Back to Journals » Cancer Management and Research » Volume 10
Prognostic significance of the 8th edition of the TNM classification for patients with extensive disease small cell lung cancer
Authors Shirasawa M, Fukui T, Kusuhara S, Hiyoshi Y, Ishihara M, Kasajima M, Nakahara Y , Otani S, Igawa S, Yokoba M, Mitsufuji H, Kubota M , Katagiri M , Sasaki J, Naoki K
Received 31 July 2018
Accepted for publication 3 October 2018
Published 21 November 2018 Volume 2018:10 Pages 6039—6047
DOI https://doi.org/10.2147/CMAR.S181789
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Xueqiong Zhu
Masayuki Shirasawa,1,* Tomoya Fukui,1,* Seiichiro Kusuhara,1 Yasuhiro Hiyoshi,1 Mikiko Ishihara,1 Masashi Kasajima,1 Yoshiro Nakahara,1 Sakiko Otani,1 Satoshi Igawa,1 Masanori Yokoba,2 Hisashi Mitsufuji,3 Masaru Kubota,1 Masato Katagiri,1 Jiichiro Sasaki,4 Katsuhiko Naoki1
1Department of Respiratory Medicine, Kitasato University School of Medicine, Kanagawa, Japan; 2Department of Medical Laboratory, Kitasato University School of Allied Health Sciences, Kanagawa, Japan; 3Fundamental Nursing, Kitasato University School of Nursing, Kanagawa, Japan; 4Research and Development Center for New Medical Frontiers, Kitasato University School of Medicine, Kanagawa, Japan
*These authors contributed equally to this work
Background: Small cell lung cancer (SCLC) is typically categorized according to disease extent as limited or extensive, and utility of the 8th TNM classification, recommended for lung cancer staging, which demonstrates a strong association with non-small-cell lung cancer (NSCLC) management, remains unclear.
Methods: This retrospective study included 277 consecutive SCLC patients treated at a single institution between 2008 and 2016.
Results: According to the currently used two-stage system, 186 (65.7%) of the patients were classified as having extensive disease (ED)-SCLC. Among the ED-SCLC patients, ten (5.3%), 38 (20.4%), 32 (17.2%), and 106 (57.0%) were categorized into stages M0, M1a, M1b, and M1c, respectively, according to the 8th TNM classification. There was a significant difference in overall survival based on the M descriptors: 15.8 (95% CI 9.4–22.2) months in the M1b group vs 7.3 (95% CI 5.7–8.9) months in the M1c group (P<0.001). Multivariate analysis showed that in addition to the known prognostic factors such as performance status, serum albumin, and lactate dehydrogenase, M descriptor was a prognostic factor (HR 1.95, 95% CI 1.38–2.77; P<0.001).
Conclusion: The 8th TNM classification has a prognostic value in SCLC. Similarly to NSCLC, treatment approaches should be considered on the basis of the 8th TNM classification, especially stage IVA separate from stage IVB in ED-SCLC patients.
Keywords: small cell lung cancer, extensive disease, TNM stage, prognosis
Introduction
Histologically, lung cancer can be broadly classified into non-small-cell lung cancer (NSCLC) and small cell lung cancer (SCLC). In NSCLC, the TNM staging established by the American Joint Committee on Cancer Staging and the Union for International Cancer Control is used to select treatment options such as surgery, radiotherapy, and systemic chemotherapy.1,2 Conversely, SCLC is typically categorized according to disease extent as limited disease (LD), which defines tumors that are limited to the ipsilateral hemithorax and regional lymph nodes and can be encompassed within a tolerable radiation field, and extensive disease (ED), which defines tumors outside these confines.3
SCLC accounts for around 15% of all lung cancer cases and is an aggressive disease characterized by widely disseminated metastases and a poor prognosis.4–6 Unlike other lung cancer types, SCLC is highly responsive to radiotherapy and chemotherapeutic drugs with survival benefit.3,7–11 Regardless of their high sensitivity for initial therapy, the median survival of SCLC patients has improved little in recent decades and remains at around 17 months for LD-SCLC and 8–13 months for ED-SCLC.12–15 The results of several recent studies investigating the efficacy of combined-modality therapies, such as prophylactic cranial irradiation and thoracic radiotherapy in ED-SCLC patients, remain controversial.16–18 Therefore, it is necessary to develop strategies and new anticancer drugs in patients with this aggressive disease.
In 2015, the International Association for the Study of Lung Cancer (IASLC) proposed the 8th edition of the TNM classification for lung cancer based on a new database composed of 94,708 cases diagnosed in 16 countries around the globe between 1999 and 2010.2 One of the most significant differences in the new criteria was the change in the M descriptors from three (M0, M1a, and M1b) to four (M0, M1a, M1b, and M1c).19 The concept of oligometastasis includes patients with metastases limited in number and organ site. In the case of some solid tumors, patients with oligometastasis can survive for a longer period than those with polymetastases.20 Such concepts are related to segmentation of TNM classification. Although the 8th TNM classification has been demonstrated to show a strong correlation with the management of NSCLC patients, insufficient data exist to support its use for the treatment of SCLC patients. Only a few studies have suggested that the TNM classification is correlated with SCLC prognosis,21,22 and the specific association between the M descriptors and prognosis in SCLC patients remains unclear.
In the current study, we evaluated the utility of the 8th TNM staging system for SCLC patients and determined whether the prognosis of SCLC was associated with the M descriptors based on the 8th TNM classification.
Materials and methods
Study patients and collection of clinical data
This retrospective study enrolled 277 consecutive patients who were pathologically diagnosed with SCLC and treated at the Kitasato University Hospital in Kanagawa, Japan, between January 2008 and December 2016. Results of computed tomography (CT), positron emission tomography (PET)-CT, bone scintigraphy, and brain magnetic resonance imaging (MRI) were reviewed to classify the patients using the 8th TNM classification as well as the classical two-stage system of LD and ED. LD-SCLC was defined as a tumor disease that was limited to the ipsilateral hemithorax and regional lymph nodes and could be encompassed in a safe radiotherapy field, and ED-SCLC was defined as a tumor with distant metastases beyond one radiation field. SCLC patients were classified according to the 8th TNM classification. Furthermore, survival times were analyzed for ED-SCLC patients in M0 (no distant metastasis), M1a (pleural or pericardial effusion without definite distant metastasis), M1b (a single metastatic lesion in a single organ), and M1c (multiple metastatic lesions in multiple organs or in a single organ) stages. For each patient, the following data were extracted in addition to staging: age at diagnosis; sex; smoking status; the Eastern Cooperative Oncology Group (ECOG) performance status (PS); and laboratory data including levels of albumin, lactate dehydrogenase (LDH), sodium, neuron-specific enolase (NSE), and pro-gastrin-releasing peptide (pro-GRP) obtained before treatment.
Evaluation of response and survival
Tumor response was classified in accordance with the Response Evaluation Criteria for Solid Tumors (version 1.1) based on the results of a complete medical history, physical examination, chest X-ray, CT of the chest and abdomen, and other procedures such as MRI of the brain, PET-CT, and bone scintigraphy. Progression-free survival (PFS) was defined as the time from the diagnosis of SCLC to the date of disease progression or the date of censoring at the final follow-up examination, and overall survival (OS) was defined as the time from the day of diagnosis to the date of death or the date of last contact (data cutoff: October 31, 2017).
Statistical analyses
All survival analyses were performed using the Kaplan–Meier method. Survival rates between subgroups based on prognostic factors were compared using the log-rank test. To identify prognostic factors, the Cox proportional hazards model was used for univariate and multivariate analyses. A two-tailed P-value of less than 0.05 was considered to indicate a statistically significant difference for all analyses. The multivariate analysis was performed with adjustment for covariates, including significant clinical factors based on univariate analyses. All analyses were performed using the SPSS software program, version 25.0 (IBM Corporation, Armonk, NY, USA).
This study was conducted in accordance with the Declaration of Helsinki, and only de-identified patient data were used. The retrospective study was approved by the Kitasato University Medical Ethics Organization (B17-253), which waived the requirement for patients’ informed consent owing to the nature of the study.
Results
Patient characteristics
There were 315 patients with histologically proven SCLC during the study period. After the exclusion of 38 patients who received only best supportive care, the remaining 277 patients with SCLC, comprising 91 (34.3%) LD-SCLC and 186 (65.7%) ED-SCLC patients (Figure 1), were included in the final analyses. Characteristics of the study patients are shown in Table 1. The median age was 70 (range 33–91) years, 228 (82.3%) patients were male, and only seven (2.5%) patients were non-smokers (Table 1). A total of 49 (17.8%) patients had concomitant interstitial pneumonia. All 277 patients received CT scans of the chest and abdomen, whereas 208 (75.1%), 47 (17.0%), and 259 (93.5%) patients received PET-CT, bone scintigraphy, and MRI or CT scan of the brain, respectively, as part of the initial staging evaluation.
The 8th TNM staging for SCLC patients
According to the IASLC staging system, 11 (12.1%), 13 (14.3%), and 67 (73.6%) of the 91 LD-SCLC patients were categorized into stages I, II, and III, respectively. Among the 186 ED-SCLC patients, ten (5.4%), 70 (37.6%), and 106 (57.0%) were classified into stages III (M0), IVA (M1a and M1b), and IVB (M1c), respectively (Figure 1 and Table 1).
Treatment in SCLC patients
All patients underwent chemotherapy with or without radiotherapy, and six LD-SCLC patients (five with stage I and one with stage II) underwent surgery followed by adjuvant chemotherapy. A total of 45 (16.2%) patients received chemoradiotherapy (CRT), including 40 and five patients who received concurrent and sequential CRT, respectively. Prophylactic cranial irradiation was administered in 14 (5.1%) patients following response to initial treatment, and 49 (17.7%) and 24 (8.7%) patients received palliative radiotherapy for brain and thoracic diseases, respectively. The most commonly used first-line chemotherapy regimens were carboplatin (CBDCA)-based doublet therapy in 89 (32.2%) patients and amrubicin monotherapy in 80 (29.0%) patients. The median number of regimens was 1 (range 1–3) in stage I, 1 (range 1–4) in stage II, 2 (range 1–5) in stage III, and 2 (range 1–8) in stage IV. Treatment details are presented in Table 2.
Treatment outcomes in SCLC patients
The OS times of the LD- and ED-SCLC patient groups were 37.2 (95% CI 25.7–48.7) and 13.7 (95% CI 11.9–15.5) months, respectively (Figure 2A). Among the entire study cohort, the OS of the stage I patients was superior to that of the stage II (P=0.04) and stage III (P=0.02) patients, and the OS of the stage III patients was not inferior to that of the stage II patients (P=0.47). The OS of the stage IV patients was significantly worse than that of the patients with stage I (P<0.001), II (P=0.009), or III (P<0.001) disease. The OS times of the patients with stage III and stage IV SCLC were 28.1 (95% CI 21.1–35.1) and 10.7 (95% CI 9.0–12.4) months, respectively (Figure 2B).
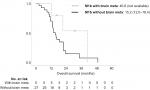
Among the ED-SCLC patients, the OS of the stage IVB patients with the M1c descriptor based on the 8th TNM classification was inferior to that of the stage III and IVA patients with the M0, M1a, or M1b descriptors (Figure 3). Specifically, the OS of the ED-SCLC patients with stage M1b was superior to that of those with stage M1c (15.8, 95% CI 9.4–22.2 vs 7.3, 95% CI 5.7–8.9 months; P<0.001). Furthermore, among the ED-SCLC patients, there were significant differences in PFS (6.2, 95% CI 5.8–6.6 vs 4.6, 95% CI 3.8–5.4 months; P=0.002) and OS (16.0, 95% CI 13.2–18.8 vs 7.3, 95% CI 5.7–8.9 months; P<0.001) between the stage III or IVA (M0, M1a, and M1b) and the stage IVB (M1c) patients. In stage M1b, patients with brain metastasis (n=5) tended to have better OS than those with metastases from other sites (40.8, 95% CI not evaluated vs 15.2, 95% CI 12.0–18.4 months; P<0.001) (Figure S1). In this study, three patients were treated with a cyber-knife treatment and one underwent brain tumor excision before chemotherapy, and all patients received whole-brain radiation therapy during the treatment.
Survival analyses with consideration of clinical characteristics
Univariate analyses of the clinical characteristics revealed that ECOG PS (2–4 vs 0–1; P=0.006), serum albumin (low vs normal; P<0.001), and serum LDH (high vs normal; P<0.001), which were well-known prognostic factors, were significantly associated with OS. M0 (HR 1.43, 95% CI 1.12–1.83; P=0.005), M1a (HR 1.33, 95% CI 1.07–1.66; P=0.010), and M1b (HR 2.23, 95% CI 1.43–3.49, P<0.001) were significantly associated with better survival compared to M1c, and there were no differences in M0 vs M1a (HR 1.87, 95% CI 0.82–4.24; P=0.135), M0 vs M1b (HR 1.22, 95% CI 0.81–1.82; P=0.339), or M1a vs M1b (HR 0.769, 95% CI 0.44–1.33; P=0.347). M descriptor status was based on the 8th TNM classification (M1c vs M0, M1a, and M1b; P<0.001), and we performed multivariate analyses adjusted for ECOG PS, albumin level, LDH level, and M descriptor status, all of which had P-values less than 0.05 in the univariate analyses. Our analysis revealed that high LDH level (HR 1.73, 95% CI 1.18–2.54; P=0.005) and ED-SCLC with a stage M1c descriptor (HR 1.95, 95% CI 1.38–2.77; P<0.001) were unfavorable prognostic factors (Table 3).
  | Table 3 Overall survival analyses of the patients with extensive disease small cell lung cancer (n=186) Abbreviations: ECOG, Eastern Cooperative Oncology Group; LDH, lactate dehydrogenase. |
Discussion
This retrospective study evaluating the revised M descriptors of the 8th TNM classification in SCLC patients found that the 8th TNM classification could provide prognostic information on SCLC, especially in patients with ED-SCLC who received chemotherapy. PET is a potentially useful modality for the accurate initial staging of SCLC. We demonstrated that the prognosis of ED-SCLC patients with stage M1b was significantly better than that of those with stage M1c ED-SCLC. In addition, the OS of the stage M1b patients was not inferior to that of the stage M1a patients. Regarding the M descriptors included in the latest IASLC report, the prognosis of NSCLC patients in stage M1c was significantly worse than that of those in stage M1b.2 Conversely, other studies found that the prognosis was not different between patients with stage M1b SCLC and those with stage M1c SCLC.21 Appropriate imaging-based diagnosis is essential during staging of lung cancer. PET can ensure that a patient’s disease is not overstaged by CT.23 In a previous study on SCLC patients,21 PET was performed in 23% of patients, whereas bone scintigraphy was performed in 41% of the patients during initial evaluation for staging. One potential explanation for our finding that the prognosis of stage M1b SCLC was different from that of stage M1c is the markedly different utilization rates of upper chest or abdominal CT (100%), brain MRI/CT (94%), PET-CT (70%), and bone scintigraphy (20%). As novel diagnostic modalities such as CT, MRI, and PET-CT have been increasingly adopted into clinical practice, the sensitivity of detecting small lesions has improved in parallel.24 In the current study, the initial comprehensive staging according to the 8th TNM classification including PET-CT and brain MRI/CT had enough power to accurately discriminate between the subgroups of ED-SCLC patients treated with chemotherapy.
The number of organ metastatic sites involved was reported to be associated with prognosis in ED-SCLC patients.25,26 The 8th TNM classification reflects the prognostic impact of the number and locations of distant metastases based on detailed information. In NSCLC, the M descriptors of the latest IASLC report, in which patients with stage M1c disease have been separated from the former category of stage M1b, were associated with a significantly worse prognosis than the currently used category of stage M1b. In the current report, the prognosis of patients with stage M1b ED-SCLC was significantly better than that of those with stage M1c ED-SCLC. The concept of oligometastases, defining a small number of metastases limited to an organ, describes an intermediate state of cancer spread between localized disease and widespread metastases20,27 and may be treated by local therapy such as surgery or radiotherapy.28–30 Among SCLC patients, metastatic involvement of the central nervous system, bone marrow, or liver is an unfavorable prognostic factor compared with that of other sites, although these variables are confounded by the number of sites that are involved.25,26 Among the patients with stage M1b ED-SCLC in the current study, there was a difference in the outcome between the brain as the only metastatic site and other organs as the metastatic site (brain [n=5], 40.8 months, 95% CI not available vs other sites [n=27], 15.2 months, 95% CI 12.0–18.4; P=0.17). All patients with stage M1b SCLC with brain metastasis received irradiation of the brain and one patient underwent brain tumor excision before chemotherapy. This finding suggests the possibility of local therapy as a beneficial approach for certain patients with systemic disease. Among NSCLC patients, the prognosis of those with a single brain metastasis is considerably better than that of those with multiple brain metastases; furthermore, NSCLC patients with a single brain metastasis benefit from locally aggressive and ablative treatments such as stereotactic irradiation or surgery.28–30 However, a consensus has not been reached regarding localized therapy for ED-SCLC patients with oligometastases. Even patients with stage M1b ED-SCLC are suggested to be considered as an optimal population for combined-modality therapeutic approaches such as local radiotherapy in combination with systemic chemotherapy.
The current study has certain limitations. First, this was a retrospective study conducted at a single institution; hence, the results cannot be considered definitive. Second, the present study suggested prognostic differences between stage M1b and M1c patients with ED-SCLC but could not confirm the utility of local therapy combined with systemic chemotherapy. The outcome for patients with stage M1b ED-SCLC may be a result of the selection criteria of the patients with SCLC and the low statistical power due to the small sample size. Whether this finding should translate into a more aggressive treatment approach for M1b disease requires further study. Third, although the ethnic differences in the sex and smoking patterns between Japanese and non-Japanese patients is uncertain, it is difficult to completely remove the bias. Finally, the patients received different chemotherapeutic regimens based on distinct patient characteristics. There is heterogeneity in the treatment regimens administered based on different patient characteristics; however, we believe that this is not a potential selection bias because all patients were included in the study. The results of the current study should not be regarded as a cause for change in treatment in clinical practice until further evaluation has been conducted by clinical trials.
Conclusion
This retrospective study including 277 subjects demonstrated the prognostic value of the 8th TNM staging system in SCLC patients treated with systemic chemotherapy. In addition to patients diagnosed with NSCLC, those with SCLC currently categorized as ED should be categorized into subgroups based on the 8th TNM classification. Appropriate patient selection based on the 8th TNM staging system should be taken into consideration for the development of optimal treatment strategies.
Acknowledgment
The authors would like to thank Enago (www.enago.jp) for the English language review.
Disclosure
The authors report no conflicts of interest in this work.
References
Detterbeck FC, Boffa DJ, Tanoue LT. The new lung cancer staging system. Chest. 2009;136(1):260–271. | ||
Goldstraw P, Chansky K, Crowley J, et al; International Association for the Study of Lung Cancer Staging and Prognostic Factors Committee, Advisory Boards, and Participating Institutions; International Association for the Study of Lung Cancer Staging and Prognostic Factors Committee Advisory Boards and Participating Institutions. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol. 2016;11(1):39–51. | ||
Socinski MA, Bogart JA. Limited-stage small-cell lung cancer: the current status of combined-modality therapy. J Clin Oncol. 2007;25(26):4137–4145. | ||
van Meerbeeck JP, Fennell DA, De Ruysscher DK. Small-cell lung cancer. Lancet. 2011;378(9804):1741–1755. | ||
Jett JR, Schild SE, Kesler KA, Kalemkerian GP. Treatment of small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e400S–e419S. | ||
Gazdar AF, Bunn PA, Minna JD. Small-cell lung cancer: what we know, what we need to know and the path forward. Nat Rev Cancer. 2017;17(12):725–737. | ||
Takada M, Fukuoka M, Kawahara M, et al. Phase III study of concurrent versus sequential thoracic radiotherapy in combination with cisplatin and etoposide for limited-stage small-cell lung cancer: results of the Japan Clinical Oncology Group Study 9104. J Clin Oncol. 2002;20(14):3054–3060. | ||
De Ruysscher D, Pijls-Johannesma M, Bentzen SM, et al. Time between the first day of chemotherapy and the last day of chest radiation is the most important predictor of survival in limited-disease small-cell lung cancer. J Clin Oncol. 2006;24(7):1057–1063. | ||
Noda K, Nishiwaki Y, Kawahara M, et al; Japan Clinical Oncology Group. Irinotecan plus cisplatin compared with etoposide plus cisplatin for extensive small-cell lung cancer. N Engl J Med. 2002;346(2):85–91. | ||
Hanna N, Bunn PA Jr, Langer C, et al. Randomized phase III trial comparing irinotecan/cisplatin with etoposide/cisplatin in patients with previously untreated extensive-stage disease small-cell lung cancer. J Clin Oncol. 2006;24(13):2038–2043. | ||
Sundstrøm S, Bremnes RM, Kaasa S, et al; Norwegian Lung Cancer Study Group. Cisplatin and etoposide regimen is superior to cyclophosphamide, epirubicin, and vincristine regimen in small-cell lung cancer: results from a randomized phase III trial with 5 years’ follow-up. J Clin Oncol. 2002;20(24):4665–4672. | ||
Gaspar LE, Gay EG, Crawford J, Putnam JB, Herbst RS, Bonner JA. Limited-stage small-cell lung cancer (stages I-III): observations from the National Cancer Data Base. Clin Lung Cancer. 2005;6(6):355–360. | ||
Govindan R, Page N, Morgensztern D, et al. Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol. 2006;24(28):4539–4544. | ||
Foster NR, Mandrekar SJ, Schild SE, et al. Prognostic factors differ by tumor stage for small cell lung cancer: a pooled analysis of North Central Cancer Treatment Group trials. Cancer. 2009;115(12):2721–2731. | ||
Fiegl M, Pircher A, Waldthaler C, et al. Small steps of improvement in small-cell lung cancer (SCLC) within two decades: a comprehensive analysis of 484 patients. Lung Cancer. 2014;84(2):168–174. | ||
Slotman B, Faivre-Finn C, Kramer G, et al. Prophylactic cranial irradiation in extensive small-cell lung cancer. N Engl J Med. 2007;357:664–672. | ||
Slotman BJ, van Tinteren H. Which patients with extensive stage small-cell lung cancer should and should not receive thoracic radiotherapy? Transl Lung Cancer Res. 2015;4(3):292–294. | ||
Nosaki K, Seto T. The Role of Radiotherapy in the Treatment of Small-Cell Lung Cancer. Curr Treat Options Oncol. 2015;16(12):56. | ||
Eberhardt WE, Mitchell A, Crowley J, et al; International Association for Study of Lung Cancer Staging and Prognostic Factors Committee, Advisory Board Members, and Participating Institutions.. The IASLC Lung Cancer Staging Project: Proposals for the Revision of the M Descriptors in the Forthcoming Eighth Edition of the TNM Classification of Lung Cancer. J Thorac Oncol. 2015;10(11):1515–1522. | ||
Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol. 1995;13(1):8–10. | ||
Nicholson AG, Chansky K, Crowley J, et al; Staging and Prognostic Factors Committee, Advisory Boards, and Participating Institutions; Staging and Prognostic Factors Committee Advisory Boards and Participating Institutions. The International Association for the Study of Lung Cancer Lung Cancer Staging Project: Proposals for the Revision of the Clinical and Pathologic Staging of Small Cell Lung Cancer in the Forthcoming Eighth Edition of the TNM Classification for Lung Cancer. J Thorac Oncol. 2016;11(3):300–311. | ||
Li J, Zhao Y, Li C, Zhu L, Liu C, Liu L. The revision of 8th edition TNM stage criteria is more accurate in prediction postoperative survival for SCLC patients. Int J Surg. 2017;48:83–85. | ||
Vinjamuri M, Craig M, Campbell-Fontaine A, Almubarak M, Gupta N, Rogers JS. Can positron emission tomography be used as a staging tool for small-cell lung cancer? Clin Lung Cancer. 2008;9(1):30–34. | ||
Dayen C, Debieuvre D, Molinier O, et al. New insights into stage and prognosis in small cell lung cancer: an analysis of 968 cases. J Thorac Dis. 2017;9(12):5101–5111. | ||
Albain KS, Crowley JJ, LeBlanc M, Livingston RB. Determinants of improved outcome in small-cell lung cancer: an analysis of the 2,580-patient Southwest Oncology Group data base. J Clin Oncol. 1990;8(9):1563–1574. | ||
Albain KS, Crowley JJ, Livingston RB. Long-term survival and toxicity in small cell lung cancer. Expanded Southwest Oncology Group experience. Chest. 1991;99(6):1425–1432. | ||
Niibe Y, Chang JY. Novel insights of oligometastases and oligo-recurrence and review of the literature. Pulm Med. 2012;2012:261096. | ||
Tsao MN, Rades D, Wirth A, et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): An American Society for Radiation Oncology evidence-based guideline. Pract Radiat Oncol. 2012;2(3):210–225. | ||
Mehta MP, Tsao MN, Whelan TJ, et al. The American Society for Therapeutic Radiology and Oncology (ASTRO) evidence-based review of the role of radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys. 2005;63(1):37–46. | ||
Modi A, Vohra HA, Weeden DF. Does surgery for primary non-small cell lung cancer and cerebral metastasis have any impact on survival? Interact Cardiovasc Thorac Surg. 2009;8(4):467–473. |
Supplementary material
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.