Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Prognostic Value of the Neutrophil-to-Lymphocyte Ratio in Patients with Chronic Internal Carotid Artery Occlusion Complicated by Cerebral Infarction
Authors Qiu Z, Guo T, Sheng X, Tang Y, Du H
Received 5 August 2022
Accepted for publication 8 October 2022
Published 14 October 2022 Volume 2022:18 Pages 2265—2271
DOI https://doi.org/10.2147/NDT.S384512
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Zhuoyin Qiu,1,2,* Tingting Guo,1,2,* Xihua Sheng,1,2 Ying Tang,1,2 Huaping Du1,2
1Department of Neurology, Suzhou Ninth People’s Hospital, Suzhou, People’s Republic of China; 2Department of Neurology, Suzhou Ninth Hospital Affiliated to Soochow University, Suzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Huaping Du, Department of Neurology, Suzhou Ninth People’s Hospital, No. 2666, Ludang Road, Wujiang District, Suzhou, Jiangsu, 215000, People’s Republic of China, Tel +86 512-82885052, Email [email protected]
Purpose: This study aims to investigate the prognostic value of the peripheral neutrophil-to-lymphocyte ratio (NLR) in patients with chronic internal carotid artery occlusion (CICAO) complicated by cerebral infarction.
Patients and Methods: The clinical data of 99 CICAO patients complicated by cerebral infarction were retrospectively analyzed. The modified Rankin Scale (mRS) was used to assess their 3-month prognosis, and a multivariate logistic regression model was established to explore risk factors for poor prognosis.
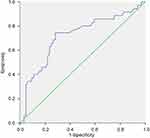
Results: Multivariate logistic regression analysis demonstrated that NLR (OR=2.114; 95% CI: 1.129– 3.959) and baseline National Institute of Health Stroke Scale (NIHSS; OR=1.288, 95% CI: 1.053– 1.574) score were risk factors of poor prognosis. The area under the receiver operator characteristic (ROC) curve of NLR in predicting the 3-month outcome after onset was 0.717 (95% CI: 0.606– 0.828, P< 0.000). The optimal cut-off value was 3.22, with a sensitivity of 0.743 and a specificity of 0.791.
Conclusion: NLR is an independent risk factor for the poor prognosis of CICAO patients complicated by cerebral infarction and can serve as an indicator for clinical prognosis.
Keywords: chronic internal carotid artery occlusion, cerebral infarction, neutrophil-to-lymphocyte ratio, prognosis, predictive factors
Introduction
Cerebral infarction has a high incidence rate, disability, recurrence, and mortality.1 Chronic internal carotid artery occlusion (CICAO), with an onset beyond four weeks, is an uncommon but important cause of cerebral infarction. Statistically, the annual cerebral infarction recurrence rate is 5%–6% among CICAO patients with transient ischemic attacks or mild cerebral infarction and up to 20% in patients with insufficient compensatory CICAO.2 Around 70% of CICAO cases are due to atherosclerosis, and the embolism caused by the thrombi from the occlusion stump or the atherosclerotic plaques is one of the common mechanisms for subsequent ischemic stroke.3 Elevated inflammatory markers correlate with poor prognosis in this population with large-vessel atherothrombotic cerebral infarction.4
The neutrophil-to-lymphocyte ratio (NLR) as a systemic inflammatory marker is clinically practicable as it is easy to perform and low cost. Furthermore, NLR predicts the disease condition and outcome in patients with vascular diseases5 and is associated with the infarct size, illness severity, and prognosis of patients with acute cerebral infarction.6 Few studies have evaluated the prognostic value of NLR for CICAO patients with cerebral infarction; therefore, this study investigated the predictive value of NLR for the 3-month outcome of CICAO patients with comorbid cerebral infarction.
Subjects and Methods
Subjects
Patients with acute cerebral infarction who were admitted to Suzhou Ninth People’s Hospital from September 2015 to September 2021 were included in this study if they 1) were aged > 18 years old, 2) had an onset-to-treatment time ≤ 1 week, 3) had unilateral ICAO confirmed by head and neck computed tomographic angiography (CTA), magnetic resonance angiography (MRA), or digital subtraction angiography (DSA), 4) manifested symptoms of neurological deficit and imaging findings were associated with CICAO, 5) had complete clinical data, including 3-month follow-up data. Patients were excluded if they 1) were not classified as large-vessel atherothrombotic cerebral infarction according to TOAST (The Trial of Org 10,172 in Acute Stroke Treatment) criteria, 2) had concurrent intracranial tumors or epilepsy, 3) had severe cardiac, lung, liver, and kidney diseases or malignancies, 4) or had infectious or immune diseases. In total, 99 patients were included in the present study, including 78 males and 21 females with an average age of 62.8 ± 11.7 years old. All study participants or their legally authorized representatives provided written informed consent during hospitalization.
Clinical Data
The patient’s demographic and clinical data were acquired, including age, gender, individual life history, risk factors for cerebrovascular disease, white blood cell (WBC) count, neutrophil count, blood lipid, C-reactive protein (CRP) level, the US National Institute of Health Stroke Scale (NIHSS) score, and head and neck imaging findings (occlusion site and contralateral artery stenosis).
Follow-Up
The patients were followed up via a clinic visit or telephone 3 months after onset and were assigned a modified Rankin Scale (mRS) score: 0, no symptoms; 1, mild symptoms without significant dysfunction; 2, mild disability; 3, moderate disability, help needed in some cases; 4, moderate-to-severe disability, help needed for walking and to meet their own needs; 5, severe disability, bedridden, incontinent, ongoing care and attention needed; 6, death. Patients were then assigned to the good prognosis group (mRS score ≤ 2) and the poor prognosis group (mRS score > 2) based on the mRS score.
Statistical Analysis
Data analysis was performed with SPSS 22.0. Measurement data were presented as mean ± standard deviation (SD) or as the median. Data that followed a normal distribution were analyzed with the t-test, and data that did not follow a normal distribution were analyzed using a non-parametric test. Enumeration data were expressed as the number of cases (n) with percentage (%) and compared using the chi-squared test. Bivariate correlations were conducted using the Spearman test. Multivariate Logistic regression was performed to identify risk factors. Accuracy of the regression model was verified with the Hosmer-Lemeshow goodness-of-fit test. The prognostic value of NLR was evaluated using the receiver operator characteristic (ROC) curve. P<0.05 referred to a statistically significant difference.
Results
Comparison of the General Data Between Groups
Patients in the poor prognosis group were older than those in the good prognosis group. The proportion of patients with comorbid diabetes, NLR levels, and NIHSS scores in the poor prognosis group was also significantly higher than those in the good prognosis group (P<0.05) (Table 1).
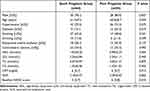 |
Table 1 Comparisons of General Data Between Two Groups |
Logistic Regression Analysis of Prognostic Risk Factors
Multivariate logistic regression was conducted using patients’ prognosis as a dependent variable (1 for poor prognosis and 0 for good prognosis) and age, comorbid diabetes, NLR, and baseline NIHSS score as independent variables, revealing that NLR and baseline NIHSS score were independent risk factors for poor prognosis (Table 2). The multivariate regression had a good fit, as indicated by the Hosmer-Lemeshow goodness-of-fit (P=0.202>0.05).
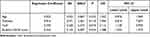 |
Table 2 Multivariate Logistic Regression Analysis of the Poor Outcome of Patients |
Prognostic Value of NLR for 3-Month Prognosis
A ROC curve was plotted to assess the prognostic value of NLR for a 3-month prognosis after onset, and the area under the curve (AUC) was 0.717 (95% CI: 0.606–0.828, P<0.000) (Figure 1). The best cut-off value was 3.22 with a sensitivity of 0.743 and specificity of 0.791.
Comparisons of General Data in Patients with Different NLR Levels
Patients were classified into two groups using the best cut-off value of 3.22. Patients with NLR>3.22 had a higher incidence of diabetes and contralateral internal carotid artery stenosis, as well as a higher NIHSS score than patients with NLR≤3.22 (P<0.05; Table 3).
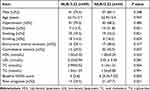 |
Table 3 Comparisons of General Data in Patients with Different Levels of NLR |
Correlation Analysis of NLR and NIHSS
There was a positive correlation between NLR level and baseline NIHSS score in patients with CICAO and cerebral infarction (r=0.305, P=0.002).
Discussion
CICAO is an important cause of cerebrovascular ischemic events, and there are significant differences in the clinical manifestations and prognosis across CICAO patients complicated by cerebral infarction. Furthermore, collateral circulation is closely interrelated with the prognosis of patients with cerebral infarction. Asymptomatic CICAO patients have a high opening rate of collateral circulation, and those with collateral circulation opening tend to have mild clinical symptoms and a good prognosis when they are complicated by cerebral infarction.7 The main etiology of occlusion is atherosclerosis, and inflammation contributes to atherogenesis,8 as well as the formation of collateral circulation through multiple mechanisms.9 An elevated lymphocyte count correlates with excellent collateral circulation, while a high WBC count and NLR level are associated with poor collateral circulation.10 The present study indicated that a high NLR level was closely associated with a poor 3-month outcome of CICAO patients with cerebral infarction, illustrating that NLR can serve as a prognostic factor.
Recently, neuroinflammation has received increasing attention in ischemic stroke. An extensive body of research has verified that inflammatory mechanisms play a vital role in the pathogenesis and progression of ischemic stroke.11–13 NLR is widely applied in evaluating the severity and prognosis of multiple diseases as a simple, convenient inflammatory marker. A review of NLR as a bio-markers of morbidity and mortality rates for cardiovascular surgery suggested that it could help identify patients at high risk of periprocedural adverse events.14 A meta-analysis showed that an elevated NLR level was associated with mortality, poor outcomes, and hemorrhagic transformation of cerebral infarction patients; thus, NLR could be utilized to instruct clinical decisions as a potential prognostic biomarker.6 In the study of Gong et al15 of 1060 ischemic stroke patients receiving intravenous thrombolysis, NLR elevated was an independent risk factor for early-stage neurological deterioration, and patients with low NLR levels benefited more from thrombolysis. Compared to high-sensitivity C-reactive protein, NLR is strongly associated with the occurrence of stroke-associated pneumonia.16 Hu et al17 reported that NLR is associated with 90-day poor outcomes in stroke patients, however, the AUC of high NLR was insufficiently high to predict the poor outcome. In contrast, the AUC of NLR (0.717) in the present study had a good predictive value. Overall, inflammation occurs throughout the occurrence, development, stroke-related complications, and prognosis of cerebral infarction. Indeed, whether NLR is a good predictor for stroke in different etiologies requires further exploration.
The underlying mechanism between NLR increase and poor prognosis is involved in the overactivation of inflammatory responses and immunosuppression. Neutrophils are short-lived, innate immune cells and play a limited immunological role. After cerebral infarction, neutrophils migrate toward the ischemic area through the disrupted blood-brain barrier under the mediation of cytokines and chemokines.18 Meanwhile, neutrophils release oxygen radicals and matrix metalloproteinases to further disrupt the blood-brain barrier and recruit more immune cells, worsening tissue edema and inducing cell death.19 A study revealed that inhibiting neutrophil aggregation in the ischemic penumbra could alleviate neurological deficits in mouse models.20 Lymphocytes also play a vital role in the immune response after cerebral infarction. They are detected in the cerebral tissues within 24 h of ischemic stroke and continue to increase to exert neuroprotective effects.21 Patients with large-vessel occlusive stroke have significantly increased levels of WBC and lymphocytes, and the elevation is closely associated with patient prognosis. This study indicated that vessel occlusion could induce an inflammatory response in cerebral tissues.22 Another study revealed that after cerebral infarction, increased lymphocytes mediate the autoimmune response and release oxygen radicals and inflammatory factors to aggravate brain injury.23 This discrepancy between the two studies might be due to different lymphocyte subgroups. CD4+ regulatory T lymphocytes are a subgroup of CD4+ T cells that are immunosuppressive and decrease the production of inflammatory factors, playing a protective role against multiple ischemic diseases including ischemic stroke.24 It was demonstrated that a decrease in regulatory T lymphocytes was interrelated with a poor prognosis in cerebral infarction patients.25 Regulatory T lymphocytes may exert neuroprotective effects by maintaining the integrity of the blood-brain barrier, inhibiting the activation of microglial cells, and regulating the microglial phenotype transformation.24
The limitations of this study reside in three aspects. First, the study has a selection bias since it is a single-center retrospective study with a small sample size. Second, the NLR level was not dynamically monitored. Last, occluded internal carotid artery was not further assessed via high-resolution MR. In the future, a multi-center study with larger sample size is required.
Conclusion
Taken together, neutrophils and lymphocytes are crucial in cerebral infarction given their regulatory role in neuroinflammation and neuroprotective effects. NLR is an inflammatory index that is easy to acquire and low cost, and a high NLR level is correlated with a poor prognosis; thus, an increased NLR level can be used as an indicator of poor 3-month prognosis in CICAO patients with cerebral infarction.
Ethical Approval
The study was approved by the Ethical Committee of Suzhou Ninth People’s Hospital (No. KY2022-008-01) and conducted in accordance with the Declaration of Helsinki.
Funding
This work was supported by the Suzhou Youth Science and technology project (KJXW2016065) and Basic research of Suzhou Medical and health care (SYSD2020044).
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
1. Feigin VL, Stark BA, Johnson CO. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795–820. doi:10.1016/S1474-4422(21)00252-0
2. Wan M, Yan L, Xu Z, et al. Symptomatic and Asymptomatic Chronic Carotid Artery Occlusion on High-Resolution MR Vessel Wall Imaging. AJNR Am J Neuroradiol. 2022;43(1):110–116. doi:10.3174/ajnr.A7365
3. Saini H, Cerejo R, Williamson R, Malhotra K. Internal carotid artery occlusion: management. Curr Neurol Neurosci Rep. 2022;22(7):383–388. doi:10.1007/s11910-022-01201-x
4. Cao L, Guo Y, Zhu Z. Study of the Inflammatory Mechanisms in Hyperhomocysteinemia on Large-Artery Atherosclerosis Based on Hypersensitive C-Reactive Protein-A Study from Southern China. J Stroke Cerebrovasc Dis. 2019;28(7):1816–1823. doi:10.1016/j.jstrokecerebrovasdis.2019.04.021
5. Afari ME, Bhat T. Neutrophil to lymphocyte ratio (NLR) and cardiovascular diseases: an update. Expert Rev Cardiovasc Ther. 2016;14(5):573–577. doi:10.1586/14779072.2016.1154788
6. Li W, Hou M, Ding Z, Liu X, Shao Y, Li X. Prognostic value of neutrophil-to-lymphocyte ratio in stroke: a systematic review and meta-analysis. Front Neurol. 2021;12:686983. doi:10.3389/fneur.2021.686983
7. Xu B, Li C, Guo Y, Xu K, Yang Y, Yu J. Current understanding of chronic total occlusion of the internal carotid artery. Biomed Rep. 2018;8(2):117–125. doi:10.3892/br.2017.1033
8. Kim SJ, Schneider DJ, Feldmann E, Liebeskind DS. Intracranial atherosclerosis: review of imaging features and advances in diagnostics. Int J Stroke. 2022;17(6):599–607. doi:10.1177/17474930211066427
9. Mechtouff L, Bochaton T, Paccalet A, et al. Matrix Metalloproteinase-9 and Monocyte Chemoattractant Protein-1 Are Associated With Collateral Status in Acute Ischemic Stroke With Large Vessel Occlusion. Stroke. 2020;51(7):2232–2235. doi:10.1161/STROKEAHA.120.029395
10. Kelesoglu S, Yilmaz Y, Elcik D, Kalay N. Systemic immune inflammation index: a novel predictor for coronary collateral circulation. Perfusion. 2021;1:1951885990.
11. Shi K, Tian DC, Li ZG, Ducruet AF, Lawton MT, Shi FD. Global brain inflammation in stroke. Lancet Neurol. 2019;18(11):1058–1066. doi:10.1016/S1474-4422(19)30078-X
12. Rust R, Gronnert L, Schwab ME. Inflammation after Stroke: a Local Rather Than Systemic Response? Trends Neurosci. 2018;41(12):877–879. doi:10.1016/j.tins.2018.09.011
13. Sheng X, Du H, Tang Y. Decreased Serum Total Bilirubin Level Predicts Early Neurological Deterioration in Patients with Acute Ischemic Stroke. Neuropsychiatr Dis Treat. 2021;17:1977–1982. doi:10.2147/NDT.S315330
14. Serra R, Ielapi N, Licastro N, et al. Neutrophil-to-lymphocyte Ratio and Platelet-to-lymphocyte Ratio as Biomarkers for Cardiovascular Surgery Procedures: a Literature Review. Rev Recent Clin Trials. 2021;16(2):173–179. doi:10.2174/1574887115999201027145406
15. Gong P, Liu Y, Gong Y, et al. The association of neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and lymphocyte to monocyte ratio with post-thrombolysis early neurological outcomes in patients with acute ischemic stroke. J Neuroinflammation. 2021;18(1):51. doi:10.1186/s12974-021-02090-6
16. Wu T, Zhang H, Tian X, Cao Y, Wei D, Wu X. Neutrophil-to-Lymphocyte Ratio Better Than High-Sensitivity C-Reactive Protein in Predicting Stroke-Associated Pneumonia in Afebrile Patients. Neuropsychiatr Dis Treat. 2021;17:3589–3595. doi:10.2147/NDT.S340189
17. Hu Y, Huang K, Ji Z, et al. High neutrophil-to-lymphocyte ratio is associated with poor clinical outcome in patients with critically ill stroke. Minerva Anestesiol. 2020;86(9):939–947. doi:10.23736/S0375-9393.20.14310-4
18. Pu Z, Bao X, Xia S, Shao P, Xu Y. Serpine1 regulates peripheral neutrophil recruitment and acts as potential target in ischemic stroke. J Inflamm Res. 2022;15:2649–2663. doi:10.2147/JIR.S361072
19. Pun PB, Lu J, Moochhala S. Involvement of ROS in BBB dysfunction. Free Radic Res. 2009;43(4):348–364. doi:10.1080/10715760902751902
20. Neumann J, Riek-Burchardt M, Herz J, et al. Very-late-antigen-4 (VLA-4)-mediated brain invasion by neutrophils leads to interactions with microglia, increased ischemic injury and impaired behavior in experimental stroke. Acta Neuropathol. 2015;129(2):259–277. doi:10.1007/s00401-014-1355-2
21. Xie L, Li W, Hersh J, Liu R, Yang SH. Experimental ischemic stroke induces long-term T cell activation in the brain. J Cereb Blood Flow Metab. 2019;39(11):2268–2276. doi:10.1177/0271678X18792372
22. Kollikowski AM, Schuhmann MK, Nieswandt B, Mullges W, Stoll G, Pham M. Local Leukocyte Invasion during Hyperacute Human Ischemic Stroke. Ann Neurol. 2020;87(3):466–479. doi:10.1002/ana.25665
23. Kleinschnitz C, Schwab N, Kraft P, et al. Early detrimental T-cell effects in experimental cerebral ischemia are neither related to adaptive immunity nor thrombus formation. Blood. 2010;115(18):3835–3842. doi:10.1182/blood-2009-10-249078
24. Wang HY, Ye JR, Cui LY, Chu SF, Chen NH. Regulatory T cells in ischemic stroke. Acta Pharmacol Sin. 2022;43(1):1–9. doi:10.1038/s41401-021-00641-4
25. Santamaria-Cadavid M, Rodriguez-Castro E, Rodriguez-Yanez M, et al. Regulatory T cells participate in the recovery of ischemic stroke patients. Bmc Neurol. 2020;20(1):68. doi:10.1186/s12883-020-01648-w
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.