Back to Journals » OncoTargets and Therapy » Volume 13
Prognostic Value of the Preoperative Lymphocyte-to-C-Reactive Protein Ratio and Albumin-to-Globulin Ratio in Patients with Osteosarcoma
Authors Hu H, Deng X, Song Q , Lv H, Chen W, Xing X, Zhu J, Tan Z, Cheng X, Wang B, Shao Z, Zhang Y
Received 16 October 2020
Accepted for publication 26 November 2020
Published 9 December 2020 Volume 2020:13 Pages 12673—12681
DOI https://doi.org/10.2147/OTT.S287192
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Federico Perche
Hongzhi Hu,1,2,* Xiangtian Deng,2,3,* Qingcheng Song,2,* Hongzhi Lv,2 Wei Chen,2 Xin Xing,2 Jian Zhu,2,3 Zhanchao Tan,2 Xiaodong Cheng,2 Baichuan Wang,1 Zengwu Shao,1 Yingze Zhang1,2
1Department of Orthopaedics, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, People’s Republic of China; 2Department of Orthopaedic Surgery, The Third Hospital of Hebei Medical University, Shijazhuang 050051, People’s Republic of China; 3School of Medicine, Nankai University, Tianjin 300071, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yingze Zhang; Zengwu Shao Tel +86 18533112888
; 86 13971021748
Email [email protected] [email protected]
Purpose: Growing evidence indicates that preoperative biomarkers could be identified as independent prognostic factors in various cancers. The purpose of this study was to assess prognostic value of the preoperative lymphocyte-to-C-reactive protein ratio (LCR), albumin-to-globulin ratio (AGR), lymphocyte–monocyte ratio (LMR), and C-reactive protein to albumin ratio (CAR) in patients with osteosarcoma.
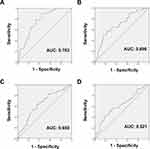
Methods: A total of 137 osteosarcoma patients treated at our hospital between 2011 and 2019 were enrolled in the study. Patient demographics, clinical characteristics, and laboratory data were collected and analyzed. The optimal cutoff values of LCR, AGR, LMR, and CAR were assessed with receiver operating characteristic (ROC) analysis. Kaplan–Meier analysis was performed to estimate overall survival (OS). Univariate and multivariate Cox regression models were employed to determine the independent prognostic factors. The hazard ratios (HR) and 95% confidence intervals (95% CI) were calculated to evaluate relative risk.
Results: The optimal cutoff values of LCR, AGR, LMR, and CAR were 0.14, 1.79, 3.05 and 0.24, respectively. According to the univariate analysis, OS was remarkably associated with neoadjuvant chemotherapy (P < 0.001), pathological fracture (P < 0.001), local recurrence (P = 0.020), metastasis (P < 0.001), LCR (P = 0.035), AGR (P = 0.028), LMR (P = 0.010), and CAR (P = 0.004). In multivariate analyses, pathological fracture (P = 0.025), metastasis (P < 0.001), LCR (P = 0.012), and AGR (P = 0.001) were identified as independent risk predictors for OS.
Conclusion: The present study provides new evidence that the preoperative LCR and AGR could serve as independent prognostic factors for patients with osteosarcoma. These findings will help physicians to stratify patients for appropriate treatment protocols and facilitate decision-making so as to improve the patients’ survival condition.
Keywords: osteosarcoma, biomarker, albumin-to-globulin ratio, C-reactive protein, lymphocyte, prognosis
Background
Osteosarcoma, predominantly affecting children and adolescents, is the most common primary malignant bone tumor with a poor prognosis.1,2 Standard therapy consists of cycles of neoadjuvant chemotherapy followed by surgical resection, with subsequent several continuation cycles of adjuvant chemotherapy.3 With advances in multi-disciplinary treatment, the 5-year overall survival (OS) of patients with osteosarcoma has improved significantly.4 However, the overall oncological outcome of osteosarcoma patients remains unsatisfactory, especially in those with local recurrence and distant metastasis.5 The conventionally established prognostic parameters for osteosarcoma such as tumor size, alkaline phosphatase, lactate dehydrogenase, have been demonstrated to be inherently inaccurate and inadequate for prognostic prediction.6–11 Therefore, there is an urgent need to explore more powerful, comprehensive, and multidimensional predictors to provide additional prognostic information.
Systemic inflammatory responses and nutritional status are associated with the development and progression of malignancies.12–15 Previous studies have confirmed the relationship between inflammation and nutrition, and the systemic inflammation was reported to lead to a worse nutritional status, thus resulting in a poor prognosis in cancer patients.16–20 Numerous studies have evaluated the potential of systemic inflammatory markers based on blood examination to serve as prognostic biomarkers in various cancer patients, including osteosarcoma.21–24 Previous studies have indicated that preoperative biomarkers, including lymphocyte–monocyte ratio (LMR), Glasgow prognostic score (GPS), C-reactive protein to albumin ratio (CAR), neutrophil–lymphocyte ratio (NLR), systemic immune-inflammation index (SII), prognostic nutritional index (PNI), and neutrophil–platelet score (NPS), might be effective prognostic parameters to assess clinical features and prognosis of patients with osteosarcoma.11,22,25–27 However, the prognostic significance of the preoperative lymphocyte-to-C-reactive protein ratio (LCR) and albumin-to-globulin ratio (AGR) in osteosarcoma has not been elucidated.
Accumulating evidence has assessed the pivotal role of preoperative LCR and AGR on predicting survival benefits in various cancers.16,23,28,29 Therefore, we performed the retrospective study to evaluate the prognostic value of the two factors in our patients with osteosarcoma. In addition, other inflammatory indicators in osteosarcoma patients, such as LMR and CAR, were also investigated.
Methods
Patients and Study Design
The study protocol was approved by Ethics committee of the Third Hospital of Hebei Medical University. All the patients gave written informed consent to review their clinical records. In addition, parental or legal guardian informed consent was obtained for any patient under the age of 18 years, and that this study was conducted in accordance with the Declaration of Helsinki.
A total of 137 osteosarcoma patients treated at our hospital between January 2011 and August 2019 were enrolled in the study. Participants were included if they (1) were pathologically confirmed osteosarcoma; (2) did not receive any previous anti-cancer treatment; (3) had detailed medical records and laboratory results; and (4) had regular medical follow-up. The participants in the following conditions were excluded: (1) patients with clinical evidence of immune disease, hematologic diseases, infection or other inflammatory diseases; (2) patients with a history of nonsteroidal anti-inflammatory drugs (NSAIDs) use within 3 months; and (3) patients with incomplete medical records.
Data Collection and Definition
All the medical records and clinical information of the patients were extracted independently by three authors (HZH, XTD and QCS). The following clinical parameters were collected from the medical data: age, sex, tumor localization, Enneking stage, presence of pathological fracture, local recurrence, metastasis, neoadjuvant chemotherapy, and laboratory test results (including albumin level, CRP, neutrophil count, platelet count, and lymphocyte count).
Preoperative blood samples from each patient were obtained within 2 weeks before operation. The calculation formulas of LCR, AGR, LMR, and CAR22,23,29–31 were described as follows: LCR = lymphocyte count (number/L)/CRP (mg/L), AGR = albumin/(total serum protein – albumin). LMR = lymphocyte count (number/L)/monocyte (number/L), and CAR = CRP (mg/L)/albumin (g/L).
Follow-Up
Routine follow-up of all patients after operation was performed every month for the first 3 months after surgery, then every 6 months for the next 2 years, and annually thereafter. The routine examinations during the follow-up included physical examination, surgical site X-ray, and laboratory tests. Chest computed tomography (CT) scan was performed every 3 months and bone scan was conducted every 6 months to detect potential metastases. Tumor responses were evaluated by CT/magnetic resonance imaging (MRI) scans using the Response Evaluation Criteria in Solid Tumors (RECIST).32 OS, the main end point, was defined as the time from the date of surgery to the latest follow-up of this study (August 2020) or death.
Statistical Analysis
All statistical analyses were performed by using SPSS 20.0 (IBM Corporation, Armonk, NY, USA). Categorical variables were presented as frequencies and percentages were analyzed by the chi‐squared test or Fisher’s exact test as applicable. The optimal cutoff values of the inflammation-based prognostic variables were defined according to a receiver operating characteristic (ROC) curve. Survival analysis was performed by using the Kaplan–Meier method, and a Log rank test was used to determine significance. Univariate and multivariate Cox regression models were performed to determine the independent prognostic factors. The hazard ratios (HR) and 95% confidence intervals (95% CI) were utilized to evaluate relative risk. A two-tailed P-value < 0.05 was defined as statistically significant.
Results
Clinical Characteristics of Patients
The clinical characteristics of the patients are demonstrated in Table 1. According to the inclusion criteria, a total of 137 patients were enrolled in the current study, including 80 males and 57 females, the median age at diagnose was 26 years (range, 9–82). Among all the patients, majority of the tumors were located in extremities (82.5%). One hundred and three patients were in Enneking stage I/II (75.2%) and 34 patients were in stage III (24.8%), respectively. Pathological fracture was presented in 34 patients (24.8%). Furthermore, tumor recurrence and metastasis occurred in 24 and 61 patients, respectively. In all, 122 patients (89.1%) were received the neoadjuvant chemotherapy, and all the enrolled patients received adjuvant chemotherapy after surgery.
 |
Table 1 Clinicopathological Characteristics of Patients |
Identification of Optimal Cutoff Values for LCR, AGR, LMR and CAR
ROC analyses were performed to identify the optimal cutoff value of each predictor for survival analysis. As shown in Figure 1, the areas under the curve (AUC) for survival were 0.763 (95% CI 0.683–0.843, P < 0.001), 0.690 (95% CI 0.602–0.779, P < 0.001), 0.650 (95% CI 0.558–0.742, P = 0.002), and 0.621 (95% CI 0.527–0.715, P = 0.014) for LCR, AGR, LMR and CAR, respectively. Based on the maximum Youden index, the optimal cutoff values were recognized as 0.14 (Youden index of 0.457) for LCR, 1.79 (Youden index of 0.345) for AGR, 3.05 (Youden index of 0.270) for LMR, and 0.24 (Youden index of 0.24) for CAR, respectively.
Association of Clinical Characteristics with Preoperative LCR, AGR, LMR and CAR
The relationship between these inflammation-based biomarkers and characteristics is shown in Table 1. The results suggested that preoperative LCR was significantly related with Enneking stage (P < 0.001), neoadjuvant chemotherapy (P < 0.001), pathological fracture (P < 0.001), local recurrence (P < 0.001) and metastasis (P < 0.001). Nevertheless, there were no great differences between preoperative LCR and age, sex, and tumor site. Similarly, a significant relationship between preoperative AGR and tumor site (P = 0.037), pathological fracture (P < 0.001), and metastasis (P < 0.001) was detected in our study. However, no significant correlations were found between preoperative AGR and age, sex, Enneking stage, neoadjuvant Chemotherapy, and local recurrence.
In addition, our study also revealed that preoperative LMR and CAR were dramatically associated with neoadjuvant Chemotherapy, pathological fracture local recurrence, and metastasis (P < 0.05). Whereas distribution of age, sex, tumor site and Enneking stage did not differ significantly among these two groups.
Univariate and Multivariate Survival Analyses
The average time of follow-up was 55 (range, 4–112) months. As displayed in Figure 2, the survival curves revealed that patients with higher LCR, AGR, and LMR had obviously better OS than those with lower LCR (P < 0.001), AGR (P < 0.001), and LMR (P = 0.008). However, patients with lower CAR were markedly associated with improved OS (P = 0.003).
According to the univariate analysis, OS was closely associated with neoadjuvant chemotherapy (P < 0.001), pathological fracture (P < 0.001), local recurrence (P = 0.020), metastasis (P < 0.001), LCR (P = 0.035), AGR (P = 0.028), LMR (P = 0.010), and CAR (P = 0.004). Furthermore, the variables with significance in univariate analysis were selected to identify the independent prognostic factors for OS in multivariate analysis. The results revealed that pathological fracture (HR = 2.605, 95% CI 1.130–6.005, P = 0.025), metastasis (HR = 2.876, 95% CI 1.608–5.147, P < 0.001), LCR (HR = 0.349, 95% CI 0.154–0.791, P =0.012), and AGR (HR = 0.351, 95% CI 0.184–0.668, P = 0.001) were independent risk predictors for OS (Table 2).
 |
Table 2 Univariate and Multivariate Cox Regression Analyses of Factors Associated with Overall Survival |
Discussion
The progression of malignancies is not only related to the intrinsic characteristics of tumor cells but is also associated with the systemic inflammatory response and body’s immunonutritional status.16,33,34 In cancer patients, the systemic inflammation can result in a worse nutritional status which will slowly lead the patients into cachexia.35 Systemic inflammation caused by complex host–tumor interactions exerts a critical role in the development of disease in patients with cancers.34 The inflammatory response in cancer might be involved in the hypoxia, local tissue damage, cancer progression, angiogenesis, and malignant transformation.14,36,37 The poor nutritional condition, related with the immune-suppressed condition, will contribute to the cancer development.38,39 Therefore, understanding the patient’s systemic inflammatory response and nutritional status can allow researchers to stratify the prognosis of cancer patients.
Various preoperative markers, such as PNI, SII, NIR, LCR, AGR, LMR, and CAR, have been employed to reflect the cancer-related systemic inflammation and immunonutritional status.16,23,25,31,40 Recent studies have displayed that the preoperative LCR could reflect both the immunological response and systemic inflammation in cancer patients.23,28,41 Serum CRP (C-reactive protein to albumin ratio), as a well-established inflammatory marker, has been demonstrated to exert an essential role in tumor development. The high preoperative CRP level was shown to be associated with a poor prognosis in cancer patients.42,43 On the contrary, peripheral lymphocytes play a formative role in host cell immune response against tumors.44 A recent multicenter study revealed that pre-operative LCR could effectively predict the short- and long-term oncological outcome for gastric cancer (GC) patients undergoing radical gastrectomy.41 Moreover, Okugawa et al23 also demonstrated that the preoperative LCR was an independent prognostic factor for both the disease-free survival (DFS) and OS in GC patients. However, no relevant studies have reported the prognostic role of preoperative LCR in patients with osteosarcoma.
Similarly, serum albumin and globulin can also be used to reflect the systemic inflammation and nutritional status.45,46 Low albumin and elevated globulin levels were reported to reflect impaired immunonutritional status, which was involved in cancer progression and metastasis.45,47 AGR, which combines albumin and globulin, is associated with nutritional status and systemic inflammation in cancer patients.48 The low preoperative AGR value is correlated with several clinicopathological variables related to tumor progression and could be utilized to identify cancer patients with poor prognosis.16,29 The prognostic value of the AGR has been evaluated in numerous cancers, such as glioblastoma,16 non-small-cell lung cancer,29 esophageal cancer.49 However, little was known about the prognostic value of the preoperative AGR in patients with osteosarcoma.
According to these pieces of evidence mentioned above, we hypothesized that malnutrition and systematic inflammation are inseparable for predicting prognosis of patients with osteosarcoma. In this study, we systemically evaluated the clinical significance and prognostic value of preoperative markers, including LCR, AGR, LMR and CAR, in 137 osteosarcoma patients. Consistent with the findings in other studies,23,26,27,29 high levels of preoperative LCR, AGR, LMR, and low level of CAR were significantly correlated with favorable prognosis (P < 0.05) in our study. Of note, multivariate analysis revealed that low preoperative LCR and AGR were independent prognostic factors for OS in patients with osteosarcoma. To our knowledge, this is the first study to evaluate the prognostic value of LCR and AGR in patients with osteosarcoma. However, whether these two indicators could be incorporated into cancer patients’ stratification system to guide individualized or personalized therapy still needs to be further confirmed in future prospective studies.
There were several limitations in this study that should be clarified. Firstly, it was a retrospective, single-center study. Secondly, some other unknown physiological and pathophysiological factors that could inevitably influence LCR and AGR were not evaluated. In addition, the sample size enrolled in our study is relatively small. This may be greatly due to the relatively low incidence of osteosarcoma compared to other common malignancies. Therefore, further investigations involving multicenter prospective randomized controlled studies and large sample size should be conducted to confirm our findings.
In conclusion, despite the limitations mentioned above, our study remains informative. The present study provides new evidence that the preoperative LCR and AGR could serve as effective and independent prognostic indicators for patients with osteosarcoma. These findings will help physicians to stratify patients for appropriate treatment protocols and facilitate decision-making so as to improve the patients’ survival condition.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Luetke A, Meyers PA, Lewis I, Juergens H. Osteosarcoma treatment - where do we stand? A state of the art review. Cancer Treat Rev. 2014;40(4):523–532. doi:10.1016/j.ctrv.2013.11.006
2. Li M, Jin X, Li H, Yang C, Deng S, Wu G. Comprehensive analysis of key genes and regulatory elements in osteosarcoma affected by bone matrix mineral with prognostic values. Front Genet. 2020;11:533. doi:10.3389/fgene.2020.00533
3. Janeway KA, Grier HE. Sequelae of osteosarcoma medical therapy: a review of rare acute toxicities and late effects. Lancet Oncol. 2010;11(7):670–678. doi:10.1016/S1470-2045(10)70062-0
4. Bielack SS, Kempf-Bielack B, Delling G, et al. Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol. 2002;20(3):776–790. doi:10.1200/JCO.2002.20.3.776
5. Zhu N, Hou J, Ma G, Guo S, Zhao C, Chen B. Co-expression network analysis identifies a gene signature as a predictive biomarker for energy metabolism in osteosarcoma. Cancer Cell Int. 2020;20:259. doi:10.1186/s12935-020-01352-2
6. Yang M. Prognostic role of pathologic fracture in osteosarcoma: evidence based on 1677 subjects. J Cancer Res Ther. 2015;11(2):264–267. doi:10.4103/0973-1482.151428
7. Kaste SC, Liu T, Billups CA, Daw NC, Pratt CB, Meyer WH. Tumor size as a predictor of outcome in pediatric non-metastatic osteosarcoma of the extremity. Pediatr Blood Cancer. 2004;43(7):723–728. doi:10.1002/pbc.20077
8. Buddingh EP, Anninga JK, Versteegh MI, et al. Prognostic factors in pulmonary metastasized high-grade osteosarcoma. Pediatr Blood Cancer. 2010;54(2):216–221. doi:10.1002/pbc.22293
9. Ren HY, Sun LL, Li HY, Ye ZM. Prognostic significance of serum alkaline phosphatase level in osteosarcoma: a meta-analysis of published data. Biomed Res Int. 2015;2015:160835. doi:10.1155/2015/160835
10. Marais LC, Bertie J, Rodseth R, Sartorius B, Ferreira N. Pre-treatment serum lactate dehydrogenase and alkaline phosphatase as predictors of metastases in extremity osteosarcoma. J Bone Oncol. 2015;4(3):80–84. doi:10.1016/j.jbo.2015.09.002
11. Yang Q, Chen T, Yao Z, Zhang X. Prognostic value of pre-treatment Naples prognostic score (NPS) in patients with osteosarcoma. World J Surg Oncol. 2020;18(1):24. doi:10.1186/s12957-020-1789-z
12. Mellman I, Coukos G, Dranoff G. Cancer immunotherapy comes of age. Nature. 2011;480(7378):480–489. doi:10.1038/nature10673
13. Kanda M, Mizuno A, Tanaka C, et al. Nutritional predictors for postoperative short-term and long-term outcomes of patients with gastric cancer. Medicine (Baltimore). 2016;95(24):e3781. doi:10.1097/MD.0000000000003781
14. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–444. doi:10.1038/nature07205
15. Dinc T, Yildiz BD, Kayilioglu I, Sozen I, Tez M, Coskun F. Prognostic value of preoperative inflammation-based prognostic scores on hospital mortality after gastric cancer surgery. Asian Pac J Cancer Prev. 2014;15(18):7909–7911. doi:10.7314/APJCP.2014.15.18.7909
16. Xu WZ, Li F, Xu ZK, et al. Preoperative albumin-to-globulin ratio and prognostic nutrition index predict prognosis for glioblastoma. Onco Targets Ther. 2017;10:725–733. doi:10.2147/OTT.S127441
17. Li K, Xu Y, Hu Y, Liu Y, Chen X, Zhou Y. Effect of enteral immunonutrition on immune, inflammatory markers and nutritional status in gastric cancer patients undergoing gastrectomy: a randomized double-blinded controlled trial. J Invest Surg. 2019. doi:10.1080/08941939.2019.1569736
18. Alifano M, Mansuet-Lupo A, Lococo F, et al. Systemic inflammation, nutritional status and tumor immune microenvironment determine outcome of resected non-small cell lung cancer. PLoS One. 2014;9(9):e106914. doi:10.1371/journal.pone.0106914
19. Giannousi Z, Gioulbasanis I, Pallis AG, et al. Nutritional status, acute phase response and depression in metastatic lung cancer patients: correlations and association prognosis. Support Care Cancer. 2012;20(8):1823–1829. doi:10.1007/s00520-011-1282-x
20. Sánchez-Lara K, Turcott JG, Juárez E, et al. Association of nutrition parameters including bioelectrical impedance and systemic inflammatory response with quality of life and prognosis in patients with advanced non-small-cell lung cancer: a prospective study. Nutr Cancer. 2012;64(4):526–534. doi:10.1080/01635581.2012.668744
21. Toiyama Y, Shimura T, Yasuda H, et al. Clinical burden of C-reactive protein/albumin ratio before curative surgery for patients with gastric cancer. Anticancer Res. 2016;36(12):6491–6498. doi:10.21873/anticanres.11248
22. Li YJ, Yao K, Lu MX, Zhang WB, Xiao C, Tu CQ. Prognostic value of the C-reactive protein to albumin ratio: a novel inflammation-based prognostic indicator in osteosarcoma. Onco Targets Ther. 2017;10:5255–5261. doi:10.2147/OTT.S140560
23. Okugawa Y, Toiyama Y, Yamamoto A, et al. Lymphocyte-to-C-reactive protein ratio and score are clinically feasible nutrition-inflammation markers of outcome in patients with gastric cancer. Clin Nutr (Edinburgh, Scotland). 2020;39(4):1209–1217. doi:10.1016/j.clnu.2019.05.009
24. Saito H, Kono Y, Murakami Y, et al. Prognostic significance of the preoperative ratio of C-reactive protein to albumin and neutrophil-lymphocyte ratio in gastric cancer patients. World J Surg. 2018;42(6):1819–1825. doi:10.1007/s00268-017-4400-1
25. Huang X, Hu H, Zhang W, Shao Z. Prognostic value of prognostic nutritional index and systemic immune-inflammation index in patients with osteosarcoma. J Cell Physiol. 2019;234(10):18408–18414. doi:10.1002/jcp.28476
26. Liu B, Huang Y, Sun Y, et al. Prognostic value of inflammation-based scores in patients with osteosarcoma. Sci Rep. 2016;6:39862. doi:10.1038/srep39862
27. Liu T, Fang X-C, Ding Z, Sun Z-G, Sun L-M, Wang Y-L. Pre-operative lymphocyte-to-monocyte ratio as a predictor of overall survival in patients suffering from osteosarcoma. FEBS Open Biol. 2015;5:682–687. doi:10.1016/j.fob.2015.08.002
28. He Y, Gong R, Peng K-W, Liu L-Z, Sun L-Y, Wang H-Y. Lymphocyte-to-C-reactive protein ratio is a potential new prognostic biomarker for patients with lung cancer. Biomark Med. 2020;14:717–726. doi:10.2217/bmm-2019-0452
29. Zhang H, Zhang B, Zhu K, et al. Preoperative albumin-to-globulin ratio predicts survival in patients with non-small-cell lung cancer after surgery. J Cell Physiol. 2019;234(3):2471–2479. doi:10.1002/jcp.26766
30. Yu S-T, Zhou Z, Cai Q, et al. Prognostic value of the C-reactive protein/albumin ratio in patients with laryngeal squamous cell carcinoma. Onco Targets Ther. 2017;10:879–884. doi:10.2147/OTT.S128391
31. Cai L, Song Y, Zhao X. Prognostic significance of lymphocyte monocyte ratio in patients with ovarian cancer. Medicine (Baltimore). 2020;99(14):e19638. doi:10.1097/MD.0000000000019638
32. Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92(3):205–216. doi:10.1093/jnci/92.3.205
33. Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi:10.1016/j.cell.2011.02.013
34. Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–503. doi:10.1016/S1470-2045(14)70263-3
35. Zhang Y, Zhu JY, Zhou LN, Tang M, Chen MB, Tao M. Predicting the prognosis of gastric cancer by albumin/globulin ratio and the prognostic nutritional index. Nutr Cancer. 2020;72(4):635–644. doi:10.1080/01635581.2019.1651347
36. Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet (London, England). 2001;357(9255):539–545. doi:10.1016/S0140-6736(00)04046-0
37. Heikkilä K, Ebrahim S, Lawlor DA. A systematic review of the association between circulating concentrations of C reactive protein and cancer. J Epidemiol Community Health. 2007;61(9):824–833. doi:10.1136/jech.2006.051292
38. Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009;30(7):1073–1081. doi:10.1093/carcin/bgp127
39. Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–899. doi:10.1016/j.cell.2010.01.025
40. Wang H, Ding Y, Li N, et al. Prognostic value of neutrophil-lymphocyte ratio, platelet-lymphocyte ratio, and combined neutrophil-lymphocyte ratio and platelet-lymphocyte ratio in stage IV advanced gastric cancer. Front Oncol. 2020;10:841. doi:10.3389/fonc.2020.00841
41. Cheng CB, Zhang QX, Zhuang LP, Sun JW. Prognostic value of lymphocyte-to-C-reactive protein ratio in patients with gastric cancer after surgery: a multicentre study. Jpn J Clin Oncol. 2020;50:1141–1149. doi:10.1093/jjco/hyaa099
42. Baba H, Kuwabara K, Ishiguro T, et al. C-reactive protein as a significant prognostic factor for stage IV gastric cancer patients. Anticancer Res. 2013;33(12):5591–5595.
43. Nozoe T, Iguchi T, Adachi E, Matsukuma A, Ezaki T. Preoperative elevation of serum C-reactive protein as an independent prognostic indicator for gastric cancer. Surg Today. 2011;41(4):510–513. doi:10.1007/s00595-009-4297-x
44. Sarraf KM, Belcher E, Raevsky E, Nicholson AG, Goldstraw P, Lim E. Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg. 2009;137(2):425–428. doi:10.1016/j.jtcvs.2008.05.046
45. Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J. 2010;9:69. doi:10.1186/1475-2891-9-69
46. Hill LA, Bodnar TS, Weinberg J, Hammond GL. Corticosteroid-binding globulin is a biomarker of inflammation onset and severity in female rats. J Endocrinol. 2016;230(2):215–225. doi:10.1530/JOE-16-0047
47. Li Q, Meng X, Liang L, Xu Y, Cai G, Cai S. High preoperative serum globulin in rectal cancer treated with neoadjunctive chemoradiation therapy is a risk factor for poor outcome. Am J Cancer Res. 2015;5(9):2856–2864.
48. Sun Y, Huang Z, Lin H, Chi P. Prognostic impact of preoperative immunonutritional status in rectal mucinous adenocarcinoma. Future Oncol. 2020;16(8):339–351. doi:10.2217/fon-2019-0793
49. Oki S, Toiyama Y, Okugawa Y, et al. Clinical burden of preoperative albumin-globulin ratio in esophageal cancer patients. Am J Surg. 2017;214(5):891–898. doi:10.1016/j.amjsurg.2017.04.007
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.