Back to Journals » Therapeutics and Clinical Risk Management » Volume 13
Prognostic impact of blood pressure and heart rate at admission on in-hospital mortality after primary percutaneous intervention for acute myocardial infarction with ST-segment elevation in western Romania
Authors Bordejevic DA , Caruntu F, Mornos C, Olariu I, Petrescu L, Tomescu MC , Citu I , Mavrea A , Pescariu S
Received 8 May 2017
Accepted for publication 31 July 2017
Published 23 August 2017 Volume 2017:13 Pages 1061—1068
DOI https://doi.org/10.2147/TCRM.S141312
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Diana Aurora Bordejevic,1,* Florina Caruntu,1,* Cristian Mornos,2 Ioan Olariu,2 Lucian Petrescu,2 Mirela Cleopatra Tomescu,1 Ioana Citu,1 Adelina Mavrea,1 Sorin Pescariu2
1Internal Medicine Department, 2Cardiology Department, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania
*These authors contributed equally to this work
Background: The purpose of this retrospective study was to evaluate the prognostic impact of systolic blood pressure (SBP) and heart rate (HR) on in-hospital mortality in ST-segment elevation acute myocardial infarction (STEMI) patients, after primary percutaneous intervention (PCI).
Patients and methods: The study included 294 patients admitted for STEMI. They were divided into five groups according to the SBP at admission: group I, <105 mmHg; group II, 105–125 mmHg; group III, 126–140 mmHg; group IV, 141–158 mmHg; and group V, ≥159 mmHg. Increased HR was defined as ≥80 beats per minute (bpm). In-hospital death was defined as all-cause death during admission and classified into cardiac and noncardiac death.
Results: Among the 294 patients admitted for STEMI, 218 (74%) were men. The mean age was 62±17 years. In-hospital mortality rate was 6% (n=18), with 11 (3.7%) deaths having cardiac causes. The highest mortality was registered in group I (n=9, 16%, P=0.018). Compared to the other groups, group I patients were older (P=0.033), more often smokers (P=0.026), and had a history of myocardial infarction (P=0.003), systemic hypertension (P=0.023), diabetes (P=0.041), or chronic kidney disease (P=0.0200). They more often had a HR ≥80 bpm (P=0.028) and a Killip class 3 or 4 at admission (P=0.020). The peak creatine phosphokinase-MB level was significantly higher in this group (P=0.005), while the angiographic findings more often identified as culprit lesions were the right coronary artery (P=0.005), the left main trunk (P=0.040), or a multivessel coronary artery disease (P=0.044). Multivariate analysis showed that group I patients had a significantly higher risk for both all-cause death (P=0.006) and cardiac death (P=0.003). Patients with HR ≥80 bpm also had higher mortality rates (P=0.0272 for general mortality and P=0.0280 for cardiac mortality).
Conclusion: The present study suggests that SBP <105 mmHg and HR ≥80 bpm at admission of STEMI patients are associated with a higher risk of in-hospital death, even after primary PCI.
Keywords: blood pressure, heart rate, STEMI, primary PCI, outcome
Introduction
In Romania, cardiovascular diseases account for 63% of all deaths, while in Europe the percentage is 37%.1 Acute myocardial infarction (AMI) is by far the leading cause of death in patients with ischemic heart disease. In our country, ~13,000 people annually suffer from AMI, with mortality rates reaching worrying levels. The risk of death is maximum within the first 2 hours of onset of the disease. According to the data from some studies, 52% of deaths occur before the patient reaches the hospital. The mortality rate drops dramatically after admission: 19% in the first 24 hours and only 8% on the second day. Finally, 21% of deaths occur later, up to 30 days.1
Studies published over the past 20 years have undoubtedly demonstrated that early coronary reperfusion significantly reduces mortality, reduces the infarct area, and leads to a better preservation of contractile heart function.6 Furthermore, reperfusion significantly reduces the risk of ventricular fibrillation. A prompt intervention in these patients, according to existing resuscitation protocols (basic support and advanced support of life), triple their survival chances and can reduce the risk of developing post-resuscitation neurological sequel by more than 50%.2
Over the past decade, in-patient treatment of patients with myocardial infarction has improved substantially as a result of the efforts made by the Romanian Society of Cardiology to implement progress in the field, in line with international guidelines. For prehospital quantification of the prognostic risk of patients with AMI, the parameters that can be quantified during the first medical consultation are very useful and are routinely included in the medical examination: heart rate (HR) and blood pressure (BP).
The Global Registry of Acute Coronary (GRACE) score is appropriate for use in both ST-segment elevation myocardial infarction (STEMI) and non-STEMI patients, but it requires a calculator, an electrocardiogram, cardiac biomarkers, and serum creatinine levels, which may not be available at the first medical contact.3 The thrombolysis in myocardial infarction score is easier to calculate than the GRACE score, but it also requires access to the cardiac biomarkers and an electrocardiogram.4
The present study aims to investigate the prognostic impact of BP and HR at admission on intrahospital prognosis of STEMI patients treated with primary percutaneous coronary intervention (PCI).
Patients and methods
Patient selection
Between January and April 2017, 326 patients with STEMI were admitted to the Cardiology Clinic of the Timisoara Institute of Cardio-Vascular Diseases. The hospitalization was done within the first 12 hours of the onset of the symptoms. Among them, 294 patients underwent primary PCI and were included in this study.
BP at admission was defined as the first BP, measured in a sitting or dorsal position, in the emergency room. Depending on systolic blood pressure (SBP) at admission, patients were classified into five groups: group I, with SBP ≤105 mmHg; group II, with SBP 105–125 mmHg; group III, with SBP 126–140 mmHg; group IV, with SBP 141–158 mmHg; and group V, with SBP ≥159 mmHg.
HR at admission was defined as the first HR determined in the hospital emergency room, in sitting or in “decubitus.” Increased HR was defined as values ≥80 beats per minute (bpm). We used the cutoff value of 80 bpm to define increased HR, as in clinical studies with STEMI patients undergoing primary PCI, an elevated HR (80 bpm or greater) identified those at increased risk of death.5
The diagnosis of STEMI was based on the presence of at least two of the following three criteria: 1) typical angina with duration of >20 minutes; 2) the presence of ST-segment elevation ≥1 mV, with duration >0.08 seconds measured from point J, in at least two adjacent leads; 3) transient increase in cardiac enzymes to at least twice the normal laboratory value.2
The study protocol was approved by the ethics commission of Timisoara Institute of Cardiovascular Diseases. Before enrollment, all patients signed the informed consent for participation in the study, according to Human Rights Declaration of Helsinki.
Data extraction
Baseline data were extracted from hospital records and included age, gender, cardiovascular history, and risk factors, such as known ischemic heart disease, old MI, systemic hypertension, smoking, diabetes mellitus, hypercholesterolemia, and chronic kidney disease.
Definition of covariates
Hypertension has been defined as systemic BP ≥140/90 mmHg or the use of antihypertensive agents.6
Hypercholesterolemia was defined as total cholesterol ≥190 mg/dL or the use of cholesterol-lowering medication.7
Diabetes mellitus was defined as fasting blood glucose ≥126 mg/dL or the use of antidiabetic treatment.8
Chronic kidney disease was defined in the presence of a glomerular filtration rate <60 mL/min/1.73 m2 body surface area, calculated using the Modification of Diet in Renal Disease (MDRD) Study Group equation.9
We used the classification of heart failure severity in patients with AMI proposed by Killip as following: class 1, with no clinical signs of heart failure; class 2, with rales in the lungs, third heart sound, and elevated jugular venous pressure; class 3, with acute pulmonary edema; and class 4, with cardiogenic shock or arterial hypotension (measured as SBP <90 mmHg) and evidence of peripheral vasoconstriction (oliguria, cyanosis, and diaphoresis).10
Primary PCI
Primary PCI was performed as a matter of urgency according to standard procedures. Significant coronary stenosis was defined in the presence of a reduction in internal diameter of at least 75% in the anterior descending, circumferential, or right coronary artery and at least 50% in the left coronary artery. Multivessel coronary artery disease (CAD) was defined in the presence of significant stenosis in several coronary arteries. After coronary angiography, percutaneous coronary angioplasty was performed in 294 patients.
Follow-up and outcomes
The primary end point was in-hospital mortality, defined as death of any cause during the admission for STEMI.
Cardiac deaths were considered as those occurring due to cardiogenic shock, acute pulmonary edema, cardiac rupture, or ventricular fibrillation.
Noncardiac deaths were defined as deaths having an extracardiac cause, such as stroke, acute renal failure, or sepsis.
Statistical analysis
The statistical analysis was performed using MedCalc Statistical Software version 12.7.7 (Ostend, Belgium). Continuous variables are presented as mean ± standard deviation (SD) and categorical variables as number (n) and percentage (%). The five patient groups were compared using the chi-square test for the categorical variables and the independent t-test for the continuous ones. Relative risk (RR) and confidence interval (CI) of 95% of various parameters, related to intrahospital death, were estimated by univariate analysis. Parameters with statistically significant risk in univariate analysis were included in the multivariate analysis by logistic regression. For the independent predictors identified by multivariate logistical regression, receiver operating characteristic (ROC) analysis was performed. Values of P<0.05 were considered statistically significant.
Results
Baseline characteristics
Of the 294 patients with STEMI subjected to primary PCI, 218 (74%) were men. The average age was 62±17 years (33–95 years). The distribution by age group of patients with STEMI is shown in Figure 1.
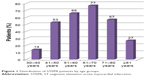  | Figure 1 Distribution of STEMI patients by age groups. |
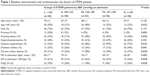
According to the SBP at admission, STEMI patients were divided into five groups. The baseline characteristics and cardiovascular history and risk factors among the five patient groups are presented in Table 1. Compared to the other groups, group I patients (with SBP <105 mmHg at admission) were more often elderly (P=0.033), smokers (P=0.026), with a history of old MI (P=0.003), systemic hypertension (P=0.023), diabetes (P=0.041), or chronic kidney disease (P=0.0200). They had more often a HR ≥80 bpm (P=0.028) and a Killip class 3 or 4 at admission (P=0.020). Group V patients, with SBP ≥159 mmHg at admission, were more frequently hypertensive and diabetic.
Angiographic data
Table 2 presents the results of the emergency coronarography and the peak values of creatine phosphokinase (CPK)-MB. For patients in group I, the most common lesions responsible for the AMI were located in the right coronary artery, the left coronary artery trunk, or on more than two vessels, and the peak CPK-MB values were significantly higher.
In-hospital mortality
During the hospitalization, 18 deaths (6%) occurred, 11 of them having a cardiac cause (3.7%) and the other seven having noncardiac causes (3.3%), as presented in Table 3.
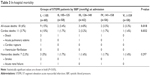  | Table 3 In-hospital mortality |
The patients in group I (n=60) had an intrahospital mortality rate of 15%, significantly higher than the rest of the groups (P=0.018). Between the other groups, the differences in mortality rates were not significant.
Cardiac deaths occurred significantly more frequently in group I (P=0.032), whereas noncardiac events had a similar distribution in the five groups.
In patients who had SBP <105 mmHg at admission, the RR of death due to any cause was 4.9 (95% CI 1.977–12.205, P=0.006), and the RR of cardiac death was 5.4 (95% CI 1.723–17.249, P=0.003; Table 3).
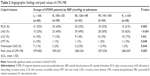
HR ≥80 bpm is another predictive parameter of the increased risk of death in patients with STEMI, as outlined in Table 4.
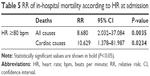
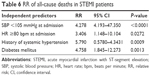
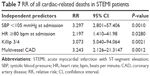
The multivariate logistic regression analysis selected those variables with independent predictive power for the risk of intrahospital death. These independent variables are highlighted in Tables 5–7.
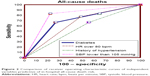
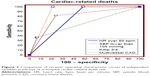
We compared the predictive power of the selected independent variables using the ROC curves, analyzing the area under the curve (AUC). The graphs representing the ROC curves are shown in Figures 2 and 3.
Regarding the risk of death in post-PCI STEMI patients, the best predictor was SBP ≤105 mmHg (AUC =0.804, 95% CI 0.712–0.896, P<0.0001), followed by diabetes mellitus (AUC =0.697, 95% CI 0.582–0.813, P=0.0013), HR ≥80 bpm (AUC =0.664, 95% CI 0.541–0.747, P=0.0272), and history of hypertension (AUC =0.554, 95% CI 0.439–0.670, P=0.0009).
Significant differences between areas under the ROC curves, which indicate significant differences between predictive capacities, were also observed for diabetes mellitus and history of hypertension (0.143, 95% CI 0.0033–0.283, P=0.044).
In the case of post-PCI STEMI cardiac death risk, the strongest predictor was Killip class ≥3 at admission (AUC =0.896, 95% CI 0.872–0.919, P=0.0429), followed by SBP ≤105 mmHg (AUC =0.791, 95% CI 0.669–0.913, P=0.0057), HR ≥80 bpm (AUC =0.756, 95% CI 0.727–0.785, P=0.0023), and multivascular CAD (AUC =0.648, 95% CI 0.498–0.798, P=0.0015).
Significant differences between the areas under the ROC curves were observed for HR ≥80 bpm versus the Killip class ≥3 (0.140, 95% CI 0.106–0.173, P<0.0001) and for the Killip class ≥3 versus multivessel CAD (0.248, 95% CI 0.0955–0.399, P=0.0014).
Discussion
Early post-AMI mortality is an important indicator of hospital and health performance. Therefore, the efficacy of the AMI treatment has been studied in several randomized trials, but with several limitations. Thus, a study involving STEMI patients in 12 European countries reported an increased use of primary PCI but pointed out that there are considerable differences between states.11 A number of regional differences related to the organization of the health system, procedures, and health programs, and which are associated with prognosis, were not included in the evaluation.12,13 International studies on AMI cannot have a unitary vision based on the selected data from hospitals and those reported in national registers. There are also no unitary criteria for assessing mortality.
Our retrospective study is the first study in Romania addressing the prognostic impact of HR and SBP at admission on STEMI patients undergoing primary PCI. The results show that these easily determinable clinical parameters are independent predictors of intrahospital mortality.
BP is the measured result of the interactions between numerous and complex factors that control blood vessel size, as well as their response to neurohormonal stimuli and cardiac output. Neurohormonal stimuli can induce hypertension by increasing systolic flow and/or peripheral vascular resistance. There is much evidence that a sustained increase in BP is, at any age, an independent factor of cardiovascular risk.14
The predictive value of HR for CAD mortality risk is higher in hypertensive than in normotensive patients. There is evidence that hypertensive patients with HR >80 bpm have a higher risk than those with HR <60 bpm.15 Therefore, HR has a major role in the occurrence and maintenance of hypertension. Increased HR at rest is associated with an increased risk of total and cardiovascular mortality, regardless of age, race, sex, presence of diabetes, or cardiovascular disease.16
The first major evaluation of HR in relation to classical cardiovascular risk factors, including hypertension, was conducted by a study in France. Subjects with HR ≥85 bpm had a SBP 12 mmHg higher and a diastolic BP 7 mmHg higher when compared to those with HR <65 bpm.17
The Chicago epidemiological study demonstrated a clear association between hypertension and HR, this association being more important for SBP.18
Increased HR is associated with endothelial dysfunction, accelerated atherosclerosis, and an increased risk of cardiovascular mortality, especially in the presence of acute coronary syndromes.19 In our study, the mean HR was 75±18 bpm in post-PCI STEMI survivors, 89±15 in the case of in-hospital deaths of all causes (P=0.0423), and 92±12 bpm in the patients with cardiac deaths (P=0.0021).
A HR ≥80 bpm increased 3.4 times the risk of in-hospital death of any cause (P=0.027) and doubled the risk of cardiac death (P=0.028). It proved to be an independent predictor of intrahospital mortality in STEMI patients who performed primary PCI. These results are concordant to those of the Goteborg study, which showed a threefold death risk in subjects with HR =90–99 bpm compared to those with HR ≤60 bpm.20
An even stronger predictor was SBP at admission. It had an average value of 136±24 mmHg for the entire group of STEMI patients. The mean SBP was 139±22 mmHg in survivors and 110±35 mmHg in those who died (P<0.0001). SBP at admission <105 mmHg increased 4.9 times the risk of all-cause death (P=0.0060) and 5.4 times the risk of cardiac death (P=0.0039).
A series of studies have shown that prognosis is better in patients with AMI who have a higher BP at admission.21–25 SBP is included in several acute coronary syndrome prognosis scores.26–32 SBP being the result of interaction between peripheral vascular resistance and cardiac output, a higher admission value reflects not only higher peripheral systemic resistance but also a better systolic ventricular function due to lower myocardial injury.
In our study, mortality was significantly higher in group I, which included STEMI patients with SBP <105 mmHg, compared to the other four subsets of SBP values. Patients in group I (n=60), with the highest mortality (15%), were more frequently elderly (≥65 years), with a history of MI and chronic kidney disease. They had admission HR ≥80 bpm, Killip classes ≥3, and high CPK values more often. Angiographic data in these patients revealed more frequently involvement of the left main trunk or multivessel CAD.
The lowest mortality (3.3%) was recorded in group V (SBP ≥159 mmHg), in which STEMI patients were younger, nonsmokers, and more often hypertensive and diabetic. They had lower CPK-MB values, and the culprit lesion was found more frequently on the left anterior descending coronary artery.
In group I, cardiac deaths were twice as common as noncardiac causes (10% vs 5%, P=0.3), whereas in group V, the two types of deaths had equal frequencies (1, 6%).
In our study, HR ≥80 bpm and SBP <105 mmHg were the only variables that predicted both all-cause and cardiac-related death risk in STEMI patients after primary PCI. Systemic hypertension and diabetes mellitus were independent predictors only for all-cause deaths, while Killip ≥3 class at admission and multivessel CAD were independent predictors for cardiac-related deaths.
Study limitations
This is a retrospective observational study conducted at a single hospital for a period of 4 months and included a relatively small number of patients, with a low number of in-hospital events. The study did not include data regarding prehospital and in-hospital treatment, ischemic time (from onset of symptoms to coronary angioplasty), left ventricular ejection fraction, major nonfatal cardiovascular events occurred during hospitalization, and mortality at 30 days and at 1 year.
Conclusion
Our study suggests that vital signs (HR and SBP) reported on admission of STEMI patients can provide valuable information on the risk of in-hospital death after primary PCI.
Thus, HR ≥80 bpm and SBP ≤105 mmHg correlate with an increased risk of death, while HR <80 bpm and SBP ≥159 mmHg are associated with a better prognosis.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Tatu-Chiţoiu G, Deleanu D, Petriş A, et al. The First Romanian Registry for ST-Elevation Myocardial Infarction (RO-STEMI) (1997–2009). Final Report. Amaltea Medical Publishing House; 2009. ISBN 978-973-162-068-8. | ||
ESC, Steg PG, James SK, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569–2619. | ||
Fox KA, Dabbous OH, Goldberg RJ, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ. 2006;333:1091. | ||
Morrow DA, Antman EM, Giugliano RP, et al. A simple risk index for rapid initial triage of patients with ST-elevation myocardial infarction: an In TIMI II substudy. Lancet. 2001;358:1571–1575. | ||
Parodi G, Bellandi B, Valenti R, et al. Heart rate as an independent prognostic risk factor in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. Atherosclerosis. 2010;211(1):255–259. | ||
Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension. Eur Heart J. 2013;34:2159–2219. | ||
Cohen JD, Cziraky MJ, Cai Q, et al. 30-year trends in serum lipids among United States adults: results from the National Health and Nutrition Examination Surveys II, III, and 1999–2006. Am J Cardiol. 2010;106:969–975. | ||
Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia. Available from: https://www.idf.Org/web data/docs/WHO_IDF_definition_diagnosis_of_diabetes.pdf | ||
Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. | ||
Kourosh S, Diana S, Hassan J, et al. Prediction of survival after myocardial infarction using Killip class. Int J Clin Med. 2012;3:563–568. | ||
Laut KG, Gale CP, Lash TL, Kristensen SD. Determinants and patterns of utilization of primary percutaneous coronary intervention across 12 European countries: 2003–2008. Int J Cardiol. 2013;168: 2745–2753. | ||
Curry LA, Spatz E, Cherlin E, et al. What distinguishes top-performing hospitals in acute myocardial infarction mortality rates? A qualitative study. Ann Intern Med. 2011;154:384–390. | ||
White HD, Chew DP. Acute myocardial infarction. Lancet. 2008;372:570–584. | ||
Guyton AC, Hail JE, Lohmeier TE, et al. Role of the kidney and volume control in the pathogenesis of hypertension. In Robertson JIS, editor. Handbook of Hypertension, Vol I: Clinical Aspects of Essential Hypertension. Amsterdam: Elsevier; 1983:216–238. | ||
Benetos A, Rudnichi A, Thomas F, et al. Influence of heart rate on mortality in a French population: role of age, gender and blood pressure. Hypertension. 1999;33:44–52. | ||
Julius S, Krause L, Schork N, et al. Hyperkinetic borderline hypertension in Techumseh, Michigan. J Hypertens. 1991;9:77–84. | ||
Morcet JF, Safar M, Thomas F, Guize L, Benetos A. Association between heart rate and other risk factors in a large French population. J Hypertension. 1999;17:1671–1676. | ||
Dyer AR, Perski V, Stamler J, et al. Heart rate as a prognostic factor for coronary heart disease and mortality: findings in three Chicago epidemiologic studies. Am J Epidemiol. 1980;112:736–749. | ||
Tendera M. Increased heart rate in chronic and acute coronary syndromes. Medicographia. 2002;3:189. | ||
Wilhelmsen L, Berglund G, Elmfeldt D, et al. The multifactor primary prevention trial in Göteborg, Sweden. Eur Heart J. 1986;7:279–288. | ||
Braunwald E, Antman EM, Beasley JW, et al. Committee on the Management of Patients with Unstable Angina. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction – summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina). J Am Coll Cardiol. 2002;40:1366–1374. | ||
Bertrand ME, Simoons ML, Fox KA, et al. Management of acute coronary syndromes: acute coronary syndromes without persistent ST segment elevation; recommendations of the Task Force of the European Society of Cardiology. Eur Heart J. 2002;21:1406–1432. | ||
Gheorghiade M, Abraham WT, Albert NM, et al; OPTIMIZE-HF Investigators and Coordinators. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006;296:2217–2226. | ||
Pitsavos C, Panagiotakos D, Zombolos S, et al; Greek Study of Acute Coronary Syndromes (GREECS) Investigators Group. Systolic blood pressure on admission predicts in-hospital mortality among patients presenting with acute coronary syndromes: the Greek study of acute coronary syndromes. J Clin Hypertens. 2008;10:362–366. | ||
Shiraishi J, Kohno Y, Sawada T, et al. Systolic blood pressure at admission, clinical manifestations, and in-hospital outcomes in patients with acute myocardial infarction. J Cardiol. 2011;58:54–60. | ||
The GRACE Investigators. Rationale and design of the GRACE (Global Registry of Acute Coronary Events) Project: a multinational registry of patients hospitalized with acute coronary syndromes. Am Heart J. 2001;141:190–199. | ||
The GUSTO Investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N Engl J Med. 1993;329:673–682. | ||
The GUSTO IIb Investigators. A comparison of recombinant hirudin with heparin for the treatment of acute coronary syndromes. N Engl J Med. 1996;335:775–782. | ||
InTIME-II Investigators. Intravenous NPA for the treatment of infarcting myocardium early; InTIME-II, a double-blind comparison of single-bolus lanoteplase vs accelerated alteplase for the treatment of patients with acute myocardial infarction. Eur Heart J. 2000;21:2005–2013. | ||
Krumholz HM, Chen J, Wang Y, Radford MJ, Chen YT, Marciniak TA. Comparing AMI mortality among hospitals in patients 65 years of age and older: evaluating methods of risk adjustment. Circulation. 1999;99:2986–2992. | ||
Williams BA, Wright RS, Murphy JG, Brilakis ES, Reeder GS, Jaffe AS. A new simplified immediate prognostic risk score for patients with acute myocardial infarction. Emerg Med J. 2006;23:186–192. | ||
Pogorevici A, Citu IM, Bordejevic DA, Caruntu F, Tomescu MC. Canada acute coronary syndrome is a stronger baseline predictor than age ≥75 years of in-hospital mortality in acute coronary syndrome patients in western Romania. Clin Interv Aging. 2016;11:1–8. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.