Back to Journals » International Journal of General Medicine » Volume 14
Prognosis and New Predictors of Early Left-Ventricular Thrombus Following ST-Elevation Myocardial Infarction
Authors Zhang Q, Zhang Z, Jin L, Wang C, Zheng H, Li S, Yu M, Si D , Zhang W
Received 8 October 2021
Accepted for publication 17 November 2021
Published 30 November 2021 Volume 2021:14 Pages 8991—9000
DOI https://doi.org/10.2147/IJGM.S343418
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Qian Zhang,1 Zhongfan Zhang,1 Lina Jin,2 Chengbing Wang,3 Haikuo Zheng,1 Shouping Li,1 Miao Yu,1 Daoyuan Si,1 Wenqi Zhang1
1Department of Cardiology, China-Japan Union Hospital of Jilin University, Jilin Provincial Molecular Biology Research Center for Precision Medicine of Major Cardiovascular Disease, Changchun, People’s Republic of China; 2Department of Epidemiology and Biostatistics, School of Public Health, Jilin University, Changchun, Jilin, People’s Republic of China; 3Department of Neurology, China-Japan Union Hospital of Jilin University, Changchun, Jilin, People’s Republic of China
Correspondence: Daoyuan Si;Wenqi Zhang
Department of Cardiology, China-Japan Union Hospital of Jilin University, Xiantai Street No. 126, Changchun, Jilin, People’s Republic of China
Tel +86 135 78949866
; +86 136 44407485
Fax +86 431 84995233
; +86 431 84995259
Email [email protected]; [email protected]
Objective: In the current era of primary percutaneous coronary intervention (PPCI), the prognosis of the left ventricular thrombus (LVT) is not well assessed.
Methods: We performed a retrospective, single-center study of 1305 consecutive ST-segment-elevation myocardial infarction (STEMI) patients treated with PPCI. During a mean period of 27 months of follow-up, the major adverse cardiovascular and cerebrovascular events (MACCE) were recorded.
Results: The incidence of LVT (n = 47) was 3.60%. The independent risk factors of LVT included anterior STEMI, left ventricular (LV) aneurysm, reduced LV ejection fraction (LVEF), dilated LV end-diastolic dimension (LVEDD), and delayed door-to-balloon time (DTBT). During follow-up, LVT was an independent risk factor for MACCE [hazard ratio (HR)=3.46; 95% confidence interval (CI) = 2.23– 3.38; P < 0.01]. Patients with LVT were more likely to have the following complications: heart failure (P < 0.001), embolic events (P = 0.034), and all-cause mortality (P = 0.020). Notably, the regression of LVT was not independently associated with those three adverse events (P > 0.05).
Conclusion: In the era of PPCI, the presence of early LVT following STEMI was associated with adverse events. Furthermore, the prognosis of patients with LVT did not improve even if the LVT regressed. LVT was likely a generalized indicator of impaired cardiac performance, rather than the cause. This indicated that prophylactic therapy and identifying individuals with a high risk of developing LVT were of substantial importance.
Keywords: left ventricular thrombus, ST-segment elevation myocardial infarction, prognosis, risk factors
Introduction
The left ventricular thrombus (LVT) is a feared complication for its risks of embolization to peripheral arteries and vital organs after acute myocardial infarction.1,2 Comparing ST-segment-elevation myocardial infarction (STEMI) patients with LVT to those without LVT, the rate of embolic events in patients with LVT was four-fold higher, and the rate of long-term mortality was two-fold higher.3 In the current era of primary percutaneous coronary intervention (PPCI), the formation of LVT subsequent to STEMI remains relatively common. The estimated incidence is up to 15% despite advances in reperfusion and timely anti-thrombotic therapy.4–6 Regardless of STEMI treatments, risk factors for LVT that have been identified are an anterior STEMI, large infarct area, and reduction in systolic function.7–9 Given the high-risk and increasing burden of LVT, data of which we are aware regarding their prediction to predict its occurrence remains a clinical challenge. Furthermore, data on the prognosis of LVT-related events are not well assessed in the era of PPCI.10,11 Consequently, we conducted a retrospective study to evaluate the risk factors and prognosis of LVT in patients admitted for STEMI and treated with PPCI in the Provincial Chest-Pain Center.
Materials and Methods
Study Population and Design
Consecutive STEMI patients (N = 1363), who underwent PPCI from January 2017 to September 2019 at the China-Japan Union Hospital were screened in our study. The STEMI was defined in accordance with the new World Health Organization (WHO) criteria as revised in 2000: a rise in cardiac troponin levels accompanied by clinical symptoms of myocardial ischemia, and pathological Q waves and/or changes in the electrocardiogram (ECG) (new or presumed-new ST segment elevation at the J-point in least two or more consecutive leads, with ST segment elevation within the cut-off of ≥0.2 mV in leads V1, V2, or V3; and ≥0.1 mV in other leads).12 In total, 58 patients were excluded by the following criteria: combination with previous stress cardiomyopathy (n = 13), myocarditis (n = 11), dilated cardiomyopathy (DCM; n = 8), and patients who died before the first echocardiogram (n = 26). The remaining 1305 patients enrolled in our study were classified as patients with LVT (LVT group, n = 47) and without LVT (control group, n = 1258) (Figure 1). Written informed consent was obtained from the patients prior to enrolment. The trial was approved by the Institutional Review Board of The China-Japan Union Hospital of Jilin University (Approval No. 2019012804).
 |
Figure 1 Study flow chart. Abbreviations: STEMI, ST-elevation myocardial infarction; PCI, percutaneous coronary intervention; LVT, left ventricular thrombus. |
A retrospective analysis was performed using the agency’s electronic records and database. Hematological parameters were collected from the antecubital vein before the patient received any fibrinolytic therapy. Management of vascular lesions were performed during PCI at the operator’s discretion. PCI results were interpreted by two experienced senior operators. Two-dimensional echocardiography is generally performed within 72 h of admission by experienced sonographers. If the diagnosis of LVT is suspectable, patients will perform a mandatory second assessment, including two-dimensional echocardiography or cardiac magnetic resonance before discharge. In accordance with the recommendation by the American Echocardiography Association, the Simpson method was used to evaluate the left ventricular ejection fraction (LVEF).13 LVT was diagnosed as a protruding or independently active mass in the left ventricular cavity throughout systole and diastole that was different from the notochord structure, papillary muscle, trabecula, technical artifact, or tangent view of the left ventricular wall.14 Treatment of all patients with LVT was left to the discretion of the attending physician based on the patient’s clinical status.
Follow-Up
Clinical outcomes were assessed through clinic visits or telephone visits. The major adverse cardiovascular and cerebrovascular event (MACCE) was defined as the first occurrence of any component of the composite outcome of all-cause death, heart failure, non-fatal myocardial reinfarction, revascularization, stroke, or systemic thromboembolism during a mean period of 27 months of follow-up. Stroke was diagnosed based on neurological examinations and MRI scans.15 The secondary outcome was LVT regression and the incidence of bleeding events, including clinically relevant bleeding events and major bleeding events. The standard of bleeding was defined by the Bleeding Academic Research Consortium.16
Statistical Analysis
Continuous variables were presented as “mean ± standard deviation” or “median [quartile]” (ie, “M [Q1, Q3]”), and compared using the Student’s t test or rank-sum test. Categorical variables were presented as counts and percentages and compared using the Rao-Scott chi-squared test. Multivariate, logistic regression was performed to identify the independent risk factor of early occurrence of LVT, adjusted for sex, age, and the covariates that were statistically significant in univariate analysis [Diagnosis, left ventricular (LV) aneurysm, fibrinogen, delayed door-to-balloon time (DTBT),LV ejection fraction (LVEF), dilated LV end-diastolic dimension (LVEDD)]. For the primary endpoint, the association of LVT with time-to-MACCE was estimated by Kaplan-Meier curves. The association between LVT and MACCE was examined using the Cox proportional-hazard, regression model, adjusted for age, hypertension, and diabetes mellitus status. R version 3.6.3 (University of Auckland, Oakland, New Zealand) was used to perform the statistical analyses. Statistical significance was set at P < 0.05.
Results
Clinical Characteristics Between the Two Groups
A total of 1305 STEMI patients were included in this retrospective, single-center study. LVT was diagnosed before hospital discharge in 47 of the 1305 STEMI patients (3.60%). Baseline characteristics are listed in Table 1. There were no statistically significant differences between the LVT and the control groups regarding age, sex, smoking history, or concomitant diseases (such as hypertension and diabetes). Patients who were admitted to the hospital within 12 h after experiencing chest pain were less likely to develop LVT. The average DTBT of the LVT group was statistically significantly longer than that of the control group.
 |
Table 1 Baseline Demographics |
The results from hematological parameters obtained upon admission were similar between the two groups, except for the level of fibrinogen and creatinine, which was significantly higher in the LVT group (P < 0.05). The echocardiography findings demonstrated that more patients in the LVT group had signs of lower LVEF, LV aneurysm, and dilated LVEDD; all were significantly different between the two groups (P < 0.05). Moreover, coronary angiography showed that the anterior descending artery was the chief culprit of all patients in LVT group.
Predictors of LVT
To further identify the risk factors related to LVT, a multivariate, logistic, regression analysis was performed (Table 2). After adjusting for sex and age, the independent risk factors of LVT after STEMI were an anterior STEMI [odds ratio (OR): 35.72, 95% confidence interval (CI): 7.26–647.22, P = 0.001], LV aneurysm (OR: 41.33, 95% CI: 10.25–247.31, P < 0.001), lower LVEF (OR: 0.95, 95% CI: 0.91–0.98, P = 0.005), delayed DTBT per 20 (OR: 1.18, 95% CI: 1.04–1.35, P = 0.011), and dilated LVEDD (OR: 1.08, 95% CI: 1.02–1.15, P = 0.010).
 |
Table 2 Multivariate Logistic Regression Analysis for Assessment of Independent Predictors of LVT |
Clinical Outcomes
Among the 1305 patients without LVT, the follow-up data for 39 patients were incomplete, and these patients were excluded from this study. During a mean period of 27 months of follow-up, the primary endpoint of MACCE was significantly higher in the LVT group vs the control group (46.8% vs 18%, P < 0.001) (Table 3 and Figure 2). Heart failure (29.8% vs 9.1% P < 0.001), embolic events (6.4% vs 1.9% P = 0.034), and all-cause mortality (12.8% vs 5% P = 0.020) were significantly increased in the LVT group. There were no significant differences in other components of MACCE in the LVT group vs the control group (P > 0.05 for all). There was no significant difference in the incidence of bleeding events between the two groups (P = 0.195). After adjusting for the relevant factors (age, hypertension, and diabetes) in the multivariate Cox proportional hazard model (Table 4), LVT remained a significant, independent predictor of MACCE (HR = 3.46; 95% CI 2.23–3.38; P < 0.001).
 |
Table 3 Univariate Logistic Regression for MACCE |
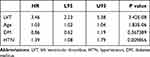 |
Table 4 Multivariate Analysis of Predictors of MACCE in Patients with LVT During a Mean Period of 27 Months |
Adverse Outcomes According to Occurrence of LVT Regression
As shown in Table 5, total LVT regression occurred in 33 patients (70.21%) within a median time of 14 months (interquartile range: 6 to 25 months). Heart failure occurred in 24.24% and 42.86% of LVT-regression and LVT-persistent patients, respectively. All-cause mortality occurred in 9.10% and 21.43% of LVT-regression and LVT-persistent patients, respectively. Reduced stroke was observed in patients with LVT regression (6.10% vs 14.28%). However, no statistically significant differences were observed between patients with LVT regression and patients with persistent LVT for these adverse events (heart failure, embolic events, and all-cause mortality; P > 0.05 for all parameters).
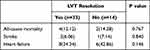 |
Table 5 The Relationship Between LVT Resolution and the Adverse Outcomes |
Discussion
This study provided new data and insights into the contemporary incidence, prediction, and prognosis of LVT in patients with STEMI in PPCI practice. Based on the results of this study, we have made three essential findings: (1) Studies have consistently demonstrated that the independent risk factors of LVT were anterior STEMI, lower LVEF, LV aneurysm, and dilated LVEDD. Furthermore, our study showed that a shorter DTBT significantly reduced the incidence of LVT. (2) The presence of LVT was independently associated with an increased incidence of MACCE over a mean period of 27 months of follow-up. Notably, the regression of LVT was not independently associated with adverse events.
Incidence and Predictors of LVT in the Current Era
The incidence of LVT following STEMI was 3.60% in our study, which was consistent with previous studies.6,17,18 There is growing evidence that the principal risk factors closely associated with LVT after STEMI are both the presence of anterior-territory STEMI and LV dysfunction.18–20 In our study, we also found that the location of the vessel infarct in the left anterior descending (LAD) was the single most important independent predictor of LVT after STEMI. Patients with anterior STEMI had a 10-fold increased risk of LVT formation. Furthermore, LVEF was the strongest independent predictor of LVT formation, which was significantly lower in patients with LVT. Dilated LVEDD and an aneurysm appeared to be more common in patients with LVT. LV remodeling and stasis of blood might play a positive role in LVT formation. This finding has frequently been described in previous studies.4,21,22 In addition, though many studies have demonstrated that shorter DTBTs are associated with a promising prognosis in STEMI patients,23,24 the value of DTBT in LVT formation following STEMI has been controversial.25–27 In our study, patients with delayed DTBT had a significantly higher probability of demonstrating LVT, emphasizing the importance of shorter DTBT. It is a well-known information that kidney injury predisposes to thrombus formation. Notably, previous studies confirmed that acute kidney injury (AKI) had a predictive value both in in-hospital outcomes and long-term outcomes of patients with STEMI, suggesting that creatinine and blood urea nitrogen might be helpful in patients at higher clinical risk. We also found that the level of creatinine in the LVT group was significantly higher. Unfortunately, the multivariate analysis is not statistically significant, which needs to be confirmed by prospective studies. In addition, a total of 19 STEMI patients were treated with IABP in our study.28,29 Consistent with prior study, the prognosis remained poor despite IABP support in patients with STEMI. We found IABP support therapy had no relationship with the formation of LVT.30
Clinical Outcome of LVT
In our study, we found that LVT was an independent risk factor for MACCE over a mean period of 27 months of follow-up, after adjusting for principal confounders. Increased risk of heart failure, embolic events, and all-cause mortality were variables that also reached statistically significant differences between the two groups. Heart failure is the principal adverse event in patients with LVT. It is well established that heart failure is a strong predictor of LVT in STEMI patients.31,32 Inversely, LVT might be an important trigger of heart failure. In the pre-thrombolytic period, LVT was associated with a 5.5-fold increase in embolic events.33 Chen et al concluded that the relative risk of embolic complications in patients with LVT after acute myocardial infarction (AMI) increased nearly 4-fold, regardless of follow-up time and detection tools.3 Consistent with prior studies, a 3.37-fold higher risk of an embolic event was observed in patients with LVT in our study. A retrospective study of 128 LVT patients reported that all-cause mortality occurred in 13% of the patients within a 1-year follow-up.22 Another study followed-up the patients who underwent PCI for STEMI for 1-year, and they detected a mortality rate of 10%.10 Likewise, in our study, we reported a mortality rate of 12.8% in patients with LVT, and found that mortality was statistically significantly different between the LVT group and non-LVT group. These findings highlight the worst prognosis associated with LVT.
During the follow-up of the patients with LVT, we did not note any significant differences in the rates of adverse events (heart failure, embolic events, or all-cause mortality) between patients with and without LVT regression. Several studies before the PCI era tried to determine the association between the presence of LVT and embolic events.33,34 Surprisingly, these studies did not demonstrate a convincing relationship. Lemaitre et al, in a study of 105 heart failure (HF) patients with LVT, reported a lower risk of long-term consequences (death <3%) and the potential for the patients to experience reverse remodeling. Notably, however, the patients with LVT had a higher incidence of embolic events within 30 d.35 Consistent with our findings, Lemaitre et al demonstrated that the presence of LVT did not seem to be associated with mortality or preclude reverse remodeling. In addition, Lattuca et al recently performed a retrospective study of 159 LVT patients who were screened from ordinary patients.36 Similar to our results, they found that the presence of LVT presented a high risk of clinical complications and LVT regression was not associated with heart failure or embolic events. The only difference between our results and theirs was that they reported that LVT regression was associated with reduced mortality. Variations in study subjects and treatment factors (DTBT, antithrombotic combinations, and treatment duration) might have contributed to the differing results. Consequently, our results emphasized that patients with LVT after STEMI were likely a generalized indicator of impaired cardiac performance, rather than the cause.
Some limitations of the current study should be considered. First, we based the diagnosis of LVT mainly on echocardiography, which might have less sensitivity and specificity than other imaging methods, such as CMR and left ventriculography. However, CMR and left ventriculography are not suitable as the basic screening tests in STEMI patients. Furthermore, we used CMR and left ventriculography to confirm the diagnosis of LVT obtained by routine echocardiography in cases when diagnostic confidence was low. Second, a different therapy strategy might affect the clinical outcome. However, several recent studies have shown that there is no statistical difference in rates of MACCE or LVT regression between novel oral anticoagulants (DOACs) and vitamin K antagonist therapeutic strategies.36–38
Conclusion
In conclusion, our study indicated that LVT was not uncommon in patients with STEMI treated with PPCI. Anterior STEMI, LV dysfunction, LV aneurysm, delayed DTBT, and increased LVEDD were independent risk factors of LVT. Furthermore, LVT was an independent predictor of MACCE over a mean period of 27 months of follow-up. Importantly, we showed that LVT was likely a generalized indicator of impaired cardiac performance; patients with LVT had a particularly high risk of subsequent cardiovascular events after STEMI. This further indicated that prophylactic therapy and identifying individuals at high risk are of substantial importance.
Abbreviations
PPCI, primary percutaneous coronary intervention; LVT, left ventricular thrombus; STEMI, ST-segment elevation myocardial infarction; LVEF, left ventricular ejection fraction; MACCE, major adverse cardiovascular and cerebrovascular event; LVEDD, left ventricular end-diastolic dimension; DTBT, delayed door-to-balloon time; CMR, cardiac magnetic resonance.
Data Sharing Statement
The datasets used during the current study are available from the corresponding author upon request (Wenqi Zhang).
Ethical Approval and Consent to Participate
The study was approved by the Institutional Review Board of The China-Japan Union Hospital of Jilin University (Approval No. 2019012804). All participants provided informed consent to participate in this research and it was conducted in accordance with the Declaration of Helsinki.
Consent for Publication
The authors confirm that all contents of this study can be published.
Acknowledgments
The authors thank the entire staff of the cardiology laboratory and sonographers for their assistance during this study. Daoyuan Si and Wenqi Zhang are co-correspondence authors for this study.
Funding
This work was supported by grants from the Scientific and Technological Developing Scheme of Ji Lin Province (20210204199YY) and Science and Technology of Jilin Province (20180520054JH and 20200801076GH).
Disclosure
The authors have no conflicts of interest to declare.
References
1. Jordan RA, Miller RD, Edwards JE, et al. Thrombo-embolism in acute and in healed myocardial infarction. I. Intracardiac mural thrombosis. Circulation. 1952;6(1):1–6. doi:10.1161/01.CIR.6.1.1
2. Ram P, Shah M, Sirinvaravong N, et al. Left ventricular thrombosis in acute anterior myocardial infarction: evaluation of hospital mortality, thromboembolism, and bleeding. Clin Cardiol. 2018;41(10):1289–1296. doi:10.1002/clc.23039
3. Chen PF, Tang L, Yi JL, Pei JY, Hu XQ. The prognostic effect of left ventricular thrombus formation after acute myocardial infarction in the contemporary era of primary percutaneous coronary intervention: a meta-analysis. Eur J Intern Med. 2020;73:43–50. doi:10.1016/j.ejim.2019.10.029
4. Phan J, Nguyen T, French J, et al. Incidence and predictors of left ventricular thrombus formation following acute ST-segment elevation myocardial infarction: a serial cardiac MRI study. Int J Cardiol Heart Vasc. 2019;4(24):100395.
5. McCarthy CP, Vaduganathan M, McCarthy KJ, Januzzi JL
6. Robinson AA, Jain A, Gentry M, McNamara RL. Left ventricular thrombi after STEMI in the primary PCI era: a systematic review and meta-analysis. Int J Cardiol. 2016;221:554–559. doi:10.1016/j.ijcard.2016.07.069
7. Weinsaft JW, Kim HW, Crowley AL, et al. LV thrombus detection by routine echocardiography: insights into performance characteristics using delayed enhancement CMR. JACC Cardiovasc Imaging. 2011;4(7):702–712. doi:10.1016/j.jcmg.2011.03.017
8. Solheim S, Seljeflot I, Lunde K, et al. Frequency of left ventricular thrombus in patients with anterior wall acute myocardial infarction treated with percutaneous coronary intervention and dual antiplatelet therapy. Am J Cardiol. 2010;106(9):1197–1200. doi:10.1016/j.amjcard.2010.06.043
9. Asinger RW, Mikell FL, Elsperger J, Hodges M. Incidence of left-ventricular thrombosis after acute transmural myocardial infarction. Serial evaluation by two-dimensional echocardiography. N Engl J Med. 1981;305(6):297–302. doi:10.1056/NEJM198108063050601
10. Moss AJ, Shah ASV, Zuling ET, et al. Left ventricular thrombus after primary PCI for ST-elevation myocardial infarction: 1-year clinical outcomes. Am J Med. 2019;132(8):964–969. doi:10.1016/j.amjmed.2019.02.033
11. You J, Wang X, Wu J, et al. Predictors and prognosis of left ventricular thrombus in post-myocardial infarction patients with left ventricular dysfunction after percutaneous coronary intervention. J Thorac Dis. 2018;10(8):4912–4922. doi:10.21037/jtd.2018.07.69
12. Alpert JS, Thygesen K, Antman E, et al. Myocardial infarction redefined–a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J. 2000;21(18):1502–1513.
13. Lang RM, Bierig M, Devereux RB, et al. American Society of Echocardiography’s Nomenclature and Standards Committee; Task Force on Chamber Quantification; American College of Cardiology Echocardiography Committee; American Heart Association; European Association of Echocardiography, European Society of Cardiology Recommendations for Chamber Quantification. Eur J Echocardiogr. 2006;7(2):79–108.
14. Haugland JM, Asinger RW, Mikell FL, Elsperger J, Hodges M. Embolic potential of left ventricular thrombi detected by two-dimensional echocardiography. Circulation. 1984;70(4):588–598. doi:10.1161/01.CIR.70.4.588
15. Kernan WN, Ovbiagele B, Black HR, et al. American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Guidelines for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack: a Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association . Stroke. 2014;45(7):2160–2236.
16. Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–2747. doi:10.1161/CIRCULATIONAHA.110.009449
17. Khoury S, Carmon S, Margolis G, Keren G, Shacham Y. Incidence and outcomes of early left ventricular thrombus following ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. Clin Res Cardiol. 2017;106(9):695–701. doi:10.1007/s00392-017-1111-4
18. Shacham Y, Leshem-Rubinow E, Ben Assa E, et al. Frequency and correlates of early left ventricular thrombus formation following anterior wall acute myocardial infarction treated with primary percutaneous coronary intervention. Am J Cardiol. 2013;111(5):667–670. doi:10.1016/j.amjcard.2012.11.016
19. Habash F, Vallurupalli S. Challenges in management of left ventricular thrombus. Ther Adv Cardiovasc Dis. 2017;11(8):203–213. doi:10.1177/1753944717711139
20. Jiang YX, Jing LD, Jia YH. Clinical characteristics and risk factors of left ventricular thrombus after acute myocardial infarction: a matched case-control study. Chin Med J (Engl). 2015;128(18):2415–2419. doi:10.4103/0366-6999.164869
21. Meurin P, Brandao Carreira V, Dumaine R, et al. College National des Cardiologues Français; Collège National des Cardiologues des Hôpitaux Français, Paris, France. Incidence, diagnostic methods, and evolution of left ventricular thrombus in patients with anterior myocardial infarction and low left ventricular ejection fraction: a prospective multicenter study. Am Heart J. 2015;170(2):256–262.
22. McCarthy CP, Murphy S, Venkateswaran RV, et al. Left ventricular thrombus: contemporary etiologies, treatment strategies, and outcomes. J Am Coll Cardiol. 2019;73(15):2007–2009. doi:10.1016/j.jacc.2019.01.031
23. McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47(11):2180–2186. doi:10.1016/j.jacc.2005.12.072
24. Rollando D, Puggioni E, Robotti S, et al. Symptom onset-to-balloon time and mortality in the first seven years after STEMI treated with primary percutaneous coronary intervention. Heart. 2012;98(23):1738–1742. doi:10.1136/heartjnl-2012-302536
25. Rabbani LE, Waksmonski C, Iqbal SN, et al. Determinants of left ventricular thrombus formation after primary percutaneous coronary intervention for anterior wall myocardial infarction. J Thromb Thrombolysis. 2008;25(2):141–145. doi:10.1007/s11239-007-0064-2
26. Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283(22):2941–2947. doi:10.1001/jama.283.22.2941
27. Zhang Q, Si D, Zhang Z, et al. Value of the platelet-to-lymphocyte ratio in the prediction of left ventricular thrombus in anterior ST-elevation myocardial infarction with left ventricular dysfunction. BMC Cardiovasc Disord. 2020;20(1):428. doi:10.1186/s12872-020-01712-w
28. Hayıroğlu Mİ, Bozbeyoglu E, Yıldırımtürk Ö, Tekkeşin Aİ, Pehlivanoğlu S. Effect of acute kidney injury on long-term mortality in patients with ST-segment elevation myocardial infarction complicated by cardiogenic shock who underwent primary percutaneous coronary intervention in a high-volume tertiary center. Turk Kardiyol Dern Ars. 2020;48(1):1–9. doi:10.5543/tkda.2019.84401
29. Çinar T, Hayiroğlu Mİ, Şeker M, et al. The predictive value of age, creatinine, ejection fraction score for in-hospital mortality in patients with cardiogenic shock. Coron Artery Dis. 2019;30(8):569–574. doi:10.1097/MCA.0000000000000776
30. Hayıroğlu Mİ, Çanga Y, Yıldırımtürk Ö, et al. Clinical characteristics and outcomes of acute coronary syndrome patients with intra-aortic balloon pump inserted in intensive cardiac care unit of a tertiary clinic. Turk Kardiyol Dern Ars. 2018;46(1):10–17. doi:10.5543/tkda.2017.11126
31. Zhang Q, Wang CM, Shi ST, Chen H, Zhou YJ. Relationship of left ventricular thrombus formation and adverse outcomes in acute anterior myocardial infarction in patients treated with primary percutaneous coronary intervention. Clin Cardiol. 2019;42(1):69–75. doi:10.1002/clc.23106
32. Gianstefani S, Douiri A, Delithanasis I, et al. Incidence and predictors of early left ventricular thrombus after ST-elevation myocardial infarction in the contemporary era of primary percutaneous coronary intervention. Am J Cardiol. 2014;113(7):1111–1116. doi:10.1016/j.amjcard.2013.12.015
33. Vaitkus PT, Barnathan ES. Embolic potential, prevention and management of mural thrombus complicating anterior myocardial infarction: a meta-analysis. J Am Coll Cardiol. 1993;22(4):1004–1009. doi:10.1016/0735-1097(93)90409-T
34. Gottdiener JS, Gay JA, VanVoorhees L, DiBianco R, Fletcher RD. Frequency and embolic potential of left ventricular thrombus in dilated cardiomyopathy: assessment by 2-dimensional echocardiography. Am J Cardiol. 1983;52(10):1281–1285. doi:10.1016/0002-9149(83)90588-X
35. Lemaître AI, Picard F, Maurin V, Faure M, Dos Santos P, Girerd N. Clinical profile and midterm prognosis of left ventricular thrombus in heart failure. ESC Heart Fail. 2021;8(2):1333–1341. doi:10.1002/ehf2.13211
36. Lattuca B, Bouziri N; ACTION Study Group, et al. Antithrombotic therapy for patients with left ventricular mural thrombus. J Am Coll Cardiol. 2020;75(14):1676–1685.
37. Ali Z, Isom N, Dalia T, et al. Direct oral anticoagulant use in left ventricular thrombus. Thromb J. 2020;29(18):29. doi:10.1186/s12959-020-00242-x
38. Guddeti RR, Anwar M, Walters RW, et al. Treatment of left ventricular thrombus with direct oral anticoagulants: a retrospective observational study. Am J Med. 2020;133(12):1488–1491. doi:10.1016/j.amjmed.2020.05.025
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

