Back to Journals » ClinicoEconomics and Outcomes Research » Volume 7
Productivity loss and resource utilization, and associated indirect and direct costs in individuals providing care for adults with schizophrenia in the EU5
Authors Gupta S, Isherwood G, Jones K, Van Impe K
Received 13 August 2015
Accepted for publication 1 October 2015
Published 25 November 2015 Volume 2015:7 Pages 593—602
DOI https://doi.org/10.2147/CEOR.S94334
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Giorgio L Colombo
Shaloo Gupta,1 Gina Isherwood,2 Kevin Jones,3 Kristel Van Impe4
1Kantar Health, Princeton, NJ, USA; 2Kantar Health, Epsom, Surrey, UK; 3European Federation of Associations of Families of People with Mental Illness, Diestsevest, Leuven, Belgium; 4Janssen-Cilag GmbH, Neuss, Germany
Objective: This study aimed to understand the impact of providing care for adults with schizophrenia on productivity, resource utilization, and costs in the EU5 (France, Germany, Italy, Spain, and UK).
Methods: Data from the 2010, 2011, and 2013 EU5 National Health and Wellness Survey, an online questionnaire of a nationwide sample of adults, were analyzed. Schizophrenia caregivers (n=398) were matched to noncaregivers (n=158,989) and other caregivers (n=14,341) via propensity scores. Outcome measures included health care utilization, Work Productivity and Activity Impairment questionnaire-based scores, and associated direct and indirect costs (estimated from the literature). Significant differences between schizophrenia caregivers vs noncaregivers and other caregivers (eg, cancer and Alzheimer's disease) were examined.
Results: After matching, schizophrenia caregivers reported greater activity impairment (38.4% vs 26.1%), provider visits (8.0 vs 5.7), emergency room visits (0.9 vs 0.2), hospitalizations (0.8 vs 0.1), and direct costs (€2,258 vs €617) than noncaregivers, all P<0.001. Employed schizophrenia caregivers reported greater absenteeism, presenteeism, overall work impairment (35.0% vs 20.7%), and indirect costs (€6,667 vs €3,795) than noncaregivers, all P<0.001. Schizophrenia caregivers (vs other caregivers) reported greater activity impairment (38.4% vs 32.3%) and provider visits (8.0 vs 6.6), P<0.05. A greater proportion of schizophrenia caregivers (vs other caregivers) reported at least one emergency room visit (26.1% vs 20.2%) and hospitalization (20.4% vs 14.3%), P<0.05. Employed schizophrenia caregivers incurred greater indirect costs than other caregivers (€6,667 vs €5,104).
Discussion: Schizophrenia caregivers reported greater activity impairment, resource utilization, and costs than noncaregivers and other caregivers. Better support systems for schizophrenia caregivers may help reduce the burden on the health care system and caregivers.
Keywords: schizophrenia, caregiver, direct cost, indirect cost, resource utilization, productivity loss, physician visits, burden, emergency room, hospitalization
Introduction
Schizophrenia is a severe mental disorder that has been estimated to affect over 21 million people worldwide.1 Symptoms can include hallucinations, delusions, and movement disorders, as well as affective flattening, avolition, and impaired cognitive functioning.2,3 Schizophrenia is associated with significant impairments in quality of life, psychological well-being, and premature mortality, with one study suggesting that, on average, men with schizophrenia died 15 years earlier, and women 12 years earlier, compared to population estimates.4–6
Estimates suggest that the global burden of schizophrenia is substantial, affecting ~7 per 1,000 of the adult population, with an overall incidence of ~1% of the population.1 Lifetime prevalence rates were estimated to be 5.5 per 1,000 persons,7 with a more recent reported median lifetime prevalence of 4.0 per 1,000.8 The average age of disease onset is between 15 and 35 years, generally late adolescence or early 20s for males and later for females;9 however, there were no significant differences reported between overall male and female prevalence rates or between geographical areas (urban vs rural) by Saha et al in their systematic review of the literature.8 Notably, the authors reported that prevalence rates appeared to be lower in less developed countries.
The frequent severe nature of schizophrenia, multifaceted psychiatric and physical symptomatology, and impairments in functioning often necessitate the need for family caregivers to provide ongoing support. Indeed, research has suggested that between 50% and 80% of schizophrenia patients live with or have regular contact with family members.10 Critically, caregiver burden can evolve without adequate support and can be associated with significant impairments. Previous studies across a variety of disease conditions have noted an association between high caregiver demand and burden and constraints in social activities, negative impact on family life, and feelings of loss.11 A prior study conducted in Italy found that strong emotion (eg, expressed hostility or critical comments) was positively correlated with more subjective burden among relatives of people with schizophrenia.12 Further, studies suggest that informal caregivers are at greater risk of illness, psychological distress, disruption of professional and personal roles, and increased risk of mortality.13–16
A prior review of published research examining schizophrenia caregiver burden reported that these individuals frequently experience deteriorated health, including stress-related conditions, anxiety, and depression.17 Further, there appears to be a linear relationship between time spent providing care and reported burden, with investigators also noting that caregivers who cared for those patients who were high-to-moderately dependent reported greater impairment in the health, professional, and family/socially domains.18 Globally, limited research exists concerning the impact of such burden on health care resource use or productivity among this vulnerable group of caregivers.
Further work has examined the burden upon caregivers of those diagnosed with schizophrenia. In a small study in Cyprus, authors examined caregiver burden among caregivers noting that family members of male patients were more likely to report impairment.19 Gater et al also examined caregiver burden, this time utilizing qualitative methodology, noting the significant physical and emotional toll, as well as time demand, reported by caregivers.20 These two studies examined caregivers of similar demographic characteristics, with participants generally in their 50s, married,19 and employed,20 with an average of one-fifth of caregivers reporting a college education. The majority (79%) of participants in the study by Gater et al20 were female compared to ~47% in the study by Panayiotopoulos et al.19 Finally, Kate et al investigated the impact of coping strategies by family caregivers, identifying a number of maladaptive techniques that were associated with impairments in quality of life.21
Although prior literature has noted that the cost of caregiving in the context of schizophrenia is likely significant, no literature has been published in Europe on large-scale reliable estimates of the costs connected with such care.22 This represents a gap in the literature, with investigators emphasizing the critical importance of accurate financial estimates in guiding treatment and care decisions in the context of schizophrenia. A broad US-based study estimated this cost to be over 62 billion in 2002; however, more specific costs of caregiving, in particular, are yet to be investigated.23 The current study sought to enhance the understanding of the impact of providing care to adults with schizophrenia on productivity, daily activities, health care resource utilization, and associated costs in the EU5 (Germany, France, Italy, Spain, and UK).
Methods
Sample
Data from the 2010, 2011, and 2013 EU5 National Health and Wellness Survey (NHWS) were used in the analyses. The NHWS is a national, Internet-based health survey of adults (18+ years) conducted in most years (NHWS was not conducted in EU5 in 2012).
Respondents of the NHWS are recruited from an Internet panel using a random stratified sampling framework to ensure that the demographic composition (with respect to age and sex) is identical to that of the adult population based on governmental statistics. To ensure a representative sample, particularly in the older population (>65 years), online recruitment was supported by computer-assisted web interviews. Computer-assisted web interview respondents were recruited by telephone and had the choice to complete the interview on the phone while the interviewer entered the responses online, or were e-mailed a link to the survey to complete on their own.
The NHWS was approved by Essex Institutional Review Board (Lebanon, NJ, USA), and all respondents provided informed consent. All information was self-reported by respondents. It is possible for online respondents to complete more than one survey over a several-year period; only the most recent data for a given respondent were kept in these instances.
All NHWS respondents were asked, “Are you currently caring for an adult relative with any of the following conditions?” (eg, Alzheimer’s disease, stroke, multiple sclerosis, epilepsy, and cancer). Data were analyzed for respondents who self-reported being a caregiver for an adult relative with schizophrenia compared with those not providing care for an adult relative with any condition and those self-reported providing care for an adult with another condition (eg, Alzheimer’s disease, cancer, and stroke). Detailed methodology regarding all of the above has been published previously.24
Measures
Demographics
Survey respondents reported on country, age (continuous), sex (male or female), marital status (married/living with partner vs single/divorced/separated/widowed), education (college/university degree vs less than college/university degree), household income (<€20,000/<£20,000, ≥€50,000/≥£40,000, decline to answer vs €20,000 to <£50,000/£20,000 to <£40,000), employment status (currently employed [full time, part time, or self-employed] vs not currently employed).
Health characteristics
Body mass index (overweight, obese, or decline to answer vs underweight/normal weight), smoking status (current smoker, former smoker vs never smoker), alcohol consumption (currently drink vs do not drink alcohol), and exercise behavior in the past 30 days (exercised vs not exercised) were assessed. Self-reported comorbidity data were used to calculate a comorbidity burden score using the Charlson comorbidity index (CCI).
The CCI weights the presence of the following self-reported conditions and sums the result: HIV/AIDS, metastatic tumor, lymphoma, leukemia, any tumor, moderate/severe renal disease, hemiplegia, diabetes, mild liver disease, ulcer disease, connective tissue disease, chronic pulmonary disease, dementia, cerebrovascular disease, peripheral vascular disease, myocardial infarction, congestive heart failure, and diabetes with end organ damage. The original CCI predicts the likelihood of mortality. In the current study, the CCI provides an estimate of comorbidity burden, and the greater the total index score, the greater the comorbid burden on the individual.25
Productivity loss
Work productivity was measured using the Work Productivity and Activity Impairment questionnaire, a six-item validated instrument, which consists of four metrics: absenteeism (the percentage of work time missed because of one’s health in the past 7 days), presenteeism (the percentage of impairment experienced while at work in the past 7 days because of one’s health), overall work productivity loss (an overall impairment estimated that is a combination of absenteeism and presenteeism), and activity impairment (the percentage of impairment in daily activities because of one’s health in the past 7 days).26 Only respondents who report being full time, part time, or self-employed provided data for absenteeism, presenteeism, and overall work impairment. All respondents provided data for activity impairment.
Resource utilization
Health care utilization was defined by the number of traditional health care provider visits (eg, general practitioner, internist, cardiologist, neurologist, and psychiatrist), the number of emergency room (ER) visits (“how many times have you been to the ER for your own medical condition in the past six months?”), and the number of times hospitalized (“how many times have you been hospitalized for your own medical condition in the past six months?”) in the past 6 months.
Indirect costs
Indirect costs were estimated for each respondent using the human capital method. Indirect costs were calculated by using Eurostat median income (≥18 years) for 2012.27 Hourly wages were estimated by dividing annual income by the typical number of weeks worked per year and hours worked per week. Data on weeks and hours worked in 2012 were obtained from the European Foundation for the Improvement of Living and Working Conditions.28 The number of hours missed in the last week because of one’s health (absenteeism) and the number of hours health problems affected productivity while at work (presenteeism) were each multiplied by the hourly wage rates to arrive at total lost wages per week. These figures were then multiplied by the average number of work weeks in a year to obtain the total indirect annual estimates.
Direct costs
Health care resource use was assessed by the number of reported visits in the past 6 months to traditional health care providers (eg, general practitioner, internist, cardiologist, neurologist, and psychiatrist), the ER, and the number of times hospitalized, which was doubled to obtain an annual estimate. The annualized visits were then multiplied by a country- and provider-specific average unit cost.
For France, Italy, and Germany (ER visits only), direct costs were estimated by multiplying each patient’s annualized health care use by the average cost of that service reported in the literature,29 then adjusting for inflation using the health-related Harmonized Index of Consumer Prices obtained from Eurostat to 2013 values. Hospitalization and primary care cost for Germany were also found in the literature.30 For France, Germany, Italy, and Spain, the cost of a hospitalization was multiplied by three, the median number of days for a hospital stay as found in the 2007 NHWS (the most recent NHWS survey that assessed number of days per hospitalization). Costs for the UK were sourced from the Unit Costs of Health and Social Care 2013.31 Costs for Spain were extracted from Osakidetza.32
Statistical analysis
To analyze demographics, health characteristics, productivity loss, resource utilization, and direct and indirect cost differences between schizophrenia caregivers and noncaregiver, and between schizophrenia caregivers and other caregivers, bivariate analyses were performed. Chi-square tests were used with categorical variables; analysis of variances (ANOVAs) were used with continuous variables.
A propensity scoring methodology (1:2 ratio) was used to match caregivers of adults with schizophrenia and noncaregivers on age, sex, marital status, education, household income, employment status, body mass index, smoking status, alcohol consumption, exercise behaviors, and the CCI. A separate propensity match (1:2 ratio) was implemented to match schizophrenia caregivers to those providing care to adults with another condition (not schizophrenia) using the same metrics. The matching was constrained so that all matches were within each European country. Postmatch differences between these groups were re-examined to confirm sufficient balance. Differences between caregivers of adults with schizophrenia vs noncaregivers and caregivers of adults with other conditions (unmatched and matched) were analyzed on demographics, health characteristics, productivity loss, resource use, and costs using χ2 tests for categorical variables and ANOVAs for continuous variables. For all analyses, P<0.05 was considered statistically significant.
Results
Demographics and health characteristics
A total of 398 schizophrenia caregivers, 158,989 noncaregiver, and 14,341 caregivers of other conditions were identified via EU5 NHWS across 2010, 2011, and 2013. In this total sample of 173,728 adults across the EU5, 25.4% were in France, 25.3% in Germany, 25.6% in the UK, 14.0% in Italy, and 9.6% in Spain. The average age of schizophrenia caregivers was 45.3 years (SD =15.8 years), 59.6% were female, and 52.5% were currently employed.
Before matching, caregivers of adults with schizophrenia compared with noncaregivers were more likely to be female and smoke, were less likely to be married and employed, and report greater comorbidity burden as assessed via CCI, all P<0.05. Before matching, schizophrenia caregivers compared with caregivers of other conditions were younger, less likely to be married, had a lower annual household income, were more likely to currently smoke, and reported greater comorbidity burden, all P<0.05 (Table 1).
  | Table 1 Respondent demographics and health characteristics by caregiver status |
Productivity loss and resource utilization
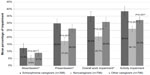
After matching, among employed respondents, schizophrenia caregivers reported greater absenteeism (12.4% vs 5.6%), presenteeism (29.9% vs 17.5%), and overall work impairment (35.0% vs 20.7%) than noncaregivers, all P<0.001. Schizophrenia caregivers also reported greater activity impairment (38.4% vs 26.1%, P<0.001) than noncaregivers.
Schizophrenia caregivers reported more activity impairment than other caregivers (38.4% vs 32.3%, P=0.001). However, no significant difference was found in work-related impairment between these two groups, which may be due to the small sample of employed respondents (52.5%; Figure 1).
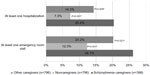
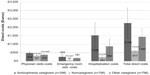
A greater proportion of schizophrenia caregivers reported at least one ER visit (26.1% vs 12.3%) and hospitalization (20.4% vs 7.3%) than noncaregivers, both P<0.001. Also, a greater proportion of schizophrenia caregivers reported at least one ER visit (26.1% vs 20.2%) and hospitalization (20.4% vs 14.3%) than other caregivers, both P<0.03 (Figure 2). After matching, schizophrenia caregivers reported a greater number of health care provider visits (8.0 vs 5.7), ER visits (0.9 vs 0.2), and hospitalizations (0.8 vs 0.1) than noncaregivers, all P<0.001. Comparing schizophrenia caregivers and other caregivers, schizophrenia caregivers reported a greater number of health care provider visits (8.0 vs 6.6, P=0.021). The number of hospitalizations were only marginally significant across schizophrenia caregivers and other caregivers (P=0.059; Figure 3).
Indirect and direct costs
Greater work productivity impairments resulted in higher estimated costs for schizophrenia caregivers than noncaregivers. On average, employed schizophrenia caregivers were estimated to incur ~€2,800 more indirect costs than noncaregivers at €6,667 and €3,795, respectively. After matching, on average, employed schizophrenia caregivers were estimated to incur ~€1,500 more indirect costs than other caregivers at €6,667 and €5,104, respectively. Absenteeism cost estimates were significantly greater for schizophrenia caregivers than other caregivers (€2,457 vs €1,458, P=0.022; Figure 4).
Average estimated medical care costs, at €2,258 per schizophrenia caregiver per year, were significantly higher than that of the noncaregiver average of €617. All resource utilization cost estimates were significantly greater for schizophrenia caregivers than noncaregivers (all P<0.001). The average estimated medical care costs, at €2,258 per schizophrenia caregiver per year, were marginally higher than those of the other caregivers average of €1,440 (P=0.084; Figure 5).
Discussion
Schizophrenia is a debilitating chronic mental illness that can exert tremendous burden on caregivers and has been associated with impairments in quality of life and physical and psychological well-being. Despite this global burden, and the importance of quantifying this burden to guide care decisions on a societal level; productivity loss, health care resource utilization, and estimates of associated direct and indirect costs among caregivers have not been investigated comprehensively in Europe. Studies within this domain of research have generally examined caregivers with similar demographics.19,20 In the previous work, and in line with the current study, caregivers tended to be middle aged (mid-40s to mid-50s), married, predominantly female, and employed. Approximately one-quarter of participants reported possessing a college education, similar to the 29% reported in the current study.
The current study found significant economic burden associated with caregiving for an individual with schizophrenia across a number of important domains. These included resource utilization, including health care provider visits, ER visits, and hospitalizations, which were all greater among schizophrenia caregivers than noncaregivers. This greater resource utilization was reflected in a significantly higher average of estimated medical care costs of €2,258 per schizophrenia caregiver per year, compared to a noncaregiver average of €617.
In addition, caregivers reported greater productivity losses, including absenteeism and presenteeism, and activity impairment, thus emphasizing the multifaceted impact of schizophrenia on caregivers and society at large. Work-related productivity loss was similar across schizophrenia caregivers and other caregivers. Due to small sample sizes of employed respondents and the limited power in the current study, significant differences across these metrics were not able to be detected. Consistent with previous research detailing the burden among caregivers,22 these results suggest that relatives of those diagnosed with schizophrenia require greater support to ensure that they are able to maintain their health and provide effective care.
Formal care programing, including family and social support interventions, may help to reduce the burden upon schizophrenia caregivers and, in turn, reduce the costs associated with caregiving on a societal level. Sharif et al demonstrated that a family-focused intervention was able to significantly reduce caregiver burden and symptom severity among patients.33 Additionally, prior research reports that family intervention may decrease the frequency of hospitalization, and enhance social functioning in people with schizophrenia, and improve coping strategies and social resources for caregivers.34,35 Furthermore, family interventions have been associated with reduced guilt and better empathy for caregivers.36 However, effective family interventions may require continuous support to manage all aspects of schizophrenia.37 Enhanced treatment options, more effective medications, and a focus on ensuring patient adherence may assist in controlling illness symptoms, and thus also in turn reduce burden upon caregivers. This message is reinforced by evidence that suggests that there is reduced burden among caregivers of higher functioning patients.38
Limitations
The current study is the first to quantify direct and indirect costs among schizophrenia caregivers in Europe and will help guide care planning and resource utilization among this vulnerable group. It is important, however, to consider the implications of these results in line with study limitations. The use of retrospective, cross-sectional data and online recruitment of caregivers may not be truly representative of the entire EU5 caregiver population. For example, the use of an Internet-based survey may bias recruitment toward a younger and/or healthier caregiver population.
This study was neither designed to examine the caregiver relationship, patient symptoms, or treatment history in detail nor were the diagnoses of schizophrenia confirmed by a health professional. This provides fertile ground for future research linking patient–caregiver factors to health impairments and direct and indirect costs. Further, indirect costs did not include time missed from work due to providing care or attending to caregiver issues, as well as prescription medication related costs. Therefore, overall indirect and direct costs may be underestimated and require further investigation. All participant responses were self-reported and may reflect recall biases and other forms of measurement error. Further, the use of a cross-sectional design precludes the ability to draw causal inferences from the data. Analyses included many covariates in the models, but other relevant covariates may not have been included, such as the caregiver’s type of employment and length of time providing care for the patient with schizophrenia.
Conclusion
Schizophrenia caregivers reported significant impairment across multiple important domains. These included greater activity impairment, more resource use, and greater direct and indirect costs than noncaregivers and caregivers of adults with other conditions. Better family and social support systems may help reduce the burden for schizophrenia caregivers, the health care system, and, in turn, reduce the societal cost of schizophrenia globally.
Acknowledgments
The authors acknowledge the background research and editorial assistance of Errol J Philip, a paid consultant to Kantar Health. Portions of this study were presented as a poster at the International Society of Pharmacoeconomics and Outcomes Research Annual European Congress 2014 in Amsterdam RAI, Amsterdam, the Netherlands: “Productivity Loss and Resource Utilization in Individuals Providing Care for Adults with Schizophrenia in the 5EU”. The poster abstract was published in Value in Health, Volume 17, Issue 7, A457: http://dx.doi.org/10.1016/j.jval.2014.08.1255.
Disclosure
S Gupta and G Isherwood are employees of Kantar Health, who were paid consultants to Janssen-Cilag in connection with the study design, analysis and interpretation of data, writing of the article, and the publication submission decision. K Van Impe is an employee of Janssen-Cilag, who funded the study and provided direction into the study design, analysis and interpretation of data, writing of the article, and the publication submission decision. K Jones holds a consultancy role with Janssen-Cilag and is an employee of the European Federation of Associations of Families of People with Mental Illness, who endorsed the study, provided expert insight into the study design, analysis and interpretation of data, reviewed the writing of the article, and provided insights on the publication submission decision. The authors report no other conflicts of interest in this work.
References
World Health Organization. World Health Organisation Health Topics: Schizophrenia; 2015. Available from: http://www.who.int/mental_health/management/schizophrenia/en/. Accessed March 18, 2015. | |
Tandon R, Gaebel W, Barch DM, et al. Definition and description of schizophrenia in the DSM-5. Schizophr Res. 2013;150:3–10. | |
National Institute of Mental Health. National Institute of Mental Health: Schizophrenia; 2009. Available from: http://www.nimh.nih.gov/health/publications/schizophrenia/index.shtml. Accessed March 18, 2015. | |
Crump C, Winkleby MA, Sundquist K, Sundquist J. Comorbidities and mortality in persons with schizophrenia: a Swedish National Cohort Study. Am J Psychiatry. 2013;170:324–333. | |
Bobes J, Garcia-Portilla MP, Bascaran MT, Saiz PA, Bousoño M. Quality of life in schizophrenic patients. Dialogues Clin Neurosci. 2007;9:215–226. | |
Solanki RK, Singh P, Midha A, Chugh K. Schizophrenia: impact on quality of life. Indian J Psychiatry. 2008;50:181–186. | |
Goldner EM, Hsu L, Waraich P, Somers JM. Prevalence and incidence studies of schizophrenic disorders: a systematic review of the literature. Can J Psychiatry. 2002;47:833–843. | |
Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2015;2:e141. | |
European Brain Council. European Brain Council Schizophrenia Fact Sheet; 2011. Available from: http://www.europeanbraincouncil.org/pdfs/Documents/SchizophreniafactsheetJuly2011.pdf. Accessed March 20, 2015. | |
Lehman AF, Steinwachs DM. Translating research into practice: the Schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophr Bull. 1998;24:1–10. | |
Magliano L, Fiorillo A, De Rosa C, Malangone C, Maj M; National Mental Health Project Working Group. Family burden in long-term diseases: a comparative study in schizophrenia vs physical disorders. Soc Sci Med. 2005;61:313–322. | |
Carrà G, Cazzullo CL, Clerici M. The association between expressed emotion, illness severity and subjective burden of care in relatives of patients with schizophrenia. Findings from an Italian population. BMC Psychiatry. 2012;12:140. | |
Hearson B, McClement S. Sleep disturbance in family caregivers of patients with advanced cancer. Int J Palliat Nurs. 2007;13:495–501. | |
Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282:2215–2219. | |
Schulz R, O’Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: prevalence, correlates, and causes. Gerontologist. 1995;35:771–791. | |
Fan YC, Chen MB, Lin KC, Bai YM, Wei SJ. [The resilience and health status of primary caregivers of schizophrenia patients]. Hu Li Za Zhi. 2014;61:29–38. | |
Caqueo-Urizar A, Gutierrez-Maldonado J, Miranda-Castillo C. Quality of life in caregivers of patients with schizophrenia: a literature review. Health Qual Life Outcomes. 2009;7:84. | |
Aranda-Reneo I, Oliva-Moreno J, Vilaplana-Prieto C, Hidalgo-Vega á, González-Domínguez A. Informal care of patients with schizophrenia. J Ment Health Policy Econ. 2013;16:99–108. | |
Panayiotopoulos C, Pavlakis A, Apostolou M. Family burden of schizophrenic patients and the welfare system; the case of Cyprus. Int J Ment Health Syst. 2013;7:13. | |
Gater A, Rofail D, Tolley C, et al. “Sometimes it’s difficult to have a normal life”: results from a qualitative study exploring caregiver burden in Schizophrenia. Schizophr Res Treatment. 2014;2014:368215. | |
Kate N, Grover S, Kulhara P, Nehra R. Relationship of caregiver burden with coping strategies, social support, psychological morbidity, and quality of life in the caregivers of schizophrenia. Asian J Psychiatr. 2013;6:380–388. | |
Awad AG, Voruganti LN. The burden of schizophrenia on caregivers: a review. Pharmacoeconomics. 2008;26:149–162. | |
McEvoy JP. The costs of schizophrenia. J Clin Psychiatry. 2007;68 (Suppl 14):4–7. | |
Gupta S, Isherwood G, Jones K, Van Impe K. Assessing health status in informal schizophrenia caregivers compared with health status in non-caregivers and caregivers of other conditions. BMC Psychiatry. 2015;21(15):162. | |
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. | |
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–365. | |
Eurostat. Mean and Median Income by Age and Sex; 2013. Available from: http://ec.europa.eu/eurostat/product?mode=view&code=ilc_di03. Accessed July 29, 2014. | |
Cabrita J, Galli da Bino C. Developments in Collectively Agreed Working Time 2012. Dublin, Ireland: Publications Office of the European Union; 2013. | |
Williams AE, Lloyd AC, Watson L, Rabe KF. Cost of scheduled and unscheduled asthma management in seven European Union countries. European Respiratory Review. 2006;15:4–9. | |
Zeidler J, Mahlich J, Greiner W, Heres S. Cost effectiveness of paliperidone palmitate for the treatment of schizophrenia in Germany. Appl Health Econ Health Policy. 2013;11:509–521. | |
Curtis L. Unit Costs of Health and Social Care 2013. Canterbury: Personal Social Services Research Unit; 2013. | |
Osakidetza, Tarifas para facturacion de servicios sanitarios y docentes de osakidetza para el ano 2013; 2013. | |
Sharif F, Shaygan M, Mani A. Effect of a psycho-educational intervention for family members on caregiver burdens and psychiatric symptoms in patients with schizophrenia in Shiraz, Iran. BMC Psychiatry. 2012;12:48. | |
Mayoral F, Berrozpe A, de la Higuera J, Martinez-Jambrina JJ, de Dios Luna J, Torres-Gonzalez F. Efficacy of a family intervention program for prevention of hospitalization in patients with schizophrenia. A naturalistic multicenter controlled and randomized study in Spain. Rev Psiquiatr Salud Ment. 2015;8(2):83–91. | |
Magliano L, Fiorillo A, Fadden G, et al. Effectiveness of a psychoeducational intervention for families of patients with schizophrenia: preliminary results of a study funded by the European Commission. World Psychiatry. 2005;4(1):45–49. | |
Girón M, Nova-Fernández F, Mañá-Alvarenga S, et al. How does family intervention improve the outcome of people with schizophrenia? Soc Psychiatry Psychiatr Epidemiol. 2015;50(3):379–387. | |
Carrà G, Montomoli C, Clerici M, Cazzullo CL. Family interventions for schizophrenia in Italy: randomized controlled trial. Eur Arch Psychiatry Clin Neurosci. 2007;257(1):23–30. | |
Flyckt L, Fatouros-Bergman H, Koernig T. Determinants of subjective and objective burden of informal caregiving of patients with psychotic disorders. Int J Soc Psychiatry. 2015;61(7):684–692. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.