Back to Journals » Journal of Blood Medicine » Volume 8
Prevalence of thrombocytopenia among pregnant women attending antenatal care service at Gondar University Teaching Hospital in 2014, northwest Ethiopia
Authors Asrie F, Enawgaw B , Getaneh Z
Received 5 March 2017
Accepted for publication 1 May 2017
Published 15 June 2017 Volume 2017:8 Pages 61—66
DOI https://doi.org/10.2147/JBM.S136152
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin Bluth
Fikir Asrie, Bamlaku Enawgaw, Zegeye Getaneh
Department of Hematology and Immunohematology, School of Biomedical and Laboratory Sciences, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Introduction: Thrombocytopenia is a common hematologic abnormality during pregnancy. Pregnant women with thrombocytopenia have a higher risk of bleeding excessively during or after childbirth, particularly if they need to have a cesarean section or other surgical intervention during pregnancy, labor or in the puerperium. The main aim of this study was to determine the prevalence of thrombocytopenia among pregnant women attending antenatal care service at Gondar University Hospital, northwest Ethiopia.
Materials and methods: A cross-sectional study was used to assess the prevalence of thrombocytopenia among pregnant women attending antenatal care service at Gondar University Hospital from January to April 2015. A total of 217 pregnant women were included in the study and a structured pretested questionnaire was used to obtain sociodemographic information, nutritional factors, obstetrics and gynecological factors, history and clinical condition. Blood samples were collected for platelet count and other platelet parameters, which were determined by using SysmexKX 21 automation. The data were entered to Epi info version 6 software and analyzed using SPSS version 20 software. Bivariable and multivariable statistical analyses were used to evaluate the effect of independent variable over the dependent variable. A p-value of <0.05 was considered as statistically significant.
Result: A total of 217 women receiving antenatal care service at Gondar University Hospital participated in the study. Thrombocytopenia among 19 pregnant women showed a prevalence of 8.8%. The mean ± standard deviation platelet count was 238.85×109/L (±74.57). Thrombocytopenia was significantly associated with patients who lived rurally (crude odds ratio =4.3, 95% confidence interval 1.48–12.76).
Conclusion: The prevalence of thrombocytopenia was 8.8% predominantly with mild type of thrombocytopenia. Thrombocytopenia was higher among pregnant women who lived rurally. Therefore, health care providers should screen routinely for thrombocytopenia to avoid excessive bleeding during pregnancy, especially in women who live rurally.
Keywords: thrombocytopenia, pregnant women, antenatal care, Gondar, Ethiopia
Introduction
Platelets are nonnucleated blood cells formed by cellular fragments of megakaryocytes, and they have a critical role in maintaining hemostasis.1 Thrombocytopenia is suspected when a patient’s platelet count is <150,000×103/mm3. The normal reference range for platelet count in a nonpregnant woman is 150,000–400,000× 103/mm3. Due to hemodilution secondary to expansion of plasma volume, platelet count in normal pregnancies may be decreased by ~10%; most of the decrease in platelet count occurs during the third trimester of pregnancy,2–5 although the absolute platelet count remains within normal reference range in most patients.3,6 Thrombocytopenia can be classified as mild (platelet count of 100,000–150,000× 103/mm3), moderate (platelet count of 50,000–100,000× 103/mm3) or severe (platelet count <50,000×103/mm3).1
During pregnancy, most cases of low platelet count are due to gestational thrombocytopenia (GT), idiopathic thrombocytopenic purpura (ITP) or preeclampsia.7 Other causes include infection, such as malaria or folate deficiency, and diseases, such as leukemia and aplastic anemia.4 GT is characterized by incidental detection of mild-to-moderate reduction in platelet count during pregnancy in otherwise healthy women with no previous history of ITP or conditions known to be associated with thrombocytopenia. It is not an early manifestation of autoimmune disease, there is no significant fetal or maternal morbidity, and normalization of platelet counts occur in the vast majority of patients postpartum.7–10 GT is responsible for ~75% of thrombocytopenia in pregnant women.7 GT is usually mild and is not usually associated with fetal thrombocytopenia.11 Platelet count in patients with GT is usually >110,000×103/mm3, whereas counts as low as 70,000×103/mm3 have been reported. In patients with platelet count <70,000×103/mm3, an alternative explanation is frequently present. Although the pathogenesis of GT is not well understood, it may involve factors such as hemodilution and/or accelerated platelet clearance.12,13 It is known that pregnant women with thrombocytopenia have a higher risk of bleeding excessively during or after childbirth, particularly if they need to have a cesarean section or other surgical intervention during pregnancy or labor. Such bleeding complications are more likely when the platelet count is <50×103/mm3.1
Thrombocytopenia during pregnancy has become a cause for unnecessary, often invasive, additional testing and cesarean deliveries. The evaluation and treatment of this condition can be expensive and distressing to the patient and can result in an adverse outcome. Obstetricians in our locality have no comprehensible guide for managing pregnant women with thrombocytopenia due to a lack of data about the frequency, severity and causes of this condition. Moreover, no relevant data are available from other parts of Ethiopia. Therefore, this study was aimed at determining the prevalence of thrombocytopenia among pregnant women attending antenatal care service at Gondar University Hospital, and estimating the proportions of the underlying causes that can give valuable information for the management of thrombocytopenia-related complications in pregnant women.
Materials and methods
Study settings and study population
An institutional-based cross-sectional study design was used to assess the prevalence of thrombocytopenia among pregnant women attending the antenatal care service at Gondar University Hospital from January to April 2015. All women between the ages of 15–49 years who visited Gondar University Hospital for antenatal care during the study period were the source population.
Data collection
Women who visited the antenatal care unit at Gondar University Hospital during the study period participated in the study. Pregnant women on anti-inflammatory drugs, had a bleeding disorder, splenomegaly, or hypertension, or were on antiretroviral treatment were excluded from the study. After obtaining written informed consent, sociodemographic nutritional factors, obstetrics and gynecological factors, history and clinical condition were collected from each study participant using a pretested structured questionnaire, those who had normal blood pressure, were free from malaria parasites and had no platelet aggregation on peripheral film examination were included in the study.
Two milliliters of venous blood was collected under aseptic conditions and transferred in to ethylene diamine tetra acetic acid (EDTA) anticoagulant tubes by mixing for 5 minutes. The specimens were labeled with identification number of each study participant. The EDTA anticoagulant specimens were kept at room temperature until analysis was done for a maximum of 4 hours after specimen collection. The complete blood cell counts were determined using SysmexKX 21 analyzer (Sysmex Corporation, Bellport, NY, USA) which applies electric impedance principle (Sysmex user manual, 2002) following the manufacturer’s instructions.
The reliability of the study findings was guaranteed by implementing quality control (QC) measures throughout the whole process of the laboratory work. All materials, equipment and procedures were adequately controlled. Sysmex were checked for linearity and validity by using lower, medium and high quality control reagents. Preanalytical, analytical and postanalytical stages of quality assurance that were incorporated in standard operating procedures were strictly followed. Appropriate volume of blood and anticoagulant was used to maintain the specimen’s quality. Every day before the samples were investigated, control reagents with low, medium and high concentration were simultaneously investigated by the Sysmex machines to maintain the reagents quality. In addition, thin blood films stained with Wright stain were prepared for all blood samples, to confirm thrombocytopenia and exclude the presence of platelet aggregation and malaria parasites.
Data processing
The data were entered, cleaned and analyzed using SPSS statistical computer software version 20 (IBM Corporation, Armonk, NY, USA). Summary statistics such as frequencies and percentages were calculated. Logistic regression was used to identify the associated factors with thrombocytopenia. A 95% confidence interval and a p-value <0.05 were considered as statistically significant.
Ethical approval
Ethical approval was obtained from the University of Gondar, School of Biomedical and Laboratory Sciences Ethical Clearance Committee, and a permission letter was obtained from Gondar University Hospital Chief Executive Officer before going ahead with the study. Each study participant were asked to participate voluntarily and provided written informed consent to participate in the study. Parental consent was obtained for participants <16 years of age. Confidentiality was kept throughout the collection and processing of specimens. Each study participant were informed about the objective of the study. Voluntary participation and the right to withdraw at any time were emphasized. In addition to this, any study subject with an abnormal test result were referred to their physicians for further investigation and management.
Results
Sociodemographic characteristics of study participants
In this study, a total of 217 woman from the antenatal care at Gondar University Hospital were included in this study. One hundred and sixty-nine (77.8%) of the study subjects were aged <30 years. The mean (± standard deviation [SD]) age of the study participants were 25.67 (±4.69) years. Most of the study subjects (192 [88.3%]) lived in an urban residence. Among the study subjects, 215 (99.1%) were married and 137 (63.1%) were housewives by occupation. Among the study subjects, 35 (16.1%) were unable to read and write (illiterate; Table 1).
  | Table 1 Sociodemographic characteristics of pregnant women attending antenatal care service at Gondar University Hospital in 2014, northwest Ethiopia |
Reproductive characteristics of pregnant women attending antenatal care at Gondar University Hospital in 2014, northwest Ethiopia
Among the study subjects, 38.2%, 36.9% and 24.9% were in the third, second and first trimester, respectively. The mean number of children that the women had were 2, with 2.3% having only one child and 47% having three and more children (Table 2).
  | Table 2 Reproductive characteristics of pregnant women attending antenatal care service at Gondar University Hospital in 2014, northwest Ethiopia |
Hematological profiles of the study subjects
The mean (± SD) hematologic profiles of the study subjects were platelet count 238.85+74.57×109/L, white blood cell (WBC) count 9.35+2.85×109/L and red blood cell (RBC) count 4.43+0.40×1012/L (Table 3).
Prevalence of thrombocytopenia
The prevalence of thrombocytopenia in this study was found in 19 women (8.8%), the remaining 198 (92.2%) women had a platelet count in the normal range. Among the thrombocytopenic pregnant women in this study, 74% had mild thrombocytopenia, 15.7% had moderate thrombocytopenia and 10.3% had severe thrombocytopenia (Figures 1 and 2).
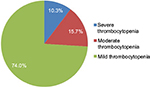  | Figure 1 Severity of thrombocytopenia among pregnant women. |
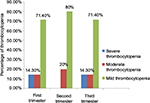  | Figure 2 Distribution of thrombocytopenia among pregnant women across the three trimesters. |
Factors associated with thrombocytopenia
Factors associated with thrombocytopenia were assessed by logistic regression and showed that living in a rural residence showed women were approximately four times more likely to develop thrombocytopenia than women living in an urban area (crude odds ratio [COR]=4.35, 95% confidence interval 1.48–12.76) (Table 4).
Discussion
This study was conducted in order to determine the prevalence of thrombocytopenia among pregnant women attending the antenatal care at Gondar University Hospital. In this study, the prevalence of thrombocytopenia among pregnant women was 8.8%. In this study, the prevalence of thrombocytopenia among pregnant women was 8.8%, which was almost comparable to the results of studies conducted by Vyas et al14 (7.67%), Nisha et al15 (8.8%), Dwivedil16 (8.17%), Shamoon et al17 (8%), Myers18 literature review (8%–10%), Jeffrey et al19 clinical review (8%), and Jodkowska et al20 (7%–10%). However, the result of this study was lower than in studies conducted in Switzerland (11.6%),21 Ethiopia (13.5%),22 Ghana (15.3%),23 Israel (21.8%),24 and Nigeria (13.5%).25 The difference may be due to sociodemographic differences of the study subjects and differences in the study design. Among the thrombocytopenic pregnant women in our study, 74% had mild thrombocytopenia, 15.7% had moderate thrombocytopenia and 10.3% had severe thrombocytopenia. These results are in line with studies conducted in Ethiopia, Ghana, India and Nigeria14,22,23,25,26 which showed a high frequency presence of mild type thrombocytopenia. This study showed that there was no association between the trimesters and thrombocytopenia (p>0.05). This result is similar with previous studies conducted in Ethiopia.22
In summary, thrombocytopenia is a crucial problem among pregnant women with the prevalence of thrombocytopenia shown to be 8.8%, dominantly mild type thrombocytopenia. Thrombocytopenia was higher among pregnant women in the study area who were from a rural residence. For this reason, screening of pregnant women should include a platelet count, especially if they reside in a rural area.
Limitation of the study
The study was a cross-sectional study and it did not include control groups. Since this study is not a follow-up study, it may lack many independent factors of thrombocytopenia assessment.
Acknowledgments
We would like to acknowledge the Department of Haematology, School of Biomedical and Laboratory Sciences, University of Gondar, for all the support to conduct this research work. We also would like to extend our deepest appreciation to the study participants for their willingness in providing the information set for the study.
Author contributions
FA conceived and designed the study, was involved in the literature review and wrote and edited the final draft of the article.
BE and ZG collected the data, carried out the data and statistical analysis and were involved in literature review, writing and editing of the final draft. All authors approved the final version of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
Reference
Katke RD Gohil DP. Thrombocytopenia during pregnancy: an institutional based study. Int J Reprod Contracept Obstet Gynecol. 2014;3(4):947–951. | ||
Sainio S, Kekomaki R, Riikonon S, Teramo K. Maternal thrombocytopenia at term: a population-based study. Acta Obstet Gynecol Scand. 2000;79(9):744–749. | ||
Boehlen F, Hohlfeld P, Extermann P, Perneger TV, de Moerloose P. Platelet count at term pregnancy: a reappraisal of the threshold. Obstet Gynecol. 2000;95(1):29–33. | ||
McCrae KR. Thrombocytopenia in pregnancy: differential diagnosis, pathogenesis, and management. Blood Rev. 2003;17(1):7–14. | ||
Ballem PJ. Hematological problems of pregnancy. Can Fam Physician. 1988;34:2531–2537. | ||
Boehlen F. Thrombocytopenia during pregnancy: importance, diagnosis and management. Hamostaseologie. 2006;26(1):72–74. | ||
Burrows RF, Kelton JG. Fetal thrombocytopenia and its relation to maternal thrombocytopenia. N Engl J Med. 1993;329(20):1463–1466. | ||
Ruggeri M, Schiavotto C, Castaman G, Tosetto A, Rodeghiero F. Gestational thrombocytopenia: a prospective study. Haematologica. 1997;82(3):341–342. | ||
Samuels P, Bussel JB, Braitman LE, et al. Estimation of the risk of thrombocytopenia in the offspring of pregnant women with presumed immune thrombocytopenic purpura. N Engl J Med. 1990;323(4):229–235. | ||
How HY, Bergmann F, Koshy F, et al. Idiopathic thrombocytopenic purpura: a practice guideline developed by explicit methods for the American Society of Haematology. Blood. 1996;88(1):3–40. | ||
Shehata N, Burrows R, Kelton JG. Gestational thrombocytopenia. Clin Obstet Gynecol. 1999;42(2):327–334. | ||
Kadir RA, McLintock C. Thrombocytopenia and disorders of platelet function in pregnancy. Semin Thromb Hemost. 2011;37(6):640–652. | ||
Vyas, Rupa, Shah S, et al. Comparative study of mild versus moderate to severe thrombocytopenia in third trimester of pregnancy in a tertiary care hospital. NHL J Med Sci. 2014;3(1):8–11. | ||
Nisha S, Amita D, Uma S, Tripathi AK, Pushplata S. Prevalence of and characterization of thrombocytopenia in pregnancy in India women. Indian J Hematol Blood Transfus 2012;28(2):77–81. | ||
Dwivedi P, Puri M, Nigam A, Agarwal K. Fetomaternal outcome in pregnancy with severe thrombocytopenia. Eur Rev Med Pharmacol Sci. 2012;16(11):1563–1566. | ||
Shamoon RP, Muhammed NS, Jaff MS. Prevalence and etiological classification of thrombocytopenia among a group of pregnant women in Erbil City, Iraq. Turk J Hematol. 2009;26(23):123–128. | ||
Myers B. Thrombocytopenia in pregnancy. Obstert Gynecol. 2009; 11(3):177–183. | ||
Jeffrey A, Levy CPT, MC, FS, Lance D, Murphy MD. Thrombocytopenia in pregnancy. J Am Board Fam Pract. 2002;15:290–7. | ||
Jodkowska A, Martynowicz H, Kaczmarek-Wdowiak B, Mazur. Thrombocytopenia in pregnancy – pathogenesis and diagnostic approach. Postepy Hig Med Dosw (Online). 2015;69(0):1215–1221. | ||
Boehlen F, Hohlfeld P, Extermann P, Perneger TV, de Moerloose P. Platelet count at term pregnancy: a reappraisal of the threshold. Obstet Gynecol. 2000;95(1):29–33. | ||
Belayneh F, G/Mariam A, Solomon F. The prevalence of thrombocytopenia, and associated factors among pregnant women attending antenatal care at Hawassa University Referral Teaching and Hospital. J Harmoniz Res Med Hlth Sci. 2015;2(4):175–182. | ||
Olayemi E, Akuffo FW. Gestational thrombocytopenia women among pregnant Ghanaian women. Pan Afr Med J. 2012;12:34. | ||
Parnas M, Sheiner E, Shoham-Vardi I, et al. Moderate to severe thrombocytopenia during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2006;128(1–2):163–168. | ||
Ajibola SO, Akinbami A, Adewumi A, et al. Gestational thrombocytopenia women among pregnant women in Legos Nigeria. Niger Med J. 2014;55(2):139–143. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


