Back to Journals » Cancer Management and Research » Volume 12
Prognostic Value of Inflammation Biomarkers for Survival of Patients with Neuroblastoma
Authors Zheng C, Liu S, Feng J, Zhao X
Received 11 January 2020
Accepted for publication 18 March 2020
Published 1 April 2020 Volume 2020:12 Pages 2415—2425
DOI https://doi.org/10.2147/CMAR.S245622
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Chen Zheng,* Shuaibin Liu,* Jiexiong Feng, Xiang Zhao
Department of Pediatric Surgery, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiang Zhao
Department of Pediatric Surgery, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430030, Hubei Province, People’s Republic of China
Email [email protected]
Purpose: The prognostic significance of inflammation-based biomarkers for neuroblastoma (NB) has not been investigated before. The aim of this study was to evaluate the prognostic value of pre-treatment inflammation biomarkers in children patients with NB.
Patients and Methods: Patients diagnosed with NB from 2008 to 2016 in our institution were enrolled in this study. The clinical data and survival outcomes were retrospectively reviewed. Inflammation biomarkers or scores including C-reactive protein (CRP), albumin (ALB), Glasgow Prognostic Score (GPS), modified Glasgow Prognostic Score (mGPS), high-sensitivity modified Glasgow Prognostic Score (Hs-mGPS), neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR), lymphocyte to monocyte ratio (LMR) and system inflammation index (SII) were tested in this study. Univariate and multivariate survival analyses were performed to assess the prognostic value of these inflammation indicators for overall survival (OS) of children with NB. Kaplan–Meier survival curves were also conducted.
Results: A total of 70 children diagnosed with neuroblastoma were enrolled in this study. NLR, PLR, LMR and SII were found to be not predictive of OS for NB patients. However, CRP, ALB, GPS and CAR were significantly associated with OS of NB patients. Multivariate analysis adjusting for age, sex, histology, tumor size, tumor stage and metastasis revealed that ALB, CAR, GPS and Hs-mGPS were significantly associated with OS of NB patients. Receiver operating characteristic (ROC) curves and Akaike Information Criterion (AIC) analyses revealed that Hs-mGPS is superior to other inflammation biomarkers in predicting OS of NB patients. Subgroup survival analysis for immature NB patients revealed similar results.
Conclusion: Hs-mGPS is an effective prognostic factor for OS of patients with NB and is promising to be used as a factor for risk stratification and an indicator for more aggressive therapy.
Keywords: inflammation, neuroblastoma, biomarker, Glasgow Prognostic Score, survival
Introduction
The links between inflammation and cancer are well established nowadays. Increasing evidences suggested that not only inflammations can cause cancers but also cancers can cause inflammations.1 Cancer-related inflammation may lead to alteration of the cancer biology and tumor-microenvironment and contribute to the progression of malignancy through multiple mechanisms including promotion of proliferation, inhibition of apoptosis, induction of angiogenesis, facilitating metastasis, immunosuppression, and resistance to chemotherapeutic drugs.1–3 Researchers are also beginning to focus on anti-inflammatory agents as new approaches for cancer prevention and treatment.1,2
The association between inflammation and cancer also promoted the investigation of the prognostic role of inflammation-based biomarkers for cancer patients. In recent years, several blood inflammation biomarkers or inflammation-based scores have been found to be predictive of survival for multiple types of cancers. These potential prognostic inflammation indicators include C-reactive protein (CRP), albumin (ALB), Glasgow Prognostic Score (GPS), C-reactive protein to albumin ratio (CAR), neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and systemic immune-inflammation index (SII).4–30
Neuroblastomas (NBs) are the most common extracranial solid malignancy in childhood.31 NBs are a heterogeneous group of tumors composed of cellular aggregates with different degrees of differentiation, from mature ganglioneuroma (GN) to less mature ganglioneuroblastoma (GNB) to immature neuroblastoma (NB).31,32 Although the overall survival (OS) rate for NB increased during the past several decades, the 5-year OS is only about 71% for all children diagnosed with NB.31 Improvement of the risk stratification factor and therapeutic methods for NB is still required.
Numerous evidences also revealed that inflammatory molecules and inflammatory cells play important roles in the progression and metastasis of NB.33–43 However, the prognostic significance of inflammation biomarkers in the blood for the survival of NB patients has not been investigated before. Therefore, we conducted the current retrospective study to investigate the prognostic significance of pre-treatment blood inflammation biomarkers or scores for the OS of the patients with NB in our institution. The results showed that NLR, PLR, LMR, and SII were not predictive of OS, while CAR and Hs-mGPS were significantly associated with OS of NB patients in both univariate model and multivariate model survival analysis.
Materials and Methods
Patients
Between January 2008 to December 2016, 86 consecutive patients pathologically diagnosed with neuroblastic tumors at Tongji Hospital of Huazhong University of Science and Technology were retrospectively reviewed. The inclusion criteria were as follows: (1) patients pathologically diagnosed with GN, GNB, or NB; (2) patients with complete follow-up data and clear end points; (3) patients with complete data of laboratory test of pre-treatment inflammation biomarkers. The exclusion criteria were as follows: (1) Patients with evidence of infectious disease or other inflammatory conditions; (2) patients with incomplete clinical data or incomplete survival data. Finally, 70 children patients with complete data were enrolled in this study.
The patients were routinely followed up every 3 months during the first 3 years after initial treatment and every 6 months subsequently. The last follow-up date was November 2019. Clinical characteristics of the patients including age at diagnosis, sex, INSS (International Neuroblastoma Staging System) stage, metastasis status at diagnosis and tumor size were extracted. Since age at diagnosis younger than 18 months usually associated with good survival of NB patients, the age status was categorized accordingly (age ≤18 months versus age >18 months).31
Ethical Approval
This study was approved by the Ethics Committee of Tongji Hospital of Huazhong University of Science and Technology. The study was performed in accordance with the ethical standards of the Declaration of Helsinki. Written informed consent was obtained from all the participants’ legal guardians.
Inflammation-Based Biomarkers or Scores
The blood test for CRP level, ALB level, neutrophil counts, lymphocyte counts, monocyte counts, and platelet counts were obtained 1 to 7 days before surgery or any other treatment was carried out. Three types of GPS score were calculated as previously reported: (1) traditional GPS, which is derived by allocating 1 point each for elevated CRP (>10 mg/L) and hypoalbuminemia (serum albumin <35 g/L), so that patients with both, one, or none of these conditions would have scores of 2, 1, or 0; (2) modified GPS (mGPS), in which hypoalbuminemia was assigned a score of 0 in the absence of an elevated CRP; (3) high-sensitivity modified GPS (Hs-mGPS), in which 3 mg/L (rather than 10 mg/L) is used as the CRP cut-off value.44 CAR was calculated as CRP to ALB ratio. NLR was calculated as neutrophil counts to lymphocyte counts ratio. PLR was platelet counts to lymphocyte counts ratio. LMR was lymphocyte counts to monocyte counts ratio. SII was calculated as platelet counts × neutrophil counts/lymphocyte counts.20–22
Statistical Analysis
Univariate and multivariate survival analyses were performed by Cox proportional hazards model to estimate the hazard ratios (HR) with 95% confidence intervals (CI). An observed HR > 1 indicated worse outcomes for the tested biomarkers. The time-dependent receiver operating characteristic (ROC) curve and area under curve (AUC) analyses were used to evaluate the sensitivity and specificity of the investigated biomarkers. The optimal cutoff values for continuous variables were determined by Youden’s index (sensitivity + specificity – 1), and the value which has the highest Youden’s index was chosen as the optimal cut-off value. Akaike Information Criterion (AIC) analysis was also performed to compare the discriminative ability of different biomarkers. Survival curves were constructed using the Kaplan–Meier method and evaluated by Log-rank test. The difference between groups was evaluated by the Mantel–Haenszel chi-square test. Statistical analyses were carried out using the SPSS Statistics software version 18 (IBM Corporation, USA). AIC analyses were performed by STATA statistical software package version 15.0 (Stata Corporation, College Station, USA). All statistical tests were two-tailed and p < 0.05 was considered statistically significant.
Results
Patients Characteristics
A total of 70 patients pathologically diagnosed with neuroblastoma were enrolled in the current study, with 31 female patients and 39 male patients. Twenty-one patients were diagnosed under the age of 18 months, and 49 were diagnosed older than 18 months. Twenty-two cases were categorized as INSS 1, eight cases were INSS 2, 14 cases were INSS 3, and 26 cases were INSS 4. The histology subtypes include GN (n=1), GNB (n=13) and NB (n=56). Twenty-three patients received surgery followed by observation, 35 patients received surgery followed by routine chemotherapy, 9 patients received neoadjuvant chemotherapy and followed by surgery and routine chemotherapy, and three patients received only chemotherapy after surgical biopsy. Twenty-six cases were with a tumor size less than 5 cm (diameter) and 44 cases were with a tumor size larger than 5 cm (diameter). The average follow-up time is 53.1 months.
Survival Analysis for Overall Neuroblastoma Patients
Univariate survival analysis (Table 1) revealed that clinical characteristics including age (HR=3.31; 95% CI=1.15–9.53; p=0.026), INSS stage (HR=4.22; 95% CI=1.71–10.39; p=0.002), tumor size (HR=2.85; 95% CI=1.16–7.00; p=0.023), and metastasis (HR=4.49; 95% CI=2.10–9.62; p<0.001) were significantly associated with OS of the patients. As for the inflammation biomarkers, CRP (HR=3.96; 95% CI=1.88–8.35; p<0.001), ALB (HR=2.67; 95% CI=1.18–6.03; p=0.019), GPS (HR=4.74; 95% CI=2.19–10.25; p<0.001), mGPS (HR=3.96; 95% CI=1.89–8.25; p<0.001), Hs-mGPS (HR=8.80; 95% CI=3.55–21.8; p<0.001), and CAR (HR=8.74; 95% CI=2.07–36.80; p=0.003) were significantly associated with OS of the patients. However, NLR, PLR, LMR and SII have no predictive value for OS of NB patients.
 |
Table 1 Univariate and Multivariate Cox Regression Analyses for Overall Survival of Patients with Neuroblastoma |
Multivariate survival analyses (Table 1) for the inflammation biomarkers were performed by adjusting for clinical characteristics including age, sex, INSS stage, histology, tumor size and metastasis. The results of the multivariate analyses showed that ALB (HR=3.32; 95% CI=1.38–7.99; p=0.007), GPS (HR=2.96; 95% CI=1.16–7.56; p=0.023), Hs-mGPS (HR=6.18; 95% CI=2.21–17.27; p=0.001) and CAR (HR=6.75; 95% CI=1.48–30.82; p=0.014) were significantly associated with OS of NB patients.
ROC Curve and AIC Analysis
The ROC curve and AUC analyses were performed to determine the optimal cutoff values for CAR and the value which has the highest Youden’s index was chosen as the optimal cut-off value (0.0959). Since NLR, PLR, LMR, and SII were not shown to be predictive of OS by univariate Cox proportional model survival analysis, no further analysis was conducted for these biomarkers.
ROC curves and AUC analyses were also performed to evaluate the discriminatory ability of those inflammation biomarkers (Figure 1A and Table 2). The results revealed that Hs-mGPS has the highest AUC level (AUC=0.881; 95%=0.702–0.920; p<0.001) in predicting OS. AIC analyses also revealed that Hs-mGPS has the lowest AIC level (206.0429) in predicting OS (Table 2). These results suggested that Hs-mGPS is superior to other inflammation biomarkers in predicting OS of NB patients.
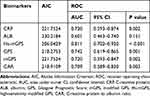 |
Table 2 ROC Curves and AIC Analyses for the Predictive Ability of the Inflammation Biomarkers in Patients with Neuroblastoma |
Kaplan–Meier Survival Curves
The survival curves of the prognostic inflammation biomarkers for patients with neuroblastoma were generated by the Kaplan–Meier method as is shown in Figure 2. Patients with elevated CRP level had significantly worse OS than those with normal CRP level (Figure 2A, p < 0.001). Patients with hypoalbuminemia had significantly worse OS than those with normal ALB level (Figure 2B, p =0.014). Patients with higher CAR value had significantly worse OS than those with lower CAR value (Figure 2C, p < 0.001). Patients with elevated GPS score (GPS, mGPS or Hs-mGPS) had significantly worse OS than those with normal GPS score (Figure 2D–F; p < 0.001, respectively).
Subgroup Analysis for Immature Neuroblastoma Patients
Univariate survival analysis (Table 3) revealed that clinical characteristics including age (HR=4.25; 95% CI=1.45–12.40; p=0.008), INSS stage (HR=3.44; 95% CI=1.29–9.19; p=0.014), tumor size (HR=2.92; 95% CI=1.16–7.31; p=0.023), and metastasis (HR=3.93; 95% CI=1.72–8.99; p=0.001) were significantly associated with OS of patients with immature NB. As for the inflammation biomarkers, CRP (HR=3.27; 95% CI=1.46–7.31; p=0.004), GPS (HR=4.03; 95% CI=1.73–9.40; p=0.001), mGPS (HR=3.27; 95% CI=1.46–7.31; p=0.004), Hs-mGPS (HR=8.94; 95% CI=3.05–26.26; p<0.001), and CAR (HR=15.35; 95% CI=2.07–113.71; p=0.008) were significantly associated with OS of patients with immature NB. However, NLR, PLR, LMR and SII have no predictive value for OS.
 |
Table 3 Univariate and Multivariate Cox Regression Survival Analyses for Overall Survival of Patients with Immature Neuroblastoma |
Multivariate survival analyses (Table 3) adjusted for clinical characteristics including age, sex, INSS stage, tumor size and metastasis showed that ALB (HR=2.81; 95% CI=1.03–7.68; p=0.044), Hs-mGPS (HR=6.01; 95% CI=1.84–19.57; p=0.003) and CAR (HR=12.52; 95% CI=1.57–100.02; p=0.017) were significantly associated with OS of the patients with immature NB.
ROC Curve and AIC Analysis
ROC curves and AUC analyses revealed that Hs-mGPS has the highest AUC level (AUC=0.807; 95%=0.687–0.927; p<0.001) in predicting OS for patients with immature NB (Figure 1B and Table 4). AIC analyses also revealed that Hs-mGPS has the lowest AIC level (167.7397) in predicting OS for patients with immature NB (Table 4). These results suggested that Hs-mGPS is also superior to other inflammation biomarkers in predicting OS for patients with immature NB.
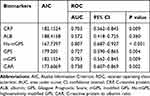 |
Table 4 ROC Curves and AIC Analyses for the Predictive Ability of the Inflammation Biomarkers in Patients with Immature Neuroblastoma |
Kaplan–Meier Survival Curves
The survival curves of the prognostic inflammation biomarkers for NB patients were generated by Kaplan–Meier method as is shown in Figure 3. Patients with elevated CRP level had significantly worse OS than those with normal CRP level (Figure 3A, p = 0.002). Serum ALB level could not significantly stratify NB patients into two different survival groups (Figure 3B, p =0.1). Patients with higher CAR value had significantly worse OS than those with lower CAR value (Figure 3C, p < 0.001). Patients with elevated GPS score had significantly worse OS than those with normal GPS score (p = 0.001, p = 0.009 and p < 0.001 for GPS, mGPS and Hs-mGPS, respectively) (Figure 3D–F).
Discussion
Numerous studies have confirmed the links between inflammation and neuroblastoma.36 For example, high expression of Chemokine receptor-4 (CXCR4) was found in NB tumors with high-stage and in NB patients with bone or bone marrow metastasis; NB patients with tumors highly expressing CXCR4 also had a significantly bad survival outcome.36,38 Pro-inflammatory transcription factor NF-κB is constitutively activated in S-type neuroblastoma and is required for the survival of tumor cell.36,40 NB cells metastasized to the bone marrow could stimulate the expression of interleukin-6 (IL-6), whereas IL-6 could also increase the proliferation of IL-6-R-positive NB cells and protect the tumor cell from etoposide-induced apoptosis; NB patients with bone metastasis were also found to have an elevated level of IL-6 in the serum.36,41 There was also evidences revealed that interactions between NB tumor and inflammatory cells promote the progression and metastasis of NB.36,39,42,43 Metastatic neuroblastoma was shown to have higher infiltration of tumor-associated macrophages (TAMs) than locoregional tumors.39 Bone marrow-derived mesenchymal stem cells (BM-MSCs) and peripheral blood mononuclear cell (PBMC)-derived macrophages could be recruited to the tumor site and activated into TAMs and cancer-associated fibroblast (CAF), and then promote the progression of neuroblastoma by forming a favorable environment.42 Tumor-infiltrating T lymphocytes (TILs) were shown to have an influence on the behavior of neuroblastoma and might be important for the treatment of NB patients.43
The relationship between blood inflammation biomarkers and the prognosis of NB patients has not been investigated before. In the present study, we for the first time demonstrated that two serum-tested inflammation-based scores (CAR and Hs-mGPS) were significantly associated with OS of NB patients in both univariate survival analysis and multivariate survival analysis adjusted by clinical risk factors. The ROC curve and AIC analysis revealed that Hs-mGPS was superior to other inflammation biomarkers in the discriminative ability of predicting OS of NB patients. A number of studies have also found similar results for the prognostic role CAR or GPS in various types of cancers.7–9,45–62 This highlighted the general prognostic role of these two inflammation-based scores in malignancies.
It has to be mentioned that both of the two composite inflammation scores were based on serum CRP and ALB levels. CRP is a non-specific serum biomarker of acute-phase inflammatory response, while Low serum ALB is often used as an indicator for malnutrition, inflammation activity and disease progression in clinical practice.4,63 Either elevated serum CRP level or low serum ALB level has been shown to be associated with poor survival in multiple types of cancer patients.4,6,23-30 Taken together with the prognostic role GPS and CAR for cancer patients, these evidences highlight the importance of serum CRP and ALB level in the prediction of survival for malignancies. Elevated CRP level or low ALB level might represent an inherent aggressive propensity of the cancers including neuroblastoma. In the present study, we also identified that elevated CRP level or low ALB level was significantly associated with poor OS of patients with neuroblastoma in the univariate analysis, but not in the multivariate analysis adjusted by clinical risk factor. However, the combined use of CRP and ALB into CAR or Hs-mGPS revealed really good results in both univariate model and multivariate model survival analysis. It is very interesting that a high serum CRP level has also been linked to PD-L1 (programmed death-ligand 1) positivity in patients with non-small cell lung cancer.4,64 Since PD-1 (programmed death 1) and PD-L1 are also involved with neuroblastoma,36 elevated serum CRP level might also be a potential indicator for immune checkpoint blockade therapy with anti-PD-1 antibodies for NB patients.
Surprisingly, we did not find any role of NLR, PLR, LMR or SII in predicting the survival of NB patients. This result is contrary to previous studies focusing on other types of malignancies, while a number of studies found a positive result for NLR, PLR, LMR or SII in the role of predicting the survival for cancer patients.5,10-13,16–22 In fact, these markers also have their theoretical foundations for predicting the survival of cancer patients. For example, neutrophils could produce various factors that could promote tumor cell proliferation and invasion; lymphocytes could mediate cytotoxic cell death and inhibiting tumor cell proliferation and metastasis; monocytes in the peripheral blood reflect the status of TAM in patients, while TAM derived from monocytes inhibit immune response and promote tumor growth; elevated platelet counts could stimulate tumor angiogenesis and promote tumor metastasis.21,65,66 As we have mentioned above, TAMs or TILs also have an influence on the behavior of NB. However, we did not find any association between NLR, LMR, PLR or SII with the survival of NB patients. We think one possible reason responsible for this discrepancy is that the normal level of blood neutrophil counts, lymphocyte counts and monocytes counts vary among children with different age group, so that those markers based on these blood cell counts lose their prognostic function in children patients.
Since three subtypes of GPS (traditional GPS, mGPS and Hs-mGPS) have been reported in previous studies, we investigated the prognostic value of all the three subtypes of GPS in our study. The results revealed that all of the three subtypes of GPS are significantly associated with the survival of NB patients in the univariate model survival analysis. However, in the multivariate analysis adjusted by clinical risk factors, only Hs-mGPS was shown to be significantly associated with OS for patients with immature NB. Hs-mGPS was also shown to be superior to the other two kinds of GPS in the ROC curve analysis and AIC analyses both in the total cohort and in the immature NB subgroup. Different from GPS and mGPS, 3 mg/L (rather than 10 mg/L) is used as the CRP cut-off value in Hs-mGPS. We think that one reason for the superior of Hs-mGPS might be that children rarely have concomitant conditions that could affect serum CRP level, such as cardiovascular disease or rheumatic diseases. The level of serum CRP in healthy children is supposed to be less than 3 mg/L, while adults with subclinical cardiovascular disease would have a CRP level lager than 3 mg/L.
CAR is another promising biomarker calculated by the ratio of CRP level to ALB level as demonstrated in previous studies.7,8 In the present study, we also find that CAR is significantly associated with the survival of NB patients either in univariate model or multivariate model survival analysis. However, the determination of the optimal cut-off value for CAR holds back its clinical use as a convenient indicator. The optimal cut-off value may vary among different studies. As we have shown in one previous study, the optimal cut-off value for CAR varies from 0.1035 to 1.5 among 4 studies investigating the prognostic role of CAR for sarcoma.44
There are some limitations to the present study. Firstly, this is a retrospective study, and only a small number of patients were enrolled, the results should be undoubtedly interpreted with caution. Secondly, the patients in this study are all Chinese children; the results may not be applicable for patients in other districts of the world. Thirdly, the MYCN amplification status, which is one of the most important risk factors for NB, is unavailable for most of the patients in this study. In the early days, the MYCN status was not detected in our institution due to technical reasons. We recommend future studies including the MYCN amplification status as covariate when investigate the independent prognostic role of these inflammation biomarkers. Prospective studies with larger sample size are also required to verify the conclusion of this study.
Conclusion
In this retrospective study, we identified that NLR, PLR, LMR, and SII were not predictive of OS for patients with NB. However, Hs-mGPS and CAR were shown to be significantly associated with OS of NB patients in both univariate analysis and multivariate analysis adjusted by clinical risk factors. The prognostic role of Hs-mGPS is superior to other inflammation biomarkers. Elevated Hs-mGPS might represent an aggressive propensity of neuroblastoma. Since CRP and ALB are both readily accessible and cheap laboratory parameters widely used in clinical routine, it is promising for Hs-mGPS to be used as a factor of risk stratification and indicator for more aggressive therapy for NB patients.
Acknowledgments
This research was supported by the National Natural Science Foundation of China (grant number 81702472) and the Sanming Project of Medicine in Shenzhen (grant number SZSM201812055). We wish to thank Xinmei Nie for her English language support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Crusz SM, Balkwill FR. Inflammation and cancer: advances and new agents. Nat Rev Clin Oncol. 2015;12(10):584–596. doi:10.1038/nrclinonc.2015.105
2. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–444. doi:10.1038/nature07205
3. Zitvogel L, Pietrocola F, Kroemer G. Nutrition, inflammation and cancer. Nat Immunol. 2017;18(8):843–850. doi:10.1038/ni.3754
4. Wang X, Liu S, Zhao X, Fang E, Zhao X, Brigman BE. The value of C-reactive protein as an independent prognostic indicator for disease-specific survival in patients with soft tissue sarcoma: a meta-analysis. PLoS One. 2019;14(7):e0219215. doi:10.1371/journal.pone.0219215
5. Semeniuk-Wojtas A, Lubas A, Stec R, Syrylo T, Niemczyk S, Szczylik C. Neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and C-reactive protein as new and simple prognostic factors in patients with metastatic renal cell cancer treated with tyrosine kinase inhibitors: a systemic review and meta-analysis. Clin Genitourin Cancer. 2018;16(3):e685–e693. doi:10.1016/j.clgc.2018.01.010
6. Kim WR, Han YD, Min BS. C-reactive protein level predicts survival outcomes in rectal cancer patients undergoing total mesorectal excision after preoperative chemoradiation therapy. Ann Surg Oncol. 2018;25(13):3898–3905. doi:10.1245/s10434-018-6828-4
7. Li YJ, Yao K, Lu MX, Zhang WB, Xiao C, Tu CQ. Prognostic value of the C-reactive protein to albumin ratio: a novel inflammation-based prognostic indicator in osteosarcoma. Onco Targets Ther. 2017;10:5255–5261. doi:10.2147/OTT.S140560
8. Li YJ, Yang X, Zhang WB, Yi C, Wang F, Li P. Clinical implications of six inflammatory biomarkers as prognostic indicators in ewing sarcoma. Cancer Manag Res. 2017;9:443–451. doi:10.2147/CMAR.S146827
9. Maretty-Kongstad K, Aggerholm-Pedersen N, Keller J, Safwat A. A validated prognostic biomarker score for adult patients with nonmetastatic soft tissue sarcomas of the trunk and extremities. Transl Oncol. 2017;10(6):942–948. doi:10.1016/j.tranon.2017.09.002
10. Miyamoto R, Inagawa S, Sano N, Tadano S, Adachi S, Yamamoto M. The neutrophil-to-lymphocyte ratio (NLR) predicts short-term and long-term outcomes in gastric cancer patients. Eur J Surg Oncol. 2018;44(5):607–612. doi:10.1016/j.ejso.2018.02.003
11. Zheng J, Cai J, Li H, et al. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as prognostic predictors for hepatocellular carcinoma patients with various treatments: a meta-analysis and systematic review. Cell Physiol Biochem. 2017;44(3):967–981. doi:10.1159/000485396
12. Valero C, Pardo L, Lopez M, et al. Pretreatment count of peripheral neutrophils, monocytes, and lymphocytes as independent prognostic factor in patients with head and neck cancer. Head Neck. 2017;39(2):219–226. doi:10.1002/hed.24561
13. Gemenetzis G, Bagante F, Griffin JF, et al. Neutrophil-to-lymphocyte ratio is a predictive marker for invasive malignancy in intraductal papillary mucinous neoplasms of the pancreas. Ann Surg. 2017;266(2):339–345. doi:10.1097/SLA.0000000000001988
14. Lim WS, Roh JL, Kim SB, Choi SH, Nam SY, Kim SY. Pretreatment albumin level predicts survival in head and neck squamous cell carcinoma. Laryngoscope. 2017;127(12):E437–E442. doi:10.1002/lary.26691
15. Willegger M, Posch F, Schieder S, et al. Serum creatinine and albumin predict sarcoma-specific survival in patients with myofibroblastic and fibroblastic sarcomas. J Orthop Res. 2017;35(12):2815–2824. doi:10.1002/jor.v35.12
16. Goto W, Kashiwagi S, Asano Y, et al. Predictive value of lymphocyte-to-monocyte ratio in the preoperative setting for progression of patients with breast cancer. BMC Cancer. 2018;18(1):1137. doi:10.1186/s12885-018-5051-9
17. Kano S, Homma A, Hatakeyama H, et al. Pretreatment lymphocyte-to-monocyte ratio as an independent prognostic factor for head and neck cancer. Head Neck. 2017;39(2):247–253. doi:10.1002/hed.24576
18. Diem S, Schmid S, Krapf M, et al. Neutrophil-to-Lymphocyte ratio (NLR) and Platelet-to-Lymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer. 2017;111:176–181. doi:10.1016/j.lungcan.2017.07.024
19. Yodying H, Matsuda A, Miyashita M, et al. Prognostic significance of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in oncologic outcomes of esophageal cancer: a systematic review and meta-analysis. Ann Surg Oncol. 2016;23(2):646–654. doi:10.1245/s10434-015-4869-5
20. Chen JH, Zhai ET, Yuan YJ, et al. Systemic immune-inflammation index for predicting prognosis of colorectal cancer. World J Gastroenterol. 2017;23(34):6261–6272. doi:10.3748/wjg.v23.i34.6261
21. Zhang W, Wang R, Ma W, et al. Systemic immune-inflammation index predicts prognosis of bladder cancer patients after radical cystectomy. Ann Transl Med. 2019;7(18):431. doi:10.21037/atm
22. Fu H, Zheng J, Cai J, et al. Systemic Immune-Inflammation Index (SII) is useful to predict survival outcomes in patients after liver transplantation for hepatocellular carcinoma within hangzhou criteria. Cell Physiol Biochem. 2018;47(1):293–301. doi:10.1159/000489807
23. Schmid M, Schneitter A, Hinterberger S, Seeber J, Reinthaller A, Hefler L. Association of elevated C-reactive protein levels with an impaired prognosis in patients with surgically treated endometrial cancer. Obstet Gynecol. 2007;110(6):1231–1236. doi:10.1097/01.AOG.0000292085.50987.f2
24. Polterauer S, Grimm C, Tempfer C, et al. C-reactive protein is a prognostic parameter in patients with cervical cancer. Gynecol Oncol. 2007;107(1):114–117. doi:10.1016/j.ygyno.2007.06.001
25. Woo HD, Kim K, Kim J. Association between preoperative C-reactive protein level and colorectal cancer survival: a meta-analysis. Cancer Causes Control. 2015;26(11):1661–1670. doi:10.1007/s10552-015-0663-8
26. Nozoe T, Saeki H, Sugimachi K. Significance of preoperative elevation of serum C-reactive protein as an indicator of prognosis in esophageal carcinoma. Am J Surg. 2001;182(2):197–201. doi:10.1016/S0002-9610(01)00684-5
27. Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J. 2010;9(1):69. doi:10.1186/1475-2891-9-69
28. Asher V, Lee J, Bali A. Preoperative serum albumin is an independent prognostic predictor of survival in ovarian cancer. Med Oncol. 2012;29(3):2005–2009. doi:10.1007/s12032-011-0019-5
29. Yamamoto M, Saito H, Uejima C, et al. Combination of serum albumin and cholinesterase levels as prognostic indicator in patients ith colorectal cancer. Anticancer Res. 2019;39(2):1085–1090. doi:10.21873/anticanres.13217
30. Lien YC, Hsieh CC, Wu YC, et al. Preoperative serum albumin level is a prognostic indicator for adenocarcinoma of the gastric cardia. J Gastrointest Surg. 2004;8(8):1041–1048. doi:10.1016/j.gassur.2004.09.033
31. PDQ(R) Pediatric Treatment Editorial Board. Neuroblastoma treatment (PDQ(R)): health professional version. In: PDQ Cancer Information Summaries. Bethesda (MD): National Cancer Institute (US); 2002.
32. Joshi VV, Silverman JF. Pathology of neuroblastic tumors. Semin Diagn Pathol. 1994;11(2):107–117.
33. Morandi F, Levreri I, Bocca P, et al. Human neuroblastoma cells trigger an immunosuppressive program in monocytes by stimulating soluble HLA-G release. Cancer Res. 2007;67(13):6433–6441. doi:10.1158/0008-5472.CAN-06-4588
34. Nohava K, Malipiero U, Frei K, Fontana A. Neurons and neuroblastoma as a source of macrophage colony-stimulating factor. Eur J Immunol. 1992;22(10):2539–2545. doi:10.1002/(ISSN)1521-4141
35. Castellani C, Singer G, Kaiser M, et al. Neuroblastoma causes alterations of the intestinal microbiome, gut hormones, inflammatory cytokines, and bile acid composition. Pediatr Blood Cancer. 2017;64(8). doi:10.1002/pbc.26425
36. Nallasamy P, Chava S, Verma SS, et al. PD-L1, inflammation, non-coding RNAs, and neuroblastoma: immuno-oncology perspective. Semin Cancer Biol. 2018;52(Pt 2):53–65. doi:10.1016/j.semcancer.2017.11.009
37. Zhao Q, Jin M, Zhang DW, et al. Serum interleukin-6 level and the rs1800795 polymorphism in its gene associated with neuroblastoma risk in Chinese children. Chin Med J. 2018;131(9):1075–1078. doi:10.4103/0366-6999.230719
38. Russell HV, Hicks J, Okcu MF, Nuchtern JG. CXCR4 expression in neuroblastoma primary tumors is associated with clinical presentation of bone and bone marrow metastases. J Pediatr Surg. 2004;39(10):1506–1511. doi:10.1016/j.jpedsurg.2004.06.019
39. Asgharzadeh S, Salo JA, Ji L, et al. Clinical significance of tumor-associated inflammatory cells in metastatic neuroblastoma. J clin oncol. 2012;30(28):3525–3532. doi:10.1200/JCO.2011.40.9169
40. Bian X, Opipari AW
41. Ara T, Song L, Shimada H, et al. Interleukin-6 in the bone marrow microenvironment promotes the growth and survival of neuroblastoma cells. Cancer Res. 2009;69(1):329–337. doi:10.1158/0008-5472.CAN-08-0613
42. Hashimoto O, Yoshida M, Koma Y, et al. Collaboration of cancer-associated fibroblasts and tumour-associated macrophages for neuroblastoma development. J Pathol. 2016;240(2):211–223. doi:10.1002/path.4769
43. Mina M, Boldrini R, Citti A, et al. Tumor-infiltrating T lymphocytes improve clinical outcome of therapy-resistant neuroblastoma. Oncoimmunology. 2015;4(9):e1019981. doi:10.1080/2162402X.2015.1019981
44. Fang E, Wang X, Feng J, Zhao X. The prognostic role of glasgow prognostic score and C-reactive protein to albumin ratio for sarcoma: a system review and meta-analysis. Dis Markers. 2020;2020:8736509. doi:10.1155/2020/8736509
45. Abe T, Tashiro H, Kobayashi T, Hattori M, Kuroda S, Ohdan H. Glasgow prognostic score and prognosis after hepatectomy for hepatocellular carcinoma. World J Surg. 2017;41(7):1860–1870. doi:10.1007/s00268-017-3909-7
46. Chang PH, Wang CH, Chen EY, et al. Glasgow prognostic score after concurrent chemoradiotherapy is a prognostic factor in advanced head and neck cancer. Chin J Cancer Res. 2017;29(3):172–178. doi:10.21147/j.issn.1000-9604.2017.03.02
47. Chang PH, Yeh KY, Wang CH, et al. Impact of the pretreatment glasgow prognostic score on treatment tolerance, toxicities, and survival in patients with advanced head and neck cancer undergoing concurrent chemoradiotherapy. Head Neck. 2017;39(10):1990–1996. doi:10.1002/hed.24853
48. He L, Li H, Cai J, et al. Prognostic value of the glasgow prognostic score or modified glasgow prognostic score for patients with colorectal cancer receiving various treatments: a systematic review and meta-analysis. Cell Physiol Biochem. 2018;51(3):1237–1249. doi:10.1159/000495500
49. Jin J, Hu K, Zhou Y, Li W. Prognostic value of the glasgow prognostic score in lung cancer: evidence from 10 studies. Int J Biol Markers. 2018;33(2):201–207. doi:10.5301/ijbm.5000308
50. Lindenmann J, Fink-Neuboeck N, Avian A, et al. Preoperative glasgow prognostic score as additional independent prognostic parameter for patients with esophageal cancer after curative esophagectomy. Eur J Surg Oncol. 2017;43(2):445–453. doi:10.1016/j.ejso.2016.10.015
51. Liu Y, He X, Pan J, Chen S, Wang L. Prognostic role of glasgow prognostic score in patients with colorectal cancer: evidence from population studies. Sci Rep. 2017;7(1):6144. doi:10.1038/s41598-017-06577-2
52. Okano N, Kasuga A, Kawai K, et al. The modified glasgow prognostic score in patients with gemcitabine-refractory biliary tract cancer. Anticancer Res. 2018;38(3):1755–1761. doi:10.21873/anticanres.12412
53. Okuno T, Wakabayashi M, Kato K, et al. Esophageal stenosis and the glasgow prognostic score as independent factors of poor prognosis for patients with locally advanced unresectable esophageal cancer treated with chemoradiotherapy (exploratory analysis of JCOG0303). Int J Clin Oncol. 2017;22(6):1042–1049. doi:10.1007/s10147-017-1154-6
54. Pan QX, Su ZJ, Zhang JH, Wang CR, Ke SY. Glasgow prognostic score predicts prognosis of intrahepatic cholangiocarcinoma. Mol clin oncol. 2017;6(4):566–574. doi:10.3892/mco.2017.1166
55. Petrelli F, Barni S, Coinu A, et al. The modified glasgow prognostic score and survival in colorectal cancer: a pooled analysis of the literature. Rev Recent Clin Trials. 2015;10(2):135–141. doi:10.2174/1574887110666150317121413
56. Saijo M, Nakamura K, Masuyama H, et al. Glasgow prognostic score is a prognosis predictor for patients with endometrial cancer. Eur J Obstet Gynecol Reprod Biol. 2017;210:355–359. doi:10.1016/j.ejogrb.2017.01.024
57. Topkan E, Selek U, Ozdemir Y, et al. Prognostic value of the glasgow prognostic score for glioblastoma multiforme patients treated with radiotherapy and temozolomide. J Neurooncol. 2018;139(2):411–419. doi:10.1007/s11060-018-2879-4
58. Walsh SM, Casey S, Kennedy R, Ravi N, Reynolds JV. Does the modified Glasgow Prognostic Score (mGPS) have a prognostic role in esophageal cancer? J Surg Oncol. 2016;113(7):732–737. doi:10.1002/jso.v113.7
59. Xiao Y, Ren YK, Cheng HJ, Wang L, Luo SX. Modified glasgow prognostic score is an independent prognostic factor in patients with cervical cancer undergoing chemoradiotherapy. Int J Clin Exp Pathol. 2015;8(5):5273–5281.
60. Yamada S, Fujii T, Yabusaki N, et al. Clinical implication of inflammation-based prognostic score in pancreatic cancer: glasgow prognostic score is the most reliable parameter. Medicine. 2016;95(18):e3582. doi:10.1097/MD.0000000000003582
61. Zhou ZH, Ji CD, Zhu J, et al. The prognostic value and pathobiological significance of glasgow microenvironment score in gastric cancer. J Cancer Res Clin Oncol. 2017;143(5):883–894. doi:10.1007/s00432-017-2346-1
62. Zhu J, Wang H, Liu CC, Lu Y, Tang H. The Glasgow Prognostic Score (GPS) is a novel prognostic indicator in advanced epithelial ovarian cancer: a multicenter retrospective study. J Cancer Res Clin Oncol. 2016;142(11):2339–2345. doi:10.1007/s00432-016-2228-y
63. Konigsbrugge O, Posch F, Riedl J, et al. Association between decreased serum albumin with risk of venous thromboembolism and mortality in cancer patients. Oncologist. 2016;21(2):252–257. doi:10.1634/theoncologist.2015-0284
64. Akamine T, Takada K, Toyokawa G, et al. Association of preoperative serum CRP with PD-L1 expression in 508 patients with non-small cell lung cancer: a comprehensive analysis of systemic inflammatory markers. Surg Oncol. 2018;27(1):88–94. doi:10.1016/j.suronc.2018.01.002
65. Li N, Yu Z, Zhang X, et al. Elevated mean platelet volume predicts poor prognosis in colorectal cancer. Sci Rep. 2017;7(1):10261. doi:10.1038/s41598-017-11053-y
66. Chen Y, Jin M, Shao Y, Xu G. Prognostic value of the systemic inflammation response index in patients with adenocarcinoma of the oesophagogastric junction: a propensity score-matched analysis. Dis Markers. 2019;2019:4659048. doi:10.1155/2019/4659048
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



