Back to Journals » Neuropsychiatric Disease and Treatment » Volume 13
Prognostic value of restless legs syndrome in hemodialysis patients: a systematic review and meta-analysis
Authors Li J , Zhang T, Shao Q
Received 19 March 2017
Accepted for publication 28 April 2017
Published 16 June 2017 Volume 2017:13 Pages 1569—1574
DOI https://doi.org/10.2147/NDT.S137478
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Wai Kwong Tang
Jing Li,1,* Tao Zhang,2,* Qingmiao Shao3
1Department of Transplantation, The First Central Hospital of Tianjin, 2Department of Nephrology, The First Affiliated Hospital of Tianjin Chinese Medical University, 3Department of Cardiology, The Second Hospital of Tianjin Medical University, Tianjin, People’s Republic of China
*These authors contributed equally to this work
Background: Previous studies have revealed that restless legs syndrome (RLS) not only is frequently prevalent in dialysis patients but also increases the risk of death in dialysis patients, especially in hemodialysis (HD) patients. However, inconsistent results also still exist, having attracted confusion and discussion. Owing to mixed and inconclusive results, we conducted to perform the comprehensive meta-analysis to evaluate the potential prognostic value of RLS in HD patients.
Materials and methods: We conducted a systematic literature search using electronic databases (PubMed, Ovid, Embase and Web of Science) to identify relevant studies reporting on all-cause mortality and cardiovascular (CV) events in HD patients suffering from RLS. We searched the literature published up to December 5, 2016, or earlier. We used both fixed- and random-effects models to calculate the overall effect estimate. An I2>50% indicates at least moderate statistical heterogeneity. A sensitivity analysis and subgroup analysis were performed to find the origin of heterogeneity.
Results: A total of four studies including 1,839 patients found that there was no significant association between RLS and all-cause mortality (hazard ratio [HR]: 1.649; 95% confidence interval [CI]: 0.778–3.496) and CV events (HR: 0.863; 95% CI: 0.600–1.127) in HD patients. Heterogeneity among the studies was observed for all-cause mortality (I2=80.7%, P=0.001).
Conclusion: Our meta-analysis suggests that there was no significant effect of RLS on all-cause mortality and CV events in HD patients. Therefore, large-scale and well-designed studies are needed to validate the association between RLS and the risk of death in HD patients.
Keywords: restless legs syndrome, hemodialysis, cardiovascular events, mortality, meta-analysis
Introduction
Restless legs syndrome (RLS), a neurological disorder characterized by an almost irresistible urgent, uncontrolled need to move the limbs that is exacerbated by rest and temporarily relieved by motor activity, is worse in the evening and overnight with significant relief in the morning.1–3 RLS affects 5%–10% of adults in the general population and is also associated with increased mortality.4–6 Previous studies found that the prevalence of RLS among hemodialysis (HD) patients is significantly higher than that of the general population.7,8 In recent years, RLS, as a common neurological and sensorimotor disorder, has received more attention from the potential prognostic value in HD patients. A series of studies that have been conducted to investigate the association between RLS and adverse outcomes found that RLS increased all-cause mortality and cardiovascular (CV) events in HD patients.9–11 The relevant mechanisms and factors involved in the relationship between RLS and prognostic value in HD patients are not well clarified. Then, Stefanidis et al12 reported a controversial result that RLS does not affect 3-year mortality in HD patients. Therefore, taking the current research situation into consideration, we performed a systematic review and meta-analysis of prospective observational studies to evaluate the association between RLS and adverse outcomes in HD patients.
Materials and methods
This meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria.13
Search strategies and inclusion criteria
PubMed, Ovid, Embase and Web of Science were searched by two independent researchers (JL and TZ) to identify the relevant studies that evaluated the association between RLS and adverse outcomes in HD patients up to December 5, 2016. The following search terms (in title, abstract or keywords fields) were used as follows: “restless legs syndrome” or “RLS” and “renal failure” or “end-stage renal disease or ESRD” or “hemodialysis or HD” or “dialysis”. Titles and abstracts as well as the reference lists of all of the identified reports were examined independently by two reviewers (JL and TZ) to include potentially relevant studies that reported the association between RLS and adverse outcomes in HD patients.
Studies were considered eligible for this study if they met the following criteria: 1) if they were of a prospective observational study design; 2) if they clearly defined the adverse outcomes, including all-cause mortality and CV events; 3) if they reported the hazard ratio (HR) and the corresponding 95% confidence interval (CI) for RLS and all-cause mortality/CV events in HD patients; 4) only studies that included patients with a diagnosis of RLS that is clearly defined and according to the current guideline-based definitions.
Data extraction
Two reviewers (JL and TZ) independently screened the abstracts or titles of the studies from the electronic search to identify all potential eligible studies. Potentially relevant reports were then retrieved as complete manuscripts and assessed for compliance with the inclusion criteria. Data extraction was performed from eligible studies by two blinded reviewers (JL and TZ) using a standard data extraction form to determine the eligibility for inclusion and extract data. The extracted data elements of this review included: 1) publication details: first author’s last name, publication year and studied population; 2) study design; 3) characteristics of the studied population: sample size, age, gender, the proportion of combined diabetes mellitus and duration of follow-up; 4) end point events; 5) the number of deaths during the follow-up period, and HR and 95% CI about RLS and adverse outcomes in HD patients. Disagreements were resolved by consensus after rechecking the source data and consultation with the third reviewer (QS).
Quality assessment
To limit the heterogeneity secondary to differences among study designs, the quality of each study was evaluated according to a critical review checklist of the Dutch Cochrane Center which was proposed by Meta-analysis Of Observational Studies in Epidemiology (MOOSE).14 The key points of this checklist are as follows: 1) clear definition of study population; 2) clear definition of outcomes and outcome assessment; 3) independent assessment of outcome parameters; 4) sufficient duration of follow-up; 5) no selective loss during follow-up and 6) important confounders and prognostic factors identified. If a study did not clearly mention one of these key points, we considered that it had not been performed and, consequently, that there was a possibility for the underestimation of the reported characteristics.
Statistical analysis
Pooled effect sizes were presented as the HR with 95% CI. We conducted fixed-effects meta-analysis using the inverse variance method for pooling effect sizes, and random-effects meta-analysis using the inverse variance heterogeneity method. To evaluate the heterogeneity across studies, we used I2 derived from the chi-square test. An I2>50% indicates at least moderate statistical heterogeneity. When pooled analysis resulted in significant heterogeneity, the random-effects model was used. To explore the sources of heterogeneity, we performed sensitivity and subgroup analyses (sample size or geographic area). The sensitivity analysis was also performed in a random predefined manner. Publication bias was evaluated using the funnel plot. Statistical significance was defined as a two-tailed P-value of 0.05. All statistical analyses were performed using Stata 11 (Stata Corp LP, College Station, TX, USA).
Results
Literature search outcome
A flow diagram of the data search and study selection is presented in Figure 1. A total of 946 studies were found using our search criteria. We identified 53 duplicate studies, which were discarded. The remaining 893 abstracts were screened further, and we excluded 879 studies, because they were either unrelated, irrelevant, review articles or editorials. Then, full-text studies were then retrieved for detailed evaluation. Of the 14 articles, seven did not meet the inclusion criteria and three did not offer HR about RLS and all-cause mortality or CV events in HD patients, which were both excluded. The remaining four studies were included in our meta-analysis.9–12
  | Figure 1 Flow diagram of the selection process. |
Study characteristics and quality assessment
A total of four studies with 1,839 subjects were included in our meta-analysis study.9–12 The main features of the studies on the association between RLS and adverse outcomes in HD patients are given in Table 1, whereas the quality assessment of the four studies is presented in Table 2. Among these studies, two of four were conducted in Europe,9,12 with the exception of two conducted in Asia.10,11 All eligible studies were published between 2011 and 2015. Four studies were all prospective observational studies. The sample size ranged from 67 to 1,093. Mean patients’ age ranged from 63.6 to 65 years old. The proportion of male in the studies ranged between 56.7% and 63%, and the mean follow-up periods varied from 18 to 44.4 months.
  | Table 2 Assessment of the quality of the four included studies |
RLS and adverse outcomes in HD patients
All-cause mortality
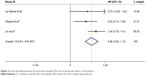
Four studies evaluated the prognostic importance of RLS for all-cause mortality in HD patients.9–12 When pooling data from the studies together, we found that there was no significant association between RLS and all-cause mortality in HD patients (HR: 1.649; 95% CI: 0.778–3.496). Heterogeneity among the studies was observed for all-cause mortality (I2=80.7%, P=0.001; Figure 2).
CV events
Three studies evaluated the prognostic importance of RLS for CV events in HD patients.9–11 When pooling data from the studies together, we found that there was no significant effect of RLS on the development of CV events in HD patients (HR: 0.863; 95% CI: 0.600–1.127) with no heterogeneity among the studies (I2=2.8%, P=0.357; Figure 3).
Sensitivity and subgroup analysis
Of the four studies that reported the association between RLS and all-cause mortality in HD patients,9–12 the heterogeneity test showed that there was significant differences among individual studies (P<0.05; I2=80.7%). A sensitivity analysis was performed to find the origin of heterogeneity. After removing the study by La Manna et al,9 which had a short follow-up period, the analysis did not find significant influences on heterogeneity across studies or overall results. Then, we performed a subgroup analysis according to the sample size (n<200 or n>200), and we found that there was no significant heterogeneity between the two small sample size studies (P=0.517; I2=0.0%)9,10 and there was a significant heterogeneity between the remaining two studies (P=0.017; I2=82.5%).11,12 In addition, we also performed a prespecified subgroup analysis of studies with geographic area of Asian and non-Asian. The proportion of total variation across studies that was due to heterogeneity rather than chance was I2=0.0% (P=0.874) in the two studies with Asian geographic area,10,11 and I2=85.1% (P=0.01) in the two studies with non-Asian geographic area.9,12 Therefore, sample size and geographic area may be a possible source of heterogeneity.
Publication bias
The result of the funnel plot for adverse outcomes in HD patients was symmetrical, indicating no publication bias (Figure 4).
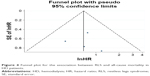  | Figure 4 Funnel plot for the association between RLS and all-cause mortality in HD patients. |
Discussion
In this meta-analysis, four studies involving 1,839 HD patients were analyzed. The result suggests that RLS does not increase the risk of all-cause mortality and CV events in HD patients.
In the past years, large epidemiological studies have indicated a positive association between RLS and all-cause mortality in the general population.4,15 Similarly, some clinic-based studies found the relationship between RLS and all-cause mortality or CV events among subjects with end-stage renal disease, in either transplanted or dialysis patients.9–11 It is reported that RLS mostly suffers from insufficient and disturbed sleep, which in turn affects a large number of physiological and psychological parameters that may be associated with increased mortality.16 In addition, comorbidities, such as diabetes, high blood pressure, iron deficiency, cancer and insomnia, in HD patients with RLS may increase the risk of mortality and CV events.17,18 Moreover, RLS plays a significant role in the sympathetic hyperactivity which results in non-dipping nocturnal blood pressure and atherosclerotic plaque rupture, leading to heart disorders.19 Some direct evidences are linked to RLS and CV events, especially for hypertension or cardiac dysfunction in HD patients.20,21 Surprisingly, our results revealed no evidence of association between RLS and all-cause mortality in HD patients, as for CV events.
There are several possible explanations for the discrepancies in the results regarding this association. First, this lack of association may lie in the different criteria used in the selection of patients. For example, Stefanidis et al12 reported that the age of patients was younger than those without RLS; Lin et al11 reported that RLS patients had higher diabetes prevalence, whereas La Manna et al9 reported that RLS patients had lower frequency of rest diuresis of >500 mL/day. In addition, differences may vary with geographic areas. Age, diabetes and missing rest diuresis are all indubitably strong mortality predictors. While of course adjustments for confounders were performed, whether in our study or in the past studies, confounding bias might not be abolished, even with properly planned multivariate analysis. Second, samples sizes of several of the studies included in our meta-analysis are in the low range compared with genetic studies for other diseases. We performed a subgroup analysis according to the sample size (n<200 or n>200), and we found that there was also significant heterogeneity between the two large sample size studies.9,10 Nonetheless, more comprehensive studies and larger samples are necessary to conclusively determine the presence of this association.
The current study does have some limitations that should be considered. First, the heterogeneity test showed that there was a significant difference among individual studies. The potential sources of differences may be sample size and geographic area. Second, the complexity of complications related to HD patients is what we should take into consideration. It is possible that there may be residual confounding from conditions not included in the analysis. Third, we did not further analyze in the severity classification measurements of RLS, which is a common limitation in this study. The levels of severity on RLS and duration of RLS symptoms may have an important influence on measured outcomes. Finally, considering current incomplete data, we did not further analyze in background therapy, such as the use of a dopamine agonist, which may have a hazardous effect on cardiac function.
Conclusion
Our meta-analysis suggests that there may be no significant effect of RLS on all-cause mortality and CV events in HD patients. There are several possible explanations for the discrepancies in the results regarding this association, such as different criteria used in the selection of patients, geographic areas, age, diabetes, missing rest-diuresis, etc. Given that, it needs large sample and multicenter studies to further assess whether RLS can directly predict all-cause mortality and CV events in HD patients.
Disclosure
The authors report no conflicts of interest in this work.
References
Ekbom KA. Restless legs syndrome. Neurology. 1960;10:868–873. | ||
Allen RP, Picchietti D, Hening WA, et al; Restless Legs Syndrome Diagnosis and Epidemiology workshop at the National Institutes of Health; International Restless Legs Syndrome Study Group. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4(2):101–119. | ||
Garcia-Borreguero D. From restless legs syndrome to Willis-Ekbom disease: a condition reaches full age. Sleep Med Rev. 2012;16:281–282. | ||
Li Y, Wang W, Winkelman JW, Malhotra A, Ma J, Gao X. Prospective study of restless legs syndrome and mortality among men. Neurology. 2013;81(1):52–59. | ||
Mallon L, Broman JE, Hetta J. Restless legs symptoms with sleepiness in relation to mortality: 20-year follow-up study of a middle-aged Swedish population. Psychiatry Clin Neurosci. 2008;62(4):457–463. | ||
Molnar MZ, Lu JL, Kalantar-Zadeh K, Kovesdy CP. Association of incident restless legs syndrome with outcomes in a large cohort of US veterans. J Sleep Res. 2016;25(1):47–56. | ||
Lin CH, Wu VC, Li WY, et al. Restless legs syndrome in end-stage renal disease: a multicenter study in Taiwan. Eur J Neurol. 2013;20(7):1025–1031. | ||
Takaki J, Nishi T, Nangaku M, et al. Clinical and psychological aspects of restless legs syndrome in uremic patients on hemodialysis. Am J Kidney Dis. 2003;41(4):833–839. | ||
La Manna G, Pizza F, Persici E, et al. Restless legs syndrome enhances cardiovascular risk and mortality in patients with end-stage kidney disease undergoing long-term hemodialysis treatment. Nephrol Dial Transplant. 2011;26:1976–1983. | ||
Otsubo S, Tsuchiya K, Akiba T, Nitta K. Relationship between restless legs syndrome and mortality in hemodialysis patients. Nephrol Dial Transplant. 2014;29(suppl 3):iii285. | ||
Lin CH, Sy HN, Chang HW, et al. Restless legs syndrome is associated with cardio/cerebrovascular events and mortality in end-stage renal disease. Eur J Neurol. 2015;22(1):142–149. | ||
Stefanidis I, Vainas A, Giannaki CD, et al. Restless legs syndrome does not affect 3-year mortality in hemodialysis patients. Sleep Med. 2015;16(9):1131–1138. | ||
Swartz MK. The PRISMA statement: a guideline for systematic reviews and meta-analyses. J Pediatr Health Care. 2011;25(1):1–2. | ||
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) Group. JAMA. 2000;283(15):2008–2012. | ||
Li Y, Walters AS, Chiuve SE, Rimm EB, Winkelman JW, Gao X. Prospective study of restless legs syndrome and coronary heart disease among women. Circulation. 2012;126(14):1689–1694. | ||
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. | ||
Gao X, Schwarzschild MA, O’Reilly EJ, Wang H, Ascherio A. Restless legs syndrome and Parkinson’s disease in men. Mov Disord. 2010;25:2654–2657. | ||
Elwood P, Hack M, Pickering J, Hughes J, Gallacher J. Sleep disturbance, stroke, and heart disease events: evidence from the Caerphilly cohort. J Epidemiol Community Health. 2006;60(1):69–73. | ||
Walters AS, Rye DB. Review of the relationship of restless legs syndrome and periodic limb movements in sleep to hypertension, heart disease, and stroke. Sleep. 2009;32(5):589–597. | ||
Gholamrezaei A, Amra B, Mortazavi M. Cardiovascular risk and mortality in end-stage renal disease patients with restless legs syndrome; need for further investigation and looking for underlying mechanisms. Sleep Med. 2013;14(4):385–386. | ||
Giannini G, Zanigni S, Melotti R, et al. Association between restless legs syndrome and hypertension: a preliminary population-based study in South Tyrol, Italy. Eur J Neurol. 2014;21(1):72–78. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.