Back to Journals » Infection and Drug Resistance » Volume 15
Prevention and Treatment of Carbapenem-Resistant Organism Bacilli from Liver Transplantation Donors – Single Center Experience
Authors He L, Fu Z, Wang M, Wang X, Wang L, Li G, Lin D
Received 2 November 2021
Accepted for publication 14 December 2021
Published 6 January 2022 Volume 2022:15 Pages 47—52
DOI https://doi.org/10.2147/IDR.S346494
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Li He,1,* Zhi Fu,2,* Menglong Wang,2 Xin Wang,1 Lu Wang,1 Guangming Li,2 Dongdong Lin2
1Department of Intensive Care Unit, Beijing Youan Hospital, Capital Medical University, Beijing, 100069, People’s Republic of China; 2Department of General Surgery Center, Beijing Youan Hospital, Capital Medical University, Beijing, 100069, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Guangming Li; Dongdong Lin
Department of General Surgery Center, Beijing Youan Hospital, Capital Medical University, Beijing, 100069, People’s Republic of China
Tel +86 10 83997733
; Tel/Fax +86 10 83997733
Email [email protected]; [email protected]
Objective: To evaluate and explore the effectiveness of the new prevention and control measures for the donor-derived infection (DDI) associated with CRO after liver transplantation.
Methods: The data of 120 organ donors and recipients from January 2018 to May 2020 were retrospectively analyzed at The Liver Transplantation Center of Beijing Youan Hospital, Capital Medical University, to investigate the epidemiological status of CRO in donors. The cases were divided into two groups. The implemented group was treated according to the execution of a clustered CRO prevention and control measure based on active screening combined with early initiation of prophylactic/therapeutic administration of antibiotics. The effectiveness of the prevention and control measures was evaluated by comparing the length of postoperative ICU stay, total postoperative length of hospital stay, duration of ventilator use, duration of restricted antibiotics use, the incidence of DDI, incidence and composition distribution of DDI-related CRO, and incidence of severe DDI-relevant adverse events between the two groups.
Results: There was a high detection rate of 39.32% (105 strains) of drug-resistant bacteria in the donors. Fifty-six strains of CRO were detected. Participants in group B, which implemented the new prevention and control measures, were transferred out of the ICU sooner (P = 0.023), used fewer restrictive antibiotics (P = 0.003), and were discharged more quickly (P = 0.013) than those in group A. Postoperative DDI incidences (P = 0.113) and severe DDI-related adverse events were not statistically different between the two groups (P = 0.062). CR-Kp-related DDI was less common in group B (P = 0.021).
Conclusion: The situation of donor-derived drug-resistant bacterial infections remains critical. The clustered prevention and control measures for CRO based on active screening combined with early initiation of prophylactic/therapeutic application of antibiotics would be beneficial.
Keywords: organ donation, liver transplantation, drug-resistant bacteria, epidemiology, carbapenem-resistant Enterobacteriaceae, active screening, novel β-lactamase inhibitors
Introduction
Liver transplantation is an important treatment for end-stage liver disease (ESLD).1,2 The related surgical procedures, immune status of the recipient, host-graft alloimmune mechanisms, and donor-derived infection (DDI) greatly increase the risk of postoperative infection.3 Infections have been a major cause of postoperative mortality in liver transplantation.4 Organ donation from cardiac or brain-dead donors has become the primary source for organ transplantation centers. These donors are susceptible to various infections, especially drug-resistant bacterial infections, due to ICU admissions, undergoing major surgery, tracheostomy and mechanical ventilation, various medically invasive treatments or operations, and history of broad-spectrum antibiotics use,5 which makes the problem of DDI after transplantation more serious. Among all these problems, the adverse consequences of CRE infections are particularly prominent. Studies have shown a crude mortality rate of 25% to 71% due to CR-Kp infections after liver transplantation.6,7 The high morbidity and mortality associated with CRE infections increase the burden on families and society and result in the loss of precious transplanted organs. Therefore, there is a greater need for preventing and controlling donor-derived CRE infections after liver transplantation.
In the present study, the data of organ donors and recipients who underwent liver transplantation at The Liver Transplantation Center of Beijing Youan Hospital, Capital Medical University, were retrospectively analyzed to investigate the current epidemiological status of donor-derived CRO and to explore its prevention and control by evaluating effective, active screening measures adopted by our center since September 2019.
Materials and Methods
Case Entry and Grouping
Patients with heterogeneous in situ liver transplantation performed in our center from January 2018 to August 2019, and their donors were randomly grouped according to whether the new CRO prevention and control measures should have been taken. Liver transplantation recipients with routine infection monitoring organs were 65 in A, and new CRO prevention and control measures, 55 in B.
Group A were donors and recipients who underwent organ donation and heterogeneous in situ liver transplantation in our center from January 2018 to August 2019. They were given routine anti infection treatment and clinical infection index monitoring after operation. Group B were donors and recipients who underwent organ donation and heterogeneous in situ liver transplantation in our center from September 2019 to may 2020. The donors were screened by CRO. The donor was screened for CRO and decided whether to give anti CRO treatment according to the infection risk; The donor CRO positive and its receptor were isolated in a single room, anti CRO treatment as soon as possible, postoperative monitoring was strengthened, and the isolation was removed for three consecutive negative times to prevent nosocomial infection.
The General Characteristics of the Donors
A total of 120 donors were enrolled, including 104 males and 16 females, aged 51 (± 4) years. Among the donors, 78 (65%) had cerebrovascular disease, 31 (25.83%) had a traumatic craniocerebral injury, 10 (8.33%) had hypoxic-ischemic encephalopathy, and 1 (0.83%) had intracranial cartilaginous mucosal fibroma. The length of the ICU stay from the onset of disease to organ donation was seven (± 6) days, The median length of stay was 8 days.
The General Characteristics of the Recipients
A total of 120 recipients, including 102 males and 18 females, aged 55 (± 13) years, with allogeneic in situ liver transplantation for the first time at The Liver Transplantation Center of Beijing Youan Hospital, were included in the study. The prevalent disease in the recipients was 27 cases (22.5%) of cirrhosis, 25 cases (20.83%) of liver failure, and 68 cases (56.67%) of primary liver cancer.
4. Donors and recipients were all Chinese mainland China, which accords with the process and regulation of organ donation after the death of Chinese citizens. Organ donation and organ use were examined by organ transplant ethics committee. The donors and recipients gave informed consent, and the present study passed the ethical review for Beijing Youan Hospital, Capital Medical University. There was no difference in the data concerning the preoperative conditions between the two groups.
Methods
Prevention and Control Measures of the Donor-Derived CRE
Routine surveillance, prevention, and control: the vital signs, routine blood tests, hepatic and renal functions, C-reactive protein (CRP), and calcitoninogen (PCT) were monitored in the donors, and pathogenic cultures of blood, urine, sputum, drainage fluid, and organ preservation solution was performed as needed. Piperacillin-tazobactam was selected for the routine anti-infective therapy, with CRO therapy given to donors with CRO infection or high-risk infection.
The prevention and control measures based on active screening of CRO included: 1) Single-room isolation, hand hygiene; 2) addition of active preoperative screening of CRE with pharyngeal and rectal swabs for donors; 3) Drug-resistant bacteria monitoring of receptor blood, ascites, airway secretions and other samples; 4) early prophylactic or therapeutic antibiotic implementation for donors/recipients. For CRAB, Cefoperazone Sodium + Sulbactam Sodium combined with tigecycline was selected. For CRPA, piperacillin-tazobactam in combination with ciprofloxacin was selected. For CRE/CR-Kp, ceftazidime-avibactam was chosen as the fundamental therapy, combined with tigecycline and/or polymyxin, carbapenems (in case of minimum inhibitory concentration (MIC) < 8, increase the administration dose, with a single dosing duration > 3h), and adjusted according to the in vitro drug sensitivity test.
Observations
The Pathogenic Results (Only Include Donors’ Data)
These included the detection rate of drug-resistant bacteria, detection rate and CRO distribution in the donors.
Evaluation Indicators for the Effectiveness of the New Prevention and Control Measures of CRO Infection
The indicators for the effectiveness of the new measures were the length of postoperative ICU stay, the total length of postoperative hospital stay, duration of ventilator use, duration of restricted antibiotics use, the incidence of DDI, incidence and distribution of DDI-related CRO, and incidence of severe DDI-related adverse events.
Serious DDI-Related Adverse Event
A second required surgery for DDI, graft removal, or resulting in recipient death.
Diagnosis of DDI After Liver Transplantation
(1) The donor had clear CRO infection or colonization. (2) Within two week after the operation, the recipient specimens were cultured with CRO homologous to the donor. According to the diagnostic criteria for nosocomial infection, the comprehensive diagnosis was made according to the clinical manifestations and related laboratory examinations. (3) The test method were pathogen culture and drug sensitivity test.
Observation Time
DDI diagnosis time is within 2 week after liver transplantation; the overall observation time of the two patients is the complete hospitalization of the liver transplantation, the admission to discharge or death.
Statistical Analysis
Descriptive statistics were conducted for the results related to the donors’ pathogenesis, and the countable data were expressed as the number of cases (percentage). The SPSS 19.0 software was adopted for statistical analysis of the evaluation of the effectiveness of the new prevention and control measures of infection. Numerical data that conformed to a normal distribution were expressed as mean ± standard deviation, and the independent samples t-test was adopted for comparison. Numerical data that did not conform to a normal distribution were expressed as median (interquartile range), and the Mann–Whitney U-test was used for comparison. Countable data was expressed by rate, and comparison was conducted by the X2 test or Fisher’s exact test. P < 0.05 was considered statistically significant.
Results
Pathological Results of the Donors
A total of 267 strains of pathogenic bacteria were detected in 120 donor-related specimens and organ preservation solutions; 105 strains were drug-resistant with a detection rate of 39.32%. A total of 56 strains of CRO, 36 strains of Extended-Spectrum β-Lactamases (ESBL) producing drug-resistant bacteria, 12 strains of Methicillin-resistant Staphylococcus aureus (MRSA), and one strain of Vancomycin-resistant Enterococcus (VRE) were detected. The top two detection sites of drug-resistant bacteria were the airway secretions in 48 cases (45.71%) and organ preservation solution in 36 cases (34.28%).
Distribution and Epidemiological Trend of Donor-Derived CRE
A total of 56 cases of CRE were detected in 120 cases of donor and organ preservation solution, including 27 strains of CRAB (48.21%). There were 23 strains of CRE (41.07%), 82.6% of which were the CR-Kp (19) strains. There were six strains of CRPA (10.71%). The number of cases with CRAB and CR-Kp was significantly higher in group B due to the addition of pharyngeal and rectal swabs screening (Table 1). The most elevated detection site of CRE was the airway secretions in 28 cases (50%), followed by organ preservation solution in 15 patients (26.78%).
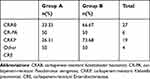 |
Table 1 Pathogenic Composition of CRO-Positive Donors in Both Groups |
The carbapenem resistance rate of donor Acinetobacter baumannii was 81.82% (9/11) in group A and 90% (18/20) in group B, P = 0.552; The carbapenem resistance rate of Pseudomonas aeruginosa was 37.5% (3/8) in group A and 27.27% (3/11) in group B, P = 1.00; The carbapenem resistance rate of Enterobacter was 21.21% (7/33) in group A and 16.16% (16/99) in group B, P = 0.508. There was no significant difference. The carbapenem resistance rate of gram-negative bacilli did not increase significantly (Table 2).
 |
Table 2 Carbapenem-Resistance Rate of the Gram-Negative Bacilli in the Donors of the Two Groups |
Postoperative Recovery and the Occurrence of Complicated DDI in Both Groups of Recipients
The length of postoperative ICU stay was 3 (2) days, the duration of restricted antibiotics use was 12.4 ± 7.39 days, and the postoperative length of hospital stay was 18 ± 10 days in group B, which were shorter than those in group A, with the introduction of new prevention and control measures. The differences were statistically significant (P = 0.023, 0.003, and 0.013, respectively, and all < 0.05). The duration of ventilator use was 28 (17) hours and 30 (26) hours in each group, respectively (P = 0.086 > 0.05), and the difference was not statistically significant (Table 3).
 |
Table 3 Comparison of Postoperative Recovery in Liver Transplant Recipients Between the Two Groups |
The incidence of postoperative DDI was 16.92% (11 patients) in group A and 7.27% (4 patients) in group B (P = 0.113). There were five (6/11) cases of CRE-DDI in group A and none (0/4) in group B (P = 0.021 < 0.05), the difference was statistically significant. There was no statistically significant difference in the incidence of CRAB-DDI and CRPA-DDI (P = 0.865, 0.790) and DDI-related adverse reactions (P=0.062) in the recipients between the two groups (Table 4).
 |
Table 4 Comparison of the Distribution of Postoperative DDI-CRO Infection and Incidence of Adverse Events in Liver Transplant Recipients Between the Two Groups |
Discussion
The rapid popularity and spread of carbon penicillin antibiotics in the medical establishment of CRE. CRE are among the most challenging antibiotic-resistant pathogens emerged in the clinical setting, due to their ability to spread rapidly in healthcare environments and to cause infections associated with high morbidity and mortality, for which very limited treatment options are available.8 Both WHO and CDC determine the CRO primary risk level.9 It was found that CRE transplantation or infection is closely related to the widespread use of carbon-penicillin antibiotics, long-term hospitalization, long ICU hospitalization, immunosuppressor use, and organ transplantation,9 so that the recipients are at high risk of CRE transplantation or infection.
For donors, there is often a history of ICU admission, major surgery, tracheostomy and mechanical ventilation, intubation of deep venous, the indwelling of urinary catheters, prolonged bed rest, and use of broad-spectrum antibiotics, making them vulnerable to various infections, especially drug-resistant bacterial infections.10 The distribution of infectious agents varies depending on the endemic region. In this study, a total of 267 pathogenic strains were detected in 120 donor-related specimens and organ preservation solutions, with 105 drug-resistant strains and a 39.32% detection rate of drug-resistant bacteria. A total of 56 CRO strains were detected, accounting for 53.33%. The highest detection site was airway secretions in 28 cases (50%), followed by organ preservation solution in 15 cases (26.78%).The high detection rate of drug-resistant strains in this study may be related to the detection of multiple strains from the same donor or infected donor. A foreign study several years ago11 included an active screening of rectal swabs for CRE and found a high rate of colonization there. In the present study, donors in group B underwent rectal swabs screening, and the detection of CRAB and CR-Kp was significantly higher.
Meanwhile, research shows that the trend of carbapenem-resistant highly virulent Klebsiella pneumoniae was increasing every year, and horizontal transfer of virulence genes might occur.12 These drug-resistant bacteria are highly pathogenic and have limited clinical options for antibiotics, which can easily cause adverse outcomes and even death. Thus, it is necessary to strengthen the understanding of CRO and carry out reasonable and effective prevention and control in the transplantation wards.
Infection prevention and control in liver transplant donor sources focuses on early detection, early intervention, and early treatment. Active screening is one of the essential measures in the prevention and control of CRO. Studies have shown that the intestines serve as a reservoir for Enterobacteriaceae and the colonization of the CRE strains is a significant risk factor for the migration to other parts of the body leading to infection.13 A previous study has shown that the incidence of the CRE intestinal carriers and non-carriers infections migrating to other sites was 16% and 3%, respectively.14 More effective prevention and control should be carried out based on active screening, including isolation between donor and recipient, hand hygiene, rational use of antibiotics, etc. Therefore, in this study, the implementation group B adopted cluster CRE prevention and control measures based on active screening to expose possible pathogens as early as possible and to target their prevention and treatment. Since infection control is the focus of postoperative treatment after liver transplantation, high-level broad-spectrum antibiotics are often applied for prolonged coverage, which is highly susceptible to antibiotic abuse and induces the development of drug-resistant bacteria. Compared with group A, the implementation group B had shorter use time of restricted antibiotics, shorter ICU and hospitalization time, and lower incidence of CRE related DDI. In the treatment of CRE related DDI, empirical application of ceftazidime and avibactam is beneficial. Therefore, the early detection, timely and strict prevention and control of infections, and the early application of sensitive antibiotics would be better for transplant patients, it also meets the requirement of optimizing the management of antibiotic use. Based on the above findings, it might be beneficial to include the recipients in the screening process, along with prevention and control, as early as possible, especially for donors and recipients who are at high risk for CRO. It will also reduce the occurrence of nosocomial infections to some extent, but this still needs further study.
Conclusion
The donor-derived drug-resistant bacterial infections remain a serious form of infection. CRE prevention and control measures based on active screening combined with early initiation of prophylactic/therapeutic application of antibiotics might be beneficial for CRE-related DDIs. Meanwhile, the effective application of combined avibactam could reduce the occurrence of CRE-related DDI.
Ethics Statements
All organs were donated voluntarily with written informed consent, and that the organ donations were conducted in accordance with the Declaration of Istanbul.
Funding
Hospital Management Center Key Medical Specialty Development Plan of Beijing (ZYLX202124). Science and Technology Development Project of Beijing Municipal Medical Research Institutes-Institute Cooperation (Y-2020H8-1).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hilmi IA, Al-Khafaji A, Damian D, Rosario-Rivera BL, Abdullah A, Kellum JA. Liberation from renal replacement therapy after cadaveric liver transplantation. Transplant Direct. 2016;2(11):e110. doi:10.1097/TXD.0000000000000622
2. Togashi J, Akamastu N, Kokudo N. Living donor liver transplantation for hepatocellular carcinoma at the University of Tokyo Hospital. Hepatobiliary Surg Nutr. 2016;5(5):399–407. doi:10.21037/hbsn.2016.08.05
3. Kaido T, Mori A, Ogura Y, et al. Pre- and perioperative factors affecting infection after living donor liver transplantation. Nutrition. 2012;28(11–12):1104–1108. doi:10.1016/j.nut.2012.02.007
4. Kim SI. Bacterial infection after liver transplantation. World J Gastroenterol. 2014;20(20):6211–6220. doi:10.3748/wjg.v20.i20.6211
5. Lin DD, Liu JN. Management of perioperative infection in liver transplantation. Beijing Med. 2017;39(9):895–896.
6. Lübbert C, Becker-Rux D, Rodloff AC, et al. Colonization of liver transplant recipients with KPC-producing Klebsiella pneumoniae is associated with high infection rates and excess mortality: a case-control analysis. Infection. 2014;42(2):309–316. doi:10.1007/s15010-013-0547-3
7. Satlin MJ, Jenkins SG, Walsh TJ. The global challenge of carbapenem-resistant Enterobacteriaceae in transplant recipients and patients with hematologic malignancies. Clin Infect Dis. 2014;58(9):1274–1283. doi:10.1093/cid/ciu052
8. Logan LK, Weinstein RA. The epidemiology of carbapenem-resistant Enterobacteriaceae: the impact and evolution of a global menace. J Infect Dis. 2017;215(suppl_1):S28–S36. doi:10.1093/infdis/jiw282
9. Tacconelli E, Carrara E, Savoldi A, et al.; WHO Pathogens Priority List Working Group. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18(3):318–327. doi:10.1016/S1473-3099(17)30753-3
10. Taminato M, Fram D, Pereira RRF, et al. Infection related to Klebsiella pneumoniae producing carbapenemase in renal transplant patients. Rev Bras Enferm. 2019;72(3):760–766. doi:10.1590/0034-7167-2019-0009
11. Moore NM, Cantón R, Carretto E, Peterson LR, Sautter RL, Traczewski MM; Carba-R Study Team. Rapid Identification of Five Classes of Carbapenem Resistance Genes Directly from Rectal Swabs by Use of the Xpert Carba-R Assay. J Clin Microbiol. 2017;55(7):2268–2275. doi:10.1128/JCM.00137-17
12. Zhang Y, Jin L, Ouyang P, et al.; China Carbapenem-Resistant Enterobacteriaceae (CRE) Network. Evolution of hypervirulence in carbapenem-resistant Klebsiella pneumoniae in China: a multicentre, molecular epidemiological analysis. J Antimicrob Chemother. 2020;75(2):327–336. doi:10.1093/jac/dkz446
13. World Health Organization. Guidelines for the Prevention and Control of Carbapenem-Resistant Enterobacteriaceae, Acinetobacter Baumannii and Pseudomonas Aeruginosa in Health Care Facilities. Geneva: World Health Organization; 2017.
14. Gorrie CL, Mirceta M, Wick RR, et al. Gastrointestinal carriage is a major reservoir of Klebsiella pneumoniae infection in intensive care patients. Clin Infect Dis. 2017;65(2):208–215. doi:10.1093/cid/cix270
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
