Back to Journals » ClinicoEconomics and Outcomes Research » Volume 8
Productivity benefits of minimally invasive surgery in patients with chronic sacroiliac joint dysfunction
Authors Saavoss J, Koenig L, Cher D
Received 1 December 2015
Accepted for publication 28 January 2016
Published 11 April 2016 Volume 2016:8 Pages 77—85
DOI https://doi.org/10.2147/CEOR.S101607
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Josh D Saavoss,1 Lane Koenig,1 Daniel J Cher2
1KNG Health Consulting, LLC, Rockville, MD, 2SI-BONE, Inc., San Jose, CA, USA
Introduction: Sacroiliac joint (SIJ) dysfunction is associated with a marked decrease in quality of life. Increasing evidence supports minimally invasive SIJ fusion as a safe and effective procedure for the treatment of chronic SIJ dysfunction. The impact of SIJ fusion on worker productivity is not known.
Methods: Regression modeling using data from the National Health Interview Survey was applied to determine the relationship between responses to selected interview questions related to function and economic outcomes. Regression coefficients were then applied to prospectively collected, individual patient data in a randomized trial of SIJ fusion (INSITE, NCT01681004) to estimate expected differences in economic outcomes across treatments.
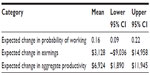
Results: Patients who receive SIJ fusion using iFuse Implant System® have an expected increase in the probability of working of 16% (95% confidence interval [CI] 11%–21%) relative to nonsurgical patients. The expected change in earnings across groups was US $3,128 (not statistically significant). Combining the two metrics, the annual increase in worker productivity given surgical vs nonsurgical care was $6,924 (95% CI $1,890–$11,945).
Conclusion: For employees with chronic, severe SIJ dysfunction, minimally invasive SIJ fusion may improve worker productivity compared to nonsurgical treatment.
Keywords: sacroiliac joint fusion, low back pain, sacroiliac joint pain, clinical trial, health care costs, indirect costs
Introduction
The sacroiliac joint (SIJ) connects the pelvis to the base of the spine and transmits forces of everyday activities. SIJ dysfunction, defined as pain and disability related to poor functioning of the SIJ, is associated with a burden of disease equivalent to that of many conditions commonly treated surgically, such as hip and knee degeneration and lumbar spinal stenosis,1 and quality of life scores that are at least as depressed, compared to these conditions.2 In patients evaluated for chronic low back pain, pain emanating from the SIJ occurs in 15%–23% of cases.3,4
Nonsurgical treatments for SIJ dysfunction include medication management, physical therapy, chiropractic treatment, intra-articular SIJ steroid injections, and percutaneous radiofrequency (RF) ablation of the lateral branches of the sacral nerve roots. High-quality evidence to support intra-articular steroid injections, which are commonly used in the US, is lacking. Two blinded randomized trials support the safety and short-term benefit (up to 3 months) of an RF ablation procedure,5,6 with modest evidence of benefit up to 1 year.7
Surgical treatments for chronic SIJ dysfunction include open SIJ fusion surgery (ie, open surgical decortication and reconstruction of the SIJ) and minimally invasive SIJ fusion. Retrospective comparative studies have provided strong evidence that both process variables (procedure time, blood loss, length of hospital stay) and clinical outcomes (pain relief at 1 and 2 years) from minimally invasive surgery are superior to open fusion,8–10 and minimally invasive approaches to SIJ fusion now appear to be preferred.11
Evidence of the clinical superiority of minimally invasive SIJ fusion was provided in INSITE, a prospective multicenter randomized controlled trial of SIJ fusion with titanium implants vs nonsurgical management (NSM) in patients with chronic SIJ dysfunction.12 In INSITE, NSM consisted of medication management, physical therapy for the SIJ according to American Physical Therapy Association guidelines, intra-articular steroid injections, and RF ablation of the lateral branches of the sacral nerve roots. These treatments were provided in a stepwise fashion to address patient pain and dysfunction. NSM was consistent with standard clinical care in the US at the time of study design. Twelve-month outcomes from this study showed that SIJ fusion reduced pain and disability levels and improved quality of life more than nonsurgical treatment. Success rates in the surgical group were >80%. Moreover, subjects who crossed over from nonsurgical to surgical treatment (allowed by the study protocol after the month 6 study visit) showed improvements in these outcomes similar to those originally assigned to surgical treatment. INSITE’s results are supported by a second US prospective multicenter clinical trial, showing similar improvements in pain, disability, and quality of life.13 A systematic review of published studies suggests that pain relief persists for 5 years.14
Due to fiscal constraints, payers and policymakers are aggressively looking for sources of cost savings, with attention often focused on high-cost procedures. While some stakeholders are interested only in direct medical costs, employers and payers may also consider indirect costs, such as the impact of disease and its treatment on aggregate worker productivity. Given the high health and quality of life burden of SIJ dysfunction, untreated disease can substantially impact worker health, leading to decreased worker productivity and turnover, all of which are associated with incremental costs. In this study, we combine data from two high-quality sources to calculate the expected changes in productivity for workers with chronic SIJ dysfunction who are treated either nonsurgically or surgically using triangular titanium implants.
Methods
To estimate the effects of surgical fusion using triangular titanium implants for chronic SIJ dysfunction on productivity, we used regression analysis and simulation based on a two-step approach used by Dall et al15 in a previous study. The first step used regression analysis based on the National Health Interview Survey (NHIS) data to estimate a general relationship between functional status and productivity, as measured by employment status and earnings. Next, functional status and other health-related factors for patients receiving surgical management and NSM of chronic SIJ dysfunction were used to predict economic outcomes using the first step’s regression results. We computed expected productivity for an individual by multiplying the predicted probability that person is working by a forecast of their earnings conditional on being employed.
Our approach extends that of Dall et al15 in two important ways. First, we accounted for selection bias resulting from censored earnings in the nonworking population. Second, we ran a multistage bootstrap simulation to compute a difference-in-difference productivity estimate across treatment groups and to conduct statistical inference. In our study, “difference-in-difference” means the difference in change scores from baseline to 6 months across treatments. The bootstrap approach allowed for better accounting for uncertainty in both the estimated relationship between functional status and economic outcomes and the effects of SIJ fusion surgery on patient outcomes.
Data sources
Many inputs for our models were from two prospective multicenter clinical trials conducted in the US. All trial sites (total of 45 sites) received institutional review board approval for the studies prior to study initiation.
Two data sources were used for this study: NHIS and prospective clinical trials. The 2013 NHIS is an ongoing cross-sectional health survey funded by the National Center for Health Statistics (NCHS) to ~33,000 adults annually.16 The survey collects data on a wide variety of topics including health status, employment, and earnings. We excluded individuals under 20 years or above 79 years of age as well as individuals who refused to respond to certain health and functional status questions. The final sample size included 31,543 individuals (see Table S1 for descriptive statistics on the NHIS sample).
The other data source was two prospective clinical trials, which were used to estimate the effects of SIJ fusion using triangular titanium implants on patient functional status and other clinical outcomes. INSITE (NCT01681004) is a randomized trial of 148 patients with SIJ dysfunction who underwent either SIJ fusion using the iFuse Implant System® (SI-BONE, Inc., San Jose, CA, USA) or NSM. NSM consisted of pain medication management, physical therapy, SIJ steroid injections, and RF ablation of the lateral branches of the sacral nerve roots. SIFI (NCT01640353) is an ongoing prospective multicenter single-arm clinical trial with enrollment criteria identical to INSITE. There were 172 subjects enrolled in SIFI. In both studies, subjects underwent preoperative and follow-up assessment using a visual analog pain score (0–100 scale) for SIJ pain, the Short Form 36 Health Survey (SF-36),17 Oswestry Low Back Disability Questionnaire (ODI),18 and the EuroQol-5D questionnaire (EQ-5D).19 Assessments took place at baseline, and at 1, 3, 6, 12, 18, and 24 months.
The 12-month results from INSITE showed marked, immediate, and sustained improvements in the surgical group in self-rated SIJ pain, disability as measured by ODI, and quality of life (using both SF-36 and EQ-5D).12 In the nonsurgical group, changes in all of these measures were minor and not clinically important. All change score difference comparisons were statistically superior in the surgical group. Twelve-month results in SIFI mirrored those observed in INSITE.13 As enrollment criteria were identical between the two studies, data from both studies were combined for the purposes of the current analysis, resulting in a final sample size of 265 subjects treated with minimally invasive SIJ fusion and 43 treated with NSM.
As the ODI, SF-36, and EQ-5D used in the SIJ fusion trials contain different informational elements that are also included in the NHIS, we used trial participant data from all three instruments. For questions and/or response categories in the NHIS that corresponded imperfectly to the other three survey instruments, we mapped responses from the NHIS to each of the relevant survey instrument responses (available from author upon request). At 6-month follow-up, less than 3% of patients had left the INSITE study and no crossover had occurred. The SIFI trial also had strong retention at 6 months (98%). As crossover in INSITE increased considerably after month 6, we used responses from the 6-month follow-up period for purposes of measuring treatment effects. Twelve-month postsurgical results from both studies were nearly identical to 6-month results. Only subjects with complete responses in all questionnaire fields used were included in this analysis.
Regression analysis
We used a two-stage Heckman selection model to estimate the relationship between earnings and functional status (Tables S2 and S3). There may be systematic unobserved differences between working and nonworking populations. For example, someone who is not working may be choosing not to work because the wage they could command is less than the wage they require to work. If so, an earnings model estimated using only data from a working population may not make unbiased predictions applicable to a nonworking population. To attempt to do so would likely result in overestimating the income of individuals entering the workforce, and thus overstating the value of the employment benefit of surgery. The Heckman model is widely used to estimate models of worker earnings in the labor economics literature, and corrects for selection bias resulting from the unobserved earnings of the nonworking population.20 The first estimation stage used a probit model to predict employment, and the second estimation stage used a linear regression equation to predict earnings. The NCHS has an earnings model to impute income.21 We included most of the explanatory variables used in the NCHS earnings model in both estimation stages of our Heckman model. However, variables included in the NCHS earnings model that were not collected from clinical trial participants and that could be affected by treatment assignment were excluded from our models. Other sources of income and presence of other working household members were included in the employment model as instruments, but excluded from the earnings model. As personal income is sometimes imputed in the NHIS, multiple imputation techniques were applied to correct for deflated standard errors. We used the results of this Heckman selection model regression analysis to estimate both the probability of working and earnings conditional on working for each patient in the clinical trial database at both baseline and 6-month follow-up.
Simulation-based productivity and earnings estimation
Difference-in-difference estimates were calculated using a multistage simulation model. In each iteration of the simulation, 265 surgical patients and 43 NSM patients were sampled with replacement from the combined INSITE and SIFI datasets. Using model estimates for each sample, we calculated the probability of working and income conditional on working from the employment and earnings predictive distributions for each observation in our bootstrapped sample at baseline and 6-month follow-up. Change in productivity was computed by subtracting the product of the baseline employment probability and baseline income from the product of the posttreatment employment probability and posttreatment income. We calculated the mean change in productivity across all observations for each treatment group, and computed a difference-in-difference estimate by comparing these averages. We ran 1,000 iterations of the simulation to generate confidence intervals (CIs). The result is an estimate of the difference in change in the probability of working and earnings potential between the two treatments at 6 months after treatment initiation.
Our models included some variables that were not collected from trial participants, such as educational attainment and marital status. Such variables were imputed by randomly matching selected trial participants with an NHIS respondent of the same sex and age category, and then populating missing variables with information from the matched NHIS respondent. If the same trial participant was resampled, he/she was not necessarily matched with the same NHIS respondent. However, within each iteration, the matched NHIS respondents were held constant for baseline and postestimation analysis.
Results
Table 1 shows characteristics of members of the NHIS sample and the two clinical trials (both at baseline and at 6 months posttreatment). As expected, patients in the NHIS were younger and reported better health status than those in the trials. Patients in the trials were nearly twice as likely to report fair or poor overall health status as compared to NHIS respondents. As a result of randomization, baseline characteristics of the SIJ fusion and NSM groups were similar. At 6 months posttreatment, SIJ fusion patients reported better health and functional status than those in the NSM group, although health and functional status improved in both groups relative to baseline.
All cost figures in this report are in US dollars, unless otherwise specified. Table 2 shows simulation results for modeled economic outcomes. For nonsurgical patients, the expected probability of working increased by 3% from baseline to 6-month follow-up (not statistically significant). In contrast, for patients undergoing SIJ fusion, the estimated likelihood of working by 6 months increased by 19% (ie, from 19% to 38%, P<0.001). The expected improvement in earnings conditional on working was higher for patients undergoing SIJ fusion compared to those undergoing NSM ($3,683 [P=0.08] vs $555 [P=0.93]), but the difference in earnings increase was not statistically significant. Combining the expected change in employment and earnings, we estimated a statistically nonsignificant increase of $1,283 in expected annual earnings for NSM patients and a statistically significant increase of $8,206 for SIJ fusion patients.
Table 3 shows incremental differences in the probability of working, earnings, and productivity at 6 months when electing for SIJ fusion as compared to NSM. That is, the table shows the difference in change scores (shown in Table 2) between the two treatments for the selected economic outcomes, along with CIs. Compared to baseline, the change in the probability working at 6 months was 16% higher (95% CI 9%–22%) in the surgical group than in the nonsurgical group. The difference in aggregate productivity, which incorporates both the likelihood of working and earnings potential, was also higher in the surgical group (mean $6,924, 95% CI $1,890–$11,945).
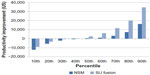
Figure 1 shows the prediction percentiles for the expected aggregate productivity change for surgical and nonsurgical patients. These intervals are wider than the mean productivity intervals shown in Table 3, because they represent the distribution of the estimated change in productivity for individuals, as opposed to average changes. Approximately 60% of surgical patients could expect a productivity improvement following surgery, as opposed to 50% of nonsurgical patients. Thirty percent of surgical patients are estimated to experience an annual productivity improvement exceeding $10,000, compared to 10% of nonsurgical patients.
Discussion
In this study, we used two data sources and a two-step regression approach to estimate indirect cost benefits of SIJ fusion surgery compared to NSM for individuals with SIJ dysfunction. We estimated that the incremental improvements in health status observed in two prospective clinical trials would result in an expected worker productivity increase valued at ~$6,900 per year. These indirect cost savings are substantial and may offset a substantial portion of the direct costs associated with surgical care. Failure to consider these indirect cost savings may result in understating the overall cost-effectiveness of surgical treatment for SIJ dysfunction.
To our knowledge, ours is the only study to estimate the indirect cost offsets associated with surgical treatment of SIJ dysfunction. While building on the approach used by Dall et al,15 we implemented a number of improvements. First, we corrected for selection bias in our employment and earnings NHIS models by using a two-stage Heckman selection model. Second, to the extent we relied on imputed income data from the NHIS, increased variability that resulted from this method was incorporated into our standard errors through the use of multiple imputation techniques. Third, when using our model to project economic outcomes for trial participants, we simulated missing model covariates from an approximate distribution rather than assuming fixed values. Finally, we used a multistage bootstrap simulation that allowed us to generate CIs that incorporate uncertainty at all stages of the estimation process.
As reviewed by Dagenais et al, several studies have estimated national indirect costs of low back pain, with US estimates ranging from $7–$28 billion per year.22 Workers with back pain lose productive times of 5.2 hours/week with an estimated national loss of $19.8 billion per year.23 Among employees with low back pain, indirect costs vary from $7,000–$25,000 per employee per year, depending on pain severity level.24,25 Analyses from other countries have shown similar impacts of low back pain on indirect costs in affected individuals.26
While the impact of back pain interventions on direct health care costs is commonly studied, assessments of indirect costs of back pain treatments are far rarer and have generally been limited to disc replacement or discectomy, and methods have varied substantially.27 Even fewer studies on indirect costs associated with surgical interventions have been published. A Norwegian randomized trial compared direct and indirect health care costs associated with disc replacement for chronic low back pain with those associated with NSM.28 Mean indirect costs for days missed work were ~€56,000 and mean costs for time spent by relatives were ~€12,000. The differences were not statistically significant. In a randomized trial of surgical vs nonsurgical care for lumbar disc herniation, indirect costs represented approximately one-quarter of surgical costs and 57% of nonsurgical costs.29 However, there were no statistical differences in mean 2-year indirect costs across groups. In a head-to-head trial of disc replacement vs fusion for lumbar disc degeneration, indirect costs were estimated from self-reported rates of absenteeism at follow-up visits and US average weekly salaries. After both surgical procedures, the likelihood of being employed decreased markedly but was similar in both groups throughout the study, suggesting no differential impact on indirect costs.30 Postsurgical lost wages averaged ~$2,800 per year.
Our study estimated an indirect 1-year cost savings of $6,900 associated with surgical vs nonsurgical care of SIJ dysfunction. A Markov simulation analysis of direct costs associated with surgical and nonsurgical treatments of SIJ dysfunction using the same clinical trial data showed an incremental cost of $9,833 at 5 years associated with use of surgical as opposed to nonsurgical treatments.31 The potential indirect cost savings of $6,900 in 1 year offsets a substantial portion (70%) of the 5-year net cost associated with surgery. This estimate may be conservative, as there is now substantial evidence from several studies with longer follow-up periods to suggest that the benefit from surgery may continue beyond 1 year.14 If the full benefit from surgery persists for at least 2 years, then overall costs (direct and indirect) may be lower in the surgical groups, ie, surgery may be cost saving from the societal perspective. More precise estimates of the incremental cost-effectiveness of surgical care can be achieved by incorporating our findings into a direct cost model and estimating total lifetime direct and indirect costs for each treatment option. We note that although 5-year follow-up suggests persistent pain relief, no clinical outcomes data are available beyond this time period.32
Our study reports indirect cost benefits from SIJ fusion using a societal perspective. This perspective implies that the full described benefit is not necessarily secured by a single party, but could instead be shared by numerous parties. Worker productivity improvements can benefit employers through increased profits, employees through increased earnings, and governments through increased tax revenue. While each party’s benefit allotment is ambiguous, it is likely that in the short term, the greatest benefits from SIJ fusion are incurred by the employer. This is true for two reasons. First, wages may not adjust immediately to changes in worker productivity. Thus, lost productivity due to SIJ dysfunction is likely to be experienced more by the employer than the employee. Second, as this study found surgery to significantly improve workforce participation, self-insured employers who offer short- or long-term disability benefits may experience a reduction in payouts. This payout reduction could be significant, as approximately one-third of employees participate in employer disability insurance programs which pay claimants, on average, ~60% of salary.33 Based on our study, and assuming an employer has a disability plan with full participation, expected reduction in disability payment could be as high as $2,976 per year (product of annual salary of $31,000 [from Table 2], 60% salary replacement, and 16% increase in probability of working and reduced probability of receiving disability payments). Another reduction in payout that we did not consider is retraining costs, which could be reduced with reduced employee turnover after SIJ fusion surgery.
Our study compared the effectiveness of SIJ fusion surgery to state-of-the-art NSM, which, at the time of study design included medication management, physical therapy, intra-articular SIJ steroid injections, and RF ablation of the lateral branches of the sacral nerve roots, delivered in a stepwise fashion to meet patient needs for pain control and improvement of SIJ-related disability. NSM in the trial was patterned after NSM commonly delivered in the US. A comparison of surgical outcomes to conservative treatment (ie, no specific treatment for SIJ dysfunction) would likely result in an increased estimated indirect cost benefit from surgery. As conservative management is not an accepted form of treatment for SIJ dysfunction, further exploration was not pursued.
Our study has some additional limitations. First, we assumed that effects of health and functional status on economic outcomes are largely independent of the cause of health or functional impairments. If this assumption does not hold, our regression models could be biased.
Second, in calculating differences in indirect costs over a single year, our model relied on an assumption regarding the persistence of the health benefit of SIJ fusion for 1 year. However, direct 1-year comparative data were not available due to trial design considerations. The randomized trial was designed to allow crossover from nonsurgical to surgical care after the 6-month visit was complete, because it was assumed that, for the target patient population, response to NSM could be inadequate for many patients. This was indeed the case, and by 12 months, nearly 80% of subjects in the NSM group crossed over to surgical care; those subjects derived pain, disability, and quality of life benefits similar to those initially assigned to SIJ fusion.12 Due to high crossover rates, direct comparative data for 12-month outcomes were not available. For our analysis, we assumed that the differences observed at 6 months in the randomized trial persisted for 12 months. This assumption is reasonable as crossover subjects showed nearly no benefit at 6 months and trial subjects, on average, had experienced SIJ pain for 6 years. Moreover, NSM subjects who elected not to cross over derived no further benefit from treatment after month 6. Finally, the 12-month postsurgical outcomes in the randomized trial were nearly entirely replicated in a separate, large (n=172) prospective multicenter single-arm trial of the same device/procedure.13 Together, these findings validate the 1-year assumption our model used.
Third, absenteeism in the form of missed workdays is excluded from the analysis. Including missed workdays in our productivity estimates would likely result in double-counting, as earnings are sometimes mechanically linked to days worked. However, to the extent lost productivity from missed work is not captured by earnings differences, our findings could understate the productivity improvements associated with surgery.
Over the next 10 years, health care costs are expected to grow faster than incomes.34 In this environment, policymakers will likely be aggressively searching for sources of cost savings. Back surgery and other orthopedic procedures have high direct medical costs and utilization rates that vary significantly across geographic regions.35 These factors may result in elevated scrutiny toward back surgery in the coming years. Basing insurance coverage policies solely on direct medical expenditures can result in unintended consequences.36 In this study, we find that SIJ fusion provides incremental improvements in health and functional status relative to nonsurgical managements, and that these improvements likely result in indirect cost savings that significantly offset net direct medical costs associated with the procedure. Payers and policymakers should consider these factors when making policies that affect access to the procedure.
Conclusion
For employees with chronic, severe SIJ dysfunction, minimally invasive SIJ fusion may improve worker productivity compared to NSM.
Disclosure
KNG Health Consulting was paid by SI-BONE for performing the research described herein. Daniel J Cher is an SI-BONE employee. The trial analyzed herein was sponsored by SI-BONE. SI-BONE manufactures a device used during minimally invasive SIJ fusion. The other authors report no other conflicts of interest in this work.
References
Cher D, Polly D, Berven S. Sacroiliac joint pain: burden of disease. Med Devices (Auckl). 2014;7:73–81. | |
Cher DJ, Reckling WC. Quality of life in preoperative patients with sacroiliac joint dysfunction is at least as depressed as in other lumbar spinal conditions. Med Devices (Auckl). 2015;8:395–403. | |
Sembrano JN, Polly DW, Jr. How often is low back pain not coming from the back? Spine. 2009;34:E27–E32. | |
Bernard TN, Jr, Kirkaldy-Willis WH. Recognizing specific characteristics of nonspecific low back pain. Clin Orthop Relat Res. 1987;(217):266–280. | |
Cohen SP, Hurley RW, Buckenmaier CC, 3rd, Kurihara C, Morlando B, Dragovich A. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008;109:279–288. | |
Patel N, Gross A, Brown L, Gekht G. A randomized, placebo-controlled study to assess the efficacy of lateral branch neurotomy for chronic sacroiliac joint pain. Pain Med. 2012;13(3):383–398. | |
Patel N. Twelve-month follow-up of a randomized trial assessing cooled radiofrequency denervation as a treatment for sacroiliac region pain. Pain Pract. Epub 2015 Jan 7. doi:10.1111/papr.12269. | |
Ledonio CGT, Polly DW, Jr, Swiontkowski MF. Minimally invasive versus open sacroiliac joint fusion: are they similarly safe and effective? Clin Orthop Relat Res. 2014;472:1831–1838. | |
Ledonio CG, Polly DW, Jr, Swiontkowski, MF, Cummings JT, Jr. Comparative effectiveness of open versus minimally invasive sacroiliac joint fusion. Med Devices (Auckl). 2014;7:187–193. | |
Smith AG, Capobianco R, Cher D, et al. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res. 2013;7:14. | |
Lorio MP, Polly DW, Jr, Ninkovic I, Ledonio CGT, Hallas K, Andersson G. Utilization of minimally invasive surgical approach for sacroiliac joint fusion in surgeon population of ISASS and SMISS membership. Open Orthop J. 2014;8:1–6. | |
Polly DW, Cher DJ, Wine KD, et al. Randomized controlled trial of minimally invasive sacroiliac joint fusion using triangular titanium implants vs nonsurgical management for sacroiliac joint dysfunction: 12-month outcomes. Neurosurgery. 2015;77(5):674–691. | |
Duhon BS, Cher DJ, Wine KD, Kovalsky DA, Lockstadt H; SIFI Study Group. Triangular titanium implants for minimally invasive sacroiliac joint fusion: a prospective study. Global Spine J. Epub 2015 Aug 11. | |
Heiney J, Capobianco R, Cher D. A systematic review of minimally invasive sacroiliac joint fusion utilizing a lateral transarticular technique. Int J Spine Surg. 2015;9:40. | |
Dall TM, Gallo P, Koenig L, Gu Q, Ruiz D. Modeling the indirect economic implications of musculoskeletal disorders and treatment. Cost Eff Resour Alloc. 2013;11:5. | |
Adams PF, Kirzinger WK, Martinez M. Summary health statistics for the U.S. population: National Health Interview Survey, 2012. Vital Health Stat. 2013;10:1–95. | |
Ware JEJ, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. | |
Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–2952; discussion 2952. | |
EuroQol Group. EuroQol – a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. | |
Heckman JJ. Sample selection bias as a specification error. Econometrica. 1979;47(1):153–161. | |
Schenker N, Raghunathan TE, Chiu PL, et al. Multiple imputation of missing income data in the National Health Interview Survey. J Am Stat Assoc. 2006;101:924–933. | |
Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8:8–20. | |
Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290:2443–2454. | |
Sadosky AB, Taylor-Stokes G, Lobosco S, Pike J, Ross E. Relationship between self-reported low-back pain severity and other patient-reported outcomes: results from an observational study. J Spinal Disord Tech. 2013;26:8–14. | |
McDonald M, DiBonaventura MD, Ullman, S. Musculoskeletal pain in the workforce: the effects of back, arthritis, and fibromyalgia pain on quality of life and work productivity. J Occup Environ Med. 2011;53:765–770. | |
Sadosky AB, DiBonaventura M, Cappelleri JC, Ebata N, Fujii K. The association between lower back pain and health status, work productivity, and health care resource use in Japan. J Pain Res. 2015;8:119–130. | |
Dagenais S, Roffey DM, Wai EK, Haldeman S, Caro J. Can cost utility evaluations inform decision making about interventions for low back pain? Spine J. 2009;9:944–957. | |
Johnsen LG, Hellum C, Storheim K, et al. Cost-effectiveness of total disc replacement versus multidisciplinary rehabilitation in patients with chronic low back pain: a Norwegian multicenter RCT. Spine. 2014;39:23–32. | |
Tosteson ANA, Skinner JS, Tosteson TD, et al. The cost effectiveness of surgical versus nonoperative treatment for lumbar disc herniation over two years: evidence from the Spine Patient Outcomes Research Trial (SPORT). Spine. 2008;33:2108–2115. | |
Fayssoux R, Goldfarb NI, Vaccaro AR, Harrop J. Indirect costs associated with surgery for low back pain – a secondary analysis of clinical trial data. Popul Health Manag. 2010;13:9–13. | |
Cher DJ, Frasco MA, Arnold RJG, Polly DW. Cost-effectiveness of minimally invasive sacroiliac joint fusion. Clinicoecon Outcomes Res. 2016;8:1–14. | |
Rudolf L, Capobianco R. Five-year clinical and radiographic outcomes after minimally invasive sacroiliac joint fusion using triangular implants. Open Orthop J. 2014;8:375–383. | |
Monaco K. Disability insurance plans: trends in employee access and employer costs. (2015). Available from: http://digitalcommons.ilr.cornell.edu/key_workplace/1395/?utm_source=digitalcommons.ilr.cornell.edu%2Fkey_workplace%2F1395&utm_medium=PDF&utm_campaign=PDFCoverPages. Accessed October 30, 2015. | |
Keehan SP, Cuckler GA, Sisko AM, et al. National health expenditure projections, 2014–24: spending growth faster than recent trends. Health Aff (Millwood). 2015;34:1407–1417. | |
Weinstein JN, Bronner KK, Morgan TS, Wennberg JE. Trends and geographic variations in major surgery for degenerative diseases of the hip, knee, and spine. Health Aff (Millwood). 2004;Suppl Variation:VAR81–VAR89. | |
Koenig L, Dall TM, Ruiz D, Jr, Saavoss J, Tongue J. Can value-based insurance impose societal costs? Value Health. 2014,17:749–751. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.