Back to Journals » OncoTargets and Therapy » Volume 9
Prognostic value of p53 mutation for poor outcome of Asian primary liver cancer patients: evidence from a cohort study and meta-analysis of 988 patients
Received 5 September 2016
Accepted for publication 11 October 2016
Published 8 December 2016 Volume 2016:9 Pages 7425—7433
DOI https://doi.org/10.2147/OTT.S121594
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tohru Yamada
Xiajie Wen,1 Fengmin Lu,1,2 Shuang Liu3
1Department of Epidemiology and Biostatistics, College of Public Health, Zhengzhou University, Zhengzhou, 2Microbiology and Infectious Disease Center, School of Basic Medical Sciences, Peking University Health Science Center, 3Beijing Artificial Liver Treatment and Training Center, Beijing Youan Hospital, Capital Medical University, Beijing, China
Abstract: Several previous studies have investigated the association between gene p53 (p53) mutation and the poor outcome of primary liver cancer (PLC) patients; however, the results remain inconsistent. In the present study, p53 mutation in 60 paired tumor and corresponding nontumor tissues derived from a cohort of 60 PLC patients was systematically analyzed. The results showed that p53 mutation was only an independent risk factor for overall survival (OS), not for recurrence-free survival (RFS), and a meta-analysis was performed to verify this. Online databases were searched up to July 1, 2016. Studies about the association between p53 mutation and the postsurgery survival of PLC patients were collected. A total of 988 patients from eight studies were analyzed; among them, 341 (34.51%) patients had p53 mutation. Pooled hazard ratios (HRs) and 95% confidence intervals (CIs) were 2.03 (1.64, 2.41) and 2.36 (1.31, 3.42) for OS and RFS, respectively. In conclusion, both the cohort study and meta-analysis suggested that the p53 mutation was associated with postsurgery OS in Asian PLC patients. However, the relationship between p53 mutation and recurrence should be confirmed by further studies.
Keywords: p53, primary liver cancer, survival, meta-analysis
Introduction
Primary liver cancer (PLC), ranked as the second and sixth leading cause of cancer deaths in males and females, respectively, is one of the most lethal human malignancy worldwide, and it is especially common in Asia.1,2 Although improved diagnostic techniques and treatment approaches have contributed more patients to receive treatment at early stages, such as liver resection, the mortality rate still remains high due to the frequent recurrence of tumor.3–5 Therefore, the identification of effective prognostic factors is extremely needed for the proper management of PLC patients.
Currently, the available main prognostic factors include the size of tumor, the number of tumor nodules, portal vein tumor thrombus (PVTT), serum level of α-fetoprotein (AFP) and serum ferritin, and whether the patient has metastasis or not. However, the prognostic significance of each single variable has been found to be unsatisfactory so far; some findings even remain controversial.4–8
The gene of p53 residing on chromosome 17p13.1 is a well-known tumor suppressor gene that controls response to several different cellular stresses, including DNA damage, hypoxia, and oncogene activation.9,10 The mutations of p53 had been found in many kinds of cancer and repeatedly reported as a prognostic factor for the clinical outcome of PLC patients.11,12
To explore the role of p53 mutation in predicting the outcome of PLC patients, p53 mutation in paired tissues of 60 Chinese PLC cases was screened for, and then the association between p53 mutation and patients’ long-term clinical outcome was analyzed. Moreover, a meta-analysis including 988 PLC patients to verify the consequence was carried out.
Materials and methods
Study population and their clinical data collection
Tumor tissue specimens were obtained from 60 Chinese patients who had underwent surgical treatment in Henan Cancer Hospital, Zhengzhou, China, between December 2008 and December 2009. All the patients were diagnosed with PLC by pathological diagnosis, and none of them received any chemotherapy or radiotherapy before surgery. By reading the electronic medical record, clinical features and biochemical indicators were collected.
The age of the patients ranged from 34 to 70 years (median 50.82 years). The male to female ratio was 43:17. Serological tests showed that out of the 60 patients, three patients (5.00%) were HBeAg positive and 59 patients (98.33%) were serum hepatitis B surface antigen positive, whereas serum anti-hepatitis C virus (HCV) antibody was present in only one (1.67%) patient. What is more, 58 (96.67%) patients had cirrhosis diagnosed by pathology.
This study was approved by the ethics committee of Peking University Health Science Center, Beijing, China. Written informed consents were obtained from all the participants.
Follow-up
After patients were discharged from hospital, by telephoning or checking patients’ medical records or visiting patients or their relatives, their medical and survival information were collected.
The first and second follow-ups were carried out 1 month and 3 months after hospital discharge, respectively. The patients were then followed up every 3 months for the first year and every 6 months for the following 5 years. The last follow-up was carried out in July 2015. Five of the patients were lost to follow-up and 44 died during the past 5 years.
Method
DNAs were extracted from 60 paired frozen PLC tissues, and for the array-based comparative genomic hybridization (a-CGH) study, the genomic DNAs were extracted using the Genomic DNA PURIFICATION Kit (Qiagen NV, Venlo, the Netherlands). Four independent polymerase chain reactions (PCRs) were used to amplify exons 2–11 of p53. The PCR products were directly sequenced to identify mutation. Chromosome aberration was comprehensively analyzed via a-CGH. In the assay, each corresponding paired adjacent nontumor tissue DNA was used as reference DNA.
In the following analysis, compared to the adjacent nontumor tissue DNA sequences, loss of heterozygosity (LOH) or point mutation of p53 would be defined as p53 mutation of the patients.
Statistical analysis
Chi-square test was used to assess the significance of the associations between p53 mutation and clinical features. Cumulative survival was tested by the Kaplan–Meier method, and the Mantel–Cox model was used to assess the effects of p53 mutation on survival and recurrence. A two-sided P-value <0.05 was defined as statistical significance. These tests were done by SPSS 21.0 (IBM Corporation, Armonk, NY, USA). Stata version 12 (StataCorp LP, College Station, TX, USA) was used, and a random-effect model was conducted if heterogeneity was substantial with the value of I2>50% and χ2 P-value <0.10; if not, fixed-effects model was used for secondary analysis.13 Publication bias was considered if P-value was <0.05 in Egger’s test.
Search strategy and study selection
Comprehensive literature search was conducted in the databases of PubMed, Cochrane Library, and Web of Science with an upper date limit to July 1, 2016. By using the random combination of the search terms “primary liver cancer or hepatocellular carcinoma”, “PLC or HCC”, “p53 or p53 mutation”, “TP53 or TP53 mutation”, and “prognosis, survival, recurrence or outcome”, a total of 653 literatures were found.
Eligible studies were required to match the following criteria: 1) proven pathology diagnosis of PLC patients; 2) reported explicit methods for the detection of p53 mutation; and 3) provided hazard ratio (HR), 95% confidence interval (CI), or crude data.
Data extraction and quality assessment
According to the guidelines of Meta-Analysis of Observational Studies in Epidemiology,14 two reviewers independently extracted the data from each eligible study and a consensus was achieved through discussion in case of disagreement between these two reviewers. Data extracted from the literatures included author, publication year, clinical features, assay method, HR, and 95% CI. If the studies did not report the raw data, HR and CI were extracted according to survival curves by using the previous published methods.15,16 The quality of each study was identified according to the Newcastle–Ottawa Quality Assessment Scale (NOS) for cohort studies.14 However, the literature’s use was limited in the following analysis if the data were not completely reported in the literatures.
Results
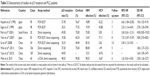
Status of p53 mutation and the clinical features of the patients
A total of 29 out of 60 patients (48.33%) were detected carrying p53 mutation in the present cohort. As the results shown in Table 1 and similar to several previous studies reported, poor mean overall survival (OS) time and short mean recurrence-free survival (RFS) time were observed among patients carrying p53 mutation (P<0.05). No other clinical features were found to be statistically different between the two groups.
Mutation of p53 predicts poor OS in PLC patients
To further evaluate the association of p53 mutation with patients’ poor prognosis after surgical treatment, Kaplan–Meier test was conducted. The results showed that patients with p53 mutation had significantly shorter OS than those without p53 mutation (P=0.002), but RFS did not differ (P=0.738); survival curves are shown in Figure 1.
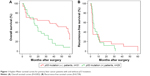  | Figure 1 Kaplan–Meier survival curves for primary liver cancer patients with and without p53 mutation. |
Next, Cox regression multivariate analysis was performed with six other potential clinical variables, including age (≤60 years/>60 years), tumor size (≤5 cm/>5 cm), tumor number (1/≥2), serum level of AFP (≤400 ng/mL/>400 ng/mL), PVTT (−/+), and cirrhosis (−/+). The results are shown in Table 2. Both p53 mutation and large tumor size were the independent predictors for short OS. Other factors, including age, PVTT, cirrhosis, tumor number, and AFP, tended to have influence on survival to some extent, but without significant P-values.
Meta-analysis
Nine studies including the results reported earlier were eligible for meta-analysis; one was performed in the UK and other eight studies including 988 patients were performed in Asia. The basic data are listed in Table 3.11,12,17–23 The mean rate of p53 mutation was 34.51%. One of these studies combined the patients from Asia and Europe including 336 Chinese patients and 73 White patients, and the data about Asian patients were used in the following study.21 The follow-up time postsurgery ranged from 2 to 8 years, and the median time was 4.8 years. Remarkable differences identified among the studies were positive rate of virus infection and cirrhosis. The positive rate of Hepatitis B virus (HBV) ranged from 15.5% to 98.3%, and that of HCV ranged from 1.49% to 77.1%. Excluding one study that did not report cirrhosis rate, the cirrhosis rates ranged from 44.4% to 95.1%. The cohort study research was pooled in the follow-up analyses. Figure 2 shows the forest plots for the association between p53 mutation and OS or RFS. Egger’s test was carried out to assess the publication bias of the studies, and it showed that the publication bias was absent in both the analyses. The P-values of the bias for OS and RFS were 0.405 and 0.830, respectively; funnel plot was also done to value the publication bias (Figure 3).
The summary HR and 95% CI for OS and RFS were 2.03 (1.64, 2.41) and 2.36 (1.31, 3.42), respectively. The result supported p53 mutation as a kind of risk factor for the poor outcome of PLC patients who underwent surgery, which is consistent with a previous report.9
Sensitivity and subgroup analysis
To ensure the reliability of this study, sensitivity analysis was performed, by excluding every individual study, the studies with a score of NOS <5, the largest effect study, and studies with follow-up <5 years. No significant change had happened, and it suggested that no individual study significantly affected the pooled HR, which indicated that the results were statistically robust.
To the authors’ knowledge, the conditions of virus infection and cirrhosis are strong factors for the OS of PLC patients and may contact with p53 conditions.24–26 Therefore, subgroup analyses were performed to eliminate the variances among clinical features in this study.
By dividing the research according to the rate of cirrhosis, HBV infection, HCV infection, number of the patients, and the test method, subgroup analyses showed that the heterogeneity comes from the difference in HBV and HCV infection rate experiment methods and patient number in each research; all the P-values were >0.10 in these subgroups (Table 4).
Discussion
A comprehensive understanding of the influential factors for the OS and RFS is crucial for the improved management of PLC patients. The currently available biomarkers, such as tumor stages, pathological type, and AFP, are representative indicators of the outcome of PLC patients, and identification of new biomarkers reflecting basic hepatocyte carcinogenesis could provide useful insights into disease development and clinical outcomes.27,28 Mutation of p53 is the most common genetic abnormality in human cancers, including PLC. Previously studies had suggested that p53 mutation had statistic relationship with AFP, vascular permeation, and histological differentiation. However, these results were inconsistent.12,17,29 In this study, the correlation was absent between p53 mutation status and AFP level, when the latter was divided by the standard 400 ng/mL, and no statistical differences were found between p53 mutation status and other nine kinds of clinical features. The results suggested that the relationship between p53 mutation and clinical features should be further tested and verified. For survival analysis, meaningful HR 2.58 (1.26, 5.27) between the p53 mutations and OS was only found by Cox regression analysis. Even the mean RFS time of patients with p53 mutation (8.28 months) was obviously shorter than the patients without (13.8 months). However, it is not an independent prognosis factor for RFS.
The possible mechanisms attributed to the prognosis-predicting value of p53 might associate with the biological function of p53. As known, p53 is an important tumor suppressor gene responding to genotoxic and oncogenic stress by inducing cell cycle arrest or apoptosis. p53 has the capacity to regulate the expression of several hundred genes, many of which are involved in mediating or regulating cell growth, division, survival, and programmed cell death.30–32 What is more, p53-null mice were susceptible to spontaneous tumor formation, and the removal of p53 would lead to rapid tumor development and death for various specific cancers.33–35 However, it is worthwhile to notice that cancer relapse is a complicated process and is affected by multiple factors, such as surgery conditions, chemotherapy, radiotherapy, and underlying diseases.36–39 Hence, basic conditions would be considered when using p53 mutation or not as a predict factor for PLC patients.
For the meta-analysis, heterogeneity is also a common problem. According to a previous study, the value of I2, which is adjusted by freedom, would be a better indicator of heterogeneity.40 In this study, the I2 values of OS and RFS were 26.3% and 0, respectively. The background of patients, including gender, age, race, cirrhosis status, and virus infection status, were possible reasons of heterogeneity.26,41,42 Interestingly, the heterogeneity was absent in OS after adjusting the studies by HBV and HCV infection rates, patient number, and experiment method, indicating that these factors might partially account for the appreciable heterogeneity. Cirrhosis might be a potential factor of heterogeneity, however most of the Asian PLC patients had hepatitis virus infection and cirrhosis, and all of the patients in the eight studies analyzed had a high cirrhosis rate, so subgroup analyses did not consider the cirrhosis rate.
Notably, there are some limitations in this study. First, only five articles and the cohort study data with 405 patients can be used for the meta-analysis of RFS. Second, it is difficult to eliminate the effects of publication bias during the meta-analysis; even Egger’s test showed that the publication bias was absent.43
Conclusion
This study suggested that p53 mutation was associated with postsurgery OS in Asia PLC patients, and it might be a new potential prognosis factor for PLC patients.
Disclosure
The authors report no conflicts of interest in this work.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. | ||
Goh GB, Chang PE, Tan CK. Changing epidemiology of hepatocellular carcinoma in Asia. Best Pract Res Clin Gastroenterol. 2015;29(6):919–928. | ||
Lang H, Sotiropoulos GC, Brokalaki EI, et al. Survival and recurrence rates after resection for hepatocellular carcinoma in noncirrhotic livers. J Am Coll Surg. 2007;205(1):27–36. | ||
Shah SA, Cleary SP, Wei AC, et al. Recurrence after liver resection for hepatocellular carcinoma: risk factors, treatment, and outcomes. Surgery. 2007;141(3):330–339. | ||
Tung-Ping Poon R, Fan ST, Wong J. Risk factors, prevention, and management of postoperative recurrence after resection of hepatocellular carcinoma. Ann Surg. 2000;232(1):10–24. | ||
Ferrin G, Aguilar-Melero P, Rodriguez-Peralvarez M, Montero-Alvarez JL, de la Mata M. Biomarkers for hepatocellular carcinoma: diagnostic and therapeutic utility. Hepat Med. 2015;7:1–10. | ||
Thomasset SC, Dennison AR, Garcea G. Ablation for recurrent hepatocellular carcinoma: a systematic review of clinical efficacy and prognostic factors. World J Surg. 2015;39(5):1150–1160. | ||
Facciorusso A, Del Prete V, Antonino M, et al. Serum ferritin as a new prognostic factor in hepatocellular carcinoma patients treated with radiofrequency ablation. J Gastroenterol Hepatol. 2014;29(11):1905–1910. | ||
Liu J, Ma Q, Zhang M, et al. Alterations of TP53 are associated with a poor outcome for patients with hepatocellular carcinoma: evidence from a systematic review and meta-analysis. Eur J Cancer. 2012;48(15):2328–2338. | ||
Vousden KH, Lu X. Live or let die: the cell’s response to p53. Nat Rev Cancer. 2002;2(8):594–604. | ||
Honda K, Sbisa E, Tullo A, et al. p53 mutation is a poor prognostic indicator for survival in patients with hepatocellular carcinoma undergoing surgical tumour ablation. Br J Cancer. 1998;77(5):776. | ||
Sugo H, Takamori S, Kojima K, Beppu T, Futagawa S. The significance of p53 mutations as an indicator of the biological behavior of recurrent hepatocellular carcinomas. Surg Today. 1999;29(9):849–855. | ||
Huedo-Medina TB, Sanchez-Meca J, Marin-Martinez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193–206. | ||
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. | ||
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Response to: practical methods for incorporating summary time-to-event data into meta. Trials. 2013;14(1):391. | ||
Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17(24):2815–2834. | ||
Hayashi H, Sugio K, Matsumata T, Adachi E, Takenaka K, Sugimachi K. The clinical significance of p53 gene mutation in hepatocellular carcinomas from Japan. Hepatology. 1995;22(6):1702–1707. | ||
Park NH, Chung Y-H, Youn KH, et al. Close correlation of p53 mutation to microvascular invasion in hepatocellular carcinoma. J Clin Gastroenterol. 2001;33(5):397–401. | ||
Yano M, Hamatani K, Eguchi H, et al. Prognosis in patients with hepatocellular carcinoma correlates to mutations of p53 and/or hMSH2 genes. Eur J Cancer. 2007;43(6):1092–1100. | ||
Su H, Zhao J, Xiong Y, et al. Large-scale analysis of the genetic and epigenetic alterations in hepatocellular carcinoma from Southeast China. Mutat Res. 2008;641(1–2):27–35. | ||
Villanueva A, Hoshida Y. Depicting the role of TP53 in hepatocellular carcinoma progression. J Hepatol. 2011;55(3):724–725. | ||
Woo HG, Wang XW, Budhu A, et al. Association of TP53 mutations with stem cell-like gene expression and survival of patients with hepatocellular carcinoma. Gastroenterology. 2011;140(3):1063–1070. | ||
Yuan RH, Chang KT, Chen YL, et al. S100P expression is a novel prognostic factor in hepatocellular carcinoma and predicts survival in patients with high tumor stage or early recurrent tumors. PLoS One. 2013;8(6):e65501. | ||
Staib F, Hussain SP, Hofseth LJ, Wang XW, Harris CC. TP53 and liver carcinogenesis. Hum Mutat. 2003;21(3):201–216. | ||
Welzel TM, Graubard BI, Quraishi S, et al. Population-attributable fractions of risk factors for hepatocellular carcinoma in the United States. Am J Gastroenterol. 2013;108(8):1314–1321. | ||
Tornesello ML, Buonaguro L, Tatangelo F, Botti G, Izzo F, Buonaguro FM. Mutations in TP53, CTNNB1 and PIK3CA genes in hepatocellular carcinoma associated with hepatitis B and hepatitis C virus infections. Genomics. 2013;102(2):74–83. | ||
Liver Cancer Study Group of J. Primary liver cancer in Japan. Clinicopathologic features and results of surgical treatment. Ann Surg. 1990;211(3):277–287. | ||
Ma WJ, Wang HY, Teng LS. Correlation analysis of preoperative serum alpha-fetoprotein (AFP) level and prognosis of hepatocellular carcinoma (HCC) after hepatectomy. World J Surg Oncol. 2013;11:212. | ||
Sheen IS, Jeng KS, Wu JY. Is p53 gene mutation an indicator of the biological behaviors of recurrence of hepatocellular carcinoma? World J Gastroenterol. 2003;9(6):1202–1207. | ||
Hu W, Feng Z, Levine AJ. The regulation of multiple p53 stress responses is mediated through MDM2. Genes Cancer. 2012;3(3–4):199–208. | ||
Sherr CJ. Principles of tumor suppression. Cell. 2004;116(2):235–246. | ||
Meek DW. Regulation of the p53 response and its relationship to cancer. Biochem J. 2015;469(3):325–346. | ||
Chen Z, Trotman LC, Shaffer D, et al. Crucial role of p53-dependent cellular senescence in suppression of Pten-deficient tumorigenesis. Nature. 2005;436(7051):725–730. | ||
Zhang J, Xu E, Ren C, et al. Mice deficient in Rbm38, a target of the p53 family, are susceptible to accelerated aging and spontaneous tumors. Proc Natl Acad Sci U S A. 2014;111(52):18637–18642. | ||
Donehower LA, Harvey M, Slagle BL, et al. Mice deficient for p53 are developmentally normal but susceptible to spontaneous tumours. Nature. 1992;356(6366):215–221. | ||
Fatemi SR, Pourhoseingholi MA, Asadi F, et al. Recurrence and five-year survival in colorectal cancer patients after surgery. Iran J Cancer Prev. 2015;8(4):e3439. | ||
Wu JW, Boudreau DM, Park Y, Simonds NI, Freedman AN. Commonly used diabetes and cardiovascular medications and cancer recurrence and cancer-specific mortality: a review of the literature. Expert Opin Drug Saf. 2014;13(8):1071–1099. | ||
Markar S, Gronnier C, Duhamel A, et al. The impact of severe anastomotic leak on long-term survival and cancer recurrence after surgical resection for esophageal malignancy. Ann Surg. 2015;262(6):972–980. | ||
Facciorusso A, Antonino M, Del Prete V, Neve V, Scavo MP, Barone M. Are hematopoietic stem cells involved in hepatocarcinogenesis? Hepatobiliary Surg Nutr. 2014;3(4):199–206. | ||
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. | ||
El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132(7):2557–2576. | ||
Li T, Qin LX, Gong X, et al. Clinical characteristics, outcome, and risk factors for early and late intrahepatic recurrence of female patients after curative resection of hepatocellular carcinoma. Surgery. 2014;156(3):651–660. | ||
Nolting A, Perleth M, Langer G, et al. GRADE Leitlinien: 5. Einschätzung der Qualität der Evidenz - Publikationsbias [GRADE guidelines: 5. Rating the quality of evidence: publication bias]. Z Evid Fortbild Qual Gesundhwes. 2012;106(9):670–676. German. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.