Back to Journals » Journal of Inflammation Research » Volume 15
Prognostic Value of Serum Procalcitonin Based Model in Moderate to Severe Traumatic Brain Injury Patients
Authors Wang R, Hua Y , He M, Xu J
Received 15 January 2022
Accepted for publication 9 August 2022
Published 30 August 2022 Volume 2022:15 Pages 4981—4993
DOI https://doi.org/10.2147/JIR.S358621
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Ning Quan
Ruoran Wang,1,* Yusi Hua,2,* Min He,3 Jianguo Xu1
1Department of Neurosurgery, West China Hospital, Sichuan University, Chengdu, People’s Republic of China; 2Department of Anesthesiology, West China Hospital, Sichuan University, Chengdu, People’s Republic of China; 3Department of Critical Care Medicine, West China Hospital, Sichuan University, Chengdu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jianguo Xu, Department of Neurosurgery, West China Hospital, Sichuan University, No. 37, Guoxue Alley, Chengdu, 610041, People’s Republic of China, Email [email protected] Min He, Department of Critical Care Medicine, West China Hospital, Sichuan University, No. 37, Guoxue Alley, Chengdu, 610041, People’s Republic of China, Email [email protected]
Objective: Procalcitonin (PCT) is an acknowledged marker of systemic inflammatory response. Previous studies have not reached agreement on the association between serum PCT and outcome of traumatic brain injury (TBI) patients. We designed this study to confirm the prognostic value of PCT in isolated TBI and those with extracranial injury, respectively.
Methods: Patients hospitalized in our hospital for moderate-to-severe TBI between March 2015 and December 2019 were included. Logistic regression analysis was performed to validate the association between PCT and in-hospital mortality in these patients. AUC (area under the receiver operating characteristics curve) of PCT and constructed model were calculated and compared.
Results: Among the included 211 patients, 81 patients suffered a poor outcome, with a mortality rate of 38.4%. Non-survivors had a higher level of serum PCT (2.73 vs 0.72, p< 0.001) and lower GCS (5 vs 7, p< 0.001) on admission than survivors. AUC of single PCT for predicting mortality in isolated TBI and those with extracranial injury were 0.767 and 0.553, respectively. Multivariate logistic regression showed that GCS (OR=0.744, p=0.008), glucose (OR=1.236, p< 0.001), cholesterol (OR=0.526, p=0.002), and PCT (OR=1.107, p=0.022) were independently associated with mortality of isolated TBI. The AUC of the prognostic model composed of GCS, glucose, cholesterol, and PCT was 0.868 in isolated TBI.
Conclusion: PCT is an efficient marker of outcome in isolated moderate-to-severe TBI but not those with extracranial injury. A prognostic model incorporating PCT is useful for clinicians to make early risk stratification for isolated TBI.
Keywords: procalcitonin, traumatic brain injury, extracranial injury, prognosis
Introduction
Traumatic brain injury (TBI) is still a widely concerning public health problem, which severely impairs patients’ quality-of-life and brings a heavy economic burden to society. It has recently been estimated that TBI would occur approximately 69 million times annually all over the world.1 Although many novel therapies aimed at preventing secondary brain injury have been proposed and proved, the mortality of moderate-to-severe TBI remains relatively high. To prevent possible adverse progress in these patients, early risk stratification is necessary for clinicians to evaluate patients’ condition and, therefore, adjust treatment strategies. Having been widely used to assess injury severity in the past four decades, the Glasgow Coma Scale (GCS) has gradually been found to have some deficiencies, including an inaccurate estimation during sedation and intubation.2,3 Recently, a growing number of studies have explored the prognostic value of biomarkers in serum or cerebrospinal fluid, such as glial fibrillary acidic protein (GFAP), S100 calcium binding protein B (S100B), neurofilament protein-light (NfL), ubiquitin carboxy-terminal hydrolase L1 (UCHL1), and Tau.4 And some studies developed multimodal prognostic calculators such as the Corticosteroid Randomization After Significant Head injury (CRASH) and International Mission for Prognosis and Analysis of Clinical Trials in Traumatic Brain Injury (IMPACT).5,6 In addition to develop novel predictive models, utilizing other markers to modify the GCS is also an effective alternative method which could make up deficiencies of conventional GCS and improve the stability of severity estimation. Previous researchers have tried combining some markers with GCS to increase the predictive value, such as age, shock index, and neutrophil-to-lymphocyte ratio.7–10 As a widely used diagnostic marker of severe infection and sepsis, procalcitonin (PCT) has been confirmed to be associated with mortality in many clinical settings, such as sepsis, cancer, and trauma.11–17 Moreover, the prognostic value of serum PCT in patients with neurological diseases including subarachnoid hemorrhage, ischemic stroke, intracerebral hemorrhage and epilepticus status have been explored.18–22 Although several researchers have illustrated the prognostic value of PCT in TBI patients, the sample size of these studies were relatively small and included subjects were not limited to homogenous moderate-to-severe TBI patients.23–26 Another important defect is that the predictive value of only a single PCT level but not a predictive model incorporating PCT and other significant factors were evaluated in these studies. Therefore, we designed this study to explore the prognostic value of PCT alone and predictive model incorporating PCT in moderate-to-severe TBI patients.
Materials and Methods
Patients
This study was performed in a tertiary hospital which was a regional trauma center in Southwest China. Patients admitted to our hospital for TBI between March 2015 and December 2019 were eligible for this study. Most TBI patients hospitalized in our hospital were moderate-to-severe TBI (GCS ≤12) patients who would get suitable treatments and critical management in the intensive care unit (ICU). Patients who met the following criteria were excluded from this study: 1) GCS on admission >12; 2) Admitted to our hospital 6 hours after injury or transferred from other hospitals; 3) patients whose relevant data were not entirely recorded; and 4) patients who had a recent history of severe infection or surgery. After screening, 211 patients were finally included in this observational study. The inclusion flowchart of patients is shown as Figure 1. Our study got approvement from the ethics committee of West China hospital and accorded with the Helsinki Declaration. Informed consent forms of each patient were obtained from themselves or their legal representatives.
 |
Figure 1 Flow diagram of included patients. Abbreviations: TBI, traumatic brain injury; GCS, Glasgow Coma Scale. |
Data Collection
Included variables were mainly collected from the records in electronic medical record system of our hospital. Injury mechanisms were obtained by talking with patients or their legal representatives on admission. Vital signs and GCS score on admission were evaluated by experienced emergency workers once patients were admitted to our hospital. Results of laboratory tests including serum PCT was acquired by analyzing the blood samples drawn on admission. The coagulopathy was confirmed based on international normalized ratio >1.6 or activated partial thromboplastin time >60 seconds. Intracranial injury types of each patient were recorded by checking the characteristics of computed tomography (CT) scan carried in our hospital. The AIS >1 of any extracranial body region was considered as the existence of extracranial injury. The primary outcome of this study was in-hospital mortality.
Statistical Analysis
Kolmogorov–Smirnov tests were performed to confirm the normality of included variables. Non-normally distributed variables and normally distributed variables were shown in the form of median (interquartile range) and mean±standard deviation, respectively. And categorical variables were presented as numbers (percentage). We compared the difference of non-normally distributed variables and normally distributed variables between two subgroups by using Mann–Whitney U-test and Student’s t-test, respectively. Difference of categorical variables were analyzed by χ2 test or Fisher test. Univariate logistic regression analysis was firstly utilized to explore the potential factors for mortality of included TBI patients. Then, potential significant factors in univariate regression were selected by conducting stepwise forward multivariate logistic regression. Significant risk factors in multivariate analysis were finally utilized to construct a prognostic model using logistic regression. We draw receiver operating characteristic (ROC) curves of single factors and the constructed prognostic model. Z-tests were conducted to compare the area under the ROC curve (AUC) difference of these factors and the model.
We considered that a two-sided p-value<0.05 was of statistical significance. SPSS 22.0 Windows software (SPSS, Inc, Chicago, IL) was used for all statistical analyses and figures drawing.
Results
Baseline Characteristics of Included Patients Grouping by Survival Outcome
A total of 211 TBI patients were included with mortality of 38.4% (Table 1). Age and sex ratio did not differ between survivors and non-survivors. Traffic accident (60.2%) and high falling injury (22.7%) ranked the first and the second among injury mechanisms. Vital signs on admission including systolic, diastolic blood pressure, and body temperature did not show significant differences between survivors and non-survivors. While non-survivors had significantly lower GCS (5 vs 7, p<0.001) and higher Abbreviated Injury Score (AIS) (5 vs 4, p<0.001) and Injury Severity Score (ISS) (25 vs 20, p<0.001). Results of laboratory tests showed that non-survivors had a lower level of platelet (80×109/L vs 113×109/L, p<0.001), cholesterol (2.25 mmol/L vs 2.87 mmol/L, p<0.001), and hemoglobin (81 g/L vs 90 g/L, p=0.010) than survivors. Whereas the blood level of glucose (12.88 mmol/L vs 8.66 mmol/L, p<0.001) and PCT (2.73 ng/mL vs 0.72 ng/mL, p<0.001) were significantly higher than survivors. Considering the intracranial radiological signs, we found that non-survivors had a higher incidence of subdural hematoma (33.3% vs 17.7%, p=0.010) and a lower incidence of epidural hematoma (3.7% vs 11.5%, p=0.036). Sixty-five patients suffered extracranial injury with an incidence of 30.8%. Compared with survivors, non-survivors had a shorter length of ICU stay (4 vs 18, p<0.001) and length of hospital stay (8 vs 30, p<0.001).
 |
Table 1 Baseline Characteristics of Included TBI Patients |
Prognostic Value of PCT and Other Index Alone for Predicting Mortality in TBI Patients with or without Extracranial Injury
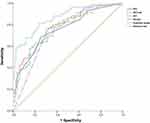
Among the included 211 TBI patients, 146 patients were isolated TBI and 65 complicated with extracranial injuries. We evaluate the prognostic value of PCT in these two groups respectively. In isolated TBI patients, the AUC of single PCT, GCS, and AIS were 0.774, 0.751, and 0.743, respectively (Table 2; Figure 2A), while in TBI patients with extracranial injuries, the AUC of single PCT, GCS, AIS, ISS were only 0.553, 0.680, 0.608, and 0.590, respectively (Figure 2B).
 |
Table 2 Predictive Value of PCT and Other Trauma Scores in Patients with Isolated TBI or Patients with TBI and Extracranial Injuries |
Logistic Regression Analysis of Risk Factors for Mortality in Isolated TBI Patients
Because of the limited prognostic value of single PCT in TBI patients with extracranial injuries, we only performed logistic regression analysis in isolated TBI patients. Univariate logistic regression showed that GCS (p<0.001), AIS head (p<0.001), platelet (p=0.008), glucose (p<0.001), albumin (p<0.001), hemoglobin (p=0.025), cholesterol (p<0.001), PCT (p=0.001), and coagulopathy (p<0.001) were associated with mortality of included TBI patients (Table 3). However, after adjusting confounding effects, multivariate logistic regression indicated only GCS (OR=0.744, p=0.008), glucose (OR=1.236, p<0.001), cholesterol (OR=0.526, p=0.002), and PCT (OR=1.107, p=0.022) were independent risk factors of mortality.
 |
Table 3 Univariate and Multivariate Logistic Regression Analysis of Risk Factors for Mortality in Isolated TBI Patients |
Prognostic Value of Logistic Model Incorporating PCT in Isolated TBI Patients
We utilized four significant factors in multivariate logistic regression to construct a prognostic model for isolated TBI patients.
The results of Table 4 showed the detailed AUC value, sensitivity, and specificity of PCT, glucose, GCS, and AIS (Figure 3). There were no statistical differences of AUC between these four factors. Whereas the AUC value of the four-factors prognostic model was 0.868, which was higher than that of PCT (Z=1.91, p<0.05), glucose (Z=1.96, p<0.05), or GCS alone (Z=2.34, p<0.05).
 |
Table 4 Prognostic Value of PCT and the Constructed Predictive Model in Patients with Isolated TBI |
Discussion
Discovered three decades ago, PCT is a prepropeptide precursor of calcitonin, which is synthesized in thyroid C cells under physiological condition.27,28 The significant increase of plasma PCT level under many kinds of inflammatory stimulations, especially the bacterial infection, is mainly attributable to induced production from neuroendocrine cells in the lung or intestine.29,30 Previous studies have illustrated that serum PCT concentration was associated with sepsis severity, development of systemic inflammatory response syndrome, and multiple organ dysfunction syndrome.31–35 PCT is confirmed as not only a reliable diagnostic indicator of bacterial infection,11,36–39 but also an effective predictor of prognosis in many kinds of brain injury patients including intracerebral hemorrhage, ischemic stroke, and aneurysmal subarachnoid hemorrhage.18–22 Previous studies with a small sample size declared the positive correlation between serum PCT and sepsis development and mortality in neurotrauma patients.23,26,40 Consistent with findings of these studies, we found that serum PCT of non-survivors was significantly higher than survivors in our study.
The possible mechanism involved in the elevated serum PCT after TBI is multifaceted. First, systemic inflammation caused by the initial injury and an invasive procedure could induce the production of PCT in TBI patients. Systemic inflammatory response syndrome (SIRS) is a common complication in TBI patients with an incidence rate of 15.2% to 21%.41,42 The SIRS early after traumatic injury is actually provoked by many factors including tissue damage, hypotension, hypoxia, cytokine release, and inflammation.43 The PCT is considered as a classic acute-phase biomarker of the systemic inflammatory response.44 Therefore, the initial elevated PCT after TBI could be considered as a reflection of developing systemic inflammation. Second, the local neural inflammation could also stimulate the synthesis of PCT in injured brain tissue. A previous study found that cerebrospinal fluid (CSF) procalcitonin concentration would increase after pediatric traumatic brain injury.24 Due to the breakdown of blood–brain barrier, PCT in CSF could enter the peripheral circulation and lead to the elevated serum PCT. Some widely concerned pro-inflammatory cytokines such as interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α), and interleukin-6 (IL-6), which take part in the process of secondary brain injury and disruption of neuronal regeneration, promote the production and release of PCT.45–49 Another explanation for the elevated PCT in brain tissue is the upregulation of CALC-I gene (the gene encoding PCT) expression in the human brain tissue.50 This mechanism was approved by the finding that increased expression of the CALC-I gene in brain tissue as a response to sepsis in animal models.49 Some researchers believed that PCT was a member of a kind of vasodilating neuropeptides families which serves as an endogenous adaptive response to ischemic insult caused by cerebral hypoperfusion after TBI.24,51
The association between serum PCT and outcome in TBI patients might be mediated by local and systemic inflammation above-mentioned. As an acute phase protein PCT could indicate the level of SIRS, which has been confirmed associated with poor outcome in isolated TBI patients.42 Previous studies have confirmed PCT as an independent predictor of multiple organ failure in the early post-traumatic phase in trauma patients with and without brain injury.25,52 And the correlation between APACHE II, SOFA reflecting organ failure severity, and serum PCT before ICU discharge has been revealed by Spearman correlation analysis.53 Therefore, a reasonable conjecture is that PCT is able to predict and evaluate the severity of multiple organ dysfunction syndrome (MODS), which is significantly associated with mortality following TBI.54 In addition to the systemic inflammation, PCT might correlate with outcome of TBI patients by the mediation of local infection. Severe systemic inflammatory and imbalanced immune status caused by TBI could render patients susceptible to subsequent local infection.55 It was estimated that 36% of patients treated in neuro-ICU would develop infectious complications.56 Respiratory tract infection, urinary tract infection, bloodstream infection, and intracranial infection such as ventriculitis and meningitis were commonly detected in these patients.57 As for TBI patients, the incidence of nosocomial infection was reported as high as 41%.58 And infection development and severity are related to poor prognosis and delayed recovery in patients with neurotrauma.58–63 Therefore, PCT could predict the outcome of TBI patients by indicating the possibilities of subsequent local infection under the influence of initial systemic inflammatory and immune status. Among all kinds of regional inflammation, the neuroinflammation may play a pivotal role in the pathophysiological process and neural regeneration of TBI. As mentioned above, elevated production of PCT is likely associated with the expression of pro-inflammatory cytokines including TNF-α, IL-1β, and IL-6 in injured brain tissue and hypoxic-ischemic injury. The relationship between radiologic lesion burden, GCS score, and PCT was analyzed in a recent study.64 Researchers considered quantitative analysis of acute phase biomarkers including PCT as an objective and supplemental assessment of neurologic status in TBI patients. A study similarly discovered that serum PCT was positively associated with severity and poor outcome of intracerebral hemorrhage patients by the mediation of increased volume of hematoma and perihematomal edema. Thus, more severe neural inflammation and injury severity indicated by elevated serum PCT is another cause leading to the poor outcome of TBI patients.65,66 As a marker of inflammation and infection, PCT is readily available by drawing the blood sample. Some studies have conducted cost-effectiveness analysis of PCT and found it performed well in detecting infection and guiding antibiotic use with relatively lower expenditure.67–69 The accessibility and fluctuation after injury of PCT makes it a potential prognostic marker of TBI.
Previous studies have explored the predictive value of single PCT on outcome and sepsis in TBI patients with several limitations. The AUC value of single PCT for predicting mortality in TBI patients was reported as ranging from 0.533 to 0.780 in previous studies,23,26,70,71 whereas the AUC of PCT in our study was 0.774 for isolated TBI and 0.553 for those with extracranial injury. Therefore, it could be concluded that PCT was a reliable prognostic marker of isolated TBI patients but not TBI patients with extracranial injuries. Though Keshav Goyal et al71 evaluated the prognostic value of serially measured PCT levels on several time points for TBI patients, the sample size of this study was very small with obvious and improper statistical analysis that an excessive number of confounding variables included into multivariate regression. In addition, they did not evaluate the prognostic value of PCT in TBI with extracranial injury individually due to the limited number of these patients.
In our study, the significant difference between isolated TBI and those with extracranial injury might mean that extracranial injury could affect and weaken the relationship between brain injury and PCT level. Therefore, PCT may be a reliable prognostic marker aimed at isolated TBI but not those with extracranial injury. Finally, another noteworthy limitation mentioned in previous studies was that a single PCT value without combining other significant factors to construct a clinical score or model could not predict the clinical course of TBI patients accurately and comprehensively. Instead, one study found that combining PCT into National Institutes of Health Stroke Scale (NIHSS) could increase the prognostic value in ischemic stroke patients.21 Another study also stated that modifying status epilepticus severity score using PCT could increase the prognostic value in status epilepticus patients.18 Therefore, we conducted this study to explore the relationship between PCT, other clinical factors, and mortality by utilizing multivariate logistic regression analysis. As a result, PCT, conventional GCS, blood glucose, and cholesterol were independently associated with mortality in isolated moderate-to-severe TBI patients. Stress induced hyperglycemia have been verified many times as a potent risk factor of mortality in TBI patients.72–75 The lower level of cholesterol in non-survivors is similar to findings of other studies indicating hypocholesterolemia is a risk factor of poor prognosis in various kinds of patients such as sepsis, intracerebral hemorrhage, and diffuse peritonitis.76–78 And one previous study found, low serum levels of high-density lipoprotein cholesterol were positively associated with diffuse axonal injury which was an indication of poor prognosis in TBI patients.79 The decreasing cholesterol level may be attributable to many factors including severe acute phase response, liver dysfunction, and hemodilution induced by blood loss. Our constructed model incorporating GCS, PCT, glucose, and cholesterol could evaluate a possible clinical course in isolated moderate-to-severe TBI patients more accurately than these factors alone.
Actually, plenty of studies have been designed and performed to develop novel and reliable prognostic tools for TBI. The two most concerned models among them are IMPACT and CRASH, which were developed to incorporate, age, GCS component, pupil reactivity and neuroimaging signs based on the large population size.5,6 The AUCs of them both have reached above 0.8 with excellent discriminability and stability. The external validation for them in more specific kinds of patients is still in progress.80,81 In addition to multimodal prognostic models, some biofluid markers including GFAP, UCHL-1, and NfL have also been explored and approved in evaluating prognosis of TBI patients.4 These biomarkers involved in the pathophysiological process of TBI have been combined to a panel and could reflect brain injury severity and disease progression more accurately than one alone. While the panel has not been widely utilized all over the world, especially in the developing countries. Therefore, some regular examined laboratory indexes including PCT may be still valuable in evaluating the prognosis of TBI in the current clinical practice. Future studies collecting both the above-mentioned biofluid markers and PCT are worthwhile to conduct to compare their prognostic value with each other.
There were several limitations in our study. First, this study was conducted in a single center with a relatively limited sample size, especially the amount of TBI patients with extracranial injury. A further study including more participants is worthwhile to perform to validate the conclusions of our study. Second, the serum PCT level was assessed on admission. Though patients admitted to our hospital 6 hours after suffering injury were excluded, the association between PCT and outcome might still be confounded by the time interval from suffering injury to drawing a blood sample. Third, we did not evaluate previously developed multimodal prognostic calculators such as IMPACT, CRASH, and measure several widely approved biomarkers such as GFAP, S100 B, NfL, and Tau so we could not compare their prognostic value with PCT’s. Fourth, only in-hospital mortality was recorded and other outcomes such as functional status and cognitive level after discharge were not evaluated in this study. Finally, the concentration of PCT in CSF which might reflect the degree of neural inflammation was not tested and, therefore, we could not analyze the relationship between serum PCT and CSF PCT.
Conclusion
PCT is useful in predicting mortality of isolated moderate-to-severe TBI patients but not TBI with extracranial injury. Our prognostic model composed of GCS, PCT, glucose, and cholesterol could guide clinicians to stratify risk level and strengthen management for isolated moderate-to-severe TBI patients.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
Ethical Approval
Our study obtained approval from the ethics committee of West China hospital (2021-1598) and accorded with the Helsinki Declaration. Informed consent forms of each patient were obtained from themselves or their legal representatives.
Author Contributions
Ruoran Wang and Yusi Hua should be considered co-first authors. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by 1·3·5 project for disciplines of excellence–Clinical Research Incubation Project, West China Hospital, Sichuan University (2020HXFH036), Knowledge Innovation Program of the Chinese Academy of Sciences (JH2022007) and General Program of the National Natural Science Foundation of China (82173175).
Disclosure
The authors declare that they have no conflict of interest.
References
1. Dewan MC, Rattani A, Gupta S, et al. Estimating the global incidence of traumatic brain injury. J Neurosurg. 2018;130:1–18.
2. Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–84. doi:10.1016/S0140-6736(74)91639-0
3. Majdan M, Steyerberg EW, Nieboer D, Mauritz W, Rusnak M, Lingsma HF. Glasgow coma scale motor score and pupillary reaction to predict six-month mortality in patients with traumatic brain injury: comparison of field and admission assessment. J Neurotrauma. 2015;32(2):101–108. doi:10.1089/neu.2014.3438
4. Wilde EA, Wanner IB, Kenney K, et al. A framework to advance biomarker development in the diagnosis, outcome prediction, and treatment of traumatic brain injury. J Neurotrauma. 2022;39(7–8):436–457. doi:10.1089/neu.2021.0099
5. Maas AI, Marmarou A, Murray GD, Teasdale SG, Steyerberg EW. Prognosis and clinical trial design in traumatic brain injury: the IMPACT study. J Neurotrauma. 2007;24(2):232–238. doi:10.1089/neu.2006.0024
6. Steyerberg EW, Mushkudiani N, Perel P, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5(8):
7. Khan M, O’Keeffe T, Jehan F, et al. The impact of Glasgow Coma Scale-age prognosis score on geriatric traumatic brain injury outcomes. J Surg Res. 2017;216:109–114. doi:10.1016/j.jss.2017.04.026
8. Wu SC, Rau CS, Kuo SCH, Chien PC, Hsieh HY, Hsieh CH. The reverse shock index multiplied by Glasgow coma scale score (rSIG) and prediction of mortality outcome in adult trauma patients: a cross-sectional analysis based on registered trauma data. Int J Environ Res Public Health. 2018;15(11):2346.
9. Wan-Ting C, Chin-Hsien L, Cheng-Yu L, et al. Reverse shock index multiplied by Glasgow Coma Scale (rSIG) predicts mortality in severe trauma patients with head injury. Sci Rep. 2020;10(1):2095. doi:10.1038/s41598-020-59044-w
10. Zhao JL, Du ZY, Yuan Q, et al. Prognostic value of neutrophil-to-lymphocyte ratio in predicting the 6-month outcome of patients with traumatic brain injury: a retrospective study. World Neurosurg. 2019;124:e411–e416.
11. Festic E, Siegel J, Stritt M, Freeman WD. The utility of serum procalcitonin in distinguishing systemic inflammatory response syndrome from infection after aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2014;20(3):375–381. doi:10.1007/s12028-014-9960-4
12. Corry JJ, Ho B, Marino E, et al. Utility of procalcitonin for diagnosis of bacterial infection-related systemic inflammatory response in the acute neurologic injury population. Clin Neurol Neurosurg. 2019;186:105534. doi:10.1016/j.clineuro.2019.105534
13. Debiane L, Hachem RY, Al Wohoush I, et al. The utility of proadrenomedullin and procalcitonin in comparison to C-reactive protein as predictors of sepsis and bloodstream infections in critically ill patients with cancer*. Crit Care Med. 2014;42(12):2500–2507. doi:10.1097/CCM.0000000000000526
14. Simon L, Saint-Louis P, Amre DK, Lacroix J, Gauvin F. Procalcitonin and C-reactive protein as markers of bacterial infection in critically ill children at onset of systemic inflammatory response syndrome. Pediatr Crit Care Med. 2008;9(4):407–413. doi:10.1097/PCC.0b013e31817285a6
15. Schuetz P, Birkhahn R, Sherwin R, et al. Serial procalcitonin predicts mortality in severe sepsis patients: results from the multicenter procalcitonin monitoring sepsis (MOSES) study. Crit Care Med. 2017;45(5):781–789. doi:10.1097/CCM.0000000000002321
16. AlRawahi AN, AlHinai FA, Doig CJ, et al. The prognostic value of serum procalcitonin measurements in critically injured patients: a systematic review. Crit Care. 2019;23(1):390. doi:10.1186/s13054-019-2669-1
17. Sedef AM, Kose F, Mertsoylu H, Ozyilkan O. Procalcitonin as a biomarker for infection-related mortality in cancer patients. Curr Opin Support Palliat Care. 2015;9(2):168–173. doi:10.1097/SPC.0000000000000142
18. Sutter R, Valença M, Tschudin-Sutter S, Rüegg S, Marsch S. Procalcitonin and mortality in status epilepticus: an observational cohort study. Crit Care. 2015;19:361. doi:10.1186/s13054-015-1072-9
19. Muroi C, Lemb JB, Hugelshofer M, Seule M, Bellut D, Keller E. Early systemic procalcitonin levels in patients with aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2014;21(1):73–77. doi:10.1007/s12028-013-9844-z
20. He D, Zhang Y, Zhang B, et al. Serum procalcitonin levels are associated with clinical outcome in intracerebral hemorrhage. Cell Mol Neurobiol. 2018;38(3):727–733. doi:10.1007/s10571-017-0538-5
21. Wang C, Gao L, Zhang ZG, et al. Procalcitonin is a stronger predictor of long-term functional outcome and mortality than high-sensitivity C-reactive protein in patients with ischemic stroke. Mol Neurobiol. 2016;53(3):1509–1517. doi:10.1007/s12035-015-9112-7
22. Li YM, Liu XY. Serum levels of procalcitonin and high sensitivity C-reactive protein are associated with long-term mortality in acute ischemic stroke. J Neurol Sci. 2015;352(1–2):68–73. doi:10.1016/j.jns.2015.03.032
23. Deng S, Zhu H, Wang K, Cao T. Procalcitonin as a marker of sepsis and outcome in patients with neurotrauma: an observation study. BMC Anesthesiol. 2013;13(1):48. doi:10.1186/1471-2253-13-48
24. Han YY, Carcillo JA, Ruppel RA, et al. Cerebrospinal fluid procalcitonin and severe traumatic brain injury in children. Pediatr Crit Care Med. 2002;3(1):39–44. doi:10.1097/00130478-200201000-00010
25. Sauerland S, Hensler T, Bouillon B, et al. Plasma levels of procalcitonin and neopterin in multiple trauma patients with or without brain injury. J Neurotrauma. 2003;20(10):953–960. doi:10.1089/089771503770195803
26. Oconnor E, Venkatesh B, Mashongonyika C, Lipman J, Hall J, Thomas P. Serum procalcitonin and C-reactive protein as markers of sepsis and outcome in patients with neurotrauma and subarachnoid haemorrhage. Anaesth Intensive Care. 2004;32(4):465–470. doi:10.1177/0310057X0403200402
27. Roos BA, Okano K, Deftos LJ. Evidence for a pro-calcitonin. Biochem Biophys Res Commun. 1974;60(3):1134–1140. doi:10.1016/0006-291X(74)90430-6
28. Jacobs JW, Lund PK, Potts JT, Bell NH, Habener JF. Procalcitonin is a glycoprotein. J Biol Chem. 1981;256(6):2803–2807. doi:10.1016/S0021-9258(19)69685-7
29. Maruna P, Nedelníková K, Gürlich R. Physiology and genetics of procalcitonin. Physiol Res. 2000;49(Suppl 1):S57–61.
30. Joyce CD, Fiscus RR, Wang X, Dries DJ, Morris RC, Prinz RA. Calcitonin gene-related peptide levels are elevated in patients with sepsis. Surgery. 1990;108(6):1097–1101.
31. Hensel M, Volk T, Döcke WD, et al. Hyperprocalcitonemia in patients with noninfectious SIRS and pulmonary dysfunction associated with cardiopulmonary bypass. Anesthesiology. 1998;89(1):93–104. doi:10.1097/00000542-199807000-00016
32. Selberg O, Hecker H, Martin M, Klos A, Bautsch W, Köhl J. Discrimination of sepsis and systemic inflammatory response syndrome by determination of circulating plasma concentrations of procalcitonin, protein complement 3a, and interleukin-6. Crit Care Med. 2000;28(8):2793–2798. doi:10.1097/00003246-200008000-00019
33. Whang KT, Steinwald PM, White JC, et al. Serum calcitonin precursors in sepsis and systemic inflammation. J Clin Endocrinol Metab. 1998;83(9):3296–3301. doi:10.1210/jcem.83.9.5129
34. Mimoz O, Benoist JF, Edouard AR, Assicot M, Bohuon C, Samii K. Procalcitonin and C-reactive protein during the early posttraumatic systemic inflammatory response syndrome. Intensive Care Med. 1998;24(2):185–188. doi:10.1007/s001340050543
35. Hatherill M, Tibby SM, Turner C, Ratnavel N, Murdoch IA. Procalcitonin and cytokine levels: relationship to organ failure and mortality in pediatric septic shock. Crit Care Med. 2000;28(7):2591–2594. doi:10.1097/00003246-200007000-00068
36. Sakran JV, Michetti CP, Sheridan MJ, et al. The utility of procalcitonin in critically ill trauma patients. J Trauma Acute Care Surg. 2012;73(2):
37. Anand D, Das S, Bhargava S, et al. Procalcitonin as a rapid diagnostic biomarker to differentiate between culture-negative bacterial sepsis and systemic inflammatory response syndrome: a prospective, observational, cohort study. J Crit Care. 2015;30(1):
38. Tomio R, Akiyama T, Shibao S, Yoshida K. Procalcitonin as an early diagnostic marker for ventriculoperitoneal shunt infections. Surg Infect (Larchmt). 2013;14(5):433–436. doi:10.1089/sur.2012.087
39. Sutter R, Tschudin-Sutter S, Grize L, Widmer AF, Marsch S, Rüegg S. Acute phase proteins and white blood cell levels for prediction of infectious complications in status epilepticus. Crit Care. 2011;15(6):R274. doi:10.1186/cc10555
40. Wang YR, Zheng QB, Wei GF, et al. Elevated PCT at ICU discharge predicts poor prognosis in patients with severe traumatic brain injury: a retrospective cohort study. J Int Med Res. 2020;48(5):300060520922456. doi:10.1177/0300060520922456
41. Chaikittisilpa N, Krishnamoorthy V, Lele AV, Qiu Q, Vavilala MS. Characterizing the relationship between systemic inflammatory response syndrome and early cardiac dysfunction in traumatic brain injury. J Neurosci Res. 2018;96(4):661–670. doi:10.1002/jnr.24100
42. Jacome T, Tatum D. Systemic Inflammatory Response Syndrome (SIRS) score independently predicts poor outcome in isolated traumatic brain injury. Neurocrit Care. 2018;28(1):110–116. doi:10.1007/s12028-017-0410-y
43. Moore FA, Moore EE. Evolving concepts in the pathogenesis of postinjury multiple organ failure. Surg Clin North Am. 1995;75(2):257–277. doi:10.1016/S0039-6109(16)46587-4
44. Nijsten MW, Olinga P, The TH, et al. Procalcitonin behaves as a fast responding acute phase protein in vivo and in vitro. Crit Care Med. 2000;28(2):458–461. doi:10.1097/00003246-200002000-00028
45. Frugier T, Morganti-Kossmann MC, O’Reilly D, McLean CA. In situ detection of inflammatory mediators in post mortem human brain tissue after traumatic injury. J Neurotrauma. 2010;27(3):497–507. doi:10.1089/neu.2009.1120
46. Ziebell JM, Morganti-Kossmann MC. Involvement of pro- and anti-inflammatory cytokines and chemokines in the pathophysiology of traumatic brain injury. Neurotherapeutics. 2010;7(1):22–30. doi:10.1016/j.nurt.2009.10.016
47. Sordillo PP, Sordillo LA, Helson L. Bifunctional role of pro-inflammatory cytokines after traumatic brain injury. Brain Injury. 2016;30(9):1043–1053. doi:10.3109/02699052.2016.1163618
48. Lloyd E, Somera-Molina K, Van Eldik LJ, Watterson DM, Wainwright MS. Suppression of acute proinflammatory cytokine and chemokine upregulation by post-injury administration of a novel small molecule improves long-term neurologic outcome in a mouse model of traumatic brain injury. J Neuroinflammation. 2008;5:28. doi:10.1186/1742-2094-5-28
49. Müller B, White JC, Nylén ES, Snider RH, Becker KL, Habener JF. Ubiquitous expression of the calcitonin-i gene in multiple tissues in response to sepsis. J Clin Endocrinol Metab. 2001;86(1):396–404. doi:10.1210/jcem.86.1.7089
50. Russwurm S, Stonans I, Stonane E, et al. Procalcitonin and CGRP-1 mRNA expression in various human tissues. Shock. 2001;16(2):109–112. doi:10.1097/00024382-200116020-00004
51. Dragunow M, Sirimanne E, Lawlor PA, Williams C, Gluckman P. Accumulation of calcitonin-gene related peptide-like immunoreactivity after hypoxic-ischaemic brain injury in the infant rat. Brain Res Mol Brain Res. 1992;14(3):267–272. doi:10.1016/0169-328X(92)90182-B
52. Hensler T, Sauerland S, Lefering R, et al. The clinical value of procalcitonin and neopterin in predicting sepsis and organ failure after major trauma. Shock. 2003;20(5):420–426. doi:10.1097/01.shk.0000093541.78705.38
53. Choi JJ, McCarthy MW. Novel applications for serum procalcitonin testing in clinical practice. Expert Rev Mol Diagn. 2018;18(1):27–34. doi:10.1080/14737159.2018.1407244
54. Lee S, Hwang H, Yamal JM, et al. IMPACT probability of poor outcome and plasma cytokine concentrations are associated with multiple organ dysfunction syndrome following traumatic brain injury. J Neurosurg. 2019;131(6):1931–1937. doi:10.3171/2018.8.JNS18676
55. Meisel C, Schwab JM, Prass K, Meisel A, Dirnagl U. Central nervous system injury-induced immune deficiency syndrome. Nat Rev Neurosci. 2005;6(10):775–786. doi:10.1038/nrn1765
56. Laborde G, Grosskopf U, Schmieder K, et al. Nosokomiale Infektionen auf einer neurochirurgischen Intensivstation [Nosocomial infections in a neurosurgical intensive care unit]. Der Anaesthesist. 1993;42(10):724–731. German.
57. Dettenkofer M, Ebner W, Hans FJ, et al. Nosocomial infections in a neurosurgery intensive care unit. Acta neurochirurgica. 1999;141(12):1303–1308. doi:10.1007/s007010050434
58. Piek J, Chesnut RM, Marshall LF, et al. Extracranial complications of severe head injury. J Neurosurg. 1992;77(6):901–907. doi:10.3171/jns.1992.77.6.0901
59. Li Y, Liu C, Xiao W, Song T, Wang S. Incidence, risk factors, and outcomes of ventilator-associated pneumonia in traumatic brain injury: a meta-analysis. Neurocrit Care. 2020;32(1):272–285. doi:10.1007/s12028-019-00773-w
60. Kesinger MR, Kumar RG, Wagner AK, et al. Hospital-acquired pneumonia is an independent predictor of poor global outcome in severe traumatic brain injury up to 5 years after discharge. J Trauma Acute Care Surg. 2015;78(2):396–402. doi:10.1097/TA.0000000000000526
61. Schirmer-Mikalsen K, Moen KG, Skandsen T, Vik A, Klepstad P. Intensive care and traumatic brain injury after the introduction of a treatment protocol: a prospective study. Acta Anaesthesiol Scand. 2013;57(1):46–55. doi:10.1111/j.1399-6576.2012.02785.x
62. Vitaz TW, Jenks J, Raque GH, Shields CB. Outcome following moderate traumatic brain injury. Surg Neurol. 2003;60(4):
63. Zygun DA, Zuege DJ, Boiteau PJ, et al. Ventilator-associated pneumonia in severe traumatic brain injury. Neurocrit Care. 2006;5(2):108–114. doi:10.1385/NCC:5:2:108
64. Carabias CS, Gomez PA, Panero I, et al. Chitinase-3-like protein 1, serum amyloid A1, C-reactive protein, and procalcitonin are promising biomarkers for intracranial severity assessment of traumatic brain injury: relationship with Glasgow coma scale and computed tomography volumetry. World Neurosurg. 2020;134:e120–e143. doi:10.1016/j.wneu.2019.09.143
65. Zhou ZW, Li F, Zheng ZT, et al. Erythropoietin regulates immune/inflammatory reaction and improves neurological function outcomes in traumatic brain injury. Brain Behav. 2017;7(11):e00827. doi:10.1002/brb3.827
66. Rodney T, Osier N, Gill J. Pro- and anti-inflammatory biomarkers and traumatic brain injury outcomes: a review. Cytokine. 2018;110:248–256. doi:10.1016/j.cyto.2018.01.012
67. Collins CD, Brockhaus K, Sim T, Suneja A, Malani AN. Analysis to determine cost-effectiveness of procalcitonin-guided antibiotic use in adult patients with suspected bacterial infection and sepsis. Am J Health System Pharm. 2019;76(16):1219–1225. doi:10.1093/ajhp/zxz129
68. Buendía JA, Guerrero Patiño D. Cost-effectiveness of procalcitonin for detection of serious bacterial infections in children presenting with fever without source. BMC Pediatr. 2022;22(1):226. doi:10.1186/s12887-022-03293-3
69. Voermans AM, Mewes JC, Broyles MR, Steuten LMG. Cost-effectiveness analysis of a procalcitonin-guided decision algorithm for antibiotic stewardship using real-world U.S. hospital data. Omics. 2019;23(10):508–515. doi:10.1089/omi.2019.0113
70. Pelinka L, Petto H, Kroepfl A, Schmidhammer R, Redl H. Serum procalcitonin and S100B are associated with mortality after traumatic brain injury. Eur J Trauma. 2003;29:316–323. doi:10.1007/s00068-003-1314-4
71. Goyal K, Tomar GS, Sengar K, et al. Prognostic value of serially estimated serum procalcitonin levels in traumatic brain injury patients with or without extra cranial injury on early in-hospital mortality: a longitudinal observational study. Neurocrit Care. 2021;34(1):182–192. doi:10.1007/s12028-020-01009-y
72. Svedung Wettervik T, Howells T, Ronne-Engström E, et al. High arterial glucose is associated with poor pressure autoregulation, high cerebral lactate/pyruvate ratio and poor outcome following traumatic brain injury. Neurocrit Care. 2019;31(3):526–533. doi:10.1007/s12028-019-00743-2
73. Smith RL, Lin JC, Adelson PD, et al. Relationship between hyperglycemia and outcome in children with severe traumatic brain injury. Pediatr Crit Care Med. 2012;13(1):85–91. doi:10.1097/PCC.0b013e3182192c30
74. Chong SL, Harjanto S, Testoni D, et al. Early hyperglycemia in pediatric traumatic brain injury predicts for mortality, prolonged duration of mechanical ventilation, and intensive care stay. Int J Endocrinol. 2015;2015:719476. doi:10.1155/2015/719476
75. Bosarge PL, Shoultz TH, Griffin RL, Kerby JD. Stress-induced hyperglycemia is associated with higher mortality in severe traumatic brain injury. J Trauma Acute Care Surg. 2015;79(2):289–294. doi:10.1097/TA.0000000000000716
76. Yamano S, Shimizu K, Ogura H, et al. Low total cholesterol and high total bilirubin are associated with prognosis in patients with prolonged sepsis. J Crit Care. 2016;31(1):36–40. doi:10.1016/j.jcrc.2015.09.033
77. Wen CP, Lee YC, Sun YT, et al. Low-density lipoprotein cholesterol and mortality in patients with intracerebral hemorrhage in Taiwan. Front Neurol. 2021;12:793471. doi:10.3389/fneur.2021.793471
78. Lee SH, Lee JY, Hong TH, Kim BO, Lee YJ, Lee JG. Severe persistent hypocholesterolemia after emergency gastrointestinal surgery predicts in-hospital mortality in critically ill patients with diffuse peritonitis. PLoS One. 2018;13(7):e0200187. doi:10.1371/journal.pone.0200187
79. Zhong YH, Zheng BE, He RH, et al. Serum levels of HDL cholesterol are associated with diffuse axonal injury in patients with traumatic brain injury. Neurocrit Care. 2021;34(2):465–472. doi:10.1007/s12028-020-01043-w
80. Lingsma H, Andriessen TM, Haitsema I, et al. Prognosis in moderate and severe traumatic brain injury: external validation of the IMPACT models and the role of extracranial injuries. J Trauma Acute Care Surg. 2013;74(2):639–646. doi:10.1097/TA.0b013e31827d602e
81. Han J, King NK, Neilson SJ, Gandhi MP, Ng I. External validation of the CRASH and IMPACT prognostic models in severe traumatic brain injury. J Neurotrauma. 2014;31(13):1146–1152. doi:10.1089/neu.2013.3003
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.