Back to Journals » Patient Preference and Adherence » Volume 12
Prior experience with cardiovascular medicines predicted longer persistence in people initiated to combinations of antihypertensive and lipid-lowering therapies: findings from two Australian cohorts
Authors Bartlett LE , Pratt NL, Roughead EE
Received 27 August 2017
Accepted for publication 28 February 2018
Published 16 May 2018 Volume 2018:12 Pages 835—843
DOI https://doi.org/10.2147/PPA.S150142
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Louise E Bartlett, Nicole L Pratt, Elizabeth E Roughead
Quality Use of Medicines and Pharmacy Research Centre, Sansom Institute for Health Research, School of Pharmacy and Medical Sciences, University of South Australia, Adelaide, SA, Australia
Purpose: Many studies of persistence involving fixed dose combinations (FDCs) of cardiovascular medicines have not adequately accounted for a user’s prior experience with similar medicines. The aim of this research was to assess the effect of prior medicine experience on persistence to combination therapy.
Patients and methods: Two retrospective cohort studies were conducted in the complete Pharmaceutical Benefits Scheme prescription claims dataset. Initiation and cessation rates were determined for combinations of: ezetimibe/statin; and amlodipine/statin. Initiators to combinations of these medicines between April and September 2013 were classified according to prescriptions dispensed in the prior 12 months as either: experienced to statin or calcium channel blocker (CCB); or naïve to both classes of medicines. Cohorts were stratified according to formulation initiated: FDC or separate pill combinations (SPC). Cessation of therapy over 12 months was determined using Kaplan–Meier survival analysis. Risk of cessation, adjusted for differences in patient characteristics was assessed using Cox proportional hazard models.
Results: There were 12,169 people who initiated combinations of ezetimibe/statin; and 26,848 initiated combinations of amlodipine/statin. A significant proportion of each cohort were naïve initiators: ezetimibe/statin cohort, 1,964 (16.1%) of whom 81.9% initiated a FDC; and amlodipine/statin cohort, 5,022 (18.7%) of whom 55.4% initiated a FDC. Naïve initiators had a significantly higher risk of ceasing therapy than experienced initiators regardless of formulation initiated: ezetimibe/statin cohort, naïve FDC versus experienced FDC HR=3.0 (95% CI 2.8, 3.3) and naïve SPC versus experienced SPC HR=4.4 (95% CI 3.8, 5.2); and amlodipine/statin cohort naïve FDC versus experienced FDC HR=2.0 (95% CI 1.8, 2.2) and naïve SPC versus experienced SPC HR=1.5 (95% CI 1.4,1.6).
Conclusion: Prescribers are initiating people to combinations of two cardiovascular medicines without prior experience to at least one medicine in the combination. This is associated with a higher risk of ceasing therapy than when combination therapy is initiated following experience with one component medicine. The use of FDC products does not overcome this risk.
Keywords: polypill, adherence, persistence, antihypertensive, lipid lowering therapy, statin
Introduction
There is good evidence to support the use of pharmacotherapies including antihypertensive and lipid-lowering medicines to reduce vascular events in at-risk patients.1–3 In patients who do not respond sufficiently to initial monotherapy, the addition of a second, and sometimes third, medicine may be required to achieve target blood pressure (BP) or lipid levels. Australian guidelines suggest initiation of monotherapy for hypertension and hyperlipidemia, with a second class of medicine added subsequently if required to achieve treatment targets.2,4 Further to this, where fixed dose combinations (FDCs) are considered appropriate, the NPS MedicineWise guidance5 and the Pharmaceutical Benefits Scheme (PBS) restrictions6 recommend stabilization on at least one component medicine contained in the combination prior to switching to a FDC formulation.
Prescribing guidance that supports the requirement to have experience with one drug before adding a second is consistent with quality use of medicines policy in Australia.7 The rationale being that individuals respond differently to medicines. For some people it may be unnecessary to start two drugs for the same risk factor, while for others who experience adverse events starting two at the same time makes it difficult to determine the causative agent.
Previous research on the use of antihypertensive medicines suggests that prescribers in Australia have not always followed local guidance in relation to initiating antihypertensive therapy.8–10 All three studies had investigated initial prescribing of combinations of antihypertensive agents, and found that 12.0%,8 21.0%,9 and 9.3%10 of initiators started two or more antihypertensive medicines without prior dispensing of any antihypertensive medicines. This may be because international guidelines1,11 differ to Australian guidelines for management of hypertension in that they support initiation to two antihypertensive medicines (including FDCs) in people with very high risk or markedly elevated blood pressure. The rationale being that FDCs of lower dose combinations lower blood pressure more rapidly than monotherapy, reduce side effects and are associated with higher adherence and persistence.12,13
Many studies that compare persistence between regimes of separate pill combinations (SPCs) and FDCs have found that FDCs are associated with longer persistence.14–20 However, a number of these studies have not adequately accounted for patients’ prior experience in taking medicines.16–20 One study considered patients’ prior experience with the actual medicines contained in the combination products but not the use of other similar-in-class medicines for the treatment of the same indication.19 Because prescriber guidance suggests stabilizing patients on individual components before switching to a FDC, patients are more likely to be prescribed FDCs following experience with a single medicine or even two separate medicines. Therefore, results from persistence studies that fail to adequately account for prior experience may be biased in favor of FDCs.
There is a theoretical basis for considering that prior experience with medicines will influence medicine-taking behaviors. Health behavioral change theories suggest that patients with prior experience to similar medicines are more likely to demonstrate improved adherence and persistence with chronic medication.21 In adopting new health behaviors, theories such as the transtheoretical model suggest patients progress through stages of readiness to change, before achieving sustained change, and that this process occurs over time.22 Patients new to treatment do not always pass through these stages in sequence.23–25 Some may move back and forward through these states as they fail and re-attempt to change their behavior. This corresponds with stops and restarts in medicine-taking behaviors as individuals come to understand their disease and the need for medicines. Increased persistence over the longer term occurs when skills such as remembering to take medicines and fill prescriptions become routine habits.26 The time to developing these habits may vary, but once developed habits have been found to predict subsequent persistence in experienced users of anti-hypertensives.27
Because prior experience is likely to affect persistence to chronic therapies, the aim of this research was to demonstrate the size of this effect in two cohorts of patients initiating combinations of cardiovascular medicines. We conducted an analysis of two cohorts initiating combination therapies with high volume use in Australia: ezetimibe plus statin; and amlodipine plus statin.28 Initiation to these combinations and therapy cessation rates were compared according to prior exposure and the formulation initiated (FDC or SPC). We hypothesized that people with prior exposure to medicines within the class would persist with therapy longer than those with no prior experience regardless of formulation.
Patients and methods
Study design and population
Two retrospective cohort studies were undertaken using the complete PBS prescription claims dataset that contains records for all Government subsidized prescriptions dispensed in Australia. The data analyzed included all dispensings for medicines supplied between April 2012 and December 2014. The PBS dataset includes patient demographics, medicine information, prescriber and dispensing information, and is described in more detail by Paige et al,29 and Van Gool.30 We identified two cohorts: patients supplied initial combination therapy of ezetimibe and statin; and patients supplied initial combination therapy of amlodipine and statin in the 6-month period from April to September 2013. Initiation was defined as no dispensing of the combination as either a SPC or FDC in the prior 12 months. Combination therapy was deemed to have started when both medicines were dispensed on the same day or within 30 days of each other. For the ezetimibe/statin initiators, patients were all naïve to ezetimibe, but may have filled prior statin prescriptions in keeping with the PBS restriction for use of ezetimibe as second line therapy. Initiators to amlodipine/statin may have filled either prescriptions for statins or calcium channel blockers (CCBs) prior to initiation but not both. The different inclusion criteria reflect the difference in the indications of these two combinations where ezetimibe is subsidized as second line treatment following statin therapy, and amlodipine and atorvastatin are both first line therapies for separate risk factors, ie, hypertension or heart failure and hyperlipidemia.
Each cohort was described according to prior use as: experienced if participants had received at least one prior dispensing for one class of medicine in the combination; or naïve having no dispensing of either class of medicine in the combination. Cohorts were further stratified according to formulation initiated: FDC; or SPC. All lipid-lowering and antihypertensive prescriptions for each participant were obtained for a minimum of 15 months follow-up.
The following medicines listed on the Pharmaceutical Benefits Schedule according to anatomical and therapeutic chemical codes were included in this study: all lipid-lowering medicines (C10); and antihypertensive agents (C07, C08C, C08D, C08G, C09AA, C09BA, C09CA, C09DA, C09XA, C09DX, C03AA).31
Ethical considerations
The design and methods for this study were approved by the Commonwealth Department of Human Services (DHS) External Request Evaluation Committee for analysis of PBS data. Additional approval to conduct these studies in the complete PBS dataset was obtained from the Department of Health. The study used de-identified data and conforms to management and release of data in accordance with the principals of the Australian Government Privacy Act, 1988.
Outcome measures
For each therapy (lipid lowering or antihypertensive) Kaplan–Meier analyses were performed over 12 months follow-up to assess the treatment duration of the first episode. Cessation to therapy was defined as a break of 60 days or more following exhaustion of the supply in the last dispensing for any lipid-lowering or antihypertensive medicines. PBS prescription durations were assigned as 30 days for all statins and 28 days for anti-hypertensives. This assumption was based on the 75th percentile for prescription refills for each medicine in the dataset. The 75th percentile also correlated well with the number of daily doses dispensed in a standard PBS prescription for most of these medicines. Length of treatment to any lipid-lowering therapy in the ezetimibe and statin cohort included time from initiation to cessation of all lipid-lowering medicines. For the amlodipine and statin cohort the length of treatment was the shorter duration of the two, ie, when combination antihypertensive and lipid-lowering therapy was ceased. All patients in each cohort had a minimum of 15 months follow-up and censoring occurred at study end where supply of prescriptions fell within the last 3 months.
A second Kaplan–Meier analysis was conducted where patients who received only one dispensing of either therapy were removed from the cohorts. This analysis included only those patients demonstrating “early stage” persistence to both therapies,32 and was conducted because cessation following the dispensing of the first prescription is likely to be in response to adverse effects which could bias results against naïve initiators.
Statistical analysis
The following baseline characteristics were determined at the time patients initiated combination therapy (index date): age; gender; concession status (concessional or general beneficiary); prescriber type (specialist physician or general practitioner); patients qualifying for the PBS safety-net in the 6 months either side of index date; the number of co-dispensed PBS medicines (co-dispensing is defined as the overlap of supply of PBS medicine[s] within the 75th percentile refill interval for each medicine); the number of comorbidities based on RxRisk-V index and medicines co-dispensed on index date.33 These patient characteristics were compared using chi square for differences in proportions and Wilcoxon rank sum tests for variables not normally distributed. Cox regression was used to model time to cessation of therapy between naïve and experienced user cohorts. Patient characteristics that differed between the two cohorts and considered potential confounders were included (stepwise) in the Cox proportional hazards models. The proportional hazard assumption was checked by visual assessment of graphs plotting the log of the negative log of the estimated survivor function against log. All analyses were conducted in SAS Enterprise Guide version 5.1.
Results
Overall, 12,169 people initiated combinations of ezetimibe/statin and 26,848 initiated combinations of amlodipine/statin. A significant proportion initiated these combinations naïve to either class of medicine: within the ezetimibe/statin cohort 1,964 (16.1%) were naïve users, of whom 81.9% initiated a FDC; and within the amlodipine/statin cohort 5,022 (18.7%) were naïve users, of whom 55.4% initiated the FDC (Figures 1 and 2).
  | Figure 1 Patient flow diagram for Cohort 1: ezetimibe and statin users. |
  | Figure 2 Patient flow diagram for Cohort 2: amlodipine and statin users. |
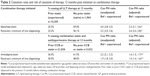
Naïve initiators in both cohorts were younger, had fewer comorbidities and fewer co-dispensed medicines, and were more likely to have their initial combination medicines prescribed by a general practitioner (Table 1A and B).
In the amlodipine/statin and ezetimibe/statin cohorts, cessation rates were significantly higher in those who initiated therapy naïve to both classes of medicines (Figures 3 and 4). Following adjustment for the different characteristics of the naïve and experienced populations, naïve initiators to combinations of amlodipine/statin and ezetimibe/statin were 1.6 and 3.3 times more likely (respectively) to cease therapy during the first 12 months of treatment (Table 2). The second persistence analysis, where patients who filled only one prescription at initiation of combination therapy were removed, confirmed these results; cessation rates remained significantly higher in naïve initiators in both the ezetimibe/statin and amlodipine/statin cohorts.
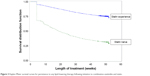  | Figure 3 Kaplan–Meier survival curves for persistence to any lipid-lowering therapy following initiation to combination ezetimibe and statin. |
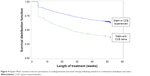  | Figure 4 Kaplan–Meier survival curves for persistence to antihypertensive and statin therapy following initiation to combination amlodipine and statin. |
When the two cohorts were stratified according to formulation initiated, all naïve initiators had significantly higher cessation rates compared to the corresponding experienced cohort regardless of whether a FDC or SPC was initiated (Table 3). Cessation rates at 12 months in naïve initiators of both formulations ranged from 60.4% to 69.0% and for experienced initiators, the cessation rates ranged from 19.5% to 38.0%.
Discussion
This study, which included the analysis of two separate cohorts, found that a significant number of people commenced combination lipid-lowering therapy or combination statin and anti-hypertensive who were naïve to both medicines. According to the PBS restrictions,34 the majority of the population eligible for combination ezetimibe/statin therapy should have at least trialed statin monotherapy before adding ezetimibe. Only a very small number of people, approximately 1/160,000 people35 with homozygous hypercholesterolemia were eligible to initiate combination ezetimibe/statin without prior experience to statin therapy. Our results raise the concern that many naïve initiators to ezetimibe/statin combinations may not be treated optimally with a statin and potentially prescribed ezetimibe unnecessarily.
Both the FDC and SPC formulations of amlodipine and statin medicines are registered in Australia for first line pharmacotherapy, however prescribing guidance5 and the PBS restriction36 recommend initiation of amlodipine and atorvastatin FDC after trialing a separate pill anti-hypertensive, ideally a CCB. Contrary to this restriction for subsidy, 18.7% of people initiating this combination had no dispensing of a CCB or statin in the prior 12 months.
As hypothesized, persistence to therapy was greater in those with prior experience of a medicine in class than in naïve users. Our results confirmed this and demonstrate the large effect prior experience can have on measures of persistence and therefore its potential to bias results in studies comparing this outcome. We found that those initiating either combination therapy as naïve users were younger and less likely to be concession card holders than those who initiated combinations experienced to one of the medicines within the class. Younger age and higher prescription costs have been associated with higher cessation rates in other studies of persistence to antihypertensive and statin therapy.37–39 We also found that naïve initiators were more commonly prescribed FDCs than SPCs. While the reasons that practitioners more frequently prescribe FDCs to naïve users are unknown; prescribers may assume FDCs will improve persistence in at-risk populations who are new to treatment. However, our results do not support this assumption because cessation rates in both FDC and SPC naïve initiators were similar and significantly higher than experienced initiators across both cohorts.
PBS data does not include information on adverse events therefore it is not possible to determine the reason why patients cease filling prescriptions and the extent to which adverse events contributed to cessation rates. To approximate the effect of adverse events we conducted a second persistence analysis where patients who filled only one prescription were excluded. This resulted in lower cessation rates in both cohorts. Despite this improvement, a significant gap between cessation rates of naïve and experienced users remained, indicating that adverse events only partially explained the difference. There may also be psychological reasons that explain the higher cessation rates in those naïve to combination therapy.40,41 As discussed in the introduction, behavior change theories predict that it takes time and practice to achieve persistence to therapy.22 Lack of opportunity to develop routine medicine-taking habits is likely to be a factor influencing the high cessation rates found in naïve initiators in these two cohorts.
The results of this study support current Australian prescribing guidance that promotes starting one new medicine at a time where clinically possible. Persistence may also be improved if patients new to chronic therapies are encouraged to link medicine taking to other daily routines to support habit forming behavior.27
The strengths of this study were the measurement of persistence to combinations of cardiovascular medicines in the entire PBS population. The PBS dataset included under co-payment prescriptions for general beneficiaries, providing almost complete capture of medicine use in the Australian population since April 2012. Two possible exceptions are medicines supplied as industry samples or as private prescriptions. The retrospective study design also meant that patients’ medicine-taking behavior was not affected by researcher contact, a potential source of bias in persistence studies that involve researcher or health professional and patient interactions.42 As the PBS dataset is complete from April 2012 onwards, we were limited to a 12-month look back period to determine prior use of similar in-class medicines. This may have slightly overestimated the proportion of naïve users, as a longer look back period of 2 or 3 years may have identified more people with prior exposure to these medicines, however, this would bias our results towards the null, given experienced users had longer persistence rates.
Other limitations of the PBS dataset are the lack of information on diagnosis, severity of illness and date of death. Not censoring for death is unlikely to significantly impact results as the average age was 56–69, and follow-up limited to 12 months. Finally, prescriber data are not linked to PBS data, therefore the extent of primary non-persistence (patients who don’t fill any prescriptions) was not captured in this study and the direction of this potential bias between experienced and naïve users is unknown.
Conclusion
This study found that almost one in five new users of combination cardiovascular therapies initiate two medicines together, and that these patients were at higher risk of ceasing therapy in the first 12 months of treatment compared to those who had been using at least one medicine within the class. We also found the use of FDCs was more common than SPCs in naïve initiators to combination therapy but that FDC formulations did not reduce the risk of ceasing therapy. Prescribers need to consider the higher risk of treatment cessation in new users regardless of formulation initiated and consider starting new medicines incrementally where possible.
Acknowledgments
All authors have completed the unified competing interest form at http://www.icmje.org/coi-disclosure (available on request from the corresponding author) and declare this work was supported by an Australian Government National Health and Medical Research Council (NHMRC) centre for research excellence in post-marketing surveillance of medicines and devices grant (GNT1040938).
Author contributions
Louise E Bartlett designed the research, analyzed the data, and drafted the manuscript. Elizabeth E Roughead and Nicole Pratt contributed to the research design, data analysis, interpretation, critical review and revision of the final manuscript. All authors have approved this version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
Louise E Bartlett is a part-time employee of the Commonwealth Department of Health. Elizabeth E Roughead is supported by an NHMRC Fellowship (GNT1110139). Nicole Pratt is supported by an NHMRC Early Career Fellowship (Grant Number GNT1035889). The authors report no other conflicts of interest in this work.
References
Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–2381. | ||
National Vascular Disease Prevention Alliance. Guidelines for the Management of Absolute Cardiovascular Disease Risk. Canberra Australia: National Stroke Foundation; 2012. Available from: https://www.heartfoundation.org.au/images/uploads/publications/Absolute-CVD-Risk-Full-Guidelines.pdf. Accessed January 28, 2018. | ||
James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (jnc 8). JAMA. 2014;311(5):507–520. | ||
National Heart Foundation of Australia. Guideline for the diagnosis and management of hypertension in adults. Melbourne: National Heart Foundation of Australia; 2016. Available from: http://heartfoundation.org.au/for-professionals/clinical-information/hypertension. Accessed January 28, 2018. | ||
NPS Medicinewise. Key points on fixed dose combination medicines: NPS Medicinewise; 2013 [updated 20 Dec 2013]. Available from: http://www.nps.org.au/topics/combination-medicines/for-health-professionals/key-points. Accessed January 28, 2018. | ||
Commonwealth Department of Health. Pharmaceutical Benefits Schedule pbs.gov.au, 2016. Available from: http://www.pbs.gov.au/medicine/item/9373H. Accessed January 28, 2018. | ||
Commonwealth Department of Health and Ageing. National Medicines Policy. Canberra ACT: Commonwealth Government; 2000. Available from: http://www.health.gov.au/internet/main/publishing.nsf/Content/national-medicines-policy. Accessed January 28, 2018. | ||
Gadzhanova S, Ilomäki J, Roughead EE. Antihypertensive use before and after initiation of fixed-dose combination products in Australia: a retrospective study. Int J Clin Pharm. 2013;35(4):613–620. | ||
Gadzhanova S, Roughead EE, Bartlett LE. Long-term persistence to mono and combination therapies with angiotensin converting enzymes and angiotensin II receptor blockers in Australia. Eur J Clin Pharmacol. 2016;72(6):765–771. | ||
Schaffer AL, Pearson S-A, Buckley NA. How does prescribing for antihypertensive products stack up against guideline recommendations? An Australian population-based study (2006–2014). Br J Clin Pharmacol. 2016;82(4):1134–1145. | ||
Leung AA, Nerenberg K, Daskalopoulou SS, et al. Hypertension Canada’s 2016 Canadian Hypertension Education Program Guidelines for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2016;32(5):569–588. | ||
Düsing R. The case for single pill combinations. Curr Med Res Opin. 2014;30(12):2423–2424. | ||
Bangalore S, Ley L. Improving treatment adherence to antihypertensive therapy: the role of single-pill combinations. Expert Opin Pharmacother. 2012;13(3):345–355. | ||
Baser O, Andrews LM, Wang L, Xie L. Comparison of real-world adherence, healthcare resource utilization and costs for newly initiated valsartan/amlodipine single-pill combination versus angiotensin receptor blocker/calcium channel blocker free-combination therapy. J Med Econ. 2011;14(5):576–583. | ||
Zeng F, Patel BV, Andrews L, Frech-Tamas F, Rudolph AE. Adherence and persistence of single-pill ARB/CCB combination therapy compared to multiple-pill ARB/CCB regimens. Curr Med Res Opin. 2010;26(12):2877–2887. | ||
Patel BV, Scott Leslie R, Thiebaud P, et al. Adherence with single-pill amlodipine/atorvastatin vs a two-pill regimen. Vasc Health Risk Manag. 2008;4(3):673–681. | ||
Panjabi S, Lacey M, Bancroft T, Cao F. Treatment adherence, clinical outcomes, and economics of triple-drug therapy in hypertensive patients. J Am Soc Hypertens. 2013;7(1):46–60. | ||
Simons LA, Ortiz M, Calcino G. Persistence with a single pill versus two pills of amlodipine and atorvastatin: the Australian experience, 2006–2010. Med J Aust. 2011;195(3):134–137. | ||
Xie L, Frech-Tamas F, Marrett E, Baser O. A medication adherence and persistence comparison of hypertensive patients treated with single-, double- and triple-pill combination therapy. Curr Med Res Opin. 2014;30(12):2415–2422. | ||
Machnicki G, Ong SH, Chen W, Wei ZJ, Kahler KH. Comparison of amlodipine/valsartan/hydrochlorothiazide single pill combination and free combination: adherence, persistence, healthcare utilization and costs. Curr Med Res Opin. 2015;31(12):2287–2296. | ||
Holmes EAF, Hughes DA, Morrison VL. Predicting adherence to medications using health psychology theories: a systematic review of 20 years of empirical research. Value Health. 2014;17(8):863–876. | ||
Prochaska JO. Transtheoretical model of behavior change. In: Gellman MD, Turner JR, editors. Encyclopedia of Behavioral Medicine. New York, NY: Springer; 2013:1997–2000. | ||
Munro S, Lewin S, Swart T, Volmink J. A review of health behaviour theories: how useful are these for developing interventions to promote long-term medication adherence for TB and HIV/AIDS? BMC Public Health. 2007;7:104. | ||
World Health Organization. Adherence to Long Term Therapies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003. Contract No.: ISBN 92 4 154599 2. | ||
Brawley LR, Culos-Reed SN. Studying adherence to therapeutic regimens. Control Clin Trials. 2000;21(5 Suppl):S156–S163. | ||
Reach G. Role of habit in adherence to medical treatment. Diabet Med. 2005;22(4):415–420. | ||
Alison Phillips L, Leventhal H, Leventhal EA. Assessing theoretical predictors of long-term medication adherence: patients’ treatment-related beliefs, experiential feedback and habit development. Psychol Health. 2013;28(10):1135–1151. | ||
PBS Information Management Section PPB. PBS Expenditure and Prescriptions twelve months to 30 June 2015. In: Health Do, editor. Canberra ACT: pbs.gov.au; 2015. Available from: http://www.pbs.gov.au/info/statistics/pbs-expenditure-prescriptions-30-june-2015. Accessed April 10, 2018. | ||
Paige E, Kemp-Casey A, Korda R, Banks E. Using Australian Pharmaceutical Benefits Scheme data for pharmacoepidemiological research: challenges and approaches. Public Health Res Pract. 2015;25(4):e2541546. | ||
Van Gool K, Parkinson B, Kenny P. Medicare Australia data for research: an introduction. In: Centre for Health Economic Research and Evaluation UoTS, editor. 2011, updated 2015. Available from: http://www.crest.uts.edu.au/pdfs/Factsheet-Medicare-Australia-UpdatedNov2015.pdf. Accessed January 28, 2018. | ||
World Health Organization. ATC Structure and Principles. Oslo, Norway: Norwegian Institute of Public Health; 2009. Available from: https://www.whocc.no/atc/structure. Accessed April 10, 2018. | ||
Raebel MAP, Schmittdiel JP, Karter AJP, Konieczny JLP, Steiner JF. Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases. Med Care. 2013;51(8 Suppl 3):S11–S21. | ||
Vitry A, Wong SA, Roughead EE, Ramsay E, Barratt J. Validity of medication based co-morbidity indices in the Australian elderly population. Aust N Z J Public Health. 2009;33(2):128–130. | ||
Commonwealth Department of Health. ezetimibe + simvastatin item 9484E pbs.gov.au: Department of Health; 2016 [updated October 2016]. Available from: https://www.pbs.gov.au/medicine/item/9484E. Accessed January 28, 2018. | ||
Baum SJ, Sijbrands EJG, Mata P, Watts GF. The doctor’s dilemma: challenges in the diagnosis and care of homozygous familial hypercholesterolemia. J Clin Lipidol. 2014;8(6):542–549. | ||
Commonwealth Department of Health. amlodipine + atorvastatin item 9055N pbs.gov.au Department of Health; 2016. Available from: http://www.pbs.gov.au/medicine/item/9055N. Accessed January 28, 2018. | ||
Qvarnström M, Kahan T, Keiler H. Persistence to antihypertensive drug treatment in Swedish primary healthcare. Eur J Clin Pharmacol. 2013;69(11):1955–1964. | ||
Poluzzi E, Strahinja P, Vaccheri A, et al. Adherence to chronic cardiovascular therapies: persistence over the years and dose coverage. Br J Clin Pharmacol. 2007;63(3):346–355. | ||
Knott RJ, Petrie DJ, Heeley EL, Chalmers JP, Clarke PM. The effects of reduced copayments on discontinuation and adherence failure to statin medication in Australia. Health Policy. 2015;119(5):620–627. | ||
Kronish IM, Ye S. Adherence to Cardiovascular medications: lessons learned and future directions. Progr Cardiovasc Dis. 2013;55(6):590–600. | ||
Berglund E, Lytsy P, Westerling R. Adherence to and beliefs in lipid-lowering medical treatments: a structural equation modeling approach including the necessity-concern framework. Patient Educat Couns. 2013;91(1):105–112. | ||
Lam WY, Fresco P. Medication adherence measures: an overview. BioMed Res Int. 2015;2015:217047. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.