Back to Journals » Clinical Optometry » Volume 14
Profile of Amblyopia Among Children Aged from 5 to 15 Years at Hawassa University Comprehensive Specialized Hospital Pediatric Eye Clinic, South Ethiopia, 2020/21
Authors Gebru EA , Alem KD , G/Silassie MG
Received 7 May 2022
Accepted for publication 28 July 2022
Published 10 August 2022 Volume 2022:14 Pages 149—157
DOI https://doi.org/10.2147/OPTO.S372001
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Mr Simon Berry
Elias Abera Gebru, Kindie Desta Alem, Mikael Girum G/Silassie
Department of Ophthalmology and Optometry, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
Correspondence: Elias Abera Gebru, Department of Ophthalmology and Optometry, College of Medicine and Health sciences, Hawassa University, PO Box 1560, Hawassa, Ethiopia, Tel +251 918190360, Email [email protected]
Purpose: Functional visual impairment in children is mostly caused by amblyopia. Permanent visual impairment is caused by belated treatment of amblyopia and underlying causes, mostly due to the lack of awareness. Amblyopia affects children’s school performance, social interaction and motor skills. This study was aimed to assess the profile of amblyopia among children aged from 5 to 15 years.
Methods and Materials: A hospital-based, cross-sectional study was done from November to April 2020/21. Data were collected from all children who came to Hawassa university comprehensive specialized hospital pediatric eye out patient department in the data collection period. Visual acuity measurement, slit lamp examination, cycloplegic refraction, cover test and dilated fundus examination were conducted. Data was entered in Epi-info version 7 and analyzed by Statistical Package for Social Science version 20. Descriptive statistics were conducted to estimate the proportion of amblyopia and its causes.
Results: The proportion of amblyopia was 23.8% (18.3– 29.7). Most of the participants were within the age range of 5– 9 years (55.4%) and males (51.5%). Anisometropia was the commonest cause of amblyopia (31.25%), followed by meridional (20.83), mixed (16.67%), isometropia (12.50%), sensory deprivation (10.42%) and strabismus (8.33%).
Conclusion: The proportion of amblyopia was 23.8%. Anisometropia, meridional, sensory deprivation, isometropia, mixed type and strabismus were the identified causes of amblyopia.
Keywords: amblyopia, anisometropia, children
Introduction
During the first decade of life, there is continuous vision development due to changes in the visual system.1 Amblyopia is a snellen visual acuity (VA) difference of greater than or equal to two lines between the two eyes, or it is a reduction in VA below 6/9 in either eye after the best possible correction.2,3 It occurs when there is a deficient stimulus to the eye during the first decade of life.1–3
When there are different images in the two eyes, one eye with better VA is preferred but the other eye is suppressed.4–7 Amblyopia causes unilateral or bilateral visual impairment, which can be due to sensory deprivation or faulty binocular vision interaction. Visual impairment due to amblyopia persists even after the best possible corrections.8
The causes of amblyopia can be abnormal binocular vision interaction and/or any conditions that can disrupt the formation of a clear image during the critical period of vision development.9 More than fifty percent of children having anisometropia and/or strabismus in their critical vision development period develop amblyopia.10 The degree of visual impairment due to amblyopia depends on the age of onset and the type/severity of amylogenic factors. Based on the degree, amblyopia can be classified as mild (best corrected visual acuity (BCVA) 6/9-6/12), moderate (BCVA 6/12-6/30), and severe (BCVA 6/30-3/60).11
If amblyopia is not identified and treated in the critical period of vision development, it will cause permanent visual reduction and, finally, it will affect children’s school achievement and social life.12 In later life, if there is eye trauma on the better eye, amblyopia can also cause total blindness.13
The clinical features of amblyopia comprise reduced VA, easily affected by crowding effects,14,15 poor spatial distortions,16 unsteady and inaccurate monocular fixation,17 poor eye tracking ability,18 reduced contrast sensitivity,19 inaccurate accommodative response and poor binocularity.20,21 Amblyopia only develops in children up to the age of 8 years and if it is left untreated, it can persist throughout life.22 In the age group of 20–70+years, amblyopia is the leading cause of unilateral visual impairment exceeding cataract, diabetic retinopathy, glaucoma and macular degeneration.23
Early detection and treatment of amblyopia is the key for the prevention of visual impairment caused by it. However, there were no amblyopia studies done in South Ethiopia. This study was conducted to estimate the proportion of amblyopia and its causes in the hospital. The finding will help policy makers to design early prevention mechanisms and will also stimulate them to conduct community-based studies.
Methods and Materials
A cross-sectional hospital-based study was conducted from November to April, 2020/21. The study was conducted at Hawassa university comprehensive specialized hospital (HUCSH), south Ethiopia. This hospital is the biggest and the only tertiary eye care hospital in the region, and it serves around 16 million people from Southern nations and nationalities, people’s regional state (SNNPRS), Sidama regional state and the neighboring Oromia region. It is located at 275kms south of Addis Ababa, the capital city of Ethiopia. In the hospital, there is one pediatric eye out patient department (OPD). Most pediatric patients presented at the hospital pediatric eye OPD were children seeking eye examination secondary to different ocular disorders, referred from primary and secondary eye care units for further ocular evaluations and/or parents/teachers notice child’s poor visual performance. All children aged 5 to 15 years presented at HUCSH pediatric eye OPD were a source population. Children with visually significant fundus disorders and/or with penetrating eye injury involving the visual axis were excluded from the study.
We made the following assumptions to calculate the sample size:- Level of confidence taken to be 95%, margin of error (d) 5%, according to the study done at ophthalmology clinic of Menilik II Hospital, the prevalence was 9.1%, p = 0.091.24 Based on the above assumption, the sample size was calculated as follows:
Where n = sample size calculated
Z = level of significance
≈d = margin of error
n = (1.96) 2 *(0.09*0.91)/(0.05) 2
n = 125.85≈126
By taking the non-respondent rate of 10% = 12.6, our sample size was n = 138.6~139. But the sample size was small; therefore, we prefer to take all children who fulfilled the inclusion criteria in the study period and that was n = 205.
Operational Definitions
Pediatric
Age group of population ≤15 years.
Amblyopia
Best corrected visual acuity of poorer than 6/9 in either one or both eyes in the absence of any pathological ocular disorders.
Refractive Error
Child having ≥+1.50DS hyperopia, ≥-0.75DS myopia and/or ≥±1.50DC astigmatism in either one or both eyes.
Degree of Refractive Error
- Mild hyperopia defined as ≤+2.00DS, Moderate hyperopia defined as +2.25DS-+5.00DS, High hyperopia defined as > +5.00DS.25
- Mild myopia defined as ≤-3.00DS, Moderate myopia defined as −3.25DS- (−6.00DS), High myopia defined as > −6.00DS.26
Strabismic amblyopia
Amblyopia in the presence of manifest ocular misalignment but in the absence of refractive error.27
Anisometropic Amblyopia
Amblyopia occurs when there is uncorrected refractive error in which the difference between the corresponding major meridians is greater than −3.00 DS myopia, greater than or equal to +1.00 DS hyperopia and greater than ±1.50 astigmatism.27
Isometropic Amblyopia
High refractive error in both eyes, for myopic greater than-6.00 DS, for hyperopic greater than +5.00 DS and for astigmatism greater than ±2.50 DC.27
Sensory Deprivation Amblyopia
Amblyopia occurs when there is known ocular diagnosis like ptosis, cataract, or corneal opacity.27
Meridional (Astigmatism) Amblyopia
Amblyopia occurs when there is a regular astigmatism of >1.5 DC on any meridian.24
Mixed Amblyopia
Amblyopia caused by both strabismus and refractive error.
Data Collection Procedure
During the study period, data collectors examined all children who came to pediatric eye OPD. Written consent from parents was obtained. Demographic data and detailed patient history were collected from the parents by using structured questions on the initial patient presentation.
A full ocular assessment was conducted, including VA measurement, ocular alignment, assessment of anterior segment and posterior segment disorders. The assessment of refractive error was conducted by cycloplegic refraction using cyclopentolate 1% eye drops.
Finally, BCVA was obtained using an appropriate snellen VA chart for a child’s age. When his/her BCVA fulfills the amblyopia definition, then the diagnosis was recorded as amblyopia. The BCVA for deprivational amblyopia was taken after one month of eye surgery.
Data Collection Tools
Questionnaires
The parents and children were interviewed using a structured questionnaire to obtain information on children’s demographic data.
Clinical Tools
Snellen visual acuity chart, trial lens and frame, retinoscopy, slit lamp bio-microscope, direct ophthalmoscope and 90D lens, cyclopentolate 1% eye drops, prism bar and cover test occluder were used.
Data Quality Assurance
Training was given to the data collectors/optometrists. Data was collected after checking for consistency and completeness of questionnaires and clinical examinations on a daily basis.
Data Management and Analysis
Data cleaning and coding was first performed; then, data was entered in Epi-info version 7 and analyzed by SPSS version 20. Descriptive statistics were computed for all variables.
Ethical Considerations
Before the commencement of the study, ethical clearance was obtained from Hawassa University College of Medicine and Health sciences institutional review board with Ref.No.IRB/032/13 in accordance with the declaration of Helsinki.28 A written consent from parents/guardian was taken. The purpose and procedure of the examination were explained to the children and their parents.
Results
Socio-Demographic Characteristics of Participants
A total of 202 children participated in the study. The response rate was 98.5%. Most of the participants were males (51.5%) and with an age range of 5–9 years (55.4%) (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Children Aged from 5 to 15 Years at HUCSH Pediatric Eye OPD, South Ethiopia from November to April, 2020/21 (n = 202) |
Proportion and Clinical Characteristics of Amblyopia
Proportion of amblyopia was 23.8% (18.3–29.7).The proportion of amblyopia was high for age group of 5–9 years (27.67%), for those having; anisometropia (75.75%), strabismus (56.52%), refractive error (41.41%) and media opacity (37.50%) (Table 2).
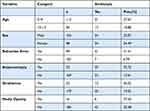 |
Table 2 Cross-Tabulation of Amblyopia with Different Variables Among Children Aged from 5 to 15 Years at HUCSH Pediatric Eye OPD, South Ethiopia from November to April, 2020/21 (n = 202) |
Most children have unaided visual acuity of 6/6 in the right eye (46.50%) and left eye (50.50%), respectively (Figure 1).
 |
Figure 1 Unaided visual acuity of children aged from 5 to 15 years at HUCSH pediatric eye OPD, south Ethiopia from November to April, 2020/21 (n = 202). |
Most children have BCVA of 6/6 in the right eye (64.90%) and left eye (65.3%) (Figure 2).
 |
Figure 2 Best corrected visual acuity of children aged from 5 to 15 years at HUCSH pediatric eye OPD, south Ethiopia from November to April, 2020/21 (n = 202). |
The proportion of amblyopia was high for children having hyperopia and constant strabismus for both right and left eyes (Table 3).
 |
Table 3 The Proportion of Amblyopia with Refractive Error and/or Strabismus for Children Aged from 5 to 15 Years at HUCSH Pediatric Eye OPD, South Ethiopia from November to April, 2020/21 (n = 202) |
Causes of Amblyopia
The most common and the least common causes of amblyopia were anisometropia and strabismus respectively (Figure 3).
 |
Figure 3 Causes of amblyopia for children aged from 5 to 15 years at HUCSH pediatric eye OPD, south Ethiopia from November to April, 2020/21 (n = 202). |
Discussions
In this study, the proportion of amblyopia was 23.8% (18.3–29.7). This finding is larger than study finding in India,29,30 Canada,31 Nepal,32,33 Saudi Arabia,34 and Ethiopia.24 This discrepancy might be due to differences in source population and study design. Many pediatric patients referred to our study area from primary and secondary eye care units for further ocular evaluations. Strabismic patients and those who need cycloplegic refraction were among the referral cases. This shows, in this study, the study population were more exposed to amylogenic factors relative to the above studies. This would have increase the proportion of amblyopia. Difference in timing of refractive amblyopia diagnosis and amblyopia definition cut-off point can be also other reasons for discrepancy.
In this study, most of the children had anisometropic amblyopia 15 (31.25%) followed by meridional 10 (20.83%), mixed 8 (16.67%), isometropic 6 (12.5%), deprivational 5 (10.42%) and strabismic 4 (8.33%). Anisometropic amblyopia was the largest in studies conducted in India,29 Nepal,32 Saudi Arabia,33 and Ethiopia.24 A higher proportion of amblyopic patients have refractive error. It is supported by many other studies, showing uncorrected refractive error as one of the major causes of visual impairment.35,36 Anisometropia causes amblyopia due to the retina of the more ametropic eye failing to get a clear image and stimuli for accommodative effort. Whereas, the image formed on the retina of the good eye is focused, clear and sharp.37 On the contrary, in studies done in India38 and Pakistan,39 most of the children had strabismic amblyopia. This discrepancy is most likely due to differences in the source population. The above studies included all children who visited the hospital, but in this study we only included school-aged children (5–15 years).
According to this study, compared to children with no strabismus, the proportion of amblyopia was high for children with strabismus. When there is ocular misalignment in one eye of the child, he/she complains about double vision. But, this will not persist for a longer duration due to the brain’s capability mechanism to avoid diplopia by suppressing the cells in the visual pathway of the misaligned eye. This adaptive mechanism decreases the sensitivity of cortical cells in the visual system, which will finally cause amblyopia.37
The proportion of amblyopia was also high for children with media opacity. Appropriate vision development needs enough light stimulus. However, when there is deprivation in the critical period of vision development, light stimuli will not be reached the retina. This will affect the normal visual process and lead to amblyopia.37
Limitation of the Study
In this study, the refractive correction adaptation period was not considered for refractive amblyopia diagnosis and this may cause slight over estimation of amblyopia.
Conclusion
The proportion of amblyopia was 23.8%. Anisometropia, meridional, sensory deprivation, isometropia, mixed type and strabismus were the identified causes of amblyopia.
Acknowledgment
We would like to thank the study participants for their active participation.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. William H, Bernarad G. Children Optometry. Spain: Butterworth Heinemann; 2004.
2. Janti SS, Raja AM, Matheen A, Charanya C, Pandurangan R. A cross sectional study on prevalence of amblyopia in school going children. J Evolution Med Dent Sci. 2014;3(30):8561–8565. doi:10.14260/jemds/2014/3086
3. Myron Y, Jay D. Ophthalmology.
4. El Mallah MK, Chakravarthy U, Hart PM. Amblyopia: is visual loss permanent? Br J Ophthalmol. 2000;84(9):952–956. doi:10.1136/bjo.84.9.952
5. Theodore G. Primary Care Optometry.
6. Terry B. Visual Problems in Children. Great Britain: Butterworth Heinemann; 1993.
7. Eileen EB. Amblyopia and Binocular Vision. Prog Retin Eye Res. 2013;33:67–84. doi:10.1016/j.preteyeres.2012.11.001
8. Pradeep S. Strabismus. India: CBS; 1999.
9. Sjostrand J, Abrahamsson M. Risk factors in amblyopia. Eye. 1990;4(6):787–793. doi:10.1038/eye.1990.124
10. Kiorpes L, Kiper DC, O’Keefe LP, Cavanaugh JR, Movshon JA. Neuronal correlates of amblyopia in the visual cortex of macaque monkeys with experimental strabismus and anisometropia. J Neurosci. 1998;18(16):6411–6424. doi:10.1523/JNEUROSCI.18-16-06411.1998
11. Children Eye Disease Investigator Group. A comparison of atropine and patching treatments for moderate amblyopia by patient age, cause of amblyopia, depth of amblyopia, and other factors. Ophthalmology. 2003;110:163. doi:10.1016/s0161-6420(02)01449-5
12. Wu C, Hunter DG. Amblyopia: diagnostic and therapeutic options. Am J Ophthalmol. 2006;141(1):175–184. doi:10.1016/j.ajo.2005.07.060
13. Harrad R, Williams C. Risk, causes and outcomes of visual impairment after loss of vision in the non-amblyopic eye, a population-based study. SurvOphthalmol. 2003;48(2):235–236.
14. Stuart JA, Burian HM. A study of separation difficulty, its relationship to VA in normal and amblyopic eyes. Am J Ophthalmol. 1962;53:471–477. doi:10.1016/0002-9394(62)94878-X
15. Flom MC, Weymouth FW, Kahneman D. Visual resolution and contour interaction. J Opt Soc Am. 1963;53:1026–1032. doi:10.1364/JOSA.53.001026
16. Bedell HE, Flom MC. Monocular spatial distortion in strabismic amblyopia. Invest Ophthalmol Vis Sci. 1981;20:263–268.
17. Brock FW, Givner I. Fixation anomalies in amblyopia. Arch Ophthalmol. 1952;47:775–786. doi:10.1001/archopht.1952.01700030794008
18. Ciuffreda KJ, Kenyon RV, Stark L. Fixational eye movements in amblyopia and strabismus. J Am Optom Assoc. 1979;50:1251–1258.
19. Hess RF, Howell ER. The threshold contrast sensitivity function in strabismic amblyopia: evidence for a two type classification. Vision Res. 1977;17:1049–1055. doi:10.1016/0042-6989(77)90009-8
20. Wood ICJ, Tomlinson A. The accommodative response in amblyopia. Am J OptomPhysiol Opt. 1975;52:243–247. doi:10.1097/00006324-197504000-00001
21. Kirschen DG, Kendall JH, Reisen KS. An evaluation of the accommodative response in amblyopic eyes. Am J OptomPhysiol Opt. 1981;58:597–602. doi:10.1097/00006324-198107000-00015
22. Harwerth RS, Smith EL, Duncan GC, et al. Multiple sensitive periods in the development of the primate visual system. Science. 1986;232(4747):235–238. doi:10.1126/science.3952507
23. National Eye Institute. VA Impairment Survey Pilot Study. Bethesda, MD: NEI; 1984.
24. Alemayehu W, Abonesh G. Profile of amblyopia at menilik II hospital in Addis Ababa. Ethiop J Health Dev. 2008;22(2):78.
25. Nathan C, Paula A. Refractive management/intervention. Am Acad Ophthalmol. 2015;1:845.
26. Evidence based optometry committee. Clinical Report: Myopia Management. American optometric Association; 2021.
27. Celik NB, Kose AO, Celik HU, Imamoglu S. BCSC Pediatric Ophthalmology and Strabismus. Section. 2020;6:10203
28. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/jama.2013.281053
29. Deepti J, Shanti P, Nitin M, Govind S. Profile of amblyopia in children of age 5 to 15 years at tertiary care center. Int J Health Clin Res. 2021;4(8):129–132.
30. Manisha G, Sudhir K, Sanjiv K. Profile of Amblyopia in School going (5-15 years) Children at State Level Referral Hospital. J Clin Diagnostic Res. 2016;10(11):SC09–SC11.
31. Drover JR, Kean PG, Courage ML, Adams RJ. Prevalence of amblyopia and other vision disorders in young Newfoundland and Labrador children. Can J Ophthalmol. 2008;43(1):89–94. doi:10.3129/i07-187
32. Sapkota K, Pirouzian A. Prevalence of amblyopia and patterns of refractive error. Nepal J Ophthalmol. 2013;5(9):38–44. doi:10.3126/nepjoph.v5i1.7820
33. Bhandari G, Byanju R, Kandel RP. Prevalence and profile of Amblyopia in children at Bhartapur Eye Hospital. Ann Pediatr Child Health. 2008;3(8):1085.
34. Kamrava M. Middle East. Africa J Opthalmol. 2015;22(1):878.
35. Li YP, Zhou MW, Forster SH, et al. Prevalence of amblyopia among preschool children in central south China. Int J Ophthalmol. 2019;12(5):820–825. doi:10.18240/ijo.2019.05.19
36. Shah M, Khan MT, Khan MD. Clinical profile of amblyopia in Pakistani children age 3 to 14 years. J Coll Physicians Surg Pak. 2005;15(6):353–357.
37. Roberta M, Zagui B. Amblyopia types, diagnosis, treatment, and new perspectives. Clin educ. 2019;25:2–4.
38. Menon VMS, Chaudhuri ZMS. Profile of amblyopia in a hospital referral practice. Indian J Ophthalmol. 2005;53(4):227–234. doi:10.4103/0301-4738.18903
39. Sethi S, Sethi MJ, Hussain I, Kundi NK. Causes of amblyopia in children coming to ophthalmology outpatient department Khyber Teaching Hospital, Peshawar. J Pak Med Assoc. 2008;58(3):125–128.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.