Back to Journals » Therapeutics and Clinical Risk Management » Volume 12
Prognostic indicators for failed nonsurgical reduction of intussusception
Authors Khorana J , Singhavejsakul J, Ukarapol N, Laohapensang M, Siriwongmongkol J, Patumanond J
Received 10 April 2016
Accepted for publication 17 June 2016
Published 9 August 2016 Volume 2016:12 Pages 1231—1237
DOI https://doi.org/10.2147/TCRM.S109785
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Jiraporn Khorana,1 Jesda Singhavejsakul,1 Nuthapong Ukarapol,2 Mongkol Laohapensang,3 Jakraphan Siriwongmongkol,1 Jayanton Patumanond4
1Division of Pediatric Surgery, Department of Surgery, 2Division of Gastroenterology, Department of Pediatrics, Chiang Mai University Hospital, Chiang Mai, 3Division of Pediatric Surgery, Department of Surgery, Siriraj Hospital, Mahidol University, Bangkok, 4Center of Excellence in Applied Epidemiology, Thammasat University Hospital, Pathumthani, Thailand
Purpose: To identify the risk factors for failure of nonsurgical reduction of intussusception.
Methods: Data from intussusception patients who were treated with nonsurgical reduction in Chiang Mai University Hospital and Siriraj Hospital between January 2006 and December 2012 were collected. Patients aged 0–15 years and without contraindications (peritonitis, abdominal X-ray signs of perforation, and/or hemodynamic instability) were included for nonsurgical reduction. The success and failure groups were divided according to the results of the reduction. Prognostic indicators for failed reduction were identified by using generalized linear model for exponential risk regression. The risk ratio (RR) was used to report each factor.
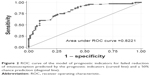
Results: One hundred and ninety cases of intussusception were enrolled. Twenty cases were excluded due to contraindications. A total of 170 cases of intussusception were included for the final analysis. The significant risk factors for reduction failure clustered by an age of 3 years were weight <12 kg (RR =1.48, P=0.004), symptom duration >3 days (RR =1.26, P<0.001), vomiting (RR =1.63, P<0.001), rectal bleeding (RR =1.50, P<0.001), abdominal distension (RR =1.60, P=0.003), temperature >37.8°C (RR =1.51, P<0.001), palpable abdominal mass (RR =1.26, P<0.001), location of mass (left over right side) (RR =1.48, P<0.001), poor prognostic signs on ultrasound scans (RR =1.35, P<0.001), and method of reduction (hydrostatic over pneumatic) (RR =1.34, P=0.023). The prediction ability of this model was 82.21% as assessed from the area under the receiver operating characteristic curve.
Conclusion: The identified prognostic factors for the nonsurgical reduction failure may help to predict the reduction outcome and provide information to the parents.
Keywords: intussusception, pneumatic reduction, hydrostatic reduction, prognostic indicators, failure rate
Introduction
Intussusception is a frequent cause of bowel obstruction in infants and preschool children. Its incidence has been found to be one to four per 2,000 infants and children worldwide.1 Intussusception is defined as the invagination of one segment of intestine into a segment of distal intestine. The diagnosis of intussusception is done according to the Brighton Collaboration Intussusception Working Group criteria.2 Treatment includes both nonsurgical and surgical procedures; the two methods of nonsurgical reduction are hydrostatic and pneumatic. Nonsurgical reduction can be done safely if there are no contraindications. Absolute contraindications such as peritonitis, perforation, and dehydration lead to nonresponsive shock.3 Surgical treatment is necessary in cases with contraindications or failed nonsurgical reduction.
Nonsurgical reduction failure is defined as intussusception that could not be reduced nonoperatively. The timeout limit of nonoperative reduction is defined in the “Materials and methods” section. The success rate of the nonsurgical reduction has been found to range from 46% to 94%.4 In our previous series, a study on the enema reduction of intussusception was found to have an overall success rate of 55.3% which was quite low compared with the other studies in the same series.5 So, this study was conducted to identify the causes of reduction failure. Many factors influence failed reductions. The duration of symptoms, emesis, bloody stool, poor prognosis sign on ultrasound scans (a thick peripheral hypoechoic rim, free intraperitoneum fluid, fluid trapped within intussusceptum, enlarged lymph node in intussusception, pathologic leading point, and absence of blood flow in the intussusception),1 and age group6 were found to be associated with failed reduction in the previous study.7 We aimed to predict the determinants of nonsurgical reduction failure.
Materials and methods
This retrospective cohort study was approved by the Ethics Committee of Chiang Mai University Hospital (CMU) and Siriraj Hospital (SI). According to the retrospective study, the Ethical committees of CMU and SI did not require patient consent. This study was a part of a series of studies on intussusception. Data from intussusception patients (International Classification of Diseases, Tenth Edition, code K56.1) who were treated with nonsurgical reduction in CMU and SI between January 2006 and December 2012 were collected. The inclusion criterion included the presence of intussusception, an age of 0–15 years, and the absence of contraindications for nonsurgical reduction. Absolute contraindications were peritonitis, abdominal X-ray signs of perforation, and/or hemodynamic instability. The chart and electronic database reviews were conducted to collect information on demographics, symptoms, signs, and investigations (sex, age, bodyweight, vomiting, abdominal pain, rectal bleeding, diarrhea, distention, constipation, duration of symptoms, temperature, palpable mass, location of the mass, white blood cell counts, neutrophils, electrolytes, abdominal radiography, and ultrasound findings). Specific radiographic findings included small bowel obstruction. Poor prognostic signs on ultrasound scans were counted if one of the signs mentioned was present. The patients were divided into a success group and a failure group according to the results of the nonsurgical reduction.
The standard nonsurgical reduction technique was performed in the patients who had no contraindications. The pneumatic reduction was performed by a radiologist under fluoroscopic guidance (in CMU) or by a pediatric surgeon under ultrasound guidance (in SI). The barium reduction was done by radiologist under fluoroscopic guidance (in SI). After resuscitation of the infants or children, nonsurgical reduction was done. In pneumatic reduction, we used the pressure enema from 80 to 120 mmHg with three attempts of 3 minutes each. In barium reduction, we controlled the pressure enema by limiting the height of the barium bucket to not >3 ft above buttocks with three attempts of 3 minutes each. We sedated the patients as appropriate. Failed reduction was defined by a remaining intussusception mass where barium or air could not pass from the cecum to the ileum through the ileocecal valve after the reduction procedure.8
Statistical analysis was done with commercial statistical software (STATA 11.0; StataCorp LP, College Station, TX, USA). The descriptive data were reported in count and percent for categorical data, and mean and standard deviation or median and interquartile range for continuous data. The univariable analysis was done by Fisher’s exact test for categorical data and Student’s t-test or Mann–Whitney U-test for continuous data. The multivariable regression analysis of the prognostic factors for intussusception reduction failure was done by generalized linear model for exponential risk regression, and reported by risk ratio (RR) clustered by an age of 3 years (due to the risk for pathologic leading point).9 The receiver operating characteristic curve was plotted for assessing the performance of the multivariable model. The statistical significance level was set as two-tailed with a P-value <0.05.
Results
One hundred and seventy intussusception patients in CMU and SI received nonsurgical reduction. The overall failure rate was 44.7% (Figure 1). The factors that influenced the failure of nonsurgical reduction were analyzed by the univariable analysis (Tables 1 and 2) and multivariable analysis (Table 3). In the univariable model, the significant factors for failure of the reduction of intussusception analyzed were age, bodyweight, vomiting, rectal bleeding, abdominal distension, constipation, temperature, location of mass, serum sodium, small bowel obstruction in the abdominal radiography, and method of reduction (P-value for each parameter are stated in Tables 1 and 2). After multivariable analysis was done, we found that the significant risk factors for failure reduction clustered by an age of 3 years were weight <12 kg (RR =1.48, P=0.004), symptom duration >3 days (RR =1.26, P<0.001), vomiting (RR =1.63, P<0.001), rectal bleeding (RR =1.50, P<0.001), abdominal distension (RR =1.60, P=0.003), temperature >37.8°C (RR =1.51, P<0.001), palpable abdominal mass (RR =1.26, P<0.001), location of mass (left over right side) (RR =1.48, P<0.001), poor prognostic signs on ultrasound scans (RR =1.35, P<0.001), and method of reduction (hydrostatic over pneumatic) (RR =1.34, P=0.023). The receiver operating characteristic curve was plotted to assess the prediction ability of this model of the described risk factors for the failed reduction as shown in Figure 2. An area under curve of 82.21% was obtained.
  | Figure 1 Flow of the study. |
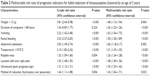  | Table 3 Multivariable risk ratio of prognostic indicators for failed reduction of intussusception clustered by an age of 3 years |
Nonsurgical reductions failed in 76 patients. All those patients were operated. The operative findings of the intussusception patients with failed nonoperative reduction are shown in Figure 3. A pathologic finding of resection and anastomosis group was the necrosis of the bowel. The pathologic leading points were found in six patients. The pathologic leading points reported were jejunal polyp, B-cell lymphoma, ileal diverticulitis, and Meckel’s diverticulum (in two patients).
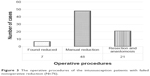  | Figure 3 The operative procedures of the intussusception patients with failed nonoperative reduction (N=76). |
Discussion
This study was the second in a series of studies on intussusception conducted in our two institutions. The first study explored the success rate of the pneumatic and hydrostatic reduction. We found that the success rate of nonsurgical reduction was 55.3%.5 So, this study was set to identify the factors that lead to failed reduction.
The significant risk factors identified in our study were weight <12 kg, symptom duration >3 days, vomiting, rectal bleeding, abdominal distension, temperature >37.8°C, palpable abdominal mass, location of mass (left over right side), poor prognostic signs on ultrasound scans, and method of reduction (hydrostatic over pneumatic).
The duration of symptoms associated with failed reduction remains controversial. In previous studies, different results were obtained regarding this issue. Reijnen et al stated that a duration of symptoms of >48 hours was a significant predictor of failure of hydrostatic reduction.10 Chung et al studied about the risk factors leading to surgical reduction and found that the long-standing duration of illness (>24 hours) was a primary factor. In that series, the intussusception was diagnosed within 48 hours in most of the cases.11 Okuyama et al concluded that barium enema reduction was safe and effective regardless of the duration of the disease.12 Also, in a study conducted in a tertiary referral center in Hong Kong, Wong et al found that a mean duration of symptoms of 2.3 days did not affect success rate of the reduction.13 Yao et al conducted a study on 316 operated intussusception patients with failed nonoperative reduction. In that study, the median duration of symptoms in the overall patients, group with an unviable intestine, and group with a viable intestine was 23, 42, and 19 hours, respectively, and this result was significantly different.14 Long duration of symptoms before presentation related to increase in the loss of intestinal viability. So, the duration of symptoms was not a contraindication for the nonoperative reduction, and some cases with a long symptom duration (minimum =1 hour and maximum =120 hours in success group) in our study had successful reduction. So, the presence of intestinal viability is an important risk factor associated with failed reduction. In this study, we found that duration of symptoms >72 hours before presentation was one of the predictors of failed nonoperative reduction.
None of the reviewed literature mentioned about the patient’s weight as a risk factor for failed reduction, while most of the studies mentioned about the age of patients. Fallon et al15 and Tota-Maharaj et al16 found that an age <1 year was significantly associated with failed reduction. In our study, we used the age for clustering the risk factors because the risk of pathologic leading point was higher in the children aged >3 years and might not be comparable. So, we used weight as a predictor and found that weight <12 kg was significantly associated with failed reduction. This result may be contributed to the small caliber of the small bowel of the small children. So, the intussusception was difficult to reduce.
Abdominal pain and vomiting are the two classic symptoms of intussusception. From the previous study, vomiting was found to be a symptom helpful in the diagnosis of intussusception but not a statistical significant predictor of failed reduction as found in our study.
Rectal bleeding and abdominal mass are the two classic signs of intussusception. He et al found that rectal bleeding was a predictor of failed reduction as in our study.7 Palpable abdominal mass was also a significant factor associated with failed reduction in our study and in the study of Wong et al.13 Regarding the location of the mass, He et al also found that the intussusception located on the left side of the abdomen was significantly associated with a lower success rate of reduction. Flaum et al found that ileocecal and ascending colon localization was associated with successful reduction.17 In our study, a mass located on the left side of abdomen was significantly associated with failed reduction. Most cases of intussusception were of ileocolic type. The location of the mass represents the length of intussusception. The length of intussusception was not mentioned in the previous study as a predictor, but some studies on small bowel intussusception used the length of intussusception to differentiate the transient intussusception and to surgically manage small bowel intussusception. Actually, an intussusception of 2 cm diameter without clinical signs that could be spontaneously reduced is the transient intussusception.1 Rajagopal et al studied about the transient and surgically managed small bowel intussusception and found that transient intussusception was associated with a shorter length of intussusception, smaller transverse diameter, thin walls, absence of the leading point, and visible peristalsis. The mean length of the transient intussusception in that study was 2.25 cm.18
In 2008, Ramachandan found that small bowel obstruction was one of the risk factors for failed reduction.19 In our study, the plain abdominal X-ray showed that small bowel obstruction was significantly associated with failed reduction in univariable analysis but not in multivariable analysis. Therefore, we found that abdominal distension was associated with reduction failure.
Fever in the previous study was considered as a risk factor for bowel resection as reported by Fike et al.20 However, a temperature >37.8°C was one of the predictors of failed reduction in our study. That might be a systemic response to intraabdominal infection and inflammation. The blood supply to intussusception might be compromised and associated with the lower success rate of reduction.
The poor prognosis signs on ultrasound scans were reported to be associated with the successful reduction in many studies. He et al also reported the presence of peritoneal fluid and trapped fluid in the intussusception as the predictors as found in our study.
In our previous series of intussusception, we studied about the method of reduction and found that the success rate of pneumatic reduction was 1.48 times more than hydrostatic reduction.5 Sanchez et al found that the reduction under ultrasonography and fluoroscopy was equally effective.21 Sadigh et al conducted a meta-analysis on air-versus-liquid enema of intussusception and found that air enema was superior to liquid enema with lower complication.22 So, the method of reduction was considered to be one of the predictors in our study.
Among the 76 cases who were operated, we found reduction in only four cases. Those cases with reduction were reviewed based on the technique of reduction and the adequacy of the sedation. In 2010, Tota-Maharaj used sedation as one of the risk factors for failed reduction. The rest of the operative cases were operated with manual reduction or bowel resection depending on the viability of the intestine.
In our series, we found eight patients (4.7%) with recurrent intussusception. Three episodes of recurrent intussusception were found in one case, and two episodes in another. The nonoperative reduction was successful in seven cases, and manual reduction was done in failed case without pathologic leading point. The recurrence rate of intussusception was up to 20% with an average of 5% in the literature.1 Gray et al presented a meta-analysis of the recurrence rate of nonoperative reduction. They found that the recurrence rates were 12.7% for contrast enema, 7.5% for ultrasound-guided noncontrast enema, and 8.5% for fluoroscopy-guided air enema.23
Bratton et al studied about hospital size and found that nonsurgical reduction was more likely to succeed in large hospitals with a larger caseload.24 In contrast, in this study, we found that duration of symptoms was significantly associated with failed reduction. In our centers, we received the cases from the referral hospital with no pediatric surgeon. So, the duration of symptoms of cases in our study was longer than the previous studies. The median duration of symptoms before presentation in our study was 34.8 hours which was also mentioned in our first series. We also performed nonsurgical reduction safely if the contraindications were not present.
Guo et al reviewed a large series of studies on intussusception which used air enema for reduction.25 They established a clinical criteria scoring system for intussusception by procedure used, duration of onset, age, stool characteristics, coexistent diarrhea, abdominal distension, and dehydration to predict the success rate. No other study proposed about the prediction factors for the successful intussusception reduction. In this study, we identified the significant risk factors associated with failed reduction. The information about prognosis of the nonoperative reduction could be provided to the referral hospital and parents. However, this was a retrospective study which was a limitation.
Conclusion
Many factors that can significantly predict the failure of nonsurgical reduction were found which included bodyweight <12 kg, symptoms duration >3 days, vomiting, rectal bleeding, abdominal distension, temperature >37.8°C, palpable abdominal mass, location of mass on the left side, poor prognostic signs on ultrasound scans, and method of reduction (hydrostatic over pneumatic). The contraindications for the nonsurgical reduction were peritonitis, free air in abdominal radiography, and nonresponsive shock. This study aimed to identify the risk factors for failure reduction, and in the next study, we will investigate the scoring system for the prediction of the failure of the reduction of intussusception.
Disclosure
The authors report no conflicts of interest in this work.
References
Columbani PM, Scholz S. Intussusception. In: Coran AG, Adzick NS, Krummel TM, Laberge J-M, Shamberger RC, Caldamone AA, editors. Pediatric Surgery. Vol 2. 7th ed. Philadelphia, PA: Saunders; 2012:1093–1110. | ||
Bines JE, Kohl KS, Forster J, et al. Acute intussusception in infants and children as an adverse event following immunization: case definition and guidelines of data collection, analysis, and presentation. Vaccine. 2004;22(5–6):569–574. | ||
Hannon EJ, Allan RA, Negus AS, Murphy F, Okoye BO. Air enema reduction of intussusception: a registrar-led, protocol-driven service is safe and effective. Pediatr Surg Int. 2013;29(8):805–809. | ||
Bekdash B, Marven SS, Sprigg A. Reduction of intussusception: defining a better index of successful non-operative treatment. Pediatr Radiol. 2013;43(6):649–656. | ||
Khorana J, Singhavejsakul J, Ukarapol N, Laohapensang M, Wakhanrittee J, Patumanond J. Enema reduction of intussusception: the success rate of hydrostatic and pneumatic reduction. Ther Clin Risk Manag. 2015;11:1837–1842. | ||
Ogundoyin O, Lawal T, Olulana D, Atalabi O. Experience with Sonogram-guided hydrostatic reduction of intussusception in children in South-West Nigeria. J West Afr Coll Surg. 2013;3(2):76–88. | ||
He N, Zhang S, Ye X, Zhu X, Zhao Z, Sui X. Risk factors associated with failed sonographically guided saline hydrostatic intussusception reduction in children. J Ultrasound Med. 2014;33(9):1669–1675. | ||
Puri P, Hollwarth ME. Pediatric Surgery Diagnosis and Management. Berlin: Springer; 2009. | ||
Banapour P, Sydorak RM, Shaul D. Surgical approach to intussusception in older children: influence of lead points. J Pediatr Surg. 2015;50(4):647–650. | ||
Reijnen JA, Festen C, van Roosmalen RP. Intussusception: factors related to treatment. Arch Dis Child. 1990;65(8):871–873. | ||
Chung JL, Kong MS, Lin JN, Wang KL, Lou CC, Wong HF. Intussusception in infants and children: risk factors leading to surgical reduction. J Formos Med Assoc. 1994;93(6):481–485. | ||
Okuyama H, Nakai H, Okada A. Is barium enema reduction safe and effective in patients with a long duration of intussusception? Pediatr Surg Int. 1999;15(2):105–107. | ||
Wong CW, Chan IH, Chung PH, et al. Childhood intussusception: 17-year experience at a tertiary referral centre in Hong Kong. Hong Kong Med J. 2015;21(6):518–523. | ||
Yao XM, Chen ZL, Shen DL, et al. Risk factors for pediatric intussusception complicated by loss of intestine viability in China from June 2009 to May 2014: a retrospective study. Pediatr Surg Int. 2015;31(2):163–166. | ||
Fallon SC, Lopez ME, Zhang W, et al. Risk factors for surgery in pediatric intussusception in the era of pneumatic reduction. J Pediatr Surg. 2013;48(5):1032–1036. | ||
Tota-Maharaj R, Rampersad B, Indalsingh R. Barium enema reduction of intussusception in a developing country. West Indian Med J. 2010;59(5):535–539. | ||
Flaum V, Schneider A, Gomes Ferreira C, et al. Twenty years’ experience for reduction of ileocolic intussusceptions by saline enema under sonography control. J Pediatr Surg. 2016;51(1):179–182. | ||
Rajagopal R, Mishra N, Yadav N, Jhanwar V, Thakur A, Mannan N. Transient versus surgically managed small bowel intussusception in children: role of ultrasound. Afr J Paediatr Surg. 2015;12(2):140–142. | ||
Ramachandran P, Gupta A, Vincent P, Sridharan S. Air enema for intussusception: is predicting the outcome important? Pediatr Surg Int. 2008;24(3):311–313. | ||
Fike FB, Mortellaro VE, Holcomb GW 3rd, St Peter SD. Predictors of failed enema reduction in childhood intussusception. J Pediatr Surg. 2012;47(5):925–927. | ||
Sanchez TR, Doskocil B, Stein-Wexler R. Nonsurgical management of childhood intussusception: retrospective comparison between sonographic and fluoroscopic guidance. J Ultrasound Med. 2015;34(1):59–63. | ||
Sadigh G, Zou KH, Razavi SA, Khan R, Applegate KE. Meta-analysis of air versus liquid enema for intussusception reduction in children. AJR Am J Roentgenol. 2015;205(5):W542–W549. | ||
Gray MP, Li SH, Hoffmann RG, Gorelick MH. Recurrence rates after intussusception enema reduction: a meta-analysis. Pediatrics. 2014;134(1):110–119. | ||
Bratton SL, Haberkern CM, Waldhausen JH, Sawin RS, Allison JW. Intussusception: hospital size and risk of surgery. Pediatrics. 2001;107(2):299–303. | ||
Guo JZ, Ma XY, Zhou QH. Results of air pressure enema reduction of intussusception: 6,396 cases in 13 years. J Pediatr Surg. 1986;21(12):1201–1203. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.