol was associated with significant improvements over benzodiazepines in recovery-related outcomes such as duration of mechanical ventilation15 and length of ICU stay.15 These results show that patients sedated with propofol recover earlier from mechanical ventilation and leave the ICU sooner compared to benzodiazepine-sedated patients. Despite higher acquisition costs of propofol compared to benzodiazepines,16 the shorter mechanical ventilation and ICU recovery times may result in cost savings by facilitating optimal resource use in the ICU.17
Several economic evaluations of ICU sedation have been published which investigate this question from the Spanish,17–19 British,20,21 USA,16,22–24 German,25 Canadian,26 and Chinese27 payers’ perspective. These studies are economic evaluations of clinical trials except for three studies22–24 which were based on meta-analytic results. Only two23,24 evaluations investigated the influence of uncertainty in economic outcomes. Hence, the necessity of economic evaluations based on rigorous effectiveness inputs incorporating sensitivity analyses still exists, even from previously evaluated perspectives. Sensitivity analysis allows estimating outcome distributions in addition to the outcomes’ mean values. This is of interest to decision makers since it allows gauging confidence in the “best choice” determined by the model by exploring its robustness to changes in the model’s inputs.
Therefore, we present an economic evaluation of propofol versus benzodiazepine sedation in mechanically ventilated ICU patients from the perspectives of four European countries and the USA based on statistically significant meta-analytic results.
Materials and methods
Methods of the meta-analysis
Search strategy
We searched MedLine (via PubMed) and EMBASE (via Scopus) databases for studies investigating the relative efficacy of propofol, the most commonly used benzodiazepines midazolam, lorazepam, and diazepam, and dexmedetomidine in adult mechanically ventilated patients. Outcomes of interest were weaning time, duration of mechanical ventilation, time to extubation, and ICU length of stay (LOS). The last search was carried out in December 2013. Exclusion criteria were non-tagret patients (not intubated, no mechanical ventilation, children), studies comparing only non-tagret regimens, comparison between the same regimen tested through different monitoring or sedation strategies, off-label use, publication not in English, German, Italian, French, or Spanish, and post hoc analyses of already included studies.
Study selection
Search results were screened firstly title-based, secondly abstract-based, and thirdly full text-based by two independent reviewers. Studies not meeting the eligibility criteria were excluded. Additionally, a careful manual check of references included in reviews and retrospective articles identified further studies for full text review. Discordance between the reviewers was resolved by discussion.
Data extraction
Data were collected independently by two experienced reviewers, cross-checked to rule out discrepancies, and finally sample-checked by a third reviewer. Inconsistencies were solved by returning to the original paper in joint sessions.
Statistical analysis
For every outcome of interest, the overall effect size for each comparison was determined as a weighted mean difference of the effect size estimates obtained from extracted data and presented as mean difference ± standard deviation (SD) and 95% confidence interval (CI).
Tests used to assess heterogeneity were c2, t2, and I2, with greater relevance given to the latter. Statistical analyses for direct comparisons and heterogeneity tests were calculated using “R” statistical computing software with the “meta” package and Review Manager (RevMan) (Version 5.2; Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) (with the DerSimonian and Laird method used for the calculation of t), which yielded the same results.
We applied random effect models in all comparisons because random effect estimates are more conservative, and for clinical reasoning, since patient groups are heterogeneous within and across studies.
Studies were stratified into sedation <24 hours (short-term sedation) and sedation >24 hours (long-term sedation). Included studies were additionally stratified into randomized controlled trials (RCTs) and non-RCTs. We conducted a primary analysis of data from 27 RCTs and a broad analysis of these 27 RCTs plus eight non-RCTs to add generalizability to the results. While RCTs provide greater internal validity and help to identify causal relationships, the restrictive exclusion criteria for patient selection may result in lower external validity.28
Further details on eligibility criteria, search strategy, data extraction, and statistical analysis can be found in the Supplementary materials.
Methods of the economic evaluation
The economic evaluation is based on a patient-level simulation model that incorporates comparative efficacy estimates from our previously described meta-analysis and payer relevant ICU and drug costs in Italy, Germany, France, Great Britain, and in the USA. It is based on results from our meta-analysis including 27 RCT17,18,29–53 and eight non-RCT19,54–60 studies reporting on at least one outcome of interest. Following evidence-based medicine principles in populating the economic model, only statistically significant results were used as effectiveness inputs.61 Three effectiveness analyses comparing propofol to benzodiazepines were carried out:
- long-term sedation >24 hours based on results extracted from 12 RCTs,17,31–34,36,39,41,44–46,49
- long-term sedation >24 hours based on results extracted from the 12 RCTs and five non-RCTs,19,54–57 and
- short-term sedation <24 hours based on results extracted from 12 RCTs.18,29,30,35–38,40,42,43,47,48
No non-RCT studies on short-term sedation were identified in the systematic literature search so that only an RCT-based analysis was carried out.
Cohorts
Two identical cohorts of 1,000 patients each were generated as treatment groups: the propofol cohort (reference treatment) and the benzodiazepine cohort (alternative treatment). Individual patients’ body weights for both cohorts were sampled from normal distribution (mean 70.5 kg, SD =15) based on an Italian study.62 These weights were used to calculate specific individual loading and maintenance sedative doses. Recovery time values for individual patients in the propofol cohort were sampled from gamma distributions. The corresponding values for the benzodiazepine-treated “twin” were obtained by adding the relevant treatment effect size found in the meta-analysis (Figure 1). The model was created in Microsoft Excel 2010.
  | Figure 1 Graphic structure of the model used to assess costs of consumed resources. Abbreviation: ICU, intensive care unit. |
Model inputs
Effectiveness inputs
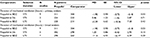
Clinical outcomes from the meta-analysis were used to derive the following recovery times considered in the present model (Table 1):
- ICU LOS: time from admission to discharge from ICU;
- duration of mechanical ventilation: time spent under mechanical ventilation before autonomous spontaneous breathing;
- weaning time: time elapsed from the decision to start weaning (as clinically indicated, discontinuation of the study drug) to extubation, when no reintubation was required;
- duration of sedation: calculated as the duration of mechanical ventilation minus weaning time.
Recovery times for both cohorts in the three scenarios are summarized in Table 1. The effect sizes are statistically significant with the exception of mechanical ventilation duration in long-term sedation. In order to include only statistically significant results in this model,61 comparisons between propofol and dexmedetomidine were omitted and the mean difference in duration of mechanical ventilation in long-term sedation was calculated using weaning time efficacy as a proxy. Consequently, there was no difference in sedation time and therefore sedative consumption in the two simulated cohorts.
Drug consumption
Both sedative agents and analgesic use were integrated in this model. Sedative doses were calculated for each individual as the sum of loading dose and continuous infusion for maintenance. Midazolam doses were used for the benzodiazepine cohort. For propofol, the loading dose (±SD) was 1.1±0.83 mg/kg and the maintenance dose was 1.61±0.97 mg/kg/h. The midazolam loading and maintenance doses were 0.1±0.06 mg/kg and 0.1±0.04 mg/kg/h, respectively. All sedative drug doses were sampled from gamma distributions. Differences in analgesic consumption are expressed in morphine milligram equivalents and derived from pooling data from the studies included in the meta-analysis.
The cost drivers considered in the model are: 1) ICU costs with mechanical ventilation, 2) ICU costs when patients are breathing spontaneously (post-extubation), and 3) drug costs (sedative and analgesic drugs).
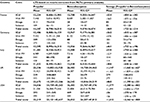
Dasta et al63 observed that daily ICU costs decreased from the first to the third day of ICU stay. Based on the presented data, we calculated the contribution of mechanical ventilation to the total daily costs as 33.5%.63 In this model, daily ICU costs per patient were calculated from the relevant national mean daily ICU costs of mechanically ventilated patients.63–66 ICU costs without mechanical ventilation were obtained by subtracting 33.5% from the total ICU costs with mechanical ventilation.63 The resulting average ICU costs per patient on days 1, 2, and past day 2 were calculated per hour and updated to the present values (Table 2). To account for different publication years of the cost studies, all cost estimates were converted to the costing year by using official inflation indices.
  | Table 2 ICU costs per hour stratified by use of mechanical ventilation and successive ICU days Abbreviations: ICU, intensive care unit; MV, mechanical ventilation. |
Composite drug costs were calculated from the costs of sedative agents and analgesic drugs. Expenses for sedation are proportional to the consumption of sedatives. Costs were calculated for each individual as the sum of loading dose and maintenance infusion costs. Analgesic drug costs were calculated similar to sedative costs. The least expensive combination of vials to reach the total dose was calculated for all drugs. Since data on country-specific hospital costs of benzodiazepines in France and morphine both in the UK and USA were missing, the lowest unit costs among those reported for the other countries were used as a proxy.
Sensitivity analysis
Two types of sensitivity analyses were performed with the studies included in the meta-analysis in order to study the impact of uncertainty in input variables: a one-way deterministic sensitivity analysis (DSA) and a probabilistic sensitivity analysis (PSA).
In the DSA, all input parameters with the exception of hourly ICU costs with mechanical ventilation were separately allowed to vary to a minimum of 20% lower and a maximum of 20% higher, while all other parameters were left unchanged. Two scenarios were assumed for the hourly costs of ICU with mechanical ventilation: equal (minimum) or double (maximum) the hourly costs without mechanical ventilation. The SDs for individual parameters such as patient weight were rescaled accordingly.
In the PSA, all input variables were allowed to vary at the same time. All parameters were sampled from gamma distribution except for effect sizes and weight, which were sampled from normal distribution. Patient-level variables such as weight, drug dose, and ICU recovery time were sampled for 10,000 iterations in an inner loop (representing the heterogeneity of patients, just like in the base case simulation), and then averaged and repeated 1,000 times in an outer loop (representing the parameter uncertainty).
Results
Results of the meta-analysis
Literature search
We identified 346 publications (59 in PubMed, 287 in Scopus). Manual check of previous reviews and meta-analyses yielded 17 articles. Title, abstract and full text screening led to the exclusion of 328 articles. Details on the selection process can be found in the Supplementary materials and a flow diagram of article selection is shown in Figure S1. Data were extracted from 35 papers identified in the full text-based selection: 27 RCTs17,18,29–53 including 2,283 patients and eight observational studies19,54–60 including 732 patients. Study characteristics are presented in Tables S1 and S2 in the Supplementary materials. Sixteen studies reported data on short-term sedation,29,30,35,37,38,40,42,43,47,48,50,51,53,58–60 16 studies investigated long-term sedation,17,19,31–34,39,41,44–46,49,54–57 and three studies presented data on both.18,36,52
Meta-analysis
Results of the meta-analysis are shown in Tables 3–6, and corresponding forest plots are shown in Figures S2–S5 in the Supplementary materials.
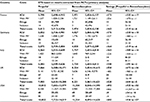
Results of the economic analysis
Three effectiveness scenarios were investigated from five payers’ perspectives. In the base case, despite higher drug costs, propofol sedation resulted in savings compared to benzodiazepines in all three scenarios: 1) Savings in long-term sedation based on RCT results ranged from €406 (95% CI: 646 to 164) in Italy to €1,632 (95% CI: 2,362 to 880) in the USA; 2) Savings in long-term sedation based on RCT and non-RCT results ranged from €564 (95% CI: 1,222 to −115) in Italy to €2,109 (95% CI: 4,111 to 30) in the USA; and 3) in short-term sedation based on RCT results from €148 (95% CI: 291 to 2) to €502 (95% CI: 936 to 57). All results of three scenarios from five payers’ perspectives are reported in Tables 7–9.
Sensitivity analysis
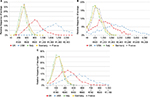
Results of the DSA are shown as tornado diagrams in Figure 2. The input parameters that were allowed to vary are reported in decreasing cost difference impact order to demonstrate the influence of uncertainty in single parameters on total costs. The results from the five countries’ perspectives are grouped and the order of the variables is based on the mean influence for each variable (high to low). In both long- and short-term sedation scenarios, the model appears to be more sensitive to ICU-related inputs (duration of ICU stay and ICU costs) than to drug-related inputs (drug costs and doses).
Results of the PSA are shown as savings histograms for three scenarios in the five investigated countries in Figure 3. The PSA demonstrates the robustness of the economic analysis to uncertainty in input variables since the results consistently maintain the direction of the base case. In the UK and USA, the curves are shifted to the left since more savings are expected because of higher ICU costs in these countries.
Scatter plots of effectiveness versus savings are shown for Italy (Figure 4). As the same pattern was observed in all other countries, Italy is presented here as the representative example. In effectiveness scenario A (long-term sedation based on results extracted from RCTs), propofol sedation resulted in higher savings and shorter ICU stays in 100% of the simulated cases in all five countries. In scenario B (long-term sedation based on results extracted from RCTs + non-RCTs), higher savings and shorter ICU stays with propofol sedation were found in 94.2% of the simulations in the UK, 97.1% in the USA, 94.5% in Italy, 95.0% in Germany, and 96.7% in France. Finally, higher savings and shorter ICU stays with propofol sedation were reported in 97.8% of the simulations in scenario C (short-term sedation based on RCT results) in the UK, 98.4% in the USA, 97.8% in Italy, 98.0% in Germany, and 98.1% in France.
Discussion
This economic analysis shows that propofol is cost saving compared to benzodiazepines for short- and long-term sedation of intensive care patients. This finding is valid for five different national settings with large differences in ICU costs, and robust to uncertainties in input variables.
Most of the previously published economic evaluations were carried out based on randomized trials.16–18,20,21,25–27 The analysis in one study was based on drug costs only;16 a narrow scope ignoring the therapeutic value of propofol in terms of shortening sedation times and ICU stays. In the majority of the economic evaluations, however, drug costs as well as mechanical ventilation and ICU costs were taken into account. Carrasco et al compiled all costs of care after start of sedation into their analysis,18 which included mechanical ventilation and ICU costs. In two economic evaluations, propofol’s economic value was assessed by accounting only for drug and human resources costs.21,25 The other economic evaluations assessed economic values by accounting for drug, ICU, and mechanical ventilation costs except for Barrientos-Vega et al who excluded ICU costs after extubation.17,19 Hence, the majority of investigators agree that the cost drivers most relevant for such comparisons are costs for ICU time, mechanical ventilation, and drugs.
Three formal economic evaluations from the US perspective were based on results from meta-analyses.22–24 Bioc et al22 assessed benzodiazepine versus non-benzodiazepine long-term sedation based on effectiveness outcomes in noncardiac surgery patients, taking into account drug and ICU costs with and without mechanical ventilation. Total costs with non-benzodiazepine sedation were $35,380 compared to $45,394 with benzodiazepine sedation. In both cases, ~71% of the total costs accrued during intubation. The specific choice of non-benzodiazepine sedative (propofol or dexmedetomidine) had little effect on the economic outcome. The other evaluations compared propofol, lorazepam, and midazolam. Cox et al24 fed a probabilistic decision model for short-term sedation with inputs from RCTs and a retrospective study. Costs of drugs, ICU costs with and without mechanical ventilation stratified by successive ICU days, laboratory investigations, and hospital stay after discharge from the ICU were evaluated, and DSA, PSA, and scenario sensitivity analyses were conducted. Propofol sedation resulted in a 12% cost reduction compared to lorazepam. MacLaren et al23 published a probabilistic decision model on short-term, medium-term, and long-term sedation. The cost drivers were drug costs and adverse event costs including hypotension, hypertriglyceridemia, post-sedation ventilation, ventilator-associated pneumonia, and agitation.23 ICU costs were not accounted for. Even in this setting, propofol was found to be cost saving in the short-term sedation scenario.
In our analysis, relative effectiveness inputs were derived from a meta-analysis, providing the highest level of evidence obtainable. Cost drivers were drug consumption and ICU recovery times. The analysis further differentiates between hourly costs with or without mechanical ventilation and hourly costs on the first, second, and subsequent days. The investigated settings included both short- and long-term sedation. In long-term sedation, we have additionally examined economic outcomes found in non-RCT studies. While the RCTs in this analysis demonstrate a causal relationship between the outcome parameters and the type of sedative, non-RCTs can only show correlations. However, restrictive exclusion criteria and strict procedural standards in RCTs do not reflect clinical routine. Therefore, the additional analysis of observational studies corroborates the findings of RCTs by confirming the effects in everyday clinical practice and thus adds external validity to the analysis.28 The larger savings found in this analysis are robust to variability as shown by the sensitivity analyses and indicate that the effect may be even stronger in everyday practice.
In current clinical practice guidelines, propofol is recommended for mechanically ventilated patients.14 Effectiveness and cost-effectiveness evaluations endorse this recommendation.31,67 Propofol has been shown to significantly reduce the duration of ICU stay in long-term sedation15 and has proved to be cost saving compared to benzodiazepine long-term sedation in this analysis. Taking into consideration that midazolam is still the most frequently used drug for sedation in the ICU,15 our analysis may suggest to clinical decision makers a reconsideration in favor of more effective and cost-saving sedative agents.
Medication failures due to adverse events were not accounted for in this analysis. However, as reported by Cox et al, the economic advantage of propofol is much more sensitive to ICU recovery times rather than intolerance to propofol or treatment failure.24 Furthermore, our analysis and all previously published analyses attempted to evaluate the level of savings per patient. Future studies should examine and evaluate such savings at macro levels ranging from single small ICU departments to the national level. This could be done by multiplying savings per patient with the size of the eligible population which could be prescribed propofol instead of benzodiazepines.
Conclusion
In the meta-analysis this work is based on, propofol was shown to be significantly more efficient compared to benzodiazepines in facilitating recovery from sedation and mechanical ventilation. This economic analysis demonstrates that propofol short- and long-term sedation is also cost saving compared to benzodiazepine sedation, even when uncertainties in input variables and different national settings are taken into account.
Acknowledgments
We thank Fresenius Kabi Deutschland GmbH for supporting this publication with an unrestricted educational grant to AdRes HE&OR for statistical analysis and modeling. We would like to acknowledge Dr Marco Bellone and Dr Orietta Zaniolo, AdRes Health, Torino, for statistical support with the meta-analysis, Mahmoud Hashim from AdRes Health, for critically reviewing the economic model, and Antonio Aliano from AdRes Health, for early collaboration on the project. Furthermore, we thank Dr Mario Pahl and Dr Aike Schweda, DBM Wissen schafft GmbH, Mühlhausen, Germany, who helped with medical writing funded by Fresenius Kabi Deutschland GmbH.
Author contributions
LP wrote the study plan and guided the modeling process. LP and MP conducted the literature search, extracted the data, and conducted the meta-analysis. MP constructed the final base case models and sensitivity analyses for all countries. LP and MP wrote the manuscript draft. All authors contributed to the study conception and design, data analysis and interpretation, and critically revised the manuscript. All authors approved the final version for publication and agree to be accountable for all aspects of the work.
Disclosure
LP is a co-owner and employee of AdRes HE&OR, which has received an educational grant from Fresenius Kabi for this project. LP has also received speaker honoraria and travel expenses refund for participating at scientific events. MP is an employee of AdRes. HB received a single honorarium from Fresenius Kabi as an invited speaker and chair of symposium in 2014. TGK received honoraria as a consultant as well as travel reimbursement from Fresenius Kabi. AF, JFB, and MW are employees of Fresenius Kabi. GDR reports no conflicts of interest in this work.
References
Lewis KS, Whipple JK, Michael KA, Quebbeman EJ. Effect of analgesic treatment on the physiological consequences of acute pain. Am J Hosp Pharm. 1994;51(12):1539–1554. | ||
Conti G, Mercurio G, Iacobone E, Auricchio D, Liberati Q. Sedation in the intensive care unit. The basis of the problem. Minerva Anestesiol. 2002;68(4):240–244. | ||
Smith I, Monk TG, White PF, Ding Y. Propofol infusion during regional anesthesia: sedative, amnestic, and anxiolytic properties. Anesth Analg. 1994;79(2):313–319. | ||
Blackwood B, Alderdice F, Burns K, Cardwell C, Lavery G, O’Halloran P. Use of weaning protocols for reducing duration of mechanical ventilation in critically ill adult patients: Cochrane systematic review and meta-analysis. BMJ. 2011;342:c7237. | ||
Branson RD. Modes to facilitate ventilator weaning. Respir Care. 2012;57(10):1635–1648. | ||
Moerer O, Plock E, Mgbor U, et al. A German national prevalence study on the cost of intensive care: an evaluation from 51 intensive care units. Crit Care. 2007;11(3):R69. | ||
Wild C, Narath M. Evaluating and planning ICUs: methods and approaches to differentiate between need and demand. Health Policy. 2005;71(3):289–301. | ||
Reves JG, Fragen RJ, Vinik HR, Greenblatt DJ. Midazolam: pharmacology and uses. Anesthesiology. 1985;62(3):310–324. | ||
Gommers D, Bakker J. Medications for analgesia and sedation in the intensive care unit: an overview. Crit Care. 2008;12 (Suppl 3):S4. | ||
Marik PE. Propofol: therapeutic indications and side-effects. Curr Pharm Des. 2004;10(29):3639–3649. | ||
McKeage K, Perry CM. Propofol: a review of its use in intensive care sedation of adults. CNS Drugs. 2003;17(4):235–272. | ||
Vanlersberghe C, Camu F. Propofol. Handb Exp Pharmacol. 2008;(182):227–252. | ||
Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263–306. | ||
Baron R, Binder A, Biniek R, et al. Evidence and consensus based guideline for the management of delirium, analgesia, and sedation in intensive care medicine. Revision 2015 (DAS-guideline 2015) – short version. Ger Med Sci. 2015;13:Doc19. | ||
Ho KM, Ng JY. The use of propofol for medium and long-term sedation in critically ill adult patients: a meta-analysis. Intensive Care Med. 2008;34(11):1969–1979. | ||
McCollam JS, O’Neil MG, Norcross ED, Byrne TK, Reeves ST. Continuous infusions of lorazepam, midazolam, and propofol for sedation of the critically ill surgery trauma patient: a prospective, randomized comparison. Crit Care Med. 1999;27(11):2454–2458. | ||
Barrientos-Vega R, Mar Sanchez-Soria M, Morales-Garcia C, Robas-Gomez A, Cuena-Boy R, Ayensa-Rincon A. Prolonged sedation of critically ill patients with midazolam or propofol: impact on weaning and costs. Crit Care Med. 1997;25(1):33–40. | ||
Carrasco G, Molina R, Costa J, Soler JM, Cabre L. Propofol vs midazolam in short-, medium-, and long-term sedation of critically ill patients. A cost–benefit analysis. Chest. 1993;103(2):557–564. | ||
Barrientos-Vega R, Sanchez-Soria MM, Morales-Garcia C, Cuena-Boy R, Castellano-Hernandez M. Pharmacoeconomic assessment of propofol 2% used for prolonged sedation. Crit Care Med. 2001;29(2):317–322. | ||
Manley NM, Fitzpatrick RW, Long T, Jones PW. A cost analysis of alfentanil+propofol vs morphine+midazolam for the sedation of critically ill patients. Pharmacoeconomics. 1997;12(2 Pt 2):247–255. | ||
Sherry KM, McNamara J, Brown JS, Drummond M. An economic evaluation of propofol/fentanyl compared with midazolam/fentanyl on recovery in the ICU following cardiac surgery. Anaesthesia. 1996;51(4):312–317. | ||
Bioc JJ, Magee C, Cucchi J, et al. Cost effectiveness of a benzodiazepine vs a nonbenzodiazepine-based sedation regimen for mechanically ventilated, critically ill adults. J Crit Care. 2014;29(5):753–757. | ||
MacLaren R, Sullivan PW. Pharmacoeconomic modeling of lorazepam, midazolam, and propofol for continuous sedation in critically ill patients. Pharmacotherapy. 2005;25(10):1319–1328. | ||
Cox CE, Reed SD, Govert JA, et al. Economic evaluation of propofol and lorazepam for critically ill patients undergoing mechanical ventilation. Crit Care Med. 2008;36(3):706–714. | ||
Muellejans B, Matthey T, Scholpp J, Schill M. Sedation in the intensive care unit with remifentanil/propofol versus midazolam/fentanyl: a randomised, open-label, pharmacoeconomic trial. Crit Care. 2006;10(3):R91. | ||
Anis AH, Wang X, Leon H, Hall R. Economic evaluation of propofol for sedation of patients admitted to intensive care units. Anesthesiology. 2002;96(1):196–201. | ||
Zhou Y, Jin X, Kang Y, Liang G, Liu T, Deng N. Midazolam and propofol used alone or sequentially for long-term sedation in critically ill, mechanically ventilated patients: a prospective, randomized study. Crit Care. 2014;18(3):R122. | ||
Hannan EL. Randomized clinical trials and observational studies: guidelines for assessing respective strengths and limitations. JACC Cardiovasc Interv. 2008;1(3):211–217. | ||
Aitkenhead AR, Pepperman ML, Willatts SM, et al. Comparison of propofol and midazolam for sedation in critically ill patients. Lancet. 1989;2(8665):704–709. | ||
Carrasco G, Cabre L, Sobrepere G, et al. Synergistic sedation with propofol and midazolam in intensive care patients after coronary artery bypass grafting. Crit Care Med. 1998;26(5):844–851. | ||
Carson SS, Kress JP, Rodgers JE, et al. A randomized trial of intermittent lorazepam versus propofol with daily interruption in mechanically ventilated patients. Crit Care Med. 2006;34(5):1326–1332. | ||
Costa J, Cabre L, Molina R, Carrasco G. Cost of ICU sedation: comparison of empirical and controlled sedation methods. Clin Intensive Care. 1994;5(5 Suppl):17–21. | ||
Degauque C, Dupuis A. A study to compare the use of propofol and midazolam for the sedation of patients with acute respiratory failure. J Drug Dev. 1991;4(4):95–97. | ||
Ghori KA, Harmon DC, Elashaal A, et al. Effect of midazolam versus propofol sedation on markers of neurological injury and outcome after isolated severe head injury: a pilot study. Crit Care Resusc. 2007;9(2):166–171. | ||
Grounds RM, Lalor JM, Lumley J, Royston D, Morgan M. Propofol infusion for sedation in the intensive care unit: preliminary report. BMJ. 1987;294(6569):397–400. | ||
Hall RI, Sandham D, Cardinal P, et al. Propofol vs midazolam for ICU sedation: a Canadian multicenter randomized trial. Chest. 2001;119(4):1151–1159. | ||
Higgins TL, Yared JP, Estafanous FG, Coyle JP, Ko HK, Goodale DB. Propofol versus midazolam for intensive care unit sedation after coronary artery bypass grafting. Crit Care Med. 1994;22(9):1415–1423. | ||
Huey-Ling L, Chun-Che S, Jen-Jen T, Shau-Ting L, Hsing-I C. Comparison of the effect of protocol-directed sedation with propofol vs. midazolam by nurses in intensive care: efficacy, haemodynamic stability and patient satisfaction. J Clin Nurs. 2008;17(11):1510–1517. | ||
Kress JP, Pohlman AS, Hall JB. Effects of sedative interruption in critically ill, mechanically ventilated patients receiving midazolam or propofol. J Clin Outcomes Manage. 2001;8(2):33–39. | ||
McMurray TJ, Collier PS, Carson IW, Lyons SM, Elliott P. Propofol sedation after open heart surgery. A clinical and pharmacokinetic study. Anaesthesia. 1990;45(4):322–326. | ||
Mesnil M, Capdevila X, Bringuier S, et al. Long-term sedation in intensive care unit: a randomized comparison between inhaled sevoflurane and intravenous propofol or midazolam. Intensive Care Med. 2011;37(6):933–941. | ||
Michalopoulos A, Nikolaides A, Antzaka C, et al. Change in anaesthesia practice and postoperative sedation shortens ICU and hospital length of stay following coronary artery bypass surgery. Respir Med. 1998;92(8):1066–1070. | ||
Roekaerts PM, Huygen FJ, de Lange S. Infusion of propofol versus midazolam for sedation in the intensive care unit following coronary artery surgery. J Cardiothorac Vasc Anesth. 1993;7(2):142–147. | ||
Ruokonen E, Parviainen I, Jakob SM, et al. Dexmedetomidine versus propofol/midazolam for long-term sedation during mechanical ventilation. Intensive Care Med. 2009;35(2):282–290. | ||
Sanchez-Izquierdo-Riera JA, Caballero-Cubedo RE, Perez-Vela JL, Ambros-Checa A, Cantalapiedra-Santiago JA, Alted-Lopez E. Propofol versus midazolam: safety and efficacy for sedating the severe trauma patient. Anesth Analg. 1998;86(6):1219–1224. | ||
Sandiumenge Camps A, Sanchez-Izquierdo Riera JA, Toral Vazquez D, Sa Borges M, Peinado Rodriguez J, Alted Lopez E. Midazolam and 2% propofol in long-term sedation of traumatized critically ill patients: efficacy and safety comparison. Crit Care Med. 2000;28(11):3612–3619. | ||
Searle NR, Cote S, Taillefer J, et al. Propofol or midazolam for sedation and early extubation following cardiac surgery. Can J Anaesth. 1997;44(6):629–635. | ||
Snellen F, Lauwers P, Demeyere R, Byttebier G, van Aken H. The use of midazolam versus propofol for short-term sedation following coronary artery bypass grafting. Intensive Care Med. 1990;16(5):312–316. | ||
Weinbroum AA, Rudick V, Sorkine P, Freedman M, Geller E, Halpern P. Midazolam versus propofol for long-term sedation in the ICU: a randomized prospective comparison. Intensive Care Med. 1997;23(12):1258–1263. | ||
Corbett SM, Rebuck JA, Greene CM, et al. Dexmedetomidine does not improve patient satisfaction when compared with propofol during mechanical ventilation. Crit Care Med. 2005;33(5):940–945. | ||
Herr DL, Sum-Ping ST, England JM. ICU sedation after coronary artery bypass graft surgery: dexmedetomidine-based versus propofol-based sedation regimens. J Cardiothorac Vasc Anesth. 2003;17(5):576–584. | ||
Maldonado JR, Wysong A, van der Starre PJ, Block T, Miller C, Reitz BA. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics. 2009;50(3):206–217. | ||
Venn RM, Grounds RM. Comparison between dexmedetomidine and propofol for sedation in the intensive care unit: patient and clinician perceptions. Br J Anaesth. 2001;87(5):684–690. | ||
DeBellis P, Gerbi G, Bacigalupo P, et al. Esperienza con remifentanil in Terapia Intensiva. [Experience with remifentanil in the ICU]. Minerva Anestesiol. 2002;68(10):765–773. Italian. | ||
Fong JJ, Kanji S, Dasta JF, Garpestad E, Devlin JW. Propofol associated with a shorter duration of mechanical ventilation than scheduled intermittent lorazepam: a database analysis using Project IMPACT. Ann Pharmacother. 2007;41(12):1986–1991. | ||
Kuru T, Alaniz C, Kewman S, Brach L, Strachan C, Watts C. Choice of sedative agent in patients with acute respiratory distress syndrome receiving low tidal volume mechanical ventilation (POSTER). Crit Care Med. 1999;27(12):A133. | ||
Park G, Lane M, Rogers S, Bassett P. A comparison of hypnotic and analgesic based sedation in a general intensive care unit. Br J Anaesth. 2007;98(1):76–82. | ||
Anger KE, Szumita PM, Baroletti SA, Labreche MJ, Fanikos J. Evaluation of dexmedetomidine versus propofol-based sedation therapy in mechanically ventilated cardiac surgery patients at a tertiary academic medical center. Crit Pathw Cardiol. 2010;9(4):221–226. | ||
Barletta JF, Miedema SL, Wiseman D, Heiser JC, McAllen KJ. Impact of dexmedetomidine on analgesic requirements in patients after cardiac surgery in a fast-track recovery room setting. Pharmacotherapy. 2009;29(12):1427–1432. | ||
Reichert MG, Jones WA, Royster RL, Slaughter TF, Kon ND, Kincaid EH. Effect of a dexmedetomidine substitution during a nationwide propofol shortage in patients undergoing coronary artery bypass graft surgery. Pharmacotherapy. 2011;31(7):673–677. | ||
Briggs AH, Weinstein MC, Fenwick EA, Karnon J, Sculpher MJ, Paltiel AD. Model parameter estimation and uncertainty: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-6. Value Health. 2012;15(6):835–842. | ||
Sistan, Comune di Ferrara, Statistica. L’abitudine al fumo e l’obesita’: Fattori di rischio per la salute. 2009. [Statistics Service of the Town of Ferrara. Smoking habit and obesity: health risk factors]. Published 2010. Available from: http://servizi.comune.fe.it/attach/statistica/docs/informanumeri_abitudine_al_fumo_2009.pdf. Accessed June 19, 2015. | ||
Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. 2005;33(6):1266–1271. | ||
Tarricone R, Torbica A, Franzetti F, Rosenthal VD. Hospital costs of central line-associated bloodstream infections and cost-effectiveness of closed vs. open infusion containers. The case of intensive care units in Italy. Cost Eff Resour Alloc. 2010;8:8. | ||
Tan SS, Bakker J, Hoogendoorn ME, et al. Direct cost analysis of intensive care unit stay in four European countries: applying a standardized costing methodology. Value Health. 2012;15(1):81–86. | ||
Le service public de la diffusion du droit. Decree of 22 February 2013 fixing for 2013 the tariff items mentioned in I and IV of Article L. 162-22-10 of the security code social and IV and V of Article 33 amended the Social Security Financing Act for 2004. Published 2013. Available from: http://legifrance.gouv.fr/eli/arrete/2013/2/22/AFSH1305231A/jo/texte. Accessed June 19, 2015. | ||
Walder B, Elia N, Henzi I, Romand JR, Tramer MR. A lack of evidence of superiority of propofol versus midazolam for sedation in mechanically ventilated critically ill patients: a qualitative and quantitative systematic review. Anesth Analg. 2001;92(4):975–983. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.