Back to Journals » International Medical Case Reports Journal » Volume 12
Primary superior lumbar hernia፡ a rare cause of lumbar swelling
Authors Mekonnen AG , Gonfa KB
Received 7 October 2018
Accepted for publication 12 February 2019
Published 4 March 2019 Volume 2019:12 Pages 67—70
DOI https://doi.org/10.2147/IMCRJ.S178727
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Alemayehu Gonie Mekonnen,1 Kebebe Bekele Gonfa2
1Department of Nursing, College of Health Sciences, Debre Berhan University, Debre Berhan, Ethiopia; 2Department of Surgery, School of Medicine, Goba Referral Hospital, Madda Walabu University, Bale-Goba, Ethiopia
Background: Superior lumbar hernia is a rare posterolateral abdominal wall defect and herniation of abdominal contents through the superior lumbar triangle. A lumbar hernia is an unusual defect and only 300 cases of primary lumbar hernias have been reported since the first case report in 1731. To date, most clinicians are usually unfamiliar with the presentation of lumbar hernias, and the diagnosis is often done in a wrong way.
Case report: A 55-year-old female patient presented with complaints of right flank pain and swelling on the right lumbar region. On abdominal examination, there was round protruding swelling immediately beneath the 12th rib of the right upper flank area. The swelling was palpable and bowel sound was heard over it. The swelling was easily reducible and protruded when the patient was coughing or straining. The opposite side of the lumbar region was normal, and chest examination was clear and normal. The hematological and urine analysis laboratory findings were normal.
Discussion: The ultrasound finding revealed the bowel contents within the hernial sac. With the diagnosis of primary acquired superior lumbar hernia, the patient underwent open surgery. The defect was reduced back and repaired using a retro-muscular or sublay prolene mesh (15 cm by 7.5 cm). The patient was discharged at post-operative day four and followed-up for four months.
Conclusion: In conclusion, the diagnosis of lumbar hernias should be considered in all patients presented with complaints of flank pain and swelling in the flank area. In the absence of obvious swelling in the flank region, ultrasound investigation might not establish the diagnosis of lumbar hernias. Hence, ultrasound would be the option to confirm the diagnosis when the swelling is palpable.
Keywords: lumbar hernia, right flank pain, mesh repair
Background
The lumbar region is bordered superiorly by the 12th rib, inferiorly by the iliac crest, medially by the erector spinal muscles, and laterally by the external oblique muscle. The superior lumbar is defined medially by the erector spine muscle group, laterally by the internal oblique muscle, and superiorly by the 12th rib.1,2 Lumbar hernias are divided into two types according to the anatomical location of the defect: superior lumbar hernia and inferior lumbar hernia.3 Superior lumbar hernia (a Grynfeltt–Lesshaft hernia) is a rare posterolateral abdominal wall defect and a herniation of abdominal contents through the superior lumbar triangle.4
A lumbar hernia is an unusual defect and only 300 cases of primary lumbar hernias have been reported since the first case report in 1731.3,4 The causes of herniation could be congenital, primary, and secondary hernias. Congenital hernias are those that are discovered in infancy and comprise 20% of all lumbar hernias. These hernias are associated with rib and vertebral anomalies.5 Primary, or spontaneous, lumbar hernias comprise about 54% of the reported cases and are associated with age, rapid weight loss, chronic disease, muscular atrophy, and strenuous physical labor.5,6 Secondary, or acquired, lumbar hernias comprise 25% and are associated with trauma (blunt, penetrating, or crushing) surgery, and infections in pelvic bones.7 Lumbar hernias may contain fat, kidney, and intraperitoneal structures. It can be a rare cause of bowel obstruction due to the strangulation of bowel loops within the hernial sac.8
Clinically, lumbar hernias present as bulges in the posterior region of the abdomen and disappear with the prone position. Most patients complain of discomfort or pain in the lumbar region.1 The area of weakness can be detected by palpation, and occasionally bowel sounds on auscultation and percussion can be heard.1 To date, most clinicians are usually unfamiliar with the presentation of lumbar hernias, and the diagnosis is often done in a wrong way.
Case report
A 55-year-old female patient from Southeast Ethiopia, presented to Goba referral hospital with complaints of right flank pain and swelling on the right lumbar region. The pain was a dull ache and not associated with urinary complaints like dysuria, frequency, urgency or hematuria. She had no cough and chest pain.
The patient reported that she had been visiting more than three hospitals with complaints of right flank pain for the last eight years and had been taking an ultrasound, magnetic resonance imaging, renal function test, and urine analysis. However, the patient reported that the results of these investigations were normal, and she was only treated with different types of anti-pain medications. Four years later, the patient noticed that swelling on the right lumbar region, and the swelling had increased gradually and was associated with pain. She had no history of flank trauma, surgery, chronic constipation, and other abdominal infections. In addition, the patient had no history of chronic cough, difficulty of urination, and history of diabetes mellitus.
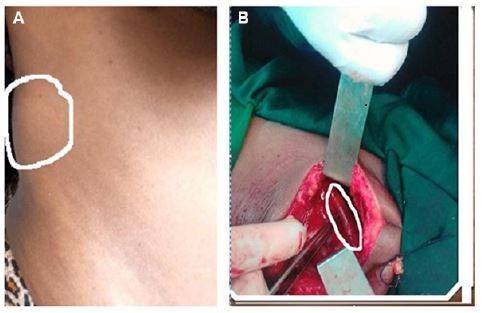
On admission, the patient was clinically active and had normal vital signs. On abdominal examination, there was round protruding swelling immediately beneath the 12th rib of the right upper flank region (Figure 1). The swelling was palpable and bowel sound was heard in the region. The swelling was easily reducible and protruded when the patient was coughing or straining. The opposite side lumbar region was normal, and chest examination was clear and normal. The hematological and urine analysis laboratory findings were normal. The ultrasound picture revealed the bowel contents within the hernial sac. Otherwise, all visceral organs were normal.
  | Figure 1 (A, B) Swelling or bulge on the right upper flank area (white circle). |
With the diagnosis of primary acquired superior lumbar hernia, the patient underwent open surgery. The open approach was designed due to the absence of laparoscopy services in the hospital. The defect was reduced back and repaired using a retro-muscular or sublay prolene mesh (15 cm by 7.5 cm) as this can maintain the maximum overlap of healthy tissue with the implanted mesh material. The patient was discharged at postoperative day four and followed up for four months. The patient had no recurrence of swelling at four months of follow-up.
Discussion
The confirmation of lumbar hernias was made in 1731. It is a rare case and accounts for less than 2% of all hernias in the abdominal wall.1 Superior lumbar hernia is more common than the inferior lumbar hernia.9 Regarding the clinical manifestation, the patients may present with a variety of signs and symptoms including mass/swelling in the flank area, lower back pain, and symptoms of bowel obstruction.3,10,14,15 Signs and symptoms of intestinal obstruction might also be present if a bowel loop has been incarcerated.10 The patient might complain about a backache, nausea, feeling of weight, or dragging sensation in the lumbar region.11 Sometimes patients might be presented with nonspecific abdominal pain or back pain which could represent sciatica.15 Likewise, the current case also presented with the complaints of right flank pain and had round protruding swelling immediately beneath the 12th rib of the right upper flank area. The swelling was palpable and bowel sound was heard over it.
When there is no obvious bulge in the flank region, ultrasound and magnetic resonance imaging may not establish the diagnosis of lumbar hernias. Ultrasound may confirm the diagnosis when the swelling is palpable.12 Computed tomography scan played the vital role in defining hernia contents accurately.14,16,17 This coincides with our case report in which the ultrasound and magnetic resonance imaging had not confirmed the lumbar hernia. Ultrasound confirmed the diagnosis of superior lumbar hernia when the swelling was noticed by the patient and palpable during physical examination.
Surgery is typically recommended to repair the defect and prevent complications.12 Either an open or laparoscopic procedure can be performed with equivalent success.13 However, the choice of the operative technique depends on the experience of the surgeon and the diameter of the hernia size.1 For primary spontaneous lumbar hernias, minimally invasive techniques are preferred.5 In the current case report, the patient underwent open surgery and the defect was repaired using an underlay prolene mesh. A similar technique has been reported by Sharma and Bhati17 and Ankush et al13 Even though the patient stayed for four days in the hospital and was followed-up for four months as an outpatient, finally, a good result was achieved. Therefore, an appropriate surgical treatment which shortens the length of hospital stay, lower consumption of analgesics, earlier return to normal activity, and less chance of wound infection should be planned.
Conclusion
In conclusion, the diagnosis of lumbar hernias should be considered in all patients that present with complaints of flank pain and swelling in the flank area. In the absence of obvious swelling in the flank region, ultrasound investigation might not establish the diagnosis of lumbar hernias. Hence, ultrasound would be the option to confirm the diagnosis when the swelling is palpable.
Ethical statement
We confirm that any aspect of the work covered in this manuscript that has involved experimental human patient has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. Institutional approval was not required for this manuscript.
Acknowledgments
We would like to thank our study subject for her participation in this case report. We also thank Mr Fetene Kassahun and Dr Seid Ahmed (English language instructor at Debre Berhan University, Ethiopia) for their English language editing support.
Disclosure
The authors report no conflicts of interest in this work.
References
Sanders JV, Cavalcante JB, Pereira IR, et al. Clinical and surgical anatomy of lumbar hernia: a review. Int Arch Med. 2017;11:10. | ||
Moreno-Egea A, Girela E, Parlorio E, Aguayo-Albasini JL. Controversies in the current management of traumatic abdominal wall hernias. Cirugia Espanola. 2007;82(5):260–267. | ||
Alves GR, de Andrade Silva RV, Corrêa JR, Haygert CJ. Grynfeltt-Lesshaft a hernia. Ann Gastroenterol. 2012;25(1):64. | ||
Petersen K, Snikeris J, Hall TS. Bleichner’s hernia – lumbar hernia. Am J Case Rep. 2013;14:26–29. | ||
Ramkaran C, Singh B. “Primary Grynfeltt’s-lumbar hernia” – a rare case. Indian J Clin Anatomy Physiol. 2016;3(3):382–384. | ||
Orcutt TW. Hernia of the superior lumbar triangle. Ann Surg. 1971;173(2):294–297. | ||
Stupalkowska W, Powell-Brett SF, Krijgsman B. Grynfeltt-Lesshaft a lumbar hernia: a rare cause of bowel obstruction misdiagnosed as a lipoma. J Surg Case Rep. 2017; 9:1–3. | ||
Hide IG, Pike EE, Uberoi R. Lumbar hernia: a rare cause of large bowel obstruction. Postgrad Med J. 1999;75(882):231–233. | ||
Dumlu E. Traumatic abdominal wall hernia after a blunt trauma; a case report. J Clin Anal Med. 2014;5(144):342–344. | ||
Hsu SD, Shen KL, Liu HD, Chen TW, Yu C. Lumbar hernia: clinical analysis of cases and review of the literature. Visceral Med. 2008;24(3):221–224. | ||
Radhakrishna V, Tanga SM. Bilateral superior lumbar hernias: a case report and review of the literature. Int Surg J. 2017;4(4):1472–1474. | ||
Sedik AM, Fathi A, Maali M, Hussein A, Elhoushy S. A traumatic lumbar hernia: case report and review of the literature. Saudi Surg J. 2017;5(2):84–86. | ||
Sarwal A, Sharma A, Khullar R, Soni V, Baijal M, Chowbey P. Primary lumbar hernia: a rare case report and a review of the literature. Asian J Endosc Surg. 2018;1(1):1758–5902. | ||
Light D, Gopinath B, Banerjee A, Ratnasingham K. Incarcerated lumbar hernia: a rare presentation. Ann R Coll Surg Engl. 2010;92(3): e13–e14. | ||
Mismar A, Al-Ardah M, Albsoul N, Younes N. Underlay mesh repair for spontaneous lumbar hernia. Int J Surg Case Rep. 2013;4(6):534–536. | ||
Goyal S, Singla S, Nakipuria DR. A spontaneous inferior lumbar hernia: rare case report and review. MOJ Surg. 2018;9(2):60–61. | ||
Sharma B, Bhati T. A rare case of lumbar hernia – a case report. J Dent Med Sci. 2017;16(11):5–8. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
