Back to Journals » Clinical Interventions in Aging » Volume 11
Prevalence of unknown and untreated arrhythmias in an older outpatient population screened by wireless long-term recording ECG
Authors Lindberg T , Bohman D, Elmstahl S , Jogréus C , Sanmartin Berglund J
Received 14 April 2016
Accepted for publication 21 June 2016
Published 10 August 2016 Volume 2016:11 Pages 1083—1090
DOI https://doi.org/10.2147/CIA.S110532
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Terese Lindberg,1,2 Doris M Bohman,1 Sölve Elmståhl,2 Claes Jogréus,1 Johan Sanmartin Berglund1
1Department of Health, Blekinge Institute of Technology, Karlskrona, 2Department of Health Sciences, Lund University, Lund, Sweden
Purpose: With longer life expectancies, the prevalence of arrhythmias is increasing; thus, there is a need for new methods to screen the older outpatient population. This population-based study describes the prevalence of arrhythmias in 200 outpatients aged ≥66 years. We also investigated the feasibility of wireless long-term recording (LTR) using the ECG-BodyKom®.
Methods: Two hundred elderly persons aged 66–93 years were recruited from the Swedish National Study on Aging and Care in 2010–2013, and data were collected via wireless LTR ECG-BodyKom.
Results: Screening with the LTR ECG revealed that persistent atrial fibrillation (AF) occurred in 10% of the outpatient population aged ≥66 years. Paroxysmal AF occurred in 5.5% of the population, with no difference between younger (60–80 years) and older (>80 years) elderly participants. Furthermore, all patients with paroxysmal AF had a CHA2DS2VASc score of ≥2 and were therefore potential candidates for follow-up and medical examination. LTR ECG-BodyKom can be considered a feasible method to screen for arrhythmias in older outpatient populations. This simple method requires little of the user, and there was high satisfaction with the equipment and a good overall experience wearing it.
Conclusion: The increasing occurrence of arrhythmias in the older population, as well as the high number of untreated cases of arrhythmias such as persistent AF and paroxysmal AF, poses a challenge for health care. Therefore, it is essential to develop effective strategies for their prevention and treatment.
Keywords: arrhythmia, older people, prevalence, wireless long-term ECG
Corrigendum for this paper has been published.
Introduction
Because older people constitute the fastest-growing proportion of the population in the industrialized world, the prevalence of arrhythmias is expected to increase.1 Consequently, arrhythmias represent a growing challenge for health care services.2,3 The onset of arrhythmia is often associated with other chronic diseases and may cause complications such as stroke. Abnormal electrocardiographic (ECG) findings are also seen in patients with syncope,4 a condition associated with twofold increased mortality in the population.5 Atrial fibrillation (AF) is a common arrhythmia that is reported to have a prevalence of 1.5%–3% in the general population in the developed world6,7 and ~20% in the oldest population.8,9 However, these statistics may underestimate the prevalence of AF, as this condition can be asymptomatic10 and screening is not routine.11 Furthermore, much of the knowledge concerning these findings is based on information obtained from inpatient populations and does not include persons ≥80 years old.12–14 These studies also represent preselected populations, which can be a source of bias.15 To prevent AF-related complications, it is important to address AF medically. Despite this, many patients with chronic AF and increased risk of stroke are not treated with anticoagulants, and undertreatment is especially common in females and patients ≥80 years old.5
The National Board of Sweden recommends cardiac screening in high-risk groups of patients and compares the cost-effectiveness of cardiac screening for cervical cancer. It also recommends that various methods for different populations to be screened should be evaluated.5 The most common way to screen for arrhythmias in the outpatient population is the use of traditional 24-hour ambulatory ECG devices, such as Holter monitors. However, there are also new long-term recording (LTR) ECG technologies in health care, such as thumb ECGs,16 which are aimed at the outpatient population.17 These newer devices have been shown to detect more arrhythmias than the traditional 24-hour ambulatory ECGs,18 which have relatively low detection rates19,20 and sensitivity, as revealed in a trial that included patients with implantable devices.21 The new wireless LTR ECGs allow for long-term monitoring from, for example, the patient’s home,18 and some devices can relay data over mobile networks in real time.22 This technology may be associated with improvements in treatment, time management, and diagnosis by enabling superior management in a timely manner.17 Like inpatient telemetry, they can allow for real-time analysis.23 However, these new devices often require active participation from the wearers, and therefore it can be difficult to detect asymptomatic AF.
It has recently been stated that disease-management programs with ECG equipment for home use and integrated telemedicine solutions will become increasingly important in ensuring safety and cost-effectiveness in health care.16 Therefore, in the present population-based study, we explored the prevalence of arrhythmias in 200 outpatients aged ≥66 years. We also examined the feasibility of using the new wireless LTR ECG-BodyKom® device to screen for arrhythmias.
Materials and methods
Study population
This study had a cross-sectional exploratory design. The study sample was drawn from the Swedish National Study on Aging and Care (SNAC). SNAC is a large, national, long-term, longitudinal, multipurpose study that involves four research centers and collects data in four different areas of Sweden24 to provide a general picture of the aging population. The present study acquired data from one of the four centers, SNAC-Blekinge (SNAC-B). The SNAC-B population consists of individuals ≥60 years old living in the Karlskrona municipality. Every month, a randomized sample of patients ≥60 years old were recruited from eleven age cohorts for medical and psychological examination at SNAC-B (~20–30 patients per month). During the period from April 2010 to December 2013, 612 participants were examined in the SNAC-B study. After power calculation and exclusion, 200 persons of the total 612 were recruited to test the LTR ECG-BodyCom®. Exclusion was based on persons who could not wear the equipment nonstop until the day after, participants who did not want to test the equipment, or if the equipment had technical problems. To compare the younger old and older old populations, the sample was divided into two age cohorts: 66–80 years and >80 years. For participation, after providing the written informed consent, participants had to wear the equipment nonstop from the day they were examined until the day after. The examiner also helped to choose participants after cognitive assessment, which included an Mini Mental State Examination test (score of >26 required for inclusion in the study). Participants were examined either at the SNAC-B research center or in their home (Figure 1).
  | Figure 1 Recruitment of the study population. |
Ethics
This project was conducted in compliance with the established ethical guidelines of the Declaration of Helsinki.25 The study received ethical clearance from the Regional Ethical Review Board in Lund to protect the interests of participants in the study (Drn LU 605-00 and LU 744-00). To ensure compliance with the Swedish Data Protection Act,26 data were stored securely and anonymized.
Data registration
To estimate the prevalence of arrhythmias, the wireless LTR ECG-BodyKom device (Kiwok Nordic AB, Stockholm, Sweden) was used. The equipment was applied to the patient at the end of the clinical examination, usually between 11 am and 4 pm, and removed the following day. Data were analyzed after recording was completed. The LTR ECG-BodyKom was compared previously with traditional 24-hour ambulatory ECG (Holter) to evaluate how well the two methods matched up with regard to the number of registered QRS complexes and to record transfer problems so that they could be rectified on a continuous basis.22 The equipment consists of a two-channel lead recording system with five electrodes attached to the participant’s chest and a sensor. The sensor transmits data via Bluetooth to a mobile telephone. Data were then transmitted across the mobile network and transferred to a database for storage before analysis with Cardio Explorer analysis software27 (Figure 2) and then manually overread by a specialist. The cost of each survey is ~110 euros, including equipment and interpretation of the ECG. The participants did not need to worry about the equipment while they had it on and were told to live their life as usual. Information about and history of cardiovascular risk factors, such as heart failure, hypertension, diabetes, stroke, ischemic cardiac disease, hypo/hyperthyroidism, medical treatment for AF, and smoking habits, were collected during the medical examination and questionnaires including a medical history. The medical examination included taking blood samples, resting ECG, examine blood pressure, and so on. Medical history, known AF, and anticoagulant use were not taken into consideration, and the examiner performing Mini Mental State Examination was not blinded to medical history. To examine how the LTR ECG-BodyKom was tolerated during the recording time, we conducted interviews in the form of questionnaires about usability. The questionnaire included multiple-choice answers to indicate level of agreement with the following statements: “The equipment was easy to use,” “I have been living normally during the past day,” and “Sleeping with the equipment worked well.”
  | Figure 2 Remote monitoring with the BodyKom® ECG device. |
Categorization of data
To describe heart rhythm, rate, and arrhythmias, the researchers categorized the data based on the Minnesota Code Manual of Electrocardiographic Findings.28 Heart rate: minimum, maximum, and mean rate; basic heart rhythm: sinus, pacemaker, chronic AF, ectopic atrial, and idioventricular rhythm; and episodes of paroxysmal AF/atrial flutter, tachycardia (>100 beats/min), bradycardia (<50 beats/min), and paroxysmal supraventricular tachycardia were recorded. Extra beats, pauses, and long RR intervals were also categorized. Causes were described as follows: interference in impulse formation as aberrant QRS, atrioventricular block, bundle branch block, and asystole.
Statistics
Descriptive statistical analyses were conducted to obtain an overview of the data. Prevalence figures are presented in age cohort groups, separately for males and females. Categorical data are presented as number and absolute frequency (percentage). Confidence intervals (CIs) (95%) were calculated for prevalence estimates. The continuous variables age and heart rate are presented as mean and SD. Differences between sex and age cohorts were calculated by the chi-square test for nominal data. Statistical analysis was performed with SPSS Version 22.0 (IBM Corporation, Armonk, NY, USA).
Results
Table 1 presents characteristics of the study sample, including sex, age, history of diagnosed heart failure, hypertension, diabetes, stroke, ischemic cardiac disease, hypo/hyperthyroidism, and smoking habits. Of the 200 patients included in the study, 112 (56.0%) were females. The mean age of the females was 75.2 years (SD ±7.4, range 66–90 years), whereas the mean age of the males was 77.0 years (SD ±8.1, range 66–96 years). There were 125 patients in the younger age cohort and 75 in the older age cohort. In the excluded population (n=412), 39% were males and 61% females. There were 32% in the younger age cohort and 68% in the older age cohort. The mean age of females was 83.8 years (SD ±8.9, range 65–102 years), while the mean age of males was 81.1 years (SD ±9.7, range 65–99 years; nonsignificant). In the included and examined population (n=200), heart failure was identified in eleven (5.5%) patients: eight females and three males. There was no statistical difference between the two age cohorts (six patients with heart failure in the 66–80 years group and five in the >80 years group, P=0.575). Ten patients (5%) had hypertension (three males and seven females). There were three patients in the 66–80 years group and seven in the >80 years group (P=0.559). Nine patients (4.5%) had diabetes, with no difference between age cohorts (six patients with diabetes in the 66–80 years group and three in the >80 years group, P=0.792). There was a history of stroke/transient ischemic attack in 6.5% of the sample (six males and seven females), with no difference between the age cohorts (P=0.951). Ischemic heart disease was found in 20 patients (10%; eleven males and nine females), with no difference between age cohorts (eleven patients in the 66–80 years group and nine in the >80 years group, P=0.465). Twenty patients had hyper/hypothyroidism (10%, 17 females and three males), with no difference between the age cohorts: ten in the 66–80 years group and ten in the >80 years group (P=0.224). Ten participants were smokers (five males and five females), with no difference between the age cohorts (P=0.575). The mean CHA2DS2VASc score for all included participants was 2.32 (range 1–7), while the mean CHA2DS2VASc score for all excluded participants was 2.77 (range 1–9), 3.15 for females and 2.25 for males. Heart failure was found in 7.5% of the population, 3.5% had diabetes, and there was a history of stroke/transient ischemic attack in 7.5% of the sample. Ischemic heart disease was found in 2.7% and hypertension in 11%.
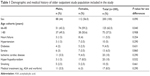  | Table 1 Demographic and medical history of older outpatient study population included in the study |
Mean heart rate for all participants was 72 beats/min. The mean heart rate was slightly higher for males (73.8 beats/min) than for females (72.7 beats/min). This difference was not significant (P=0.338). Heart rate fell below 50 beats/min in 62 cases; in most of these, bradycardia occurred only during the night. In 166 cases (83%), heart rate increased to >100 beats/min exclusively during the day in connection with physical activity.
Prevalence of essential arrhythmia in the study population
The results revealed persistent AF in 20 patients (10%); there was no significant difference between the two age cohorts. Nine (45%) of the participants with persistent AF received medical treatment (anticoagulants) for their condition, due to earlier diagnoses. Two patients (20%) with persistent AF had a history of heart failure, one (10%) had ischemic heart disease, none had a stroke, three (15%) had hyper/hypothyroidism, none were diabetics, and one (5%) had high blood pressure. There was no significant difference between males and females regarding sinus rhythm as basic rhythm (P=0.430). Sinus rhythm was detected in most of the population; the prevalence of paroxysmal AF/atrial flutter was 5.5%, and there was no difference between males and females (P=0.469). Furthermore, paroxysmal AF did not increase in the older cohort; the prevalence was 3% in the younger cohort and 2.5% in the older cohort (P=0.065). Of those with paroxysmal AF, 18% had a history of ischemic heart disease, 9% had heart failure, 9% were diabetic, 18% had hyper/hypothyroidism, and 9% had received medical treatment with acetylsalicylic acid. Among those with paroxysmal AF none were on medical treatment (anticoagulants) when detected, but all persons with paroxysmal AF had a CHA2DS2VASc score of ≥2 and were therefore candidates for follow-up and medical examination. These persons had not been previously diagnosed with paroxysmal AF. Ninety-two patients (46%) in the study populations had episodes of paroxysmal supraventricular tachycardia. Pauses occurred in 56% of the sample. Ventricular premature contractions occurred in 160 patients (81%), and supraventricular ectopic contractions occurred in 178 patients (89%), while another common arrhythmia, extra beats unspecified, occurred in 113 patients (56.5%). First- and second-degree AV block occurred in one man (0.5%) and second-degree AV block occurred in one man (0.5%) who was 78 years old (Table 2).
  | Table 2 Heart rhythm and prevalence of arrhythmia during the analysis period in the study population |
Feasibility of wearing the BodyKom
Table 3 presents information about the duration of recording with the wireless ECG system. An average recording time with the wireless sensor was calculated from >1.5 days of use. However, wireless recordings for those with shorter times were the result of terminations due to technical reasons (eg, the recorder aborted the recordings) and personal reasons (the electrode fell off or the person moved out of range of the telephone). None of the participants terminated the recordings of their own free will prior to the scheduled time, and compliance with the BodyKom was at a satisfying level. According to information obtained from interviews after the recording, 162 participants (81%) agreed that the equipment was easy to wear; only two persons (1%) disagreed. One hundred and sixty-four patients (82%) agreed that they lived their normal daily life while wearing the equipment. Furthermore, 155 participants (77.5%) thought that sleeping with the equipment worked well, only 1% disagreed. There were only an average of three equipment of BodyKom per day during the study period, but there were slots for four examinations per day in SNAC-B. This reduced the possibility of including all participants. The ECG recording quality of the wireless recorder was satisfactory, with almost negligible disturbances from artifacts, as long as the electrodes were properly attached to the person’s skin and the sensor was communicating with the telephone. Most of the participants wore the equipment for 12–24 hours. Analysis times ranged from 0.31 hours to 37.49 hours, and the mean time was 17.29 hours. The 95% CI for the mean time was 15.64–17.60 hours. There were no significant differences between males and females (P=0.464) or between the two age cohorts (P=0.564) regarding the recording time (Table 3).
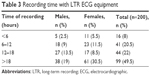  | Table 3 Recording time with LTR ECG equipment |
Discussion
The main findings of this study concerned the prevalence of persistent and paroxysmal AF in this older outpatient population. Other studies13–15,29,30 reflect the fact that the incidence of different arrhythmias increases with age but this expected age-related increased incidence is not seen in this study, probably due to small sample size or the already high age of our cohort. Sinus rhythm was the most common basic rhythm, but persistent AF occurred in 20 persons (10%), including six males and 14 females. Of these, ten persons were 66–80 years and ten were >80 years of age. Characteristics of the study sample, including sex, age, history of diagnosed heart failure, hypertension, diabetes, stroke, and ischemic cardiac disease, did differ between the included and excluded population. Among the study population testing the LTR BodyKom, 5% had hypertension compared to 11% of those excluded, and heart failure was identified in 5.5% compared to 7.5%, which may indicate that it was comparatively healthy individuals participating in the study and that the incidence of AF may be underestimated. Other studies have reported the prevalence of chronic AF in the general population to be 1.5%–3% in the developed world6,7 and have stated that chronic AF increases with age to ~20% in the oldest population.8,9 A recently published study that used intermittent ECG recording reported the occurrence of previously unknown AF in 3% of participants aged 75–76 years old.16 In addition, Rich31 reported that the incidence and prevalence of chronic AF increase progressively with age, and ~50% of patients with chronic AF are ≥75 years. The occurrence of chronic AF and a CHA2DS2VASc score of ≥2 should be addressed by medical treatment with oral anticoagulants.32 In the present study, only nine (45%) of those with persistent AF were receiving medical treatment with anticoagulants for their AF. Thus, their AF was previously diagnosed while the other eleven were undiagnosed, and they were therefore remitted to their family doctor for further examinations.
The ECG recording quality of the wireless recorder was satisfactory, with relatively negligible disturbances from artifacts. Its identification of arrhythmias was consistent with that of other long-term ECGs.2,33 This simple method requires little of the user and thus may be useful in screening the older population for arrhythmias. Although our data were gathered from a small population, they are indicative of the prevalence of arrhythmias in the elderly population. Questionnaire interviews with the participants revealed high rates of satisfaction with the equipment and a good overall experience wearing it. Participants did not need to worry about the equipment during the time they had it on. Problems reported by the participants included electrodes falling off during the night (2.5%), itching underneath electrodes (1%), and concerns about the technical equipment (3.5%). There are several types of ECG monitoring, including resting ECG, event recorders, and Holter ECGs. All of these have been tested extensively and are used in clinical environments.34 Holter monitors are often used as the standard method,18,19,35 although they have been shown to be more insensitive than implantable devices21 and do not offer, like the BodyCom®, the possibility of real-time analysis.19 Methods such as wireless LTR ECG have been shown to diagnose arrhythmias, including AF, with high sensitivity. Their ease of use not only facilitates screening for arrhythmias but may also help to improve quality of care for the older population. Screening may also be useful for identifying high-risk patients with clinically significant arrhythmias that require immediate admission to the cardiology ward. However, we must address the limitations we have mentioned earlier in this study. First, the number of analyzed persons was not very large and, therefore, the presented results must be considered with caution. A larger population allowing a more rigorous statistical analysis should be required in order to provide confidence in the robustness of this arrhythmia screening strategy. Second, we used registrations of only one day due to limited number of equipment; we do not know at present the most optimal registration time.
Conclusion
The present study shows that many older outpatients have undiagnosed and thus untreated persistent and paroxysmal AF. This is a challenge for health care providers, and it is essential to develop more effective strategies for the detection, treatment, and prevention of arrhythmias. This study confirms that the long-term wireless ECG recorder BodyKom has good feasibility for arrhythmia screening in older outpatient populations. Arrhythmia screening devices need to be simple to apply, and they must require little from those wearing them.
Acknowledgments
This project SNAC-B was part of the Swedish National study on Aging and Care (SNAC, www.snac.org), and it was financially supported by the Swedish Ministry of Health and Social Affairs. We are grateful to the participants and the participating country and municipalities. The authors received no financial support for the research, authorship, and/or publication of this article.
Disclosure
Johan Sanmartin Berglund is a board member of Kiwok Nordic AB. The authors declare no other potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
Axelsson C, Claesson A, Engdahl J, et al. Outcome after out-of-hospital cardiac arrest witnessed by EMS: changes over time and factors of importance for outcome in Sweden. Resuscitation. 2012;83(10):1253–1258. | ||
Hu S, Shao Z, Tan J [webpage on the Internet]. A real-time cardiac arrhythmia classification system with wearable electrocardiogram. In: Body Sensor Networks (BSN), 2011 International Conference on. IEEE; 2011 [cited October 12, 2014]. 119–124. Available from: http://ieeexplore.ieee.org/xpls/abs_all.jsp?arnumber=5955308. Accessed July 5, 2016. | ||
Kantelip J-P, Sage E, Duchene-Marullaz P. Findings on ambulatory electrocardiographic monitoring in subjects older than 80 years. Am J Cardiol. 1986;57(6):398–401. | ||
Brunetti ND, De Gennaro L, Dellegrottaglie G, Antonelli G, Amoruso D, Di Biase M. Prevalence of cardiac arrhythmias in pre-hospital tele-cardiology electrocardiograms of emergency medical service patients referred for syncope. J Electrocardiol. 2012;45(6):727–732. | ||
Socialstyrelsen [webpage on the Internet]. Nationella riktlinjer – Målnivåer – Hjärtsjukvård – Målnivåer för indikatorer; 2015 [cited November 26, 2015]. Available from: http://www.socialstyrelsen.se/publikationer2015/2015-10-3. Accessed July 5, 2016. | ||
Camm AJ, Lip GY, De Caterina R, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33(21):2719–2747. | ||
Björck S, Palaszewski B, Friberg L, Bergfeldt L. Atrial fibrillation, stroke risk, and warfarin therapy revisited a population-based study. Stroke. 2013;44(11):3103–3108. | ||
Heeringa J, van der Kuip DA, Hofman A, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J. 2006;27(8):949–953. | ||
Mosterd A, Hoes AW, de Bruyne MC, et al. Prevalence of heart failure and left ventricular dysfunction in the general population; The Rotterdam Study. Eur Heart J. 1999;20(6):447–455. | ||
Svennberg E, Engdahl J [webpage on the Internet]. Att leta efter förmaksflimmer–flera skäl finns för screening [cited December 8, 2015]. Available from: http://läkartidningen.se/EditorialFiles/SI/%5BDHSI%5D/DHSI.pdf. Accessed July 5, 2016. | ||
Zhang L, Gallagher R, Neubeck L. Health-related quality of life in atrial fibrillation patients over 65 years: a review. Eur J Prev Cardiol. 2015;22(8):987–1002. | ||
Hinkle LE Jr, Carver ST, Stevens M. The frequency of asymptomatic disturbances of cardiac rhythm and conduction in middle-aged men. Am J Cardiol. 1969;24(5):629–650. | ||
Ingerslev J, Bjerregaard P. Prevalence and prognostic significance of cardiac arrhythmias detected by ambulatory electrocardiography in subjects 85 years of age. Eur Heart J. 1986;7(7):570–575. | ||
Bjerregaard P. Mean 24 hour heart rate, minimal heart rate and pauses in healthy subjects 40–79 years of age. Eur Heart J. 1983;4(1):44–51. | ||
Raftery EB, Cashman PM. Long-term recording of the electrocardiogram in a normal population. Postgrad Med J. 1975;52:32–38. | ||
Svennberg E, Engdahl J, Al-Khalili F, Friberg L, Frykman V, Rosenqvist M. Mass screening for untreated atrial fibrillation: The STROKESTOP Study. Circulation. 2015;131(25):2176–2184. [CIRCULATIONAHA–114]. | ||
Kiwok [homepage on the Internet]. Kiwok; 2010. Available from: www.kiwok.se. Accessed July 5, 2016. | ||
Hendrikx T, Rosenqvist M, Wester P, Sandström H, Hörnsten R. Intermittent short ECG recording is more effective than 24-hour Holter ECG in detection of arrhythmias. BMC Cardiovasc Disord. 2014;14(1):41. | ||
Liao J, Khalid Z, Scallan C, Morillo C, O’Donnell M. Noninvasive cardiac monitoring for detecting paroxysmal atrial fibrillation or flutter after acute ischemic stroke a systematic review. Stroke. 2007;38(11):2935–2940. | ||
Culebras A, Messé SR, Chaturvedi S, Kase CS, Gronseth G. Summary of evidence-based guideline update: prevention of stroke in nonvalvular atrial fibrillation report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2014;82(8):716–724. | ||
Ziegler PD, Glotzer TV, Daoud EG, et al. Incidence of newly detected atrial arrhythmias via implantable devices in patients with a history of thromboembolic events. Stroke. 2010;41(2):256–260. | ||
Kennebäck C, Wredlert S, Jonsson S, Lind H, Teriö C. Sylvén. Technical report Tape recorder ECG re telemetric transfer … – Technical-report-Tape-recorder-ECG-re-telemetric-transferred-ECG-v1.00.pdf [Internet]. [cited November 24, 2015]. Available from: http://www.kiwok.se/Technical-report-Tape-recorder-ECG-re-telemetric-transferred-ECG-v1.00.pdf | ||
Rizos T, Güntner J, Jenetzky E, et al. Continuous stroke unit electrocardiographic monitoring versus 24-hour holter electrocardiography for detection of paroxysmal atrial fibrillation after. Stroke. 2012;43(10):2689–2694. | ||
Lagergren M, Fratiglioni L, Hallberg IR, et al. A longitudinal study integrating population, care and social services data. The Swedish National study on Aging and Care (SNAC). Aging Clin Exp Res. 2004;16(2):158–168. | ||
World Medical Association [webpage on the Internet]. Declaration of Helsinki. Ethical principles for medical research involving human subjects; 2009 [cited January 2, 2016]. Available from: http://philpapers.org/rec/ASSDOH. Accessed July 5, 2016. | ||
TSO [webpage on the Internet]. Data protection Act; 1998. Available from: www.tso.co.uk/bookshop. Accessed July 5, 2016. | ||
SR-Medizinelektronik [homepage on the Internet] [cited June 18, 2016]. Available from: http://www.sr-med.com/. Accessed July 5, 2016. | ||
Prineas RJ, Crow RS, Zhang ZM [webpage on the Internet]. The Minnesota Code Manual of Electrocardiographic Findings [cited December 2, 2014]. Available from: http://www.springer.com/medicine/cardiology/book/978-1-84882-777-6. Accessed July 5, 2016. | ||
Aronow WS, Epstein S, Koenigsberg M, Schwartz KS. Usefulness of echocardiographic left ventricular hypertrophy, ventricular tachycardia and complex ventricular arrhythmias in predicting ventricular fibrillation or sudden cardiac death in elderly patients. Am J Cardiol. 1988;62(16):1124–1125. | ||
KoSTIS JB, McCrone K, Moreyra AE, et al. Premature ventricular complexes in the absence of identifiable heart disease. Circulation. 1981;63(6):1351–1356. | ||
Rich MW. Epidemiology of atrial fibrillation. J Interv Card Electrophysiol. 2009;25(1):3–8. | ||
Jamshed N, Dubin J, Eldadah Z. Emergency management of palpitations in the elderly: epidemiology, diagnostic approaches, and therapeutic options. Clin Geriatr Med. 2013;29(1):205–230. | ||
Fensli R, Gundersen T, Snaprud T, Hejlesen O. Clinical evaluation of a wireless ECG sensor system for arrhythmia diagnostic purposes. Med Eng Phys. 2013;35(6):697–703. | ||
Davison J, Brady S, Kenny RA. 24-hour ambulatory electrocardiographic monitoring is unhelpful in the investigation of older persons with recurrent falls. Age Ageing. 2005;34(4):382–386. | ||
Bouchardy J, Therrien J, Pilote L, et al. Atrial arrhythmias in adults with congenital heart disease. Circulation. 2009;120(17):1679–1686. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
