Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Process Evaluation of Prevention of Mother-to-Child Transmission of HIV Service at Gondar City Administration Governmental Health Facilities, Northwest Ethiopia: A Mixed Approach Case Study Evaluation Design
Authors Terefe B , Kebede A, Amare Muche G
Received 23 September 2021
Accepted for publication 14 December 2021
Published 24 December 2021 Volume 2021:13 Pages 1127—1147
DOI https://doi.org/10.2147/HIV.S340103
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Bassel Sawaya
Bewuketu Terefe,1 Adane Kebede,2 Getasew Amare Muche2
1Department of Community Health Nursing, School of Nursing, College of Medicine and Health Science, University of Gondar, Gondar, Amhara, Ethiopia; 2Department of Health System and Policy, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Gondar, Amhara, Ethiopia
Correspondence: Bewuketu Terefe Email [email protected]
Introduction: Mother-to-child HIV transmission (MTCT), or vertical transmission of HIV, is one mode of HIV transmission from mother to baby during pregnancy, delivery and after childbirth. The continuation of new pediatric HIV infection due to the improper prevention of MTCT is a challenge in developing countries; however, the program is not evaluated yet in Ethiopia. Therefore, this study was aimed to assess the process of PMTCT service implementation status.
Objective: This evaluation study evaluated the implementation of process levels and identified problems of PMTCT service at Gondar city administration governmental health facilities.
Methods: A case study evaluation design with a mixed method was conducted from March to May 2020. A systematic random sampling technique was used to select participants. Data were collected using an interviewer-administered questionnaire and document review, observation, and key informant interviews. Collected data were entered using EPI data version 7 and analyzed using SPSS version 25.
Results: The study found that, generally, the PMTCT program implementation was complying with the Ethiopian national guidelines by 78.32%. All facilities had most of the minimum required resources recommended by the guidelines by 75%. The services required to be provided by the facilities were highly accommodated by 90.18%, acceptable by 77.2%, with 78% compliance. Trained human resources and continuous supply of material are the main gaps.
Conclusion: The overall level of program implementation was judged to be good. However, there is a need for improvements such as ensuring the privacy of counselling rooms, availability of human, test kits, guidelines, beds, waiting areas, drugs, and refresher training for provider. Also, counsellors should record properly the services provided to clients in their cards, such as counselling sessions.
Keywords: process evaluation, PMTCT, HIV, health facilities
Background
Mother-to-child HIV transmission (MTCT), or vertical transmission of HIV, is one mode of HIV transmission from mother to baby during pregnancy, delivery, and after childbirth.1 About 95% of new infections in infants and young children come about through MTCT. It is estimated that the rate of HIV transmission from mother to child without any treatment intervention is 20–45%, and in terms of chances of transmission possibility over time is: 5–10% is in-utero, 10–20% is intrapartum, and 5–20% is through breastfeeding.1,2
Globally, an estimated 2.3 million children are living with HIV; of this, over 2.1 million children are living in sub-Saharan Africa with HIV, 120,000 AIDS-related deaths, and 160,000 new infections among children in 2016.3 Of all health crises in the African region, HIV/AIDS has attracted the most political support and resources. In 2016, 24% of pregnant women living with HIV did not have access to antiretroviral prophylaxis (ARVs) to prevent transmission to their infants.4 Globally, 120,000 children died due to AIDS-related illnesses in 2016; this equates to 328 deaths every day,4 and millions of more children indirectly affected by families and communities.5
Ethiopia has significantly expanded the HIV/AIDS interventions program packages during the last two decades by decentralizing the free charge of Highly Active Antiretroviral Treatment (HAART) in public facilities, private clinics, and hospitals on the whole. However, the burden of HIV/AIDS is still high and requires an enormous effort in the country.6 An estimated 25.7 million people are living with HIV, and around 1.1 million people were newly infected with HIV in 2018. Among these, only 64% of them have access to ARV.7
Overall, in the context of developing nations, the continuing HIV pandemic constitutes an immense enhancement risk to pregnant women, their infants, and their families as a whole. Even though PMTCT is part and parcel of HIV/AIDS services programs, developing and implementing a program complete with strategies for ante retroviral prophylaxis, safer childbirth, and safer infant feeding practices is a complex process.8 Significant and substantial reductions in new pediatric infections can be achieved as a result of high coverage with effective interventions for the prevention of mother-to-child transmission of HIV.9 Not enough evaluation has been conducted though; globally, more than 2.1 million children whose age is between 0 years and 15 years have been acquiring and living with HIV infection.10 Among all infected children, more than 90% of them are acquiring HIV infection through Mother to child transmission (MTCT); so far, an individual holds 14% of the total HIV/AIDS positive people. Approximately 330,000 children are newly infected with HIV every single year; most of the infections have occurred in sub-Saharan African countries, including Ethiopia in the top lists.11 Developing countries including sub-Saharan countries had scored a remarkable achievement in the fight off against vertical HIV transmission, even if the prior problem of their people is still now persistent.12
Different studies have revealed that paediatrics who have HIV infection in their blood via their mother will have more exposure to morbidity and mortality than HIV-free children.13 HIV/AIDS pandemic is the third most fatal disease for Ethiopians, according to CDC investigation.14 Other follow-up forms of several studies were conducted in Gondar, Jimma and Dire Dawa at PMTCT service areas revealed that 10–15% of infants found to be HIV infected, who are borne from known HIV+ mothers.15 Services for PMTCT have been applied in Ethiopia since 2001.16 It has seen a significant gain in PMTCT since the start of the program.17
Studies showed that the accessibility of tracer items for PMTCT services was low (41%), no health facility having all tracer items for PMTCT service found, and a 50% and 62% availability of guidelines for PMTCT and staff trained in the facilities, respectively.18 Prevention of mother-to-child transmission of HIV is our golden opportunity to reduce and eliminate the passing of HIV from the mother to her child because 90% of the total HIV infection in Africa are caused by MTCT.19 Different kinds of the literature showed that the infrastructures of any health institution’s staffing of facilities and capabilities of its staff, adequate and ventilated rooms for privacy, the policy environment in which care is delivered, and the availability of resources of the institution should be fulfilled and be monitored closely.20–23 To overcome these problems, several strategic plans should be investigated in the form of evaluation.24
To run a PMTCT service with high quality, the service needs an adequate space with auditory and visual privacy, labour and delivery unit, running water, and electricity supply.25 Many studies illustrated that adequate and safe space with the consideration of good auditory and visual privacy were not fulfilled, and these made the service poor in turn.24–26 To the minimum, any PMTCT service should fulfil test kits like rapid test kits recommended by the Ethiopian government health policy/guideline; drugs like never pine and cotrimoxazole are also among them.27 Essential supplies include clean gloves, sharps box, soap or another disinfectant, disposable needles, and household bleach among the top.28 HIV counselling and testing are parts of PMTCT packages because they have a great relationship with professionals’ knowledge and attitude. Developed nations applied it and reduced the MTCT, but in developing nations, including Ethiopia, counselling and testing are still under question.23,29–31 The literature stated that there is inappropriate infant feeding in sub-Saharan countries and they put a strong and continuous nutritional counselling both to the mother and their children during ANC and PNC is one soft option.32,33
Studies indicated that MTCT could be enhanced due to lengthwise rupture of membranes, episiotomies, invasive procedures of obstetrics care, and good care of maintaining mother’s safety is the first thing by the time these problems have occurred; even suctioning of the baby’s nose and airway might be good enough.34 This evaluation will make us detect whether the third prong of PMTCT program integration with other health services like ANC, PNC, L&D is implemented as written in the national PMTCT guideline, and if not so, it identifies where the gap has occurred, and we learn experience from it and improve the service to maintain the high-quality expectation of mother and their infants including male partners. This evaluation study will be the first of its kind in the evaluation area and will come up with several implementation issues from the different perspectives of health-care providers, users, the program itself, with a detailed contextual factor.
Evaluation Methods and Materials
Evaluation Area
This evaluation study was conducted in Gondar city Administration governmental health facilities where the PMTCT is implemented. Gondar city is among one of the 13 zonal towns of the Amhara regional state in northwest Ethiopia, and it is composed of 6 sub-cities, 25 kebeles (the smallest administration unit in Ethiopia), and 11 semi-urban kebeles. According to the City Administration population registration, Gondar currently has a population of about 700,000; however, the city health sector annual plan of Ethiopian Fiscal year (EFY) of 2012 has a total population of over 344,046 (Census 10 years ago); of these, 172,679 are females, and most of them are living in the Urban Kebele parts of it (266,640). The structure of the population is composed of, under 1 year of age: 10,700, under five: 46,586, reproductive-age females from 15 to 49 years: 81,126, and pregnant women consisting of 11,595. Gondar is situated, respectively, 185km and 738km from Bahir Dar, the regional state city, and Addis Ababa, the capital of the country, in a northwest direction. The city currently has eight and fourteen functional governmental health centres and health posts, respectively. All the health centres have begun to implement PMTCT of HIV service. Gondar poly centre is the first groundbreaker other than the remaining health centres next to the University of Gondar specialized hospital. Saint Gabriel, Mintiwab, and Bilajig are among the newly emerged health facilities in the implementation of PMTCT. In addition to these health facilities, the city has one Comprehensive Specialized hospital and more than 20 private health facilities. The city is bordered by Amba Giorgi’s woreda to the north, by Chilga and Dambia woredas to the west, by Gondar zuria woredato the east. The city has private hospitals, clinics, pharmacies, drug vendors, different community voluntary health workers or providers. Based on the city administration of health office reports, the health coverage is estimated at more than 95%.
Evaluation Design, Study Period, and Approach
A single case study design by applying both the quantitative and qualitative data collection was collected concurrently from March to May 2020. The formative evaluation approach was used to adjust and to increase the program’s intervention in a better way than ever.35
Populations
Target Population
The target population of the study was all mothers and their infants, all PMTCT program managers, and all health professionals providing PMTCT service in Gondar city administration health facilities, Gondar, Amhara Regional State, Ethiopia.
Source Population
The source population of this study included all mothers following PMTCT service, program managers, and health-care providers at PMTCT service who are working in the given health facilities.
Study Population
The study population of this study consists of mothers attending at PMTCT service, program managers, and health-care providers working at PMTCT service in Gondar city health facilities during data collection time, respectively.
Sample Size
Survey
The sample size for the client is calculated using the single population proportion formula (n = [(Zα/2)2 × P (1-P)]/D2) with the assumption of a 95% level of confidence, 5% margin of error, 87% rate of process evaluation result to PMTCT detected in Jimma, east-west Ethiopia,36 and a 15% non-response rate which yielded 201. Participants were selected using the systematic random sampling technique, and every patient was interviewed based on her order of arrival.
Document Review
For client card review, the sample size was calculated by using the single population proportion formula of 81% rate, which is found at Jimma, document review result. In computing sample size to achieve adequate precision, the sampling error/precision of the study was taken as 5% and 95% confidence intervals. Then the calculated sample size is 273 with 15% non-response rate consideration.
Key Informant Interview
Evaluation studies need multiple sources of data to explore the nature of the program. Therefore, to address the “why” the program is successful or not, evaluation questions; a key informant interview with PMTCT of HIV service leaders or managers and key stakeholders was conducted. The overall sample size was determined by the concept as per data saturation.
The Sample Size for Observation
Both provision of essential components PMTCT practice and provider–patient interaction were conducted with consecutive patients. It has four parts: pretest counselling, HIV negative pretest counselling, infant feeding options counselling, and related procedural activities. The sample size for observation of patient providers’ interaction was determined based on the saturation of information.
Sampling Procedure for Clients and Observation
There are nine health facilities in Gondar city that PMTCT is currently operating. The sample size is allocated proportionally for each health facility by the total population they are serving in the PMTCT service. To access clients, a systematic sampling technique was applied.
The client and provider interaction was observed through a non-participatory observation approach for information gathering regarding how the client was counselled, examined, and provided PMTCT services to assess the compliance of health-care providers regarding the PMTCT national standards. To prevent the Hawthorne effect, the first and the last three observations were discarded, respectively. Study participants for key informant interviews were selected purposively where information reaches people to get detailed and depth information. PMTCT program leaders or managers and other key stakeholders were interviewed to get their assumptions regarding the service.
Inclusion and Exclusion Criteria
Inclusion criteria: Health-care providers who are working at Gondar city governmental health facilities, PMTCT service, and all pregnant and breastfeeding women who are attending for PMTCT consultation during the data collection included.
Exclusion criteria: Group counselling and follow-up counselling sessions were excluded from the observation due to differences in tools supposed to be used. Whereas because of tool similarity, generic outpatient tools and job aids developed by CDC/WHO are supposed to be used for group counselling; which is the providers-initiated HIV counselling and testing (PIHCT) tool is supposed to be used for individual counselling.
Data Collection Tool and Procedure
An exit interview, questionnaire-guided interview, open-ended questions, checklist, review of documents, and tape recording were used to collect data. The questions on the explanatory variables were prepared using the standard conceptual model. The questionnaire was first prepared in English and translated to Amharic, the local language, and then retranslated to English to ensure the consistency of the tool. Specifically, training included the orientation to evaluation objective, materials, conversational style, observation techniques, simulation of data collection, how to handle any possible problems that were expected to arise during data collection time, and how to maintain confidentiality and privacy. After the translation of tools to the local language, pretesting was conducted at Debark district hospital in North Gondar Zone; the tools were refined based on the findings from the pretest study.
Semi-structured questionnaires were applied to determine mothers’ accommodation and acceptability of PMTCT service. The questionnaire was divided into three parts. The first one was socio-demographic related with five variables, the second part was accommodation related with six variables, and the last one was the acceptability of the program with four variables.
Structured observations were conducted. The observation has four parts, namely, pretest counselling, posttest counselling, infant feeding options counselling, and related procedural activities. Each four-part has seven, nine, twelve, and thirteen checklists.
A document was reviewed by using twenty related clinical variables to assess data recording quality and clarity of information.
Data Collectors
Three health-care providers, two Midwives, and one BSc Nurse, and three health graduate students in Midwifery and Nursing collected the data. Two supervisors have taken the responsibility of supervision to make consistent and to minimize the data collection error. The qualitative part of the data was gathered by the principal evaluator. All data collectors and supervisors took intensive and standardized training for two consecutive days.
Data Collection Fieldwork
There are nine PMTCT service health facilities in Gondar city, and for each, a data collector was assigned. Data were collected from each facility through resource inventory tool, interviewer-administered questionnaire, direct observation, key informant of program personnel. For all health facilities, the data collectors assessed every aspect of records, documents, and resources for the availability of drugs, equipment, treatment of complications. Resource inventory was conducted using the resource inventory checklist. It incorporated direct observation of resources. A survey was conducted through a structured questionnaire. The data collectors asked all eligible mothers attending PMTCT services. Direct observation: the observation was conducted until saturation was reached. Initially, the observer took consent from Program managers and stakeholders. The first and the last three observations were dropped to minimize observer bias.
Data Management/Processing and Analysis
For quantitative data: to ensure the quality of data care was undertaken in the process of data collection and analysis. During data collection, questionnaires were checked for their completeness daily by the data collectors and supervisors. Incorrectly filled or missed questionnaires were sent back to the respective data collectors for correction, and the supervisor submitted the filled questionnaire to the evaluator after checking its consistency and completeness. The evaluator also rechecked the completed questionnaires to maintain the quality of data. The data collected on a paper-based system were prepared and entered into the computer to facilitate and prepare it for statistical analysis. The collected data will be cleaned manually before it goes to a computer for its completeness, validity, and consistency as planned before. Incomplete and invalid data were reassessed or recollected again to obtain their real effects on the study variable.
Evaluation score was developed together with stakeholders during the evaluability assessment based on major things that were supposed to be available for the program to be successfully implemented. The weight of each indicator was given based on the relevant matrix developed, and due to commitments made, a consensus was reached to make cut-off points higher based on relevant stakeholders’ decisions, and the decision of judgment criteria are >90% = Very good, 75%–90% = Good, 65%–70% = Fair, <65% = Critical. The data were entered using Epi data and exported to SPSS version 25 and open code software for data analysis. Descriptive statistics were used to describe the data.
For qualitative data: qualitative data were collected by the principal evaluator for controlling data quality and for observation drop the first and last three observations for minimizing Hawthorne effect (observer bias) and observing one health-care provider in the morning and afternoon.
Evaluation Dissemination Plan
Once the data collection and analysis were complete, a report was prepared using a standardized structure; to meet ethical considerations, anonymity was maintained, and opinions of study subjects were respected. A preliminary discussion of evaluation results was conducted with stakeholders. A draft report was shared and discussed initially with stakeholders of the PMTCT program at Gondar city administration health facilities and Gondar city health office and expert for their comments. Incorporation of all relevant comments was done, and after the approval of the thesis, hardcopies of the evaluation report were disseminated to the University of Gondar and stakeholders. Evaluation’s findings are intended to provide timely, useful, and relevant information to managers, funders, government officials, and other stakeholders that lead to improvement programs, funding decisions, accountability, and learning. As such, the results of the evaluation must be communicated accurately and appropriately to enable the audience to make use of the information. The final findings of this evaluation results were disseminated to all the concerned stakeholders in different forms to the zonal and Gondar city health offices, CDC; findings will be send through email, hard copy forms, and also to the PMTCT clinic of each health facility it will deliver in hard copy form, meeting, email, and workshops form (if possible).
Results
Availability of Resources
The result part depicts the findings of resource inventory, patient record/chart review, client’s acceptability rate, observation of patient–provider interaction, and expert key-informant interview. This section also portrays the analysis of the judgment matrix in availability, compliance, and accommodation, and acceptability dimensions. Finally, it concludes with the judgment of both programs based on dimensions.
Trained Human Resources
All health facilities of Gondar city administration have twenty-nine physicians and ninety-nine midwives of the total 342. However, physicians were usually consulted in complicated cases. Even though there are not enough trained human resources, no nurses were assigned for PMTCT. But the guideline recommends that ART-trained nurses can provide counselling services in human-resource-limited settings. Guidelines require a minimum of 6 health-care providers trained in comprehensive PMTCT; however, across all nine health facilities, there were only 33 trained health providers. All providers received training on all topics except infant feeding counselling and infection prevention. The training duration ranged from 7 to 12 days. However, for the ANC/PMTCT section, there have been only a few health-care providers’ allocations across all health facilities since the introduction of PMTCT.
Most of the PMTCT service coordinators said that
we are attempting to make our best effort to provide services for the clients, but it is difficult to provide the services by allocating only a few providers. It is obvious that the workload has been increasing, since the introduction of the PMTCT services, there is not much support or additional incentive which we get for providing additional services such as counselling and HIV testing
and the other said that
to be honest, I do not think we have enough staff in terms of the number of patients we host. Existing health professionals are not adequately trained, and most of whom are diplomas.
Of course, the medical professionals we have may be adequate regarding other health centres, but if we see them through training and educational levels or rankings, it is hard to say enough.
Concerning supportive supervision, different stakeholders: PMTCT coordinators, heads of health facilities said that even if it is not well organized, there is supervision by different concerning bodies of such Gondar town health offices, central Gondar zone health offices, Amhara regional health offices, and by other non-governmental stakeholders, they have meetings to give feedback for each other
These are among the main gaps and barriers to why the program achieves such low results in the availability dimension.
Guidelines on PMTCT, PIHCT, Infant Feeding, and Family Planning
PMTCT and PIHCT guidelines were available in the health facilities, whereas the remaining two guidelines for infant feeding and family planning were observed to be missing. However, the available guidelines were not posted on a bulletin board so that they could be accessible and visible to all health providers. Different respondents had answered their feeling at the interview about whether providers use guidelines appropriately (Table 1).
 |
Table 1 Availability of Various Supplies and Equipments at Gondar City Governmental Health Facilities, Gondar, Northwest Ethiopia, June 2020 |
One interviewee, regarding with said that
no pretending is needed to answer this question because not all health professionals use the national guideline very often. This does not mean that they don’t work correctly. I think if anyone I consult as an expert uses the guidelines when it comes to service since it’s not only could enhance the confidence of the health professionals but also for patients’ satisfaction.
Provision of Counselling Sessions and Rooms
PMTCT counselling rooms in the dimension of auditory privacy, visual privacy, and separateness, across all health facilities only, visual privacy is fulfilled. Though all facilities have one PMTCT counselling room, it did not comply with the guideline. The length and width of most rooms are approximately three by two meters. Both rooms were packed out with materials and equipment. In addition to this, most facilities used different services of ANC, PNC, examination, and treatment rooms at the same place, except the University of Gondar specialized hospital.
The rooms were situated inappropriately and had no adequate light entrance. Only five rooms had a window but were blocked by a cupboard of patient cards. Each health facility’s observations which were done on the pretest, posttest, infant feeding options, and delivery sessions showed that none of all sessions did score a full range counselling according to this evaluation observational checklists.
Of the total, only two clients received a full range (100%) of counselling pretest counselling, posttest infant feeding, and delivery sessions revealed that all procedures were complying with the guidelines. Some important parts that scored more than 80% that the counsellors did explain are: discussing the benefits of testing, providing the test result, explaining that HIV can pass to the baby during delivery, and explaining that HIV can pass to the baby in the womb to the HIV-clients that HIV can pass to the baby in the womb; these are the highest score sessions which comply with the guideline in some way.
However, other remaining crucial parts are left without discussion by the counsellors, which included encouraging and supporting mothers, using visual aid during counselling to explain the danger of mixed feeding and early weaning, and using infant feeding tools scored the lowest percentage range from 49.3% to 61.6% (Table 2).
 |
Table 2 Observation of Counseling Sessions at Gondar City Health Administration Health Governmental Facilities, Gondar, Northwest Ethiopia, June 2020 |
Provision of ARV Prophylaxis for HIV Positive Pregnant Women and Their Infants
PMTCT and exposed infant treatment outcome monitoring logbook and HIV exposed infant logbook were reviewed. The review was done on 270 (among the total 273 sample size) HIV-positive pregnant women who were under PMTCT/ART services at least for the past six months during the study period. Among 270 clients, 243 (90%) were screened for CD4 count/percentage. More than 95% of clients were referred to ART services from PMTCT as they had the PMTCT code; other 27 clients either came for delivery at the facilities or delivered at home and came to the facilities later for either their treatment or infants’ treatment.
Availability of Safe Delivery Practice for HIV Positive Pregnant Women
Safe obstetrical practice for HIV+ pregnant women include having skilled health-care providers, following the standard precautions, avoiding the artificial rupture of the membrane to shorten labour, routine episiotomy, use of vacuum extraction and forceps if possible, and limitation of vaginal examinations during labour, treatment of acute chorioamnionitis, early infant eye and cord care. As written down on the table, only early infant eye and cord care complied with the guideline; the remaining did not react appropriately. In particular, safe handling and disposal of the placenta and solid materials and proper processing of used instruments scored <60%, which is the worst (Table 3).
 |
Table 3 Observation of Procedural Sessions at Gondar City Health Administration Governmental Health Facilities, Gondar, Northwest Ethiopia, June 2020 |
Test Kits, Laboratory Materials, OI and ARV Drugs
Resource inventory taken during the evaluation period in the last six months period showed that the test kits, laboratory materials, opportunistic infection (OI), and ARV drugs were observed to be available. However, most interviewed PMTCT coordinators and heads of each health facility said that all those above-listed resources were not available always “often there will be no test kits for around two weeks or more”. Laboratory materials such as reagents for syphilis testing were said not to be available for six months. Stock out of test kits and reagents were also said to be the reason not to provide some HIV and syphilis tests as it was seen in clients’ cards. There was no reported stock out of ARV drugs, but there was a shortage of OI drugs such as anti-fungal (cotrimoxazole syrup and tablets) for at least 2 weeks each month.
Availability of Materials and Supplies
Recent job aids and IEC materials were observed to be available in sufficient amounts across all health facilities. Infection prevention supplies such as protective clothing, sterilizing equipment, sterile gauze, PMTCT leaflets, stickers, reporting formats, gloves, disposable syringes and needles, sharp box, and autoclave were available and no stock out reported in the last six months; however, half of the facilities were having no running water, laboratory referral slips, and PMTCT brochures in the examination room. All family planning equipments were available, and no stock out was reported.
ANC and PMTCT equipments like fetoscopy, weighing scale, BP apparatus, height scale, and fundal height measurement were observed at ANC and PMTCT clinic. The resource inventory part showed that all ANC supplies like vitamin A, drugs to treat syphilis, malaria prophylaxis, and multivitamins, and iron, folic acid were available, and no stock out was reported during the last six months. But for immunization, mebendazole, and Tetanus toxoid, there was stock out for at least one week each month. Labour and delivery materials such as a delivery couch, delivery set/packs/kits, protective clothing, sterilizing equipment, antiseptics, cord ligatures, disinfectants, handwashing soaps, registration books, and reporting formats were observed to be available. However, most of the equipments are not available always due to different challenges.
Availability of Auditory and Visual Privacy of ANC/PMTCT Counselling Room
Observations were conducted that revealed that in PMTCT counselling rooms in the dimension of auditory privacy, visual privacy, and separateness, across all health facilities only, visual privacy is fulfilled, but they have windows and rooms. Though all facilities have one PMTCT counselling room, it did not comply with the guideline. The length and width of most rooms are approximately three by two meters. Both rooms were packed out with materials and equipment. In addition to this, most facilities used different services of ANC, PNC, examination, and treatment rooms at the same place, except the University of Gondar specialized hospital. The rooms were situated inappropriately and had no adequate light entrance. Only five rooms had a window but were blocked by a cupboard of patient cards.
Reporting and Recording Systems
Document review assessments were taking place from daily to annual reporting and recording systems of the facilities revealed that the weekly report is the lowest and the annual reporting way is the highest, which records 69.6% and 93.4%, respectively, which is judged very well even though there is a need for more constant fashion reporting and recording systems (Figure 1 and Table 4).
 |
Table 4 Observation of Document Review at Gondar City Health Administration Governmental Health Facilities, Gondar, Northwest Ethiopia, June 2020 |
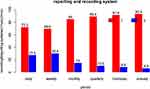 |
Figure 1 Observation of document review of reporting and recording systems at Gondar City Health Administration Health facilities, Gondar, northwest Ethiopia, June 2020. |
Accommodation of PMTCT Structure and Services
Socio-Demographic Characteristics
A total of 201 clients were interviewed. The age of respondents ranges from 15 to 49 years, with a mean age of 29 years (SD = 6.694). The majority, 175 (87.1%), of them were Orthodox Christian. One hundred and eighty-seven (93%) of them were Amhara in Ethnicity. Out of the total, 38 (18.9%) cannot read and write. The majority, 160 (79.6%), of the respondents were married. Housewives held the first rank, 56 (27.9%), and students are the least proportion, only 6 (3.0%) (Table 5).
 |
Table 5 Socio-Demographic Characteristics of Clients at Gondar City Administration Governmental Health Facilities, Gondar, Northwest Ethiopia, June 2020 |
Most of the clients, with an average of 146 (72.9%), were satisfied under the existing structure (Table 6).
 |
Table 6 Client Response About the Accommodation of PMTCT Services at Gondar City Administration Health Facilities, Gondar, Northwest Ethiopia, June 2020 |
Majority, 136 (69.1%) of the 200 respondents, said that they received their HIV test and other laboratory results within one hour; however, waiting to receive the test result takes up to 8 hours (Figure 2).
 |
Figure 2 Time spent by clients to get results at Gondar City Administration health facilities, Gondar, northwest Ethiopia, June, 2020. |
Accommodation of Mothers on the PMTCT Service
The degree of association among mothers’ accommodation the PMTCT service and independent variables were assessed by using the binary logistic model, and those variables scored less than 0.2 P-value were passed to the next multivariable logistic regression and clients whose age is between 15 and 19 are more interested by 1.32 (1.28–3.47) than clients whose age is >30 by the accommodation of the service. These variables were age, ethnicity, education, and occupation status (Table 7).
 |
Table 7 Bivariable and Multivariable Logistic Regression Analysis for the Accommodation of Mothers on PMTCT Services in Gondar City Health Facilities, Northwest Ethiopia, June 2020 (n = 201) |
Counselling Time Session of Health-Care Providers and Clients
Here, 30 of the 201 clients responded that they did not receive any pretest counselling from the providers and 25 of 171 said that there are things that did not make them comfortable. Among those uncomfortable situations are: too short a time for counselling, language barriers (providers use the English language during their conversation), not being allowed to talk to them, and not being trained to hold the majority part (Figure 3).
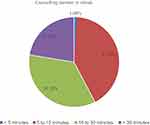 |
Figure 3 Time spent by clients for pretest counselling at Gondar City administration health facilities, Gondar, northwest Ethiopia, June 2020. |
Services That Need Improvement
Open-ended question forms were prepared for the clients to enable them to speak out what the health facility should need an improvement to make them happy and to enhance their accommodation satisfaction. They listed out various areas, including the waiting area, punctuality of the operation hours (Table 8).
 |
Table 8 Areas Where Improvement is Required for PMTCT Program According to Clients at Gondar City Administration Health Facilities, Northwest Ethiopia, June 2020 |
Acceptability of PMTCT Services
Acceptances of Pregnant Women Towards PMTCT Services Provision
Clients were interviewed on their general attitude on the provision of the PMTCT services. Responding to whether they will come back for the PMTCT services at the same clinic, the majority, 141 (70.13%) out of 201 respondents, said yes. Providers were friendly to clients, and hence, 180 (89.6%) of 2001 said that they could recommend the services to friends. Clients have also assessed their preferences on HIV pretest counselling during their ANC follow-up time, and 158 (78.6) of 201 respondents preferred the service for the sake of their children’s health by preventing opportunistic infection, starting medication, knowing their health status, and so forth (Table 9).
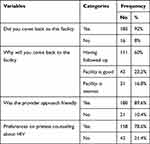 |
Table 9 Client Response About the Acceptability of PMTCT Services at Gondar City Administration Health Facilities, Gondar, Northwest Ethiopia June 2020 |
HIV Positive Pregnant Women Who Delivered Within the Health Facility
Data showed that women attending their ANC follow-up and delivered within the same health facility are very low except University of Gondar comprehensive and specialized hospital (100%) and Gondar poly health centre (75%). The reviewed PMTCT and exposed infant treatment outcome monitoring logbook has revealed that from 93 HIV pregnant women who were referred to ART from PMTCT for the past six months, only 23 delivered within the health centres, and they got all necessary facilities. The data did not include the University of Gondar comprehensive and specialized hospital, which performed much more than the others. The overall judgment matrix has shown the program’s process is good (78.32%) (Table 10).
 |
Table 10 Judgment Matrix and Analysis for PMTCT Program Evaluation at Gondar City Administration Health Facilities, Gondar Northwest Ethiopia, June 2020 |
Discussion
PMTCT service of this study was assessed based on availability, compliance, acceptability, and accommodation dimensions. Resource inventory, record review, patient acceptability rate, and observation of treatment and counselling sessions were examined to determine the clinical implementation of PMTCT service.
Generally, the provision of PMTCT services based on the four dimensions complied with the Ethiopian national guidelines by 78.32%. However, this discussion was based on specific areas of availability of resources, compliance, and accommodation of services, and acceptability of the service provision against the Ethiopian national guidelines for PMTCT. Out of the nine health facilities, University of Gondar hospital, Tseda, and Maraki health facilities have adequate room than the remaining. Overall, most had two crowded rooms with inadequate light and ventilation with no adequate privacy of visual and auditory. The health of PMTCT service must have adequate light and ventilation to prevent TB infection. Some other facilities did not have a separate room for counselling and examination. According to Ethiopia PMTCT and ART guidelines, every ART-providing health facility should have private counselling and examination room.37 This finding is in line with a study conducted in Addis Ababa, and possible reasons might be political and economic factors.25
Sufficient resources were available at all health facilities, with the University of Gondar hospital the highest and Bilajig health centre with low resources for the provision of PMTCT program, judged a good 75%. Training of health providers usually covers PMTCT, HCT, safer obstetric, infant feeding options, family planning counselling, ART, laboratory automation, DTG optimization, and infection prevention. This is different from what is expected by the Ethiopian national guidelines in human capacity development in the category of clinicians (midwives, nurses, medical doctors, and health officers), whereby they are required to be capacitated into 14 areas.37,38 The national PMTCT Guidelines recommend a minimum of 6 health-care providers trained in comprehensive PMTCT, a requirement which was highly fulfilled by the facility; however, on average, there were only four full-time health providers who are trained in PMTCT. All facilities have more or less a minimum of 5 midwives, but all midwives did not take the training. This study has the same findings as a qualitative study conducted in Lesotho and Sub-Saharan Africa review. Possible reasons might be poor economy and political commitment as well as the educational level of residents.39,40 On the other hand, a study conducted by WHO showed facilities that have increased and addressed human resource scarcity, including the use of deploying trained health-care professionals, community health workers, health extension workers, and by establishing community networking systems and make good communication with other stakeholders have a chance of great achievements.39 Because facilities did not commit on the above-listed strategies, the study found low scores. The University of Gondar has more trained providers but compared with the population, what they are serving is not greater than other facilities. WHO recognizes the need to strengthen health systems, including human resources capacity and monitoring capabilities, to maximize the quality and long-term benefits of therapy, but all health facilities have a shortage of trained health-care providers and no physician or other specialized field health provider across all the eight health centres.41
Availability of PMTCT, PIHCT, infant feeding, family planning, VCT, and IMCI (adapted to (HIV)) guidelines is predetermined in the national guidelines as one of the minimum requirements in the initiation and sustaining integrated PMTCT service delivery at the health facility level. The guidelines emphasized that to ensure full implementation of comprehensive PMTCT, the guidelines must be available in all health-care facilities providing PMTCT services and to those planning to provide them. All health facilities had a shortage of guidelines for IMCI, infant feeding and family planning, test kits, reagents, opportunistic infection drugs, iron, and folic acid, whereby its absence in the facilities affected general service provision; however, all have PMTCT and HMIS guidelines.42 Provisions of pretest, posttest, and infant feeding options were complying with the guidelines by 76.12%, 71.68%, and 71.8%, respectively, with a total complied of 83.4%. However, there were missed opportunities in recordings of the rest of provided services; for instance, it was found that more than 90% of ANC clients were recorded to be receiving post-testing for HIV against a client exit interview that showed that 78.6% of clients reported they had received pretest counselling. This is different from the national guidelines recommendations, which guide to record all services provided to support one of the principles of the PMTCT program. This study is almost similar to the same conducted in the Jimma zone.43 Recommended provision of percentage of available test kits, laboratory materials, OI, ARV Percentage of HIV+ pregnant women at ANC and delivery unit received recommended ARV prophylaxis was found to be 79.5% and 100%, respectively, with a complying achievement of 89.18%.
Client satisfaction was assessed as an accommodation dimension. The overall average satisfaction rate of the respondent was estimated at 90.18%. However, clients satisfied by those seven variables were lower than a study conducted in Adama and Kenya.44,45 Possible factors might be study setting and period, the number of factors and sample size. The guidelines require accommodation of services such as adequacy of working hours, the convenience of the waiting room, waiting time spent, and spacing for confidential counselling, and appointment system to be a key concern.46 This study found higher percentage than a study conducted in Jimma and Addis Ababa.46,47 But the study also found that among accommodation variables, time spent to see the provider, and convenience and waiting rooms/area are lower than the other parts and what the guideline-recommended, 71.1% and 77.6%, respectively. These, in turn, might have a relationship with the level of client satisfaction. Only 69.1% of 2001 clients received their results within an hour duration; this much less accommodated the above study conducted in Jimma,46 89.6, where the remaining clients were obligated to wait to get their results up to 8 hours. This is much prolonging compared with other studies and guidelines. Among the interviewees, one said,
Once a time we had assessed because many patients have withdrawal of their treatment follow up, they said to us despite the quality of your treatment, of patient acceptance and others are good and appreciable the place where the health centre is found, no priority is given to aged and needed clients, we forced to go to another facility without wanting to go and come. And if the city administration and office of the city health try to simplify the road of the clinic, the department of health centres is likely to be better suited than the others in the future
Compliance also was one of the dimensions of this study, and it aggregated by four different indicators, showed that 78% compiled with the guideline. Here, most of the providers do not have clear written policies, protocols, confidentiality training, and did not use the guidelines as recommended by the national guidelines; that is why these dimension components scored low achievement.
One PMTCT coordinator said that
no pretending is needed to answer this question because not all health professionals use the national guideline very often. This does not mean that they don’t work correctly. I think if anyone I consult as an expert uses the guidelines when it comes to service since it’s not only could enhance the confidence of the health professionals but also for patients’ satisfaction. I can say without a doubt that our clients are getting good treatment services in this health facility. You can go and see them in service. The reason they don’t use national guidelines, instructions and protocols are that we don’t have current guidelines in all sections. Secondly, because they think of using it as a waste of time and effort. Now there is some improvement.
This study was lower in HIV test coverage and linkage to care than a study conducted in Tanzania and South Africa. Possible factors might be health providers’ commitment and health-care systems of a country.48,49
Ultimately, we have to recognize that acceptability and use of maternity services are very low in Ethiopia.50 This is a limitation of this clients exit survey because only clients who came to the health facilities were interviewed for their satisfaction over accommodation and their acceptability to the program, which seems to be higher. However, here the opposite was found compared to the other dimensions in the aggregated indicator value.
Acceptability may be perceived as a prerequisite of utilization, which means it can be in a continuum of provision, acceptability, and utilization. From these findings, the high or the low level of acceptability in clients who attended the services provided at the health facilities does not mean necessarily that the community’s level of acceptability is high. Several of the organizational, political, cultural, education stock-out, and cost issues identified may be the reason.
This is a similar question as I mentioned to you earlier, but we are you sure we are increasing client’s expectations. Because all treatments preferences are based on their interest, and we are advising them all the time they need including by telephone.
Conclusion
Overall, the experience of all health facilities provided PMTCT service with a good result in complying with the national guidelines in terms of compliance, resource availability, accommodation of services, and acceptability. Providers did not use guidelines consistently, facilities did not have written policies and protocols, and the availability is good regardless few guidelines and job aids which were not available. Accommodation of services for the PMTCT program was also very good; this was highly contributed by the client’s satisfaction on the adequacy of working hours, convenience of the counselling room, spacing for confidential counselling, and appointment system. Acceptability, on the other hand, is fair in achievement.
Recommendations
It is better if health facilities consult the regional and Gondar city health office and development partners to request training on infant feeding counselling which was the only training that was found not to be provided to the counsellors as required by the guidelines. Health facilities should fulfil all the necessary resources for their better achievement. It will be better if facilities have separate rooms for testing and counselling. Attention and supervision should be given on the completeness of recording and reporting formats. Providers should be punctual, listen to clients, allow responses to them out, and talk in client’s local languages, and use guidelines. Supervisions should come back with feedback after the visit. Regional and city administration should ensure a continuous flow of resources, especially test kits, reagents to health facilities.
Strength and Limitation of the Evaluation
Since the study came with a strong design with a multi-source of data, it could go in-depth about the process of PMTCT service. The possible limitations might be that since this is a single case study design, it is not possible to generalize to other PMTCT sites. Counsellors may act differently when they are observed. Again, because this was a facility-based survey conducted only for clients who were attending the services, this may not provide the full range of opinions of pregnant women and acceptability of services to the whole community because many mothers are pregnant but did not attend the PMTCT service. However, the evaluator made exhaustive efforts to find the best available data because inevitably, some of the information needed might be incomplete or conflicting. To minimize the possible limitations of the evaluation, the evaluator dropped out the first and last three observation results; for documentary inventory, fully readable documents were assessed. Insufficient similar evaluation studies in developing countries created difficulty in contrasting the result on evaluation dimensions.
Data Sharing Statement
Data supporting the findings in this paper are available upon reasonable request from the corresponding author, and the summary data are available in the main document.
Ethical Consideration
Ethical approval was obtained from the University of Gondar, College of Medicine and health sciences, Institute of Public Health ethical review committee with Ref. No 14/02/2020. The University of Gondar, College of Medicine and health sciences, Institute of Public Health ethical review committee approved the verbal consent process. Study participants were asked for their consent before asking for any information, and verbal informed consent was taken from every study participant. In addition, they were told that the information they gave in this study would be published anonymously and they were volunteers. The objectives of the study were explained to every study participant, and they were asked for information only after they gave their consent. No people were obligated to participate in the study without their consent. Information sheets and informed consent both in Amharic and English are confidential, and there is no need of writing the participants’ names. Clients attending at Gondar city health facilities PMTCT health facilities and all mothers attending PMTCT service, stakeholders, and health care providers, including program managers, were eligible for inclusion. This study was conducted following the Declaration of Helsinki.
Acknowledgments
The authors would like to thank the health facilities administrative officials for their valuable information and cooperation, and we are happy to thank data collectors for their collaboration throughout the data collection process.
Author Contributions
All authors contributed to data analysis, drafting, or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report that there are no conflicts of interest in this work.
References
1. World Health Organization. Manual on Paediatric HIV Care and Treatment for District Hospitals: Addendum to the Pocketbook of Hospital Care of Children. World Health Organization; 2011.
2. Mepham S, Bland R, Newell ML. Prevention of mother‐to‐child transmission of HIV in resource‐rich and‐poor settings. BJOG. 2011;118(2):202–218. doi:10.1111/j.1471-0528.2010.02733.x
3. Kimambo RG. College of Public Health and Medical Sciences. Jimma University; 2011.
4. HIV/AIDS JUNPo. Ending AIDS: Progress Towards the 90-90-90 targets. Global AIDS Update. UNAIDS; 2017.
5. HIV/AIDS JUNPo. Children and HIV Fact Sheet. Geneva, Switzerland: UNAIDS; 2016.
6. Gesesew HA, Ward P, Hajito KW, Feyissa GT, Mohammadi L, Mwangi L. Discontinuation from antiretroviral therapy: a continuing challenge among adults in HIV care in Ethiopia: a systematic review and meta-analysis. PLoS One. 2017;12(1):e0169651. doi:10.1371/journal.pone.0169651
7. WHO. HIV in the WHO African Region. WHO; 2018.
8. World Health Organization. Towards the elimination of mother-to-child transmission of HIV: report of a WHO technical consultation, 9-11 November 2010, Geneva, Switzerland. WHO; 2010. Available from: https://apps.who.int/iris/handle/10665/44638. Accessed December 22, 2021.
9. World Health Organization, UNICEF. Towards the Elimination of Mother-To-Child Transmission of HIV: Report of a WHO Technical Consultation, 9–11 November 2010. Geneva, Switzerland: World Health Organization, UNICEF; 2011.
10. Smith AD, Tapsoba P, Peshu N, Sanders EJ, Jaffe HW. Men who have sex with men and HIV/AIDS in sub-Saharan Africa. Lancet. 2009;374(9687):416–422. doi:10.1016/S0140-6736(09)61118-1
11. Tsehay AK. Risk of HIV and associated factors among infants born to HIV-positive women in northwest Ethiopia. Ethiop J Health Dev. 2019;33(1):876.
12. Federal HIV/AIDS Prevention and Control Office. HIV/AIDS Strategic Plan. Vol. 2015. Office (FHAPCO); 2020.
13. Obsa S, Dabsu R, Ejeta E. Rate of mother to child transmission of HIV and factors associated among HIV exposed infants in Oromia Regional State, Ethiopia: retrospective study. Egypt Pediatr Assoc Gazette. 2018;66(3):61–65. doi:10.1016/j.epag.2018.07.002
14. Goshiye D. Quality of Prevention of Mother-To-Child Transmission of HIV Service at South Wollo Zone Governmental Hospitals, Amhara Region, Ethiopia, 2018. Addis Ababa University; 2018.
15. Koye DN, Zeleke BM. Mother-to-child transmission of HIV and its predictors among HIV-exposed infants at a PMTCT clinic in northwest Ethiopia. BMC Public Health. 2013;13(1):398. doi:10.1186/1471-2458-13-398
16. Tegegne TK, Chojenta C, Getachew T, Smith R, Loxton D. Service environment link and false discovery rate correction: methodological considerations in population and health facility surveys. PLoS One. 2019;14(7):e0219860. doi:10.1371/journal.pone.0219860
17. UNAIDS. Global Plan Towards the Elimination of New HIV Infections Among Children by 2015. UNAIDS; 2011.
18. Canavan ME, Brault MA, Tatek D, et al. Maternal and neonatal services in Ethiopia: measuring and improving quality. Bull World Health Organ. 2017;95(6):473. doi:10.2471/BLT.16.178806
19. Kate UA, Chikee AE, Chinyere OM, Anthony O, Benjamin SU. Factors associated with access barriers to Prevention of Mother to Child Transmission (PMTCT) of human immune deficiency virus services in Private Hospitals in Enugu State, South East, Nigeria. Asian J Pregnan Childbirth. 2019;2:1–9.
20. Omondi MP, Ongo’re D, Ngugi E, Nduati RW. The quality of PMTCT services and uptake of ARV prophylaxis amongst HIV positive pregnant women in Kakamega district, Kenya. Afri J Pharmacol Therap. 2012;1(2). Available from: http://journals.uonbi.ac.ke/ajpt/article/view/1142. Accessed December 22, 2021.
21. Marseille E, Hofmann PB, Kahn J. HIV prevention before HAART in sub-Saharan Africa. Lancet (London, England). 2002;359(9320):1851–1856. doi:10.1016/S0140-6736(02)08705-6
22. Morris C, Bailey KJ. Measuring health care quality: an overview of quality measures. 2014.
23. Koto MV, Maharaj PJS. Difficulties facing healthcare workers in the era of AIDS treatment in Lesotho. SAHARA J. 2016;13(1):53–59. doi:10.1080/17290376.2016.1179588
24. Okello G. Quality of prevention of mother-to-child transmission of HIV services in Soroti District, Uganda. 2017.
25. Mirkuzie AH, Hinderaker SG, Mørkve O. Promising outcomes of a national programme for the prevention of mother-to-child HIV transmission in Addis Ababa: a retrospective study. BMC Health Services Res. 2010;10(1):1–10.
26. Abaynew YJ. Quality of prevention of mother to child transmission (PMTCT) Services in Dessie Referral Hospital, Dessie City Administration, Ethiopia: client perspective. Neonatal Pediatric Med. 2016;3:123.
27. Mirkuzie AH, Hinderaker SG, Mørkve O. Promising outcomes of a national programme for the prevention of mother-to-child HIV transmission in Addis Ababa: a retrospective study. BMC Health Serv Res. 2010;10(1):267. doi:10.1186/1472-6963-10-267
28. Maheswaran H, Bland RM. Preventing mother-to-child transmission of HIV in resource-limited settings. 2009.
29. Assefa Y, Damme WV, Mariam DH, Kloos HJ. Toward universal access to HIV counselling and testing and antiretroviral treatment in Ethiopia: looking beyond HIV testing and ART initiation. AIDS Patient Care and STDs. 2010;24(8):521–525. doi:10.1089/apc.2009.0286
30. Central Statistical Agency. Health Survey AA. Ethiopia, Calverton M, USA: Central Statistical Agency (CSA)[Ethiopia] and ICF; 2016.
31. De Cock KM, Fowler MG, Mercier E, et al. Prevention of mother-to-child HIV transmission in resource-poor countries: translating research into policy and practice. JAMA. 2000;283(9):1175–1182. doi:10.1001/jama.283.9.1175
32. Ejara D, Mulualem D, Gebremedhin S. Inappropriate infant feeding practices of HIV-positive mothers attending PMTCT services in Oromia regional state, Ethiopia: a cross-sectional study. Int Breastfeed J. 2018;13(1):37. doi:10.1186/s13006-018-0181-x
33. Yah CS, Tambo EJ. Why is mother to child transmission (MTCT) of HIV a continual threat to newborns in sub-Saharan Africa (SSA)? J Infect Public Health. 2019;12(2):213–223. doi:10.1016/j.jiph.2018.10.008
34. Hunt GM, Ledwaba J, Salimo A, et al. Prevalence of HIV-1 drug resistance amongst newly diagnosed HIV-infected infants-age 4–8 weeks, enrolled in three nationally representative PMTCT effectiveness surveys, South Africa: 2010, 2011–12 and 2012–13. BMC Infect Dis. 2019;19(1):787. doi:10.1186/s12879-019-4339-y
35. Royse DBA, Deborah KP, Logan TK. Program Evaluation: An Introduction.
36. Abaynew Y. Quality of Prevention of Mother to Child Transmission (PMTCT) services in Dessie Referral Hospital, Dessie City Administration, Ethiopia: client perspective. Neonat Pediatr Med. 2016;3(123):2.
37. Health FDRoEMo. National comprehensive and integrated prevention of mother-to-child transmission of HIV guideline. 2017.
38. Federal HIV/AIDS Prevention and Control Office FMoH. Guidelines for prevention of mother-to-child transmission of HIV in Ethiopia. 2007.
39. World Health Organization. Global Update on the Health Sector Response to HIV, 2014. World Health Organization; 2015.
40. Mutabazi JC, Zarowsky C, Trottier H. The impact of programs for the prevention of mother-to-child transmission of HIV on health care services and systems in sub-Saharan Africa-a review. Public Health Rev. 2017;38(1):1–27. doi:10.1186/s40985-017-0072-5
41. Working Group on Antiretroviral Therapy and Medical Management of HIV-Infected Children. Guidelines for the use of an antiretroviral agent in paediatrics HIV infection. Available from: http://AIDSinfo.nih.gov.
42. Elfiyos B. Process Evaluation of Pediatrics Antiretroviral Treatment Service in Selected Health Facilities of Addis Ababa. Ethiopia: Jimma University; 2013.
43. (BA) RGK. Process evaluation of HIV Prevention of Mother to Child Transmission Program (PMTCT) in Agaro Health Centre, Jimma Zone, Oromia. 2001.
44. Abayneh K, Mengistie B, Oljira L, Tiruye G. Clients’ satisfaction with services for prevention of mother-to-child transmission of HIV in public health facilities in Diredawa City, Eastern Ethiopia. HIV/AIDS. 2020;12:611.
45. Asefa A, Mitike G. Prevention of mother-to-child transmission (PMTCT) of HIV services in Adama town, Ethiopia: clients’ satisfaction and challenges experienced by service providers. BMC Pregnancy Childbirth. 2014;14(1):1–7. doi:10.1186/1471-2393-14-57
46. Oleske J, Scott G. Working Group on antiretroviral therapy and medical management of HIV-infected children convened by the NPHRC, HRSA, NIH. 2001.
47. Elifiyos B. Process evaluation of paediatrics antiretroviral treatment service in selected health facilities of Addis Ababa, Ethiopia. 2013.
48. Gamell A, Luwanda LB, Kalinjuma AV, et al. Prevention of mother-to-child transmission of HIV option B+ cascade in rural Tanzania: the one stop clinic model. PLoS One. 2017;12(7):e0181096. doi:10.1371/journal.pone.0181096
49. Nicol E, Dudley L, Bradshaw D. Assessing the quality of routine data for the prevention of mother-to-child transmission of HIV: an analytical observational study in two health districts with high HIV prevalence in South Africa. Int J Med Inform. 2016;95:60–70. doi:10.1016/j.ijmedinf.2016.09.006
50. Central Statistical Agency. ORC Macro. Ethiopia demographic and health survey 2005. Addis Ababa, Ethiopia. Revised 1990 estimates of maternal mortality. 2006.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
