Back to Journals » Cancer Management and Research » Volume 11
Prognostic significance of preoperative albumin-to-globulin ratio and prognostic nutritional index combined score in Siewert type 3 adenocarcinoma of esophagogastric junction
Authors Wang Y, Zhu Z, Li C, Ma Y, You Q, Li Z, Zhang H, Song H, Xue Y
Received 18 October 2018
Accepted for publication 22 February 2019
Published 14 August 2019 Volume 2019:11 Pages 7631—7638
DOI https://doi.org/10.2147/CMAR.S191333
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Rituraj Purohit
Yimin Wang*, Ziyu Zhu*, Chunfeng Li, Yan Ma, Qi You, Zhiguo Li, Hongfeng Zhang, Hongjiang Song, Yingwei Xue
Department of Gastrointestinal Surgery, Harbin Medical University Cancer Hospital, Harbin Medical University, Harbin 150081, People’s Republic of China
*These authors contributed equally to this work
Purpose: Preoperative nutrition-inflammation-based indicators have been reported to predict the prognosis of malignancies. We evaluated the prognostic significance of a combined score of the albumin-to-globulin ratio (AGR) and prognostic nutritional index (PNI) for overall survival (OS) outcomes in patients with Siewert type 3 adenocarcinoma of esophagogastric junction (S3-AEG).
Patients and methods: The prognostic significance of variables associated with 215 S3-AEG patients’ OS were assessed through univariate and multivariate analyses. The cutoff value of the preoperative AGR and PNI were calculated by the receiver operating characteristic curve (ROC). Patients with either an elevated AGR (≥1.72, cutoff value) or PNI (≥45.55, cutoff value) were given a score of 1; otherwise, they were given a score of 0. The AGR-PNI score ranged from 0 to 2.
Results: OS was independently associated with the N stage (HR: 0.336, 95% CI: 0.141–0.805, P=0.014) and AGR-PNI score (HR: 0.623, 95% CI: 0.487–0.797, P<0.001). Patients with AGR-PNI scores of 0, 1 and 2 had significant differences in OS (P=0.001). The prognostic role of AGR-PNI was significant in patients with stage I + II (P=0.043) and stage III S3-AEGs (P=0.003). ROC analysis indicated that the predictive ability of the AGR-PNI score was better than that of the other parameters.
Conclusion: The preoperative AGR-PNI score was a significant prognosticator of postoperative survival in patients with S3-AEG and could identify high-risk populations for reasonable therapy and effective follow-up.
Keywords: adenocarcinoma of esophagogastric junction, albumin-to-globulin ratio, prognostic nutritional index
Introduction
Adenocarcinoma of esophagogastric junction (AEG) emerged and has rapidly increased in prevalence in Western countries over recent decades.1 According to the 8th edition of the American Joint Committee on Cancer (AJCC) cancer TNM staging system, Siewert type 2 and 3 AEG should be classified as gastric cancer.2 Gastric cancer greatly contributes to the global cancer burden,3 as it is the third leading cause of cancer deaths worldwide,4 which is almost identical to the situation in China.5 Due to their high rates of recurrences, the prognosis of patients with AEG or gastric cancer remains poor even after curative surgery,6,7 and the postoperative 5-year survival after surgery is less than 40%.8,9 Therefore, it would be helpful to design a scoring system to target long-term outcomes for AEG patients, as well as guide treatment and follow-up.
Accumulating evidence has revealed that systemic immune-inflammation plays pivotal roles in carcinogenesis and tumour progression. The neutrophil to lymphocyte ratio (NLR),10 platelet to lymphocyte ratio (PLR),11 prognostic nutritional index (PNI),12 and albumin to globulin ratio (AGR)13,14 are inflammation-based hallmarks that have been proved to be associated with worse prognosis in various human malignancies. Moreover, no studies have validated the prognostic value of an integrated scoring system consisting inflammation-based hallmarks in AEG. Consequently, the current study aimed to determine whether the combination of the PNI and AGR could better predict OS of patients after radical surgery for AEG.
Patients and methods
This study was approved by the Ethical Committee of Harbin Medical University Cancer Hospital and conducted in accordance with the Declaration of Helsinki.
Study population and follow-up
This retrospective study involved 215 consecutive patients who underwent radical open surgery (R0, D2) for S3-AEG in Harbin Medical University Cancer Hospital from January 1993 to January 2013. Study approval was granted by the local institution review board, and all patients involved provided written informed consent. AEG diagnoses were postoperatively confirmed by pathologists according to the current AJCC classification. Neither chemotherapy nor radiotherapy was used for treatment in this study. Patients who experienced the following situations were excluded: 1) intestinal obstruction, active bleeding, autoimmune diseases or other inflammatory disorders; 2) missing data; 3) preoperative blood product transfusion; 4) having other malignancies; and 5) AEG-unrelated death. Each AEG patient was followed up via telephone and an outpatient visit until January 2018 or their date of death. OS was measured as the interval from the date of surgery to death or latest follow-up.
Data collection
The clinical data and baseline demographics of the patients were collected from the Harbin Medical University Cancer Hospital CRC database and chart review. Blood tests were measured within one week before surgery. Serum carcinoembryonic antigen (CEA), C-reactive protein (CRP), carbohydrate antigen levels and hepatitis B virus (HBV) infection status were not routine tests at diagnosis and were excluded in this retrospective study.
Prognostic scoring system
The AGR was defined as the ratio between the serum albumin concentration (g/L) and the serum globulin concentration (g/L). In the same way, the PLR was defined as the ratio between the absolute platelet count (×109/L) and the absolute lymphocyte count (×109/L), while the NLR was defined as the ratio between the absolute neutrophil count (×109/L) and the absolute lymphocyte count (×109/L).
The prognostic nutritional index (PNI) was calculated from the serum albumin concentration and absolute lymphocyte count: serum albumin concentration (g/L) +5× total lymphocyte count (×109/L).15,16
The optimal cutoff points for the preoperative AGR and PNI were selected using receiver operating characteristic (ROC) curve analysis. The optimal cutoff points for age, tumour size, and the preoperative NLR and PLR were according to the median values.
AGR or PNI values less than their cutoff points were assigned a score of 0; otherwise, they were assigned a score of 1. The final prognostic score for AGR-PNI was calculated as the AGR score + the PNI score.
Statistical analyses
All data analyses were conducted with the SPSS version 19.0 software (IBM Corporation, Armonk, NY, USA). Two-sided P-values <0.05 were considered to be statistically significant. The relationships between the prognostic scores (AGR-PNI) and other clinicopathological parameters were elucidated with a chi-square test. Kaplan-Meier curves were constructed for survival analysis. ROC curve analyses for OS were carried out to determine the optimal cutoff values of the AGR and PNI, and the AUC values were used to compare the predictive ability of the prognosticators. Multivariate analyses were performed with the Cox hazards regression model based on the risk factors filtered by univariate analyses to determine independent factors for prognosis.
Results
Patient characteristics
Of 215 S3-AEG patients, 182 (84.7%) were male and 33 (15.3%) were female. The patients’ median age was 62 years, ranging from 30 to 85. The cut-off values of age, tumour size, and the preoperative NLR and PLR were 62 years, 5.0 cm, 2.2, and 130.8, respectively. The number of well-differentiated cancer grade cases was 99. According to the 8th edition of AJCC, 20 patients were in stage I, 67 were in stage II, and 128 were in stage III. Among these patients, 9 were in T1, 15 were in T2, 19 were in T3, 172 were in T4, and 134 had lymph node metastasis. The median follow-up period in this study was 22 months, ranging from 1.5 to 134 months. Overall, 144 patients were confirmed to be dead at the end of the follow-up. The 3-year survival rate and 5-year survival rate were 35.35% and 20.47%, respectively. The numbers of cases with different AGR-PNI scores are shown in Table 1.
 |
Table 1 Univariate and multivariate analyses of the clinicopathological characteristics for overall survival in 215 patients with S3-AEG |
Optimal cutoff values
Based on the ROC curve analyses for OS, the cutoff values were defined as 1.72 for the AGR (sensitivity, 52.1; specificity, 70.1; area under the curve (AUC), 0.600; P=0.017) and 45.55 for the PNI (sensitivity, 88.7; specificity, 70.8; AUC, 0.574; P=0.079) (Figure 1).
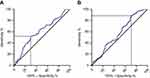 |
Figure 1 Receiver operating characteristic curve for the (A) albumin-to-globulin ratio and (B) prognostic nutritional index. |
Univariate and multivariate analyses
The results of univariate analyses showed that the T stage (P=0.002), lymph node metastasis (P=0.071), TNM stage (P<0.001), tumour size (P=0.033) and AGR-PNI score (P<0.001) were statistically significantly associated with AEG patients’ OS (Table 1). Because pTNM stage was too strong related with T and N, it was not further analysed by multivariate analysis. Then, the 4 variables were further analysed by multivariate analyses, and the results showed that the N stage (HR: 0.469, 95% CI: 0.320–0.688, P<0.001) and AGR-PNI score (HR: 0.613, 95% CI: 0.226–0.923, P<0.001) were independent prognosticators (Table 1).
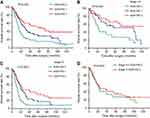
Prognostic scores and survival
Kaplan-Meier analyses revealed that the 5-year survival rates of AEG patients with AGR-PNI scores of 2, 1, and 0 were 36.2%, 13.1%, and 12.8%, respectively (P=0.001; Figure 2A). Patients with an AGR-PNI score of 2 had significantly longer mean OS than patients with an AGR-PNI score of 1 or 0 (56.0 vs 28.3 and 14.5 months; P=0.001; Figure 2A). The predictive abilities of the AGR-PNI score were dramatic in stage I + II (P=0.043; Figure 2B) and in stage III (P=0.003; Figure 2C). The mean OS was longer in stage III patients with an AGR-PNI score of 2 (24.0 months) than in stage I + II patients with an AGR-PNI score of 0 (22.0 months) (P=0.643; Figure 2D).
Prognostic scores and clinical data
AGR-PNI scores were significantly associated with age (P=0.019), tumour size (P=0.016), PLR scores (P=0.032) and NLR scores (P=0.004) (Table 2).
 |
Table 2 Relationships between AGR-PNI and the clinicopathological characteristics of 215 S3-AEG patients |
Predictive ability of prognosticators
The results of the comparison of AUC values indicated that the predictive ability of the AGR-PNI scores (Table 3, AUC, 0.653, 95% CI: 0.576–0.729, P<0.001) was better than that of other parameters (Figure 3).
 |
Table 3 Area under the ROC curves of the tumour size and of the NLR, PLR, and AGR-PNI scores |
Discussion
Mounting evidence reveals that a poor nutritional status and systemic immune-inflammation correlate with a grave prognosis in a variety of malignancies. In this study, we assessed the prognostic relevance of the nutrition-inflammation-based AGR-PNI score in S3-AEG patients after radical surgery. Our results suggested that the AGR-PNI score could serve as independent prognosticators for S3-AEG better than other parameters.
The inflammatory cells in the tumour microenvironment have been found to play crucial roles in carcinogenesis, facilitation of tumour cell proliferation, invasion and migration.17–19 Previous studies have highlighted that hypoalbuminemia is associated with inflammatory mediators and increased tumour-related mortality in several malignancies.20–23 Globulin could reflect cumulative exposure to various proinflammatory cytokines, such as interleukins and tumour necrosis factor α.24
Various recent studies have indicated that low PNI and AGR scores and high PLR and NLR scores are associated with poor prognosis in various types of malignancies.13,14,25–30 Nevertheless, these prognosticators may not comprehensively predict tumour patients’ OS. Herein, our study evaluated the prognostic value of integrated prognosticators in S3-AEG patients.
In this study, we found that the AGR-PNI score was significantly negatively correlated with AEG patients’ age and tumour size. Our data were consistent with previous studies, in which nutrition-inflammation-based prognostic indicators were dramatically associated with tumour progression.12,30,31 Our Kaplan-Meier analyses revealed that the AGR-PNI score positively correlated with AEG patients’ OS (P=0.001). The mean OS was longer in stage III patients with an AGR-PNI score of 2 (24.0 months) than in stage I + II patients with an AGR-PNI score of 0 (22.0 months). Although there was no statistical significance (P=0.643; Figure 2D), the difference was large enough to distinguish AEG patients at high risk better than the TNM stage alone. Moreover, multivariate analyses showed that the AGR-PNI score was an independent prognosticator for AEG. In addition, the prognostic value of the AGR-PNI score was verified in stage I + II patients (P=0.043) and in stage III patients (P=0.003).
Our findings also demonstrated that other integrated indicators, including the PLR score (P=0.173) and NLR score (P=0.506), failed to be independent prognostic predictors of OS for AEG in univariate analyses. These results contradicted previous studies that the PLR and NLR scores were independent predictors of OS for gastric cancer.32 The AUC value of the AGR-PNI score was higher than that of other integrated indicators we tested in this study (0.653; P<0.001), which revealed that the AGR-PNI score had a better prognostic value than other integrated indicators.
Nonetheless, we could not ignore the limitations of the current study, which might have affected our results. This retrospective study was initiated by a single centre, which was the major limitation. However, the validity of our results came from a large database with detailed information on tumour characteristics and treatment, which could investigate the prognostic value of integrated nutritional and inflammatory indicators.
Conclusion
We found that the AGR-PNI score was an independent prognostic predictor of OS for AEG. A low AGR-PNI score was associated with poor prognosis in S3-AEG patients.
Acknowledgment
This work was supported by the Harbin Science and Technology Bureau Research and Development Project of Applied Technology (No. 2017RAXXJ054) and Nn 10 Program of Harbin Medical University Cancer Hospital (No. Nn 10 PY 2017-03).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sano T. Gastric cancer: Asia and the world. Gastric Cancer. 2017;20(Suppl 1):1–2. doi:10.1007/s10120-017-0694-9
2. Amin MB, Greene FL, Edge SB, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67(2):93–99. doi:10.3322/caac.21388
3. Colquhoun A, Arnold M, Ferlay J, Goodman KJ, Forman D, Soerjomataram I. Global patterns of cardia and non-cardia gastric cancer incidence in 2012. Gut. 2015;64(12):1881–1888. doi:10.1136/gutjnl-2014-308915
4. Ford JM. Hereditary gastric cancer: an update at 15 years. JAMA Oncol. 2015;1(1):16–18. doi:10.1001/jamaoncol.2014.187
5. Chen W, Sun K, Zheng R, et al. Cancer incidence and mortality in China, 2014. Chin J Cancer Res. 2018;30(1):1–12. doi:10.21147/j.issn.1000-9604.2018.01.01
6. Moehler M, Baltin CT, Ebert M, et al. International comparison of the German evidence-based S3-guidelines on the diagnosis and multimodal treatment of early and locally advanced gastric cancer, including adenocarcinoma of the lower esophagus. Gastric Cancer. 2015;18(3):550–563. doi:10.1007/s10120-014-0403-x
7. Roviello G, Petrioli R, Marano L, et al. Angiogenesis inhibitors in gastric and gastroesophageal junction cancer. Gastric Cancer. 2016;19(1):31–41. doi:10.1007/s10120-015-0537-5
8. Fuchs CS, Niedzwiecki D, Mamon HJ, et al. Adjuvant chemoradiotherapy with epirubicin, cisplatin, and fluorouracil compared with adjuvant chemoradiotherapy with fluorouracil and leucovorin after curative resection of gastric cancer: results from CALGB 80101 (Alliance). J Clinl Oncol. 2017;35(32):3671–3677. doi:10.1200/JCO.2017.74.2130
9. Haga Y, Hato S, Ikenaga M, et al. Validation of an assessment tool: estimation of postoperative overall survival for gastric cancer. Eur J Surg Oncol. 2018;44(4):515–523. doi:10.1016/j.ejso.2018.01.002
10. Reddy JP, Hernandez M, Gunther JR, et al. Pre-treatment neutrophil/lymphocyte ratio and platelet/lymphocyte ratio are prognostic of progression in early stage classical Hodgkin lymphoma. Br J Haematol. 2018;180(4):545–549. doi:10.1111/bjh.15054
11. Zhao QT, Yuan Z, Zhang H, et al. Prognostic role of platelet to lymphocyte ratio in non-small cell lung cancers: a meta-analysis including 3,720 patients. Int Cancer. 2016;139(1):164–170. doi:10.1002/ijc.30060
12. Chan AW, Chan SL, Wong GL, et al. Prognostic Nutritional Index (PNI) predicts tumor recurrence of very early/early stage hepatocellular carcinoma after surgical resection. Ann Surg Oncol. 2015;22(13):4138–4148. doi:10.1245/s10434-015-4516-1
13. Niwa N, Matsumoto K, Ide H, Nagata H, Oya M. Prognostic value of pretreatment albumin-to-globulin ratio in patients with non-muscle-invasive bladder cancer. Clin Genitourin Cancer. 2018;16(3):e655–e661. doi:10.1016/j.clgc.2017.12.013
14. Shimizu T, Ishizuka M, Suzuki T, et al. The preoperative globulin-to-albumin ratio, a novel inflammation-based prognostic system, predicts survival after potentially curative liver resection for patients with hepatocellular carcinoma. J Surg Oncol. 2017;116(8):1166–1175. doi:10.1002/jso.24772
15. Tokunaga R, Sakamoto Y, Nakagawa S, et al. Prognostic nutritional index predicts severe complications, recurrence, and poor prognosis in patients with colorectal cancer undergoing primary tumor resection. Dis Colon Rectum. 2015;58(11):1048–1057. doi:10.1097/DCR.0000000000000458
16. Mohri T, Mohri Y, Shigemori T, Takeuchi K, Itoh Y, Kato T. Impact of prognostic nutritional index on long-term outcomes in patients with breast cancer. World J Surg Oncol. 2016;14(1):170. doi:10.1186/s12957-016-0920-7
17. Elinav E, Nowarski R, Thaiss CA, Hu B, Jin C, Flavell RA. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nature Rev Cancer. 2013;13(11):759–771. doi:10.1038/nrc3611
18. Dehne N, Mora J, Namgaladze D, Weigert A, Brüne B. Cancer cell and macrophage cross-talk in the tumor microenvironment. Curr Opin Pharmacol. 2017;35:12–19. doi:10.1016/j.coph.2017.04.007
19. Bussard KM, Mutkus L, Stumpf K, Gomez-Manzano C, Marini FC. Tumor-associated stromal cells as key contributors to the tumor microenvironment. Breast Cancer Res. 2016;18(1):84. doi:10.1186/s13058-016-0740-2
20. Carr BI, Guerra V. Serum albumin levels in relation to tumor parameters in hepatocellular carcinoma patients. Int J Biol Markers. 2017;32(4):e391–e396. doi:10.5301/ijbm.5000300
21. Tsai MH, Chuang HC, Lin YT, et al. Clinical impact of albumin in advanced head and neck cancer patients with free flap reconstruction-a retrospective study. PeerJ. 2018;6:e4490. doi:10.7717/peerj.4490
22. Ikeda S, Yoshioka H, Ikeo S, et al. Serum albumin level as a potential marker for deciding chemotherapy or best supportive care in elderly, advanced non-small cell lung cancer patients with poor performance status. BMC Cancer. 2017;17(1):797. doi:10.1186/s12885-017-3814-3
23. Miura K, Hamanaka K, Koizumi T, et al. Clinical significance of preoperative serum albumin level for prognosis in surgically resected patients with non-small cell lung cancer: comparative study of normal lung, emphysema, and pulmonary fibrosis. Lung Cancer. 2017;111:88–95. doi:10.1016/j.lungcan.2017.07.003
24. Pfensig C, Dominik A, Borufka L, Hinz M, Stange J, Eggert M. A new application for albumin dialysis in extracorporeal organ support: characterization of a putative interaction between human albumin and proinflammatory cytokines IL-6 and TNFalpha. Artif Organs. 2016;40(4):397–402. doi:10.1111/aor.12557
25. Hirashima K, Watanabe M, Shigaki H, et al. Prognostic significance of the modified Glasgow prognostic score in elderly patients with gastric cancer. J Gastroenterol. 2014;49(6):1040–1046. doi:10.1007/s00535-013-0855-5
26. Kwag SJ, Kim JG, Kang WK, Lee J-K, Oh S-T. The nutritional risk is a independent factor for postoperative morbidity in surgery for colorectal cancer. Annals Surgi Treat Res. 2014;86(4):206–211. doi:10.4174/astr.2014.86.4.206
27. Geng Y, Qi Q, Sun M, Chen H, Wang P, Chen Z. Prognostic nutritional index predicts survival and correlates with systemic inflammatory response in advanced pancreatic cancer. Eur J surg oncol. 2015;41(11):1508–1514. doi:10.1016/j.ejso.2015.07.022
28. Migita K, Takayama T, Saeki K, et al. The prognostic nutritional index predicts long-term outcomes of gastric cancer patients independent of tumor stage. Ann Surg Oncol. 2013;20(8):2647–2654. doi:10.1245/s10434-013-2926-5
29. Wu SJ, Lin YX, Ye H, Li F-Y, Xiong X-Z, Cheng N-S. Lymphocyte to monocyte ratio and prognostic nutritional index predict survival outcomes of hepatitis B virus-associated hepatocellular carcinoma patients after curative hepatectomy. J Surg Oncol. 2016;114(2):202–210. doi:10.1002/jso.24297
30. Bozkaya Y, Erdem GU, Demirci NS, et al. Prognostic importance of the albumin to globulin ratio in metastatic gastric cancer patients. Curr Med Res Opin. 2019 Feb;35(2):275–282. doi: 10.1080/03007995.2018.1479683. Epub 2018 Jun 20.
31. Neal CP, Cairns V, Jones MJ, et al. Prognostic performance of inflammation-based prognostic indices in patients with resectable colorectal liver metastases. Medical Oncol. 2015;32(5):144. doi:10.1007/s12032-015-0590-2
32. Sun X, Liu X, Liu J, et al. Preoperative neutrophil-to-lymphocyte ratio plus platelet-to-lymphocyte ratio in predicting survival for patients with stage I–II gastric cancer. Chin J Cancer. 2016;35(1):57. doi:10.1186/s40880-016-0122-2
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.