Back to Journals » OncoTargets and Therapy » Volume 10
Prognostic value and clinicopathological significance of proliferating cell nuclear antigen expression in gastric cancer: a systematic review and meta-analysis
Authors Yin SC, Li Z, Huang JY, Miao ZF, Zhang JY, Lu CY, Xu H, Xu HM
Received 3 November 2016
Accepted for publication 15 November 2016
Published 10 January 2017 Volume 2017:10 Pages 319—327
DOI https://doi.org/10.2147/OTT.S126551
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr XuYu Yang
Songcheng Yin,1,* Zhan Li,2,* Jinyu Huang,1 Zhifeng Miao,1 Junyan Zhang,1 Chunyang Lu,1 Hao Xu,1 Huimian Xu1
1Department of Surgical Oncology, 2Department of Breast Surgery, First Affiliated Hospital of China Medical University, Shenyang, People’s Republic of China
*These authors contributed equally to this work
Background: The prognostic significance of proliferating cell nuclear antigen (PCNA) expression in gastric cancer has long been assessed, yet results remain controversial. Therefore, we performed a meta-analysis to assess the prognostic value and clinicopathological significance of PCNA in gastric cancer.
Methods: A systematic literature search of PubMed, EMBASE, and the Cochrane Library databases was conducted. Summary odds ratios (ORs) and hazard ratios (HRs) with 95% confidence intervals (CIs) were calculated to investigate the correlations between PCNA expression and clinicopathological features, overall survival (OS), and disease-free survival (DFS).
Results: A total of 19 studies involving 2,852 participants were included in our analysis. The pooled HR indicated that high PCNA expression was significantly associated with poor OS (HR 1.66, 95% CI 1.32–2.08) and DFS (HR 1.81, 95% CI 1.40–2.36). Subgroup analysis revealed that the association between PCNA and OS was also significant in Asian and European patients. In addition, the pooled ORs showed that high PCNA expression was significantly associated with deeper tumor invasion (OR 2.37, 95% CI 1.71–3.27), lymph node metastasis (OR 2.49, 95% CI 1.85–3.35), and advanced stage cancer (OR 1.89, 95% CI 1.36–2.63).
Conclusion: Our meta-analysis indicates that high PCNA expression might be a prognosticator of poor survival and a promising therapeutic target for gastric cancer patients.
Keywords: proliferating cell nuclear antigen, gastric cancer, prognosis, biomarker, meta-analysis
Introduction
Gastric cancer is the fifth most common malignancy and the third leading cause of mortality worldwide. According to GLOBOCAN statistics, 951,000 new gastric cancer cases and 723,000 deaths from gastric cancer occurred globally in 2012.1 Although comprehensive treatment is available, including adequate surgical resection supplemented by neoadjuvant treatments, the 5-year survival rate of gastric cancer remains <35%.2,3 Patients with the same clinical stage can have different prognoses, indicating that the clinical stage does not completely reflect the biological behavior of the tumor. Therefore, the identification of molecular biomarkers is warranted to improve clinical staging schemes and predict prognosis.4 Prognostic biomarkers such as E-cadherin, STAT3, CD133, p53, MMP7, and lactate dehydrogenase have been explored in published articles.5–10 However, there is still a heated discussion on discovering a new biomarker to predict patient prognosis and to provide novel therapeutic targets for gastric cancer patients.
Proliferating cell nuclear antigen (PCNA) was originally discovered in 1978 by Miyachi et al11 as the antigen to an autoimmune antibody in the sera of patients with systemic lupus erythematosus.12 It was initially considered to be expressed during cell proliferation, with peak expression occurring during late G1 and S phases.13,14 However, in recent decades, PCNA has been shown to act as a molecular platform that coordinates a wide range of processes involved in genome maintenance, duplication, transmission, and cell-cycle regulation.15,16 Because cell proliferation is a requirement for tumor progression, and owing to the indispensable function of PCNA in cell proliferation, much attention has been paid to the role of PCNA in tumors.17 Indeed, PCNA was found to be involved in the prognosis of cancer patients, including those with nasopharyngeal carcinoma, lung cancer, prostate carcinoma, and gastric carcinoma.18–21
A recent meta-analysis demonstrated that high PCNA expression was significantly associated with higher mortality, suggesting that it could be a useful prognostic biomarker in gliomas and cervical cancer.22 However, controversy remains in gastric cancer about the impact of PCNA on patient survival and clinicopathological characteristics. Numerous publications have demonstrated that PCNA overexpression was associated with poor prognosis in gastric cancer patients,23–25 while some studies hold different views.26,27 To investigate this further, we conducted a meta-analysis to evaluate the association between PCNA expression and overall survival (OS), disease-free survival (DFS), and clinicopathological characteristics in gastric cancer.
Materials and methods
Search strategy and selection criteria
A comprehensive literature search of PubMed, EMBASE, and Cochrane Library databases was conducted with the MeSH terms and the following key words variably combined: “stomach”, “gastric”, “neoplasm”, “cancer”, “carcinoma”, “tumor”, “proliferating cell nuclear antigen”, and “PCNA”. The search was completed on May 20, 2016. Reference entries of eligible literature were scanned to minimize any deviation caused during the research process. This study is a meta-analysis, did not involve subjects, and was based on previous published articles; therefore, ethical approval was not required.
The inclusion criteria of studies in this meta-analysis were as follows: 1) patients diagnosed with gastric cancer by pathologists; 2) PCNA expression detected in primary tumor tissues; 3) an association between PCNA expression and parameters such as OS, DFS, or clinicopathological characteristics; 4) sufficient information to extract hazard ratios (HRs), odds ratios (ORs), and their 95% confidence intervals (CIs); and 5) full text, original research articles published in English. Reports of conferences and reviews were excluded. Only the most complete study was selected if duplicate data from other articles occurred. Two investigators (SY and ZL) independently screened all studies and identified those that were eligible for inclusion. Inconsistencies were resolved through negotiation and consultation.
Quality assessment
The methodological quality of the original studies was assessed by the Newcastle–Ottawa Scale (NOS),28 which consisted of three factors: selection, comparability of subjects, and outcome. Each study received a score from 0 to 9 (allocated as stars), and scores higher than 6 were considered high quality. Two authors (SY and JH) independently performed this assessment, and discrepancies were resolved by discussion.
Data extraction
Two researchers (SY and ZL) used a predesigned form to extract the following data independently from qualified studies: authors, country, publication year, number of participants, patient’s age, patient’s gender, cutoff value, percentage of PCNA-positive patients, clinicopathological characteristics of patients (including histological differentiation, clinical stage, T stage, lymphatic invasion, lymph node metastasis, vessel invasion, and Lauren classification), follow-up information, and survival data. Inconsistencies were resolved by consultation with a third author (HX) when the two reviewers could not reach a consensus.
Statistical analysis
HR and its 95% CI were used to evaluate the correlation between PCNA expression and patient survival. If the HR with 95% CI were reported in the original study, we extracted the data directly. If not, we extrapolated HR from survival rates with P-values from log-rank tests or Kaplan–Meier survival curves using the method reported by Parmar et al29 and Tierney et al.30 ORs with 95% CIs were chosen to investigate the association between clinicopathological features and PCNA expression. Clinicopathological features included histological differentiation, clinical stage, T stage, lymphatic invasion, lymph node metastasis, vessel invasion, and Lauren classification. An observed HR or OR >1 implied a worse prognosis in the PCNA-positive group and was considered to be statistically significant if the 95% CI did not overlap 1.
Interstudy heterogeneity was tested by I2 statistics. I2>50% indicated that the studies showed significant heterogeneity, so a random-effects model was employed; otherwise, a fixed-effects model was implemented. Subgroup analysis and meta-regression were conducted to investigate the potential heterogeneity among studies. We also performed sensitivity analysis to evaluate the stability of the results. Potential publication bias was assessed by funnel plots and Egger’s linear regression test.31 STATA statistical software (version 12.0, Stata Corporation, College Station, TX, USA) was used to perform data analyses. All P-values were two-sided and considered significant if <0.05.
Results
Search results
The processes of retrieval strategy for articles are described in Figure 1. A total of 1,049 potential articles were identified for inclusion using the search strategies described in “Materials and methods” section. Through reviewing the title and abstracts, 1,003 papers were excluded. The remaining 46 were systematically evaluated by a full-text review. A further 27 were eliminated for the following reasons: the relationship between PCNA and tumors was not relevant to gastric cancer (n=3), insufficient data about survival or clinicopathological characteristics (n=13), nondichotomous variables of PCNA were excluded (n=7), and data overlapped those used in other studies (n=4). Finally, 19 studies involving a total of 2,852 gastric cancer patients met the requirements of our meta-analysis.21,23–27,32–44
  | Figure 1 Flowchart of the study selection process. |
Study characteristics
The fundamental features of these 19 eligible articles are summarized in Table 1. Overall, 13 studies were conducted in patients from Asia and 6 from Europe. Sample sizes ranged from 32 to 841. All interstudies used the technique of immunohistochemistry (IHC) to detect the expression of PCNA. Ye et al34 reported two independent data sets including familial gastric cancer and sporadic gastric cancer. Fifteen studies reported an association between PCNA expression and clinicopathological characteristics, and 16 articles contained studies investigating the effect of PCNA expression on survival (16 for OS and 3 for DFS).
Impact of PCNA expression on OS and DFS
The correlation between PCNA expression and OS is shown in a forest plot (Figure 2). Increased PCNA expression was shown to be significantly associated with an increased mortality risk by the random-effects model (pooled HR 1.66, 95% CI 1.32–2.08), with significant heterogeneity (I2=63.9%, P<0.001). Meta-regression and subgroup analyses were conducted based on study location, publication year, and cutoff value (Table 2). The source of heterogeneity could not be detected among these factors in meta-regression (all P>0.05). Subgroup analysis using pooled HRs showed that high PCNA expression was significantly associated with poor OS in both Asian (HR 1.69, 95% CI 1.28–2.23) and European (HR 1.52, 95% CI 1.11–2.08) patients. No significant heterogeneity was detected in European countries (I2=28.7%, P=0.240), in studies conducted after 2005 (I2=0%, P=0.655), or with cutoff <50% (I2=25.1%, P=0.254).
  | Table 2 Stratified analysis of PCNA expression with overall survival in gastric cancer patients |
We also examined the impact of PCNA expression on DFS (Figure 3). High expression of PCNA in primary gastric cancer was associated with a poor DFS in the fixed-effects model (pooled HR 1.81, 95% CI 1.40–2.36); moreover, no significant heterogeneity was detected (I2=42.7%, P=0.175).
Effect of PCNA expression on clinicopathological parameters
To further explore the biological role of PCNA, we investigated the correlation between PCNA expression and clinicopathological characteristics. First, we used the fixed-effects model to combine HR with 95% CI; if significant heterogeneity existed (I2>50%) among studies, the random-effects model was used. As illustrated in Table 3, increased PCNA expression was significantly correlated with the depth of invasion (T3/T4 vs T1/T2: OR 2.37, 95% CI 1.71–3.27), lymph node metastasis (positive vs negative: OR 2.49, 95% CI 1.85–3.35), and TNM stage (III–IV vs I–II: OR 1.89, 95% CI 1.36–2.63). No significant heterogeneity was observed (I2=0.0%–37.8%). However, PCNA expression was not associated with vascular invasion (positive vs negative: OR 1.32, 95% CI 0.70–2.48), histological grade (G3/G4 vs G1/G2: OR 1.04, 95% CI 0.72–1.50), or the Lauren classification type (intestinal vs diffuse: OR 1.14, 95% CI 0.70–1.86).
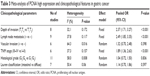  | Table 3 Meta-analysis of PCNA high expression and clinicopathological features in gastric cancer |
Sensitivity analysis
We performed a sensitivity analysis to assess the stability of our results regarding OS, DFS, and clinicopathological characteristics in gastric cancer patients. We compared the fixed-effects and random-effects models, but found no significant difference in OS (fixed-effects model: HR 1.43, 95% CI 1.26–1.62). Furthermore, the plots illustrated that our results were robust because pooled HRs or ORs were not significantly influenced by excluding any single study (Figure 4).
  | Figure 4 Sensitivity analysis of proliferating cell nuclear antigen expression on overall survival. |
Publication bias
Begg’s funnel plot showed an asymmetric distribution, and the P-values from Egger’s tests indicated that there was significant publication bias in OS (P=0.003) and Lauren classification (P=0.024). To evaluate the potential impact of publication bias, a trim-and-fill analysis was performed. The adjusted pooled HR still showed a significant association between PCNA expression and OS (HR 1.51, 95% CI 1.22–1.88), whereas the adjusted pooled OR revealed a similar correlation between PCNA expression and Lauren classification to the above meta-analysis results (OR 1.14, 95% CI 0.70–1.85). After incorporating additional studies, the funnel plots were shown to be symmetrical (Figure 5). This symmetry and the P-values from Egger’s tests indicated that there was no significant publication bias for pooled depth of invasion (P=0.9), lymph node metastasis (P=0.054), TNM stage (P=0.125), histological grade (P=0.268), or vascular invasion (P=0.865).
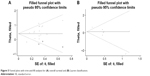  | Figure 5 Funnel plots with trim-and-fill analysis for (A) overall survival and (B) Lauren classification. |
Discussion
PCNA is indispensable for DNA replication and the maintenance of genomic integrity in actively growing cells.45 In replication machinery, the PCNA sliding clamp acts as a central scaffold to control the dynamic engagement of multiple factors at the heart of the replication fork.16 It also forms a docking platform to recruit factors during the DNA damage response and replication surveillance.16 Because of its role in cancer cell proliferation, PCNA has been widely used as a tumor marker. However, data are conflicting regarding the association between PCNA expression in tumor tissues and patient prognosis.17 Previous studies suggested that high PCNA expression is an indicator of poor prognosis in cervical cancer or gliomas.22 However, the equivalent data for patients with gastric cancer have not been reported.
Our meta-analysis of 19 individual studies involving 2,852 patients explored the relationship between PCNA and prognosis, as well as clinicopathological parameters in gastric cancer. The results indicate that high expression of PCNA predicts a poor OS and DFS in gastric cancer patients. Meanwhile, we observed significant heterogeneity among the studies regarding OS. Although the random-effects and fixed-effects models were used to pool data, neither model identified the source of heterogeneity. Meta-regression analysis showed that none of the factors thought to be the source, such as study location, publication year, and cutoff value, had a significant association with heterogeneity (all P>0.05). However, subgroup analysis indicated that heterogeneity was successfully removed in the subgroups of European countries, publication year >2005, and cutoff <50%. In addition, subgroup analysis revealed that high PCNA expression is also significantly associated with poor OS in Asian and European countries. We also evaluated the impact of PCNA expression on clinicopathological features. No significant heterogeneity was observed, so the fixed-effects model was used to show that increased PCNA expression was correlated with deeper tumor invasion, lymph node metastasis, and advanced TNM stage. These findings further verified the association between high PCNA expression and poor OS, which is consistent with our earlier results.
As we know, cancer is caused by multiple mechanisms that often appear error in DNA replication. And tumor progression cannot be separated from the proliferation and metastasis of tumor cells. PCNA is an indispensable factor for DNA replication, repair of DNA damage, chromatin structure maintenance, and cell-cycle progression, which also regulates tumor cell proliferation at both primary and metastatic sites.17,45 Interestingly, it is reported that a cancer-specific isoform of PCNA (csPCNA),46 with methyl esterification on aspartic and glutamic acid residues, is expressed in tumor tissues but not in normal tissues.45 However, its biochemical and molecular mechanisms are still unclear and further investigations will help clarify its roles in cellular malignant transformation and progression. In clinical research, a meta-analysis revealed that PCNA overexpression was correlated with advanced FIGO stage and poor survival in patients with cervical cancer, and PCNA overexpression was an important prognostic factor in glioma.22 Our results also suggested that high PCNA expression was associated with poor survival and advanced clinicopathological features in gastric cancer patients. All these results demonstrate that PCNA might be an indicator of survival for cancer patients.
It is encouraging that some targeting PCNA inhibitors have been reported recently, which open the door to potential therapeutic targeting of PCNA. There are two types of PCNA-targeting inhibitors including peptides and small molecules.45 One of the posttranslational modifications of PCNA for cell proliferation inhibition is phosphorylation of tyrosine residue 211 (pY211) of PCNA, which can be inhibited directly by peptide Y211F.47 Y211F peptide could inhibit the synthesis of DNA, which was shown as the cell-cycle arrest at the S phase and apoptosis in vitro. Similarly, intratumoral injection of the Y211F peptide had been showed to significantly inhibit tumor growth and reduce tumoral pY211-PCNA in xenograft tumor models.48,49 In addition, PCNA-I, one of the small molecules targeting PCNA inhibitors, interferes with PCNA functions by influencing trimerization of PCNA formation. Treatment with PCNA-I resulted in downregulation of chromatin-associated PCNA, inhibition of DNA replication, and suppression of the proliferation of a variety of cancer cell lines.50 Therefore, these promising approaches could be further exploited to targeting of cancer, and gastric cancer patients with a high PCNA expression might obtain a survival benefit from it.
Our analysis has a number of limitations. First, PCNA expression in gastric cancer tissues was detected by IHC in all included studies, but the accuracy of this method is dependent on the types of antibodies and their dilutions. As not all studies used the same primary antibody or antibody dilutions, this led to a potential bias. Subgroup analyses could not explore the effect of this difference on results because too few studies used the same antibodies and dilution ratios. Second, there was no uniform standard optimal threshold for evaluating PCNA IHC staining results. Cutoff values defining gastric cancer with high or low expression of PCNA were artificially set and varied from 23.8% to 75%, which might result in heterogeneity. As revealed in the subgroup analysis, heterogeneity was eliminated in the group with a cutoff value <50%. Third, each of the eligible studies had various parameters including sample size, age of participants, proportions of patients with high PCNA expression, and follow-up durations. Finally, we observed that studies reporting significant findings were more likely to be published in English language journals, whereas negative results were mostly published in native language journals, which were difficult to obtain and, thus, were excluded from our analysis.51 Egger’s test revealed significant publication bias in studies on OS and Lauren classification. The results of trim-and-fill analysis on pooled HRs or ORs indicated that our results are relatively stable and reliable.
Conclusion
In conclusion, this meta-analysis revealed that the increased PCNA expression is significantly associated with poor OS and DFS, as well as with clinicopathological characteristics, including deeper tumor invasion, lymph node metastases, and more advanced stage in gastric cancer patients. This suggests that PCNA might be a useful biomarker to predict patient prognosis and could be a valuable therapeutic target for gastric cancer.
Acknowledgments
This work was supported by National Natural Science Foundation of China (No 81372550) and Key Laboratory Programme of Liaoning Province (LZ2015080).
Disclosure
The authors report no conflicts of interest in this work.
References
Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–E386. | ||
Van Cutsem E, Sagaert X, Topal B, Haustermans K, Prenen H. Gastric cancer. Lancet. Epub 2016 May 5. | ||
Amedei A, Benagiano M, della Bella C, Niccolai E, D’Elios MM. Novel immunotherapeutic strategies of gastric cancer treatment. J Biomed Biotechnol. 2011;2011:437348. | ||
Sawada T, Yashiro M, Sentani K, et al. New molecular staging with G-factor supplements TNM classification in gastric cancer: a multicenter collaborative research by the Japan Society for Gastroenterological Carcinogenesis G-Project committee. Gastric Cancer. 2015;18(1):119–128. | ||
Xing X, Tang YB, Yuan G, et al. The prognostic value of E-cadherin in gastric cancer: a meta-analysis. Int J Cancer. 2013;132(11):2589–2596. | ||
Wu P, Wu D, Zhao L, et al. Prognostic role of STAT3 in solid tumors: a systematic review and meta-analysis. Oncotarget. 2016;7(15):19863–19883. | ||
Yiming L, Yunshan G, Bo M, et al. CD133 overexpression correlates with clinicopathological features of gastric cancer patients and its impact on survival: a systematic review and meta-analysis. Oncotarget. 2015;6(39):42019–42027. | ||
Yildirim M, Kaya V, Demirpence O, Gunduz S, Bozcuk H. Prognostic significance of p53 in gastric cancer: a meta-analysis. Asian Pac J Cancer Prev. 2015;16(1):327–332. | ||
Soleyman-Jahi S, Nedjat S, Abdirad A, Hoorshad N, Heidari R, Zendehdel K. Prognostic significance of matrix metalloproteinase-7 in gastric cancer survival: a meta-analysis. PLoS One. 2014;10(4):e0122316. | ||
Petrelli F, Cabiddu M, Coinu A, et al. Prognostic role of lactate dehydrogenase in solid tumors: a systematic review and meta-analysis of 76 studies. Acta Oncol. 2015;54(7):961–970. | ||
Miyachi K, Fritzler MJ, Tan EM. Autoantibody to a nuclear antigen in proliferating cells. J Immunol. 1978;121(6):2228–2234. | ||
Mathews MB, Bernstein RM, Franza BR Jr, Garrels JI. Identity of the proliferating cell nuclear antigen and cyclin. Nature. 1984;309(5966):374–376. | ||
Bravo R, Celis JE. A search for differential polypeptide synthesis throughout the cell cycle of HeLa cells. J Cell Biol. 1980;84(3):795–802. | ||
Bravo R, Fey SJ, Bellatin J, Larsen PM, Arevalo J, Celis JE. Identification of a nuclear and of a cytoplasmic polypeptide whose relative proportions are sensitive to changes in the rate of cell proliferation. Exp Cell Res. 1981;136(2):311–319. | ||
Srinivasan M, Jewell SD. Quantitative estimation of PCNA, c-myc, EGFR and TGF-alpha in oral submucous fibrosis – an immunohistochemical study. Oral Oncol. 2001;37(5):461–467. | ||
Moldovan GL, Pfander B, Jentsch S. PCNA, the maestro of the replication fork. Cell. 2007;129(4):665–679. | ||
Stoimenov I, Helleday T. PCNA on the crossroad of cancer. Biochem Soc Trans. 2009;37(Pt 3):605–613. | ||
Wang LF, Chai CY, Kuo WR, Tai CF, Lee KW, Ho KY. Correlation between proliferating cell nuclear antigen and p53 protein expression and 5-year survival rate in nasopharyngeal carcinoma. Am J Otolaryngol. 2006;27(2):101–105. | ||
Liu C, Liu J, Wang X, et al. Prognostic impact of nm23-H1 and PCNA expression in pathologic stage I non-small cell lung cancer. J Surg Oncol. 2011;104(2):181–186. | ||
Bantis A, Giannopoulos A, Gonidi M, et al. Expression of p120, Ki-67 and PCNA as proliferation biomarkers in imprint smears of prostate carcinoma and their prognostic value. Cytopathology. 2004;15(1):25–31. | ||
Li N, Deng W, Ma J, et al. Prognostic evaluation of Nanog, Oct4, Sox2, PCNA, Ki67 and E-cadherin expression in gastric cancer. Med Oncol. 2015;32(1):433. | ||
Lv Q, Zhang J, Yi Y, et al. Proliferating cell nuclear antigen has an association with prognosis and risks factors of cancer patients: a systematic review. Mol Neurobiol. 2016;53(9):6209–6217. | ||
Liu M, Li JS, Tian DP, Huang B, Rosqvist S, Su M. MCM2 expression levels predict diagnosis and prognosis in gastric cardiac cancer. Histol Histopathol. 2013;28(4):481–492. | ||
Yang C, Wen Y, Li H, et al. Overexpression of minichromosome maintenance 2 predicts poor prognosis in patients with gastric cancer. Oncol Rep. 2012;27(1):135–142. | ||
Konno S, Takebayashi Y, Aiba M, Akiyama S, Ogawa K. Clinicopathological and prognostic significance of thymidine phosphorylase and proliferating cell nuclear antigen in gastric carcinoma. Cancer Lett. 2001;166(1):103–111. | ||
Czyzewska J, Guzinska-Ustymowicz K, Pryczynicz A, Kemona A, Bandurski R. Immunohistochemical evaluation of Ki-67, PCNA and MCM2 proteins proliferation index (PI) in advanced gastric cancer. Folia Histochem Cytobiol. 2009;47(2):289–296. | ||
Lee KE, Lee HJ, Kim YH, et al. Prognostic significance of p53, nm23, PCNA and c-erbB-2 in gastric cancer. Jpn J Clin Oncol. 2003;33(4):173–179. | ||
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. | ||
Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17(24):2815–2834. | ||
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. | ||
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295(6):676–680. | ||
Poteca T, Poteca A, Sajin M, Comanescu M. Biological prognostic parameters in gastric carcinomas. Chirurgia (Bucur). 2014;109(3):347–354. | ||
Kuang RG, Wu HX, Hao GX, Wang JW, Zhou CJ. Expression and significance of IGF-2, PCNA, MMP-7, and alpha-actin in gastric carcinoma with Lauren classification. Turk J Gastroenterol. 2013;24(2):99–108. | ||
Ye YW, Dong RZ, Zhou Y, et al. Prognostic analysis of familial gastric cancer in Chinese population. J Surg Oncol. 2011;104(1):76–82. | ||
Kanaji S, Saito H, Tsujitani S, et al. Expression of polo-like kinase 1 (PLK1) protein predicts the survival of patients with gastric carcinoma. Oncology. 2006;70(2):126–133. | ||
Wu K, Zhao L, Li Y, Shan YJ, Wu LJ. Effects of vitamin E succinate on the expression of Fas and PCNA proteins in human gastric carcinoma cells and its clinical significance. World J Gastroenterol. 2004;10(7):945–949. | ||
Noda H, Maehara Y, Irie K, Kakeji Y, Yonemura T, Sugimachi K. Increased proliferative activity caused by loss of p21(WAF1/CIP1) expression and its clinical significance in patients with early-stage gastric carcinoma. Cancer. 2002;94(7):2107–2112. | ||
Elpek GO, Gelen T, Aksoy NH, Karpuzoglu T, Keles N. Microvessel count, proliferating cell nuclear antigen and Ki-67 indices in gastric adenocarcinoma. Pathol Oncol Res. 2000;6(1):59–64. | ||
Danesi DT, Spano M, Fabiano A, et al. Flow cytometric DNA ploidy, p53, PCNA, and c-erbB-2 protein expressions as predictors of survival in surgically resected gastric cancer patients. Cytometry. 2000;42(1):27–34. | ||
Kinugasa S, Abe S, Tachibana M, et al. Overexpression of transforming growth factor-beta1 in scirrhous carcinoma of the stomach correlates with decreased survival. Oncology. 1998;55(6):582–587. | ||
Maeda K, Chung YS, Takatsuka S, et al. Tumour angiogenesis and tumour cell proliferation as prognostic indicators in gastric carcinoma. Br J Cancer. 1995;72(2):319–323. | ||
Mangham DC, Rowlands DC, Newbold KM, Reynolds GM, Fielding JW, Hallissey MT. Expression of proliferating cell nuclear antigen (PCNA) in gastric carcinoma: no evidence for prognostic value. J Clin Pathol. 1994;47(5):473–474. | ||
Kakeji Y, Maehara Y, Adachi Y, et al. Proliferative activity as a prognostic factor in Borrmann type 4 gastric carcinoma. Br J Cancer. 1994;69(4):749–753. | ||
Jain S, Filipe MI, Hall PA, Waseem N, Lane DP, Levison DA. Prognostic value of proliferating cell nuclear antigen in gastric carcinoma. J Clin Pathol. 1991;44(8):655–659. | ||
Wang SC. PCNA: a silent housekeeper or a potential therapeutic target? Trends Pharmacol Sci. 2014;35(4):178–186. | ||
Malkas LH, Herbert BS, Abdel-Aziz W, et al. A cancer-associated PCNA expressed in breast cancer has implications as a potential biomarker. Proc Natl Acad Sci U S A. 2006;103(51):19472–19477. | ||
Zhao H, Chen MS, Lo YH, et al. The Ron receptor tyrosine kinase activates c-Abl to promote cell proliferation through tyrosine phosphorylation of PCNA in breast cancer. Oncogene. 2014;33(11):1429–1437. | ||
Zhao H, Lo YH, Ma L, et al. Targeting tyrosine phosphorylation of PCNA inhibits prostate cancer growth. Mol Cancer Ther. 2011;10(1):29–36. | ||
Yu YL, Chou RH, Liang JH, et al. Targeting the EGFR/PCNA signaling suppresses tumor growth of triple-negative breast cancer cells with cell-penetrating PCNA peptides. PLoS One. 2013;8(4):e61362. | ||
Tan Z, Wortman M, Dillehay KL, et al. Small-molecule targeting of proliferating cell nuclear antigen chromatin association inhibits tumor cell growth. Mol Pharmacol. 2012;81(6):811–819. | ||
Egger M, Zellweger-Zahner T, Schneider M, Junker C, Lengeler C, Antes G. Language bias in randomised controlled trials published in English and German. Lancet. 1997;350(9074):326–329. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



