Back to Journals » Cancer Management and Research » Volume 13
Prognostic Value of Combined CA19-9 with Aspartate Aminotransferase to Lymphocyte Ratio in Patients with Intrahepatic Cholangiocarcinoma After Hepatectomy
Authors Qiu H, Liu C, Huang M, Shen S , Wang W
Received 15 May 2021
Accepted for publication 16 July 2021
Published 3 August 2021 Volume 2021:13 Pages 5969—5980
DOI https://doi.org/10.2147/CMAR.S320380
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sanjeev K. Srivastava
Haizhou Qiu, Chang Liu, Min Huang, Shu Shen, Wentao Wang
Department of Liver Surgery and Liver Transplantation, West China Hospital, Sichuan University, Chengdu, 610041, Sichuan Province, People’s Republic of China
Correspondence: Wentao Wang
Department of Liver Surgery and Liver Transplantation, West China Hospital, Sichuan University, Chengdu, 610041, Sichuan Province, People’s Republic of China
Email [email protected]
Purpose: The prognosis of intrahepatic cholangiocarcinoma (ICC) patients after surgical resection remains poor. Effective prognostic biomarkers are expected to stratify ICC patients and optimize their treatment strategies. To investigate the prognostic value of carbohydrate antigen 19-9 (CA19-9), aspartate aminotransferase to lymphocyte ratio index (ALRI), and their combination (CAC) in predicting long-term outcomes in ICC patients after hepatectomy.
Patients and Methods: ICC patients underwent initial hepatectomy for curative purpose from January 2009 to September 2017 were reviewed retrospectively. Area under the receiver operating characteristics curve (AUC) was used to distinguish the identification effectiveness of three different measures. Kaplan–Meier curves and Cox proportional hazards regression were used to assess the value of preoperative CAC grade in predicting overall survival (OS) and disease-free survival (DFS).
Results: A total of 530 patients were included and randomly divided into two groups (derivation cohort and validation cohort). During a median follow-up of 18 months (1– 115.4 months), 317 patients (59.8%) died and 381 patients (71.9%) developed tumor recurrence. Lower ALRI, decreased serum CA19-9 level and CAC grade were found to be associated with better OS and DFS (both P< 0.001). Importantly, the AUC for CAC grade was significantly greater than ALRI and CA19-9. In addition, results from Cox proportional hazards regression from both cohorts suggest that tumor number, node invasion, and CAC grade as independent prognostic factors for both OS and DFS.
Conclusion: This study demonstrated that CAC grade is a valuable biomarker for the prognosis of ICC patients. Specifically, patients with elevated CAC grades were correlated to worse long-term outcome after the hepatectomy. Our data suggest that increased CAC grades can be used to stratify patients and help to decide their treatment strategies.
Keywords: intrahepatic cholangiocarcinoma, carbohydrate antigen 19-9, aspartate aminotransferase to lymphocyte ratio, hepatectomy, prognostic predictor, long-term outcomes
Introduction
Intrahepatic cholangiocarcinoma (ICC) arises from the epithelium of the intrahepatic and extrahepatic bile ducts. The morbidity of ICC has been steadily increasing in recent years.1,2 The risk factors for development of ICC include chronic hepatitis and cirrhosis, biliary inflammatory diseases, hepatobiliary flukes, and other unknown factors.3 ICC is highly aggressive with a 5-year survival rate less than 20%.4 Among all treatments, surgery remains the main option for the patients with early stage tumor.5 Recently, adjuvant chemotherapy has been found to provide significant benefit for patients with more aggressive tumors. Systemic, locoregional, and targeted therapies are potential choices for patients with unresectable or metastatic disease. However, even after hepatectomy, the 5-year survival rate is only 20–40%,6–8 mainly due to tumor recurrence and metastasis.5 Besides, preoperative biopsy is usually avoided and imaging examination could not find occult metastasis, which bring many challenges to the diagnosis and treatment.9 Meanwhile, there are limited options regarding systemic treatment for ICC, with combination chemotherapy regimens achieving limited responses so far.1,9 Recent randomized controlled trials found conflicting results regarding the benefit of adjuvant chemotherapy.10 Although novel treatment targets have been identified in iCCA patients, including fibroblast growth factor receptor (FGFR) aberrations,11 there are still some obstacles to get over to adapt to clinical treatment. Thus, identifying novel prognostic biomarkers is of great significance in predicting the survival of ICC patients, in order to provide timely and effective treatment options and to improve patient outcome.
Previous studies suggest that inflammation is significant in hepatic pathological changes,12,13 and defective immunity is involved in the development of ICC.14 Various inflammation-based prognostic biomarkers such as the platelet-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio are reliable and sensitive biochemical biomarkers of poor prognosis of many cancers. In clinical practice, doctors usually use aspartate aminotransferase (AST), a liver enzyme, as a routine biochemical test for the diagnosis of various diseases including HCC and ICC.15 As we learned from previous studies, AST is a reliable and sensitive biochemical indicator of liver injury.16 Higher AST levels are associated with higher hepatitis B virus (HBV) influx, which is associated with lower overall survival in HCC patients. Many studies have demonstrated the correlation between high serum AST level and liver cancer mortality. Recently, ALRI was identified as an accurate prognostic indicator for patients with HCC after liver resection and transcatheter arterial chemoembolization.17,18
CA19-9 is the most commonly used and effective serum tumor biomarker for the diagnosis of biliary tract tumors and pancreatic malignant tumors.19 CA19-9 is usually synthesized by normal human pancreatic and bile duct cells, and epithelial cells of the stomach, colon, endometrium, and saliva. There is a small amount of CA19-9 in serum and it is overexpressed in several benign gastrointestinal diseases. Importantly, the plasma level of CA19-9 is significantly increased in neoplastic diseases.20
However, there were few reports that correlate these biomarkers and examine whether the combination of them would be more useful in the context of ICC prognosis. Thus, the aim of this study is to explore the prognostic significance of combining CA19-9 with ALRI in ICC patients with radical resection.
Materials and Methods
Study Population
This study was approved by the Ethics Committee of the West China Hospital, in accordance with the guidelines of the 1975 Declaration of Helsinki. The approval number of the Institutional Review Board (IRB) was No. 2019–22. All consecutive patients undergoing initial curative hepatic resection for ICC from January 2009 to September 2017 were considered for this retrospective study. Written informed consent was obtained from all eligible patients or their relatives. Patients were randomly divided into two groups (derivation group and validation group). The inclusion criteria were: patients getting initial curative hepatic resection for ICC which was confirmed by preoperative imaging and post-operative pathology in our center, older than 18 years old, without other systemic diseases such as diabetes, hypertension, no previous medical history of other malignant tumor of liver or liver surgery. The exclusion criteria were: patients receiving radio-frequency ablation, preoperative transcatheter arterial chemoembolization, chemotherapy, or other anti-cancer treatment before hepatectomy, patients with extrahepatic metastasis, patients who underwent surgical resection for the rupture of tumor, loss to follow-up within 1 month after liver resection, and liver reserve function with a Child–Pugh grade B or C.
Definition and Calculation of CA19-9 and ALRI
Routine blood examination and liver function examination within 1 week before hepatectomy were reviewed and considered in this analysis. ALRI was calculated according to the following formula: AST value (IU/L)/lymphocyte count (109/L). The serum normal values for AST and CA19-9 were 0–40 IU/L and 0–22 U/mL, respectively. Receiver-operating characteristic (ROC) curves were applied to determine the optimal cutoff value as the Youden index attained maximum value. Taking 2 years of OS as an endpoint, the ROC curve showed that Youden index reached the maximum (0.2115) when ALRI was 16.1. CAC grade was divided into three levels from low to high degree. Patients with both low CA19-9 grade (<22) and low ALRI grade (<16.1) were classified as CAC grade 1; those with both high CA19-9 grade and high ALRI grade were classified as CAC grade 3; the rest of the patients were classified as CAC grade 2.
Data Collection and Follow-Up
Diagnoses of ICC was confirmed by postoperative pathology. According to the American Joint Commission on cancer (AJCC) 8th edition staging manual, tumor lymph node metastasis (TNM) staging was used. All clinicopathological data were obtained from electronic or handwritten medical records, including demographic information, laboratory data, and tumor histological characteristics. Among them, microvascular invasion (MVI) was defined as small vessel invasion diagnosed by histology.
The patients were followed up according to the national cancer comprehensive network (NCCN) guidance. In the first year after surgery, physical examination, tumor biomarker examination, or contrast-enhanced CT scan were regularly reviewed every 3 months, and the time interval was then extended to 6 months from the second year. In addition, we followed patients who decided not to return to the hospital for reexamination by phone. Overall survival (OS) is defined as from hepatectomy to death, or in those who are alive, to the date of the last follow-up. Disease-free survival (DFS) was defined as the time from diagnosis to tumor recurrence or death. During a median follow-up of 18 months (1–115.4 months), 317 patients (59.8%) died and 381 patients (71.9%) developed tumor recurrence. Two independent cohorts had comparable follow-up periods.
Statistical Analysis
GraphPad Prism (version 8.0, San Diego, CA), SPSS (version 23.0, Chicago, IL), and MedCalc (version 15.2.2.0, Ostend, Belgium) were used to perform statistical analyses. Receiver-operating characteristic (ROC) curves were applied to determine the optimal cut-off value as Youden index attained maximum value. Area under curves (AUC) were utilized to distinguish different indexes’ performance in predictive accuracy of OS and DFS. The 2-year survival status was set as the discriminant. χ2 test or Fisher’s exact test were used to analyze categorical variables. Kaplan-Meier curves were plotted for derivation and validation cohorts. Cox proportional hazards regression models (enter method) were adopted to identify potential independent prognostic factors for OS and DFS. Statistical significance was defined as P-values less than 0.05.
Results
Correlation Between CAC and Clinicopathological Features
Finally, 530 patients were randomly divided into a derivation group and validation group (265 cases in each group, shown in Figure 1). The demographic and clinicopathological characteristics are shown in Table 1. In the derivation cohort, the CAC grade was divided into three levels, with 35 (13.2%), 100 (37.7%), and 130 (49.1%) patients divided into the CAC grade 1, 2, and 3, respectively. Table 2 summarizes the correlation between CAC grade and clinical features in the derivation cohort. The results showed that preoperative CAC grade was significantly related to tumor size, tumor number, node invasion, and TNM stages. However, there was no significant correlation between CAC and age, gender, HbsAg, hepatolithiasis, white blood count, neutrophils, hemoglobin, GGT levels, differentiation, MVI, perineural invasion, as well as liver cirrhosis. Correlation between CAC grade and clinical characteristics in the validation cohort was summarized in Supplementary Table S1. As shown in this table, the numbers of patients in three different CAC levels were 29 (10.9%), 97 (36.6%), and 139 (52.5%). Except for the same association between the CAC grade and different indexes in the derivation cohort, it was observed that MVI was linked with the CAC grade (P=0.008).
 |
Table 1 Baseline Characteristics of 530 ICC Patients Who Underwent Hepatectomy |
 |
Table 2 Correlation Between CAC Grade and Clinicopathological Characteristics in the Derivation Cohort |
 |
Figure 1 The flow-chart of patient selection. |
Survival Analysis of Prognostic Variables in ICC Patients
A Kaplan-Meier analysis was performed to detect the correlation between ALRI, CA19-9, and CAC grade with OS and DFS. Elevated ALRI, CA19-9, and CAC were significantly correlated to worse OS and DFS (Figure 2). A similar trend was also detected in the validation cohort (Figure 3). In the univariate Cox regression analysis of the derivation cohort, 10 of 19 clinicopathological indexes were identified as potential factors affecting OS. Tumor number, differentiation, node invasion, and CAC grade were characterized as independent risk factors for OS in a multivariate Cox regression model (Table 3). Tumor number, differentiation, perineural invasion as well as CAC grade were identified are independent risk factors for DFS (Table 4). Seven and nine of the 19 characteristics were potential factors influencing OS and DFS in the validation cohort, respectively. Tumor number, node invasion, and CAC grade were independent risk factors for both OS and DFS (Supplementary Table S2 and S3). AUC was plotted to exhibit the difference of predictive value between ALRI, CA19-9, and CAC grade. It was shown that CAC grade had the highest value of AUC (Figure 4), indicating that CAC grade, compared with the other two indicators, is a better biomarker in predicting OS and DFS. In addition, despite the specificity, CAC grade got the highest value in sensitivity and accuracy compared with the two other independent risk factors, showing that CAC grade might be a better choice to predict OS and DFS (Supplementary Table S4).
 |
Table 3 Cox Regression Analysis for OS of ICC Patients in the Derivation Cohort |
 |
Table 4 Cox Regression Analysis for DFS of ICC Patients in the Derivation Cohort |
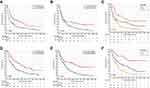 |
Figure 2 Kaplan-Meier curves for DFS and OS stratified by ALRI (A and D), CA19-9 (B and E), and CAC grade (C and F) in the derivation cohort. |
 |
Figure 3 Kaplan-Meier curves for DFS and OS stratified by ALRI (A and D), CA19-9 (B and E), and CAC grade (C and F) in the validation cohort. |
 |
Figure 4 Comparison of AUCs of ALRI, CA19-9 and CAC grade in predicting OS (A) and DFS (B) in the derivation cohort. |
Discussion
Tumor recurrence or metastasis is the major factor that determines the prognosis of ICC after hepatectomy.5 Great efforts have been made to identify effective biomarkers for predicting the prognosis. Despite limited success, ICC prognosis still largely depends on routine pathology in the clinic. In this study, we examined whether CAC grade could be a reliable biomarker for ICC prognosis. To our best knowledge, this is the first large population study to assess the prognostic significance of CAC grade in ICC patients after hepatectomy.
Ample evidence has suggested that inflammation not only acts as one result of tumor formation, but also plays a central role in promoting tumor occurrence and development.21 In the systemic inflammatory response, lymphocytes along with other components of leukocytes play an important role.22–25 CD8+ cytotoxic T-cells lead to tumor elimination, while regulatory T cells inhibit immune responses.25 Overall, lymphocytes acted as a tumor suppressor by promoting cytotoxic tumor cell death.26 Numerous studies have demonstrated that tumor infiltrating lymphocytes (TILs) are important in the tumor microenvironment and they can be used as prognostic markers for a variety of tumors.23 Usually, the greater number of TILs in patients are correlated with better prognosis and lower recurrence rate.27 AST, a key enzyme in the amino acid metabolism pathway, is a reliable and sensitive biomarker of liver injury. The progress of liver diseases may be related to mitochondrial damage, which leads to the release of AST into the cytoplasm of hepatocytes.28 Consequently, AST usually increases during tumor progression.
ALRI can reflect the damage of hepatocytes as well as the tumor burden and disease development.29 Preoperative ALRI can predict the low survival rate of liver cancer and it is negatively correlated with OS and DFS.30,31 However, ALRI has not been well studied in ICC. CA19-9, a tetrasaccharide carbohydrate called sialic Lewis A,32 is the most commonly used biomarker in the management of pancreatic cancer and ICC, but CA19-9 is also significantly increased in benign cholangiocarcinoma.33,34 Tracing levels of CA19-9 were found in salivary glands, prostate, pancreas, breast, stomach, bile duct, gallbladder, and bronchial epithelial cells of healthy adults.35 Although CA19-9 is low sensitive for early stage disease which limits its use for diagnosis, some studies have noted that higher preoperative CA19-9 values were associated with worse recurrence-free survival after surgical resection.36 Non-normalization of CA19-9 level after curative resection of biliary tract cancer was found to be associated with worse OS.37 Meanwhile, the combination of carcinoembryonic antigen (CEA) and CA 19-9 has an accuracy of 86% in diagnosing cholangiocarcinoma.38 Some investigators also found significantly higher CA19-9 levels in patients with unresectable cholangiocarcinomas.39
Previous studies have found that immunocytes deliver the specific recognition molecules of cell surface glycans, such as sialic acid binding Ig-like lectins (siglecs).32 Cell surface polysaccharides also changed significantly in the process of malignant transformation, although the exact mechanism remains to be fully elucidated.40–43 When the immune homeostasis of the mucosa is destroyed, impaired glycosylation can enhance the production of inflammatory molecules.44 A hypoxic microenvironment during tumor progression increases the transcription of glycosylation gene, including CA19-9.45 Thus, we hypothesized that the state of systemic immune response may be better represented by a combination of biomarkers.
Our study demonstrated that a high preoperative CAC grade was an independent risk factor of OS and DFS in ICC patients who underwent surgery. It is worth noting that inflammation and immune response might change after tumor resection, which may lead to a different prognosis.
Among all treatments, hepatectomy remains the main option for the ICC patients, but its resectability and curability remain low.46 Previous studies have shown that the prognosis of surgery could be evaluated by some biochemical indexes, for example, albumin and total bilirubin levels can be used to predict the risk of postoperative hepatic failure, and preoperative serum albumin <3 g/dL and bilirubin >10 mg/dL often indicate poor prognosis of ICC patients.47 Similarly, the CAC grade could be calculated from the results of blood examination, which are available and convenient for clinical workers to take optimal therapeutic regime targeting different patients. For patients with unresectable ICC, radiation therapy and chemotherapy would be adopted.1 However, the value of biomarkers’ changes in the process of these treatments need to be further studied.
Furthermore, genomic studies have paved the way towards the identification of a large number of targets, and the most promising therapeutic options for ICC originate from targeted therapies.48,49 In the current landscape of medical oncology, the identification of specific biomarkers which could have prognostic value represents one of the critical challenges.49 Owing to the accessibility of CAC grade, more studies could be taken to find out the value of tumor markers and biochemical indexes predictive of response to ICC patients getting systemic therapies.
Several limitations did exist in this study. First, this was a single institution retrospective study limited to an Asian population with a small sample size. Large-scale, multicenter prospective studies should be conducted to test and validate our results. Second, our report did not provide certain clinicopathological characteristics, such as portal hypertension and cavernous transformation of the portal vein. Moreover, other tumor biomarkers, such as CEA and bilirubin levels, were not evaluated. In addition, due to ward bed shortage, we were not able to perform surgery timely to all ICC patients with surgical indications, so the referral bias could exist. Finally, the guidance of the biomarkers to clinical immunotherapy still needs to be explored, and subgroup-analysis should be taken to clarify.
In conclusion, this study analyzed the serum inflammatory index and tumor biomarkers in patients with ICC underwent radical resection and demonstrated the value of preoperative CAC grade as a prognostic factor. Patients with elevated CAC levels were associated with worse long-term survival outcomes. CAC grade is an independent risk factor for OS and DFS in patients with ICC after hepatectomy. In the future, CAC could help to stratify patients with ICC and guide treatment strategies.
Author Contributions
Qiu H, Liu C and Huang M contributed equally to this work and should be considered as co-first author. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published, have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Supported by the Science and Technology Program of Sichuan Science and Technology Department (No. 2019YFS0029, 2019YFS0529), the National Natural Science Foundation of China (No. 81770566, 82000599), and the New Medical Technology Foundation of West China Hospital of Sichuan University (No. XJS2016004).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Rizvi S, Khan SA, Hallemeier CL, Kelley RK, Gores GJ. Cholangiocarcinoma - evolving concepts and therapeutic strategies. Nat Rev Clin Oncol. 2018;15:95–111. doi:10.1038/nrclinonc.2017.157
2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi:10.3322/caac.21492
3. Shaib YH, El-Serag HB, Nooka AK, et al. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma: a hospital-based case-control study. Am J Gastroenterol. 2007;102:1016–1021. doi:10.1111/j.1572-0241.2007.01104.x
4. Blechacz B, Komuta M, Roskams T, Gores GJ. Clinical diagnosis and staging of cholangiocarcinoma. Nat Rev Gastroenterol Hepatol. 2011;8:512–522. doi:10.1038/nrgastro.2011.131
5. Bridgewater J, Galle PR, Khan SA, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60:1268–1289.
6. Jutric Z, Johnston WC, Hoen HM, et al. Impact of lymph node status in patients with intrahepatic cholangiocarcinoma treated by major hepatectomy: a review of the national cancer database. HPB (Oxford). 2016;18:79–87. doi:10.1016/j.hpb.2015.07.006
7. Weber SM, Ribero D, O’Reilly EM, Kokudo N, Miyazaki M, Pawlik TM. Intrahepatic cholangiocarcinoma: expert consensus statement. HPB (Oxford). 2015;17:669–680. doi:10.1111/hpb.12441
8. Spolverato G, Kim Y, Alexandrescu S, et al. Management and outcomes of patients with recurrent intrahepatic cholangiocarcinoma following previous curative-intent surgical resection. Ann Surg Oncol. 2016;23:235–243. doi:10.1245/s10434-015-4642-9
9. Cillo U, Fondevila C, Donadon M, et al. Surgery for cholangiocarcinoma. Liver Int. 2019;39(Suppl 1):143–155. doi:10.1111/liv.14089
10. Rizzo A, Ricci AD, Brandi G. Recent advances of immunotherapy for biliary tract cancer. Expert Rev Gastroenterol Hepatol. 2021;15:527–536. doi:10.1080/17474124.2021.1853527
11. Rizzo A, Ricci AD, Brandi G. Futibatinib, an investigational agent for the treatment of intrahepatic cholangiocarcinoma: evidence to date and future perspectives. Expert Opin Investig Drugs. 2021;30:317–324. doi:10.1080/13543784.2021.1837774
12. Ringelhan M, Pfister D, O’Connor T, Pikarsky E, Heikenwalder M. The immunology of hepatocellular carcinoma. Nat Immunol. 2018;19:222–232. doi:10.1038/s41590-018-0044-z
13. Yang YM, Kim SY, Seki E. Inflammation and liver cancer: molecular mechanisms and therapeutic targets. Semin Liver Dis. 2019;39:26–42. doi:10.1055/s-0038-1676806
14. Shankaran V, Ikeda H, Bruce AT, et al. IFNgamma and lymphocytes prevent primary tumour development and shape tumour immunogenicity. Nature. 2001;410:1107–1111. doi:10.1038/35074122
15. Zhang GM, Xia YJ, Guo XX, et al. Reference intervals for total bilirubin, ALT, AST and creatinine in healthy Chinese elderly. Med Sci Monit. 2014;20:1778–1782. doi:10.12659/MSM.892148
16. van Beek JH, de Moor MH, de Geus EJ, et al. The genetic architecture of liver enzyme levels: GGT, ALT and AST. Behav Genet. 2013;43:329–339. doi:10.1007/s10519-013-9593-y
17. Jin J, Zhu P, Liao Y, Li J, Liao W, He S. Elevated preoperative aspartate aminotransferase to lymphocyte ratio index as an independent prognostic factor for patients with hepatocellular carcinoma after hepatic resection. Oncotarget. 2015;6(22):19217–19227. doi:10.18632/oncotarget.4265
18. Yang Z, Zhang J, Lu Y, et al. Aspartate aminotransferase-lymphocyte ratio index and systemic immune-inflammation index predict overall survival in HBV-related hepatocellular carcinoma patients after transcatheter arterial chemoembolization. Oncotarget. 2015;6(40):43090–43098. doi:10.18632/oncotarget.5719
19. Paganuzzi M, Onetto M, Marroni P, et al. CA 19-9 and CA 50 in benign and malignant pancreatic and biliary diseases. Cancer. 1988;61(10):2100–2108. doi:10.1002/1097-0142(19880515)61:10<2100::AID-CNCR2820611028>3.0.CO;2-Z
20. Koprowski H, Steplewski Z, Mitchell K, Herlyn M, Herlyn D, Fuhrer P. Colorectal carcinoma antigens detected by hybridoma antibodies. Somatic Cell Genet. 1979;5:957–971. doi:10.1007/BF01542654
21. Fest J, Ruiter R, Mulder M, et al. The systemic immune-inflammation index is associated with an increased risk of incident cancer-A population-based cohort study. Int J Cancer. 2020;146:692–698. doi:10.1002/ijc.32303
22. Chen JH, Zhai ET, Yuan YJ, et al. Systemic immune-inflammation index for predicting prognosis of colorectal cancer. World J Gastroenterol. 2017;23:6261–6272. doi:10.3748/wjg.v23.i34.6261
23. Li H, Wang J, Liu H, et al. Existence of intratumoral tertiary lymphoid structures is associated with immune cells infiltration and predicts better prognosis in early-stage hepatocellular carcinoma. Aging. 2020;12:3451–3472. doi:10.18632/aging.102821
24. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–867. doi:10.1038/nature01322
25. Quail DF, Joyce JA. Microenvironmental regulation of tumor progression and metastasis. Nat Med. 2013;19:1423–1437. doi:10.1038/nm.3394
26. Moses K, Brandau S. Human neutrophils: their role in cancer and relation to myeloid-derived suppressor cells. Semin Immunol. 2016;28:187–196. doi:10.1016/j.smim.2016.03.018
27. Webb JR, Milne K, Kroeger DR, Nelson BH. PD-L1 expression is associated with tumor-infiltrating T cells and favorable prognosis in high-grade serous ovarian cancer. Gynecol Oncol. 2016;141:293–302. doi:10.1016/j.ygyno.2016.03.008
28. Okuda M, Li K, Beard MR, et al. Mitochondrial injury, oxidative stress, and antioxidant gene expression are induced by hepatitis C virus core protein. Gastroenterology. 2002;122:366–375. doi:10.1053/gast.2002.30983
29. Casadei GA, Foschi FG, Conti F, et al. Immune inflammation indicators and ALBI score to predict liver cancer in HCV-patients treated with direct-acting antivirals. Dig Liver Dis. 2019;51:681–688. doi:10.1016/j.dld.2018.09.016
30. He C, Peng W, Li C, Wen TF. Postoperative aspartate aminotransferase to lymphocyte ratio index change is an independent predictor of survival in patients with small hepatocellular carcinoma. Medicine. 2017;96:e8540. doi:10.1097/MD.0000000000008540
31. Zhao LY, Yang DD, Ma XK, et al. The prognostic value of aspartate aminotransferase to lymphocyte ratio and systemic immune-inflammation index for overall survival of hepatocellular carcinoma patients treated with palliative treatments. J Cancer. 2019;10:2299–2311. doi:10.7150/jca.30663
32. Scarà S, Bottoni P, Scatena R. CA 19-9: biochemical and Clinical Aspects. Adv Exp Med Biol. 2015;867:247–260.
33. Duffy MJ, Sturgeon C, Lamerz R, et al. Tumor markers in pancreatic cancer: a European group on tumor markers (EGTM) status report. Ann Oncol. 2010;21:441–447. doi:10.1093/annonc/mdp332
34. Moro A, Mehta R, Sahara K, et al. The impact of Preoperative CA19-9 and CEA on outcomes of patients with intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2020;27:2888–2901. doi:10.1245/s10434-020-08350-8
35. Jalanko H, Kuusela P, Roberts P, Sipponen P, Haglund CA, Mäkelä O. Comparison of a new tumour marker, CA 19-9, with alpha-fetoprotein and carcinoembryonic antigen in patients with upper gastrointestinal diseases. J Clin Pathol. 1984;37:218–222. doi:10.1136/jcp.37.2.218
36. Tamandl D, Herberger B, Gruenberger B, Puhalla H, Klinger M, Gruenberger T. Influence of hepatic resection margin on recurrence and survival in intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2008;15:2787–2794. doi:10.1245/s10434-008-0081-1
37. Yamashita S, Passot G, Aloia TA, et al. Prognostic value of carbohydrate antigen 19-9 in patients undergoing resection of biliary tract cancer. Br J Surg. 2017;104:267–277. doi:10.1002/bjs.10415
38. Chalasani N, Baluyut A, Ismail A, et al. Cholangiocarcinoma in patients with primary sclerosing cholangitis: a multicenter case-control study. Hepatology. 2000;31:7–11. doi:10.1002/hep.510310103
39. Patel AH, Harnois DM, Klee GG, LaRusso NF, Gores GJ. The utility of CA 19-9 in the diagnoses of cholangiocarcinoma in patients without primary sclerosing cholangitis. Am J Gastroenterol. 2000;95:204–207. doi:10.1111/j.1572-0241.2000.01685.x
40. Kannagi R. Regulatory roles of carbohydrate ligands for selectins in the homing of lymphocytes. Curr Opin Struct Biol. 2002;12:599–608. doi:10.1016/S0959-440X(02)00365-2
41. Liu FT, Rabinovich GA. Galectins: regulators of acute and chronic inflammation. Ann N Y Acad Sci. 2010;1183:158–182. doi:10.1111/j.1749-6632.2009.05131.x
42. Crocker PR, Paulson JC, Varki A. Siglecs and their roles in the immune system. Nat Rev Immunol. 2007;7:255–266. doi:10.1038/nri2056
43. Crocker PR, Redelinghuys P. Siglecs as positive and negative regulators of the immune system. Biochem Soc Trans. 2008;36:1467–1471. doi:10.1042/BST0361467
44. Miyazaki K, Sakuma K, Kawamura YI, et al. Colonic epithelial cells express specific ligands for mucosal macrophage immunosuppressive receptors siglec-7 and −9. J Immunol. 2012;188:4690–4700. doi:10.4049/jimmunol.1100605
45. Galli C, Basso D, Plebani M. CA 19-9: handle with care. Clin Chem Lab Med. 2013;51:1369–1383. doi:10.1515/cclm-2012-0744
46. Wang K, Zhang H, Xia Y, Liu J, Shen F. Surgical options for intrahepatic cholangiocarcinoma. Hepatobiliary Surg Nutr. 2017;6:79–90. doi:10.21037/hbsn.2017.01.06
47. Mosconi S, Beretta GD, Labianca R, Zampino MG, Gatta G, Heinemann V. Cholangiocarcinoma. Crit Rev Oncol Hematol. 2009;69:259–270. doi:10.1016/j.critrevonc.2008.09.008
48. Morizane C, Ueno M, Ikeda M, Okusaka T, Ishii H, Furuse J. New developments in systemic therapy for advanced biliary tract cancer. Jpn J Clin Oncol. 2018;48:703–711. doi:10.1093/jjco/hyy082
49. Rizzo A, Tavolari S, Ricci AD, et al. Molecular features and targeted therapies in extrahepatic cholangiocarcinoma: promises and failures. Cancers. 2020;12:3256. doi:10.3390/cancers12113256
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
