Back to Journals » Psychology Research and Behavior Management » Volume 12
Prevalence of severe moral distress among healthcare providers in Saudi Arabia
Authors Almutairi AF , Salam M , Adlan AA , Alturki AS
Received 16 October 2018
Accepted for publication 27 December 2018
Published 11 February 2019 Volume 2019:12 Pages 107—115
DOI https://doi.org/10.2147/PRBM.S191037
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Igor Elman
Adel F Almutairi,1 Mahmoud Salam,1 Abdallah A Adlan,2 Abdullah S Alturki3
1Science and Technology Unit, King Abdullah International Medical Research Center, King Saud Bin Abdulaziz University for Health Sciences, Ministry of National Guard health affairs, Riyadh, Saudi Arabia; 2Bioethics Section, King Abdullah International Medical Research center, King Saud Bin Abdulaziz University for Health Sciences, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia; 3Research operations, King Abdullah International Medical Research center, King Saud Bin Abdulaziz University for Health Sciences, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia
Background: Moral distress is a serious problem in healthcare environments that requires urgent attention and management. It occurs when healthcare providers are unable to provide the care that they feel is right or take, what they believe to be, ethically appropriate actions for their patients. Thus, this study aims to examine moral distress among nurses and physicians working in tertiary teaching hospitals in Saudi Arabia, as well as to evaluate the level of association between moral distress and turnover.
Methods: This cross-sectional study, which employed an anonymous 21-item Moral Distress Scale, was undertaken at a large medical institution located in different regions of Saudi Arabia. The data were analyzed using bi-variate analyses, and logistic regression.
Results: Of the 342 participants, 239 (69.9%) were nurses/staff physicians and 103 (30.1%) were fellows/consultants. Approximately 24.3% of respondents experienced severe moral distress, whereas 75.7% reported mild moral distress. There was no statistically significant difference between men and women in terms of moral distress. Age was found to be a notable factor: moral distress was significantly higher in those younger than 37 years compared to those 37 years and older (P=0.015). Less than half of the participants (137, 42.8%) indicated their willingness to leave their jobs. A significant association was observed between severe moral distress and leaving the career (OR=3.16; P<0.01). Job category was also an important factor: nurses/staff physicians were almost two times more likely (OR =1.95, P=0.038) to leave their positions compared to fellows/consultants.
Conclusion: This study revealed that moral distress, which is a serious problem that compromises the well-being of caregivers, was a predictive variable for the intention of healthcare providers to leave their jobs. Therefore, it should be routinely examined, and efficient action plans should be implemented to alleviate its consequences.
Keywords: burnout, MDS-R, organizational support, nurses, physicians
Background
In healthcare environments around the globe, nurses, physicians, and other healthcare professionals often face complex practical and ethical dilemmas in their daily practice that have significant psychological effects on them.1 These dilemmas are often the result of decisions that they make that conflict with their values, beliefs, and the fundamental role of their profession in providing competent, timely, responsive, and ethical care. Within the workplace, healthcare providers may also encounter constraints (personal and/or institutional) that disrupt their agency to act as advocates for their patients. Consequently, the optimal goal of healthcare delivery, which aims to maintain the safety, equity, and quality of health services for patients and families as well as for their communities, can be compromised.
In situations when two ethical decisions compete, nurses, physicians, and other healthcare providers rely on their morals, which define for them what is right and dictate the appropriate action to be taken. These morals develop from many sources, such as family traditions and upbringing, culture, religion, social conventions and rules, and education. They can be further refined during a lifetime through human interaction, socialization, and exposure to other societies and cultures.2
Many of the factors that hinder the ability of healthcare providers to enact their moral agency and to achieve their professional goals are related to institutional constraints or conflicting ethical principles. These include inadequate resources, excessive workloads, lack of time, high patient acuity, patient care concerns, conflicting patient-family needs, and professional conflicts.1,3–6 When healthcare provides are unable to provide the care that they feel is right or take what they believe is ethically appropriate action for their patients, they feel a lack of autonomy and powerless which eventually develops a psychological reaction, called moral distress.7
The term “moral distress” was coined by an American ethicist Andrew Jameton in 1984. He attributed its cause to a situation “when one knows the right thing to do, but institutional constraints makes it nearly impossible to pursue the right course of action” (p. 6).7 Jameton further developed this definition to include two main levels of psychological reactions, namely initial distress and reactive distress. Initial distress is experienced when the healthcare provider initially feels frustrated and anxious due to a conflicting situation or an institutional barrier, whereas the second is experienced when the provider is unable to act upon the initial distress. In light of Jameton’s work, Wilkinson8 defined moral distress as “the psychological disequilibrium and negative feeling state” experienced in such situations (p. 16). An expanded and comprehensive definition was suggested by Nathaniel as “the pain or anguish affecting the mind, body or relationship in response to a situation in which the person is aware of a moral problem, acknowledges moral responsibility, and makes a moral judgment about the correct action” (p. x, 9).
Moral distress is a serious problem in healthcare environments and requires urgent attention and management due to the threats it poses to healthcare providers’ moral integrity and well-being, the quality of service delivery, and the well-being of patients and families.1 Providers who suffer moral distress as a result of being aware of their responsibilities, while lacking the power and resources to act accordingly, can exhibit feelings of frustration, anger, anxiety, helplessness and powerlessness, and guilt. They may also not feel important or intelligent and suffer from depression, nightmares, or sorrow.3,10,11 These significant physical and emotional reactions can lead to job dissatisfaction and perhaps the loss of qualified and experienced professionals.12,13
Due to its consequences, moral distress is gaining more attention in the literature, and a number of studies have demonstrated that moral distress is prevalent in nursing, especially in end-of-life decision-making.12,14–16 For example, nurses often find it difficult to cope with dying patients and family grieving. Most of the research on moral distress, however, has been conducted with acute care nurses working in specialty units, such as critical care, oncology, perinatal nursing, and medical/surgical units.17–20 In addition, several studies have been conducted in the field of mental health.10,21,22 Other studies have indicated that moral distress was also experienced by physicians, pharmacists, and respiratory therapists in different settings.17,23–25 Significantly, the factors that induce the experience of moral distress may differ based on profession and context.13 In Saudi Arabia, no research has been carried out on the moral distress of healthcare providers, most of whom are from different countries and provide care for Saudi patients and their families who are also culturally different from their own. Therefore, the purpose of this study was twofold: 1) to examine moral distress among registered nurses and physicians working in tertiary teaching hospitals in Saudi Arabia and 2) to evaluate the association between moral distress and intention to leave.
Methods
Population and sampling
The study target group was full-time registered nurses and physicians working in a number of Saudi Arabian tertiary hospitals operated by the Ministry of National Guard Health Affairs. Students; those with <1-year work experience were excluded. These hospitals are located in Riyadh, Jeddah, Almadinah, Al Ahsa, and Dammam. The participants were randomly selected from a list of names of eligible professionals at these hospitals and contacted by email to inform them about the current study, including its purpose and procedure. Those who were interested completed the study’s electronic questionnaire in English, which also comprised demographic questions. Completing the questionnaires was also considered as informed consent. The calculated sample size was 385, taking into consideration the following parameters: a 50% assumed prevalence of moral distress, 95% CI, and a 5% margin of error. Oversampling with 25% was applied to compensate for the incomplete questionnaires, which made the total number of distributed questionnaires 480.
Data collection
The data were collected using Modified Distress Scale-Revised (MDS-R), which was originally developed by Corley et al18 to measure moral distress among critical care nurses. Corley et al developed MDS based on three theoretical grounds of knowledge. These include Jameton’s7 conceptualization of moral distress, House and Rizzo’s26 role conflict theory, and Rokeach’s27 value theory. This scale is composed of 38 items that measure the frequency and intensity of moral distress. Items pertaining to intensity are rated on a 7-point Likert scale, where 0 indicates no moral distress and 6 indicates extreme moral distress; for frequency, 0 indicates that it never occurs in practice and 6 indicates that it is a common occurrence in practice. Corley et al assessed the content validity of the MDS-R and reported it to be 100%. The Cronbach’s alpha was reported to be 0.98 for the intensity scale and 0.90 for the frequency scale.24
A more recent work that Hamric et al conducted to revise and validate the MDS scale led to shortening the original 38 items to 21 and to developing six parallel versions of the scale.28 This increased its applicability to different settings and populations beyond nursing to include adult and pediatric physicians and other healthcare providers. Hamric et al also revised the response scale format from the original one mentioned above to a 0–4 scale for both the frequency and the intensity of disturbance. The content validity of the MDS-R was evaluated through consulting four professionals who are experts on moral distress. Each expert independently reviewed the scale for the clarity and relevance of each item. An inter-rater agreement of 88% was obtained, and a full agreement was achieved on 19 items. As a result, one item was completely reworded and a new one was added. The reliability of the MDS-R was evaluated, and the Cronbach’s alpha score was estimated to be 0.89. Construct validity was also demonstrated by testing a number of hypotheses.28
Data analysis
The data were analyzed using SPSS for Windows, version 25. Descriptive statistics were employed to present demographic data and responses to moral distress items. Pearson’s chi-squared test was employed to identify the differences between various exposures and the category of moral distress. Since the moral distress score was not normally distributed, the Mann–Whitney test was used to investigate the differences among the number of exposures such as gender, age, nationality, patient population, job category (nurse/staff physician vs fellow/consultant),28 intention to leave their jobs and their moral distress scores. Finally, a logistic regression model was constructed to identify factors significantly associated with the respondents’ intention to leave the jobs.
Ethicals statement
Ethical clearance and approval to undertake this study was obtained from the institutional review board at the Ministry of National Guard Health Affairs. An introductory letter explained the study objectives. Completing the questionnaire was considered a consent for participation.
Results
Demographic characteristics
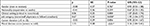
In this study, there were 342/480 participants, with 71.3% response rate of which 200 (58.4%) were nurses, 39 (11.4%) were staff physicians, and 103 (30.2%) were fellows/consultants. The 226 women participants formed the majority (66.1%), with the 116 men participants forming the minority (33.9%). The participants fell into different age categories, with a mean age of 37.9 and an SD of 7.9, and were categorized into two main groups: the first representing the young adults (<37 years) and the second representing those middle aged and older (≥37 years). Almost half the participants (137, 42.8%) intended to leave their jobs. Table 1 provides more information on the participants’ demographics.
  | Table 1 Sample’s characteristics |
Participants’ scores on items of moral distress
The participants had different views on the items that composed the scale of moral distress. The statements that had the highest percentage mean scores (PMSs) were “Carry out medical orders for what I consider to be unnecessary tests and treatments” with 33.4±31.9 and “Follow the family’s wishes to continue life support even though I believe it is not in the best interest of the patient” with 32.1±33.9. The statements that obtained the lowest PMSs were “Avoid taking action when I learn that a colleague has made a medical error and does not report it” with 12.4±19.2, “Witness students perform painful procedures on patients solely to increase their skill” with 10.6±21.3, and “Increase the dose of sedatives/opiates for an unconscious patient that I believe could hasten the patient’s death” with 5.4±13.1. The statements with their corresponding mean scores are presented in order (from the highest to lowest) in Table 2.
  | Table 2 Moral distress statements ranked from highest to lowest based on their PMS |
Factors associated with moral distress
Participants’ characteristics, including their intention to leave their job, were tested in terms of their association with moral distress. Moral distress was presented in two forms, quantitatively (median score) and qualitatively (prevalence of mild and severe moral distress). The results indicated that 26 (22.4%) men and 55 (24.3%) women had severe moral distress. However, the participants’ age was significantly associated with moral distress: those who were <37 years old (46, 29.9%) had more severe moral distress than those (35, 18.6%) who were 37 years and more (P=0.015). There was no statistically significant difference in moral distress scores between those who worked in critical care areas and those who worked in regular care units, although those working in critical care areas had more severe moral distress (55, 26%) compared to their countergroup (26, 19.7%). In addition, there were no statistically significant differences in the prevalence of severe moral distress between those working within an adult (59, 23.4%) and a pediatric (25, 24.5%) settings. The results showed no statistically significant difference between Saudis (13, 22.8%) and expatriates (68, 23.9%), and also between those with higher and lower levels of education, in terms of prevalence of severe moral distress. Interestingly, a statistically significant association was observed between moral distress and participants’ intention to leave their job, as those who were morally distressed scored higher on the item on intention to leave the job (P<0.01). Table 3 provides additional details on the factors associated with moral distress.
Since one of the main areas of investigation in this study was how moral distress affected participants’ intention to leave their job, this variable was investigated across the participants’ characteristics. The analysis indicated a statistically significant difference among participants based on job category (P=0.007): 104 (47.9%) nurses/staff physicians wanted to leave their job due to moral distress compared to fellows/consultants (33, 32.0%). Also, the career duration was significantly associated with the intention to leave due to moral distress (P<0.008). The comparison between group scores is presented in Table 4.
The binary logistic regression analysis also revealed that nurses/staff physicians were almost two times more likely (OR =1.95, P=0.038) to leave their job compared to fellows/consultants. In addition, severe moral distress was a predictive variable for the intention of participants to leave their job: (OR =3.16, P<0.01), as illustrated in Table 5.
  | Table 5 Factors associated with participants’ intention to leave their career Notes: β: coefficient of determination. *Significant at <0.05. Abbreviations: SE, standard error. |
Discussion
In healthcare environments, ethical and practical dilemmas frequently exist that can affect the psychological well-being of healthcare providers. When caregivers fail to take what they think are ethically appropriate actions for their patients, they develop a condition known as moral distress. The philosophical assumption here can be similar to what was articulated by David Hume:29 there is a conflict between what “is” going on vs what “ought” to be going on. As this is a serious problem requiring urgent attention, this study investigated the prevalence of moral distress among healthcare providers working in a multicultural setting, as well as its association with job satisfaction and turnover.
The findings of the current study indicated that 24.3% of participants experienced severe moral distress. Previous studies on moral distress have also shown it to be prevalent among healthcare providers, particularly nurses, in healthcare environments. For example, a correlational-descriptive study conducted in Tehran with 120 nurses (various work specialties) found that they had a high level of moral distress.30 In contrast, a number of studies conducted on nurses (intensive care and emergency) in different settings and countries, including the US, Sweden, and Turkey, revealed that nurses had overall low levels of moral distress.31–34
The current study’s findings and those in the literature revealed the prevalence of moral distress, yet at various levels. These variations could be attributed to a number of factors, such as differences in the work environment, organizational culture, and study populations, including their social norms and culture.30 For instance, the current study was conducted in a multicultural environment, where the healthcare providers were from different cultures around the world and represented >26 nationalities.35,36 People bring with them their own cultural values, beliefs, customs, and attitudes that shape their ethical views and behaviors,36 which could lead to inconsistencies in decision-making or taking action in ethically charged situations. Although there is a universal code of conduct for providing optimal patient care, the aforementioned factors could influence its application.
The study findings also indicated that there is a strong association between moral distress and intention to leave one’s job: those who had higher moral distress scores were more prone to leaving their positions than those with lower scores. Specifically, the study found that nurses/staff physicians were almost two times more likely to leave their jobs compared to fellows/consultants. In addition, those with severe moral distress (24.3%) were three times more likely to leave their positions (OR =3.16, P<0.01). This finding is comparable to those of many studies in the literature.15,37 For instance, a research undertaken in northern California found that the intensity of moral distress was linked to nurses’ dissatisfaction and intention to leave their jobs.31 Additionally, the literature has shown that the factors that contribute to healthcare providers’ dissatisfaction and their decision to change jobs are more often related to stress than salary and benefits. These factors include depersonalization, diminished personal accomplishment, emotional exhaustion, poor recognition, difficult workloads, safety issues with patient care, and so on.38 Severe moral distress can lead to avoidance of patients, depression, and even substance abuse.39
One possible explanation for the finding that nurses/staff physicians had higher levels of moral distress than fellows/consultants is that the members of the former group are not the final decision makers when it comes to patients’ treatment. This explanation is supported by the participants’ responses to the statement that had the highest mean scores, that is, performing medical orders they deemed unnecessary for their patients. Our results are consistent with a study conducted in Brazil with 283 critical care providers, including physicians.40 In the majority of the studies in the literature, the participants were nurses15,30–32,34,39,40 and the most common causes of moral distress included overly aggressive medical treatment, inappropriate utilization of resources, physicians providing inaccurate information to patients and their families, the provision of futile medical care, and following the family’s wishes to continue life support when it is contrary to the patient’s best interests (this was the second most significant cause of moral distress in the current study).41–43
Age was also identified as a significant factor associated with moral distress, and specifically those who were younger than 37 years old had more severe moral distress than those who were 37 years and older. Previous studies found that moral distress is positively correlated with years of experience and age progression, although there were some variations as each researcher used different age categories.44,45 In this study, the mean age of the participants was 37, and accordingly, the sample was divided into two groups. Nurses/staff physicians start working in a hospital setting and providing care to patients sometime between the ages of 23 and 25. This supports the premise that the intensity of moral distress is high among junior healthcare workers due to difficulties in coping with work stressors. However, another possible explanation for the fact that older participants scored lower on moral distress could be associated with age-related “desensitization” and withdrawal from morally troubling patient situations, rather than that they have more experience.44,46,47
Although the participants in this study were invited from a number of medical centers in Saudi Arabia, one limitation is that they all belonged to a single institution. Therefore, the standard of care, policies and procedures, and organizational climate were the same. Thus, the results may not be generalizable and reflect moral distress in other hospitals in Saudi Arabia. Although the study participants were randomly selected, there is a possibility of self-selection bias committed by some participants. There are also possibly a number of existing confounding factors that could have influenced the participants’ moral distress scores and their willingness to leave their jobs, such as organizational support, high occupancy, number of staff members, and promotion opportunities. Organizational support is one of the main factors in the literature found to be associated with moral distress. Therefore, qualitative and quantitative studies are recommended to specifically identify sources of moral distress and investigate organizational culture and support. Engaging nurses and staff physicians in decision-making related to patient care might help counteract feelings of moral distress. In addition, developing educational programs to address moral distress is imperative. It is the employer’s responsibility to mitigate the complications of moral distress and eliminate the sources, if possible, which will eventually lead to a healthy work environment and better quality of care.
Conclusion
Moral distress threatens the psychological well-being of healthcare providers. In this study, the intensity of moral distress was found to be associated with age, position, and length of experience, while gender did not seem to be a factor. Moral distress was also significantly linked to caregivers’ intention to leave their positions as those with severe moral distress were three times more likely to consider leaving their jobs. For many healthcare providers, what they do is more than a job because patients are entrusting them not only with their well-being but also with their lives. Given this level of responsibility, moral distress affects such workers to a greater degree than those in many other professions. For example, actions such as performing a painful procedure on a patient as a teaching exercise, engaging in extensive life-saving actions that only prolong a patient’s death, carrying out medical orders that seem unnecessary, or providing less than optimal care make healthcare providers feel helpless and cause them distress. It is worth conducting a qualitative study that would explore in depth the reasons behind moral distress among different genders.
Data sharing statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The research team would like to thank King Abdullah International Medical Research Center for supporting this study. They also want to express a special thanks to the study participants.
Disclosure
The authors report no conflicts of interest in this work.
References
Almutairi AF, Rondney P. Critical cultural competence for culturally diverse workforces: toward equitable and peaceful health care. ANS Adv Nurs Sci. 2013;36(3):200–212. | ||
Dickerson P. Moral Distress: Its Impact on Nursing. Dayton: CoxOhio Publications; 2010. | ||
Zuzelo PR. Exploring the moral distress of registered nurses. Nurs Ethics. 2007;14(3):344–359. | ||
Bandura A. Moral disengagement in the perpetration of inhumanities. Pers Soc Psychol Rev. 1999;3(3):193–209. | ||
Kälvemark S, Höglund AT, Hansson MG, Westerholm P, Arnetz B. Living with conflicts-ethical dilemmas and moral distress in the health care system. Soc Sci Med. 2004;58(6):1075–1084. | ||
Abuatiq A, Burkard J, Clark MJ. Literature review: patients’ and health care providers’ perceptions of stressors in critical care units. Dimens Crit Care Nurs. 2013;32(1):22–27. | ||
Jameton A. Nursing Practice: The Ethical Issues. Englewood Cliffs, NJ: Prentice Hall; 1984. | ||
Wilkinson JM. Moral distress in nursing practice: experience and effect. Nurs Forum. 1987;23(1):16–29. | ||
Nathaniel A. Moral Distress Among Nurses. Washington: Bioethics Research Library, 2002. | ||
Lützén K, Blom T, Ewalds-Kvist B, Winch S, Stress M. Moral stress, moral climate and moral sensitivity among psychiatric professionals. Nurs Ethics. 2010;17(2):213–224. | ||
Epstein EG, Delgado S. Understanding and addressing moral distress. Online J Issues Nurs. 2010;15(3)1. | ||
Hamric AB. Moral distress in everyday ethics. Nurs Outlook. 2000;48(5):199–201. | ||
Pauly B, Varcoe C, Storch J, Newton L. Registered nurses’ perceptions of moral distress and ethical climate. Nurs Ethics. 2009;16(5):561–573. | ||
Austin W. The ethics of everyday practice: healthcare environments as moral communities. ANS Adv Nurs Sci. 2007;30(1):81–88. | ||
Corley MC. Nurse moral distress: a proposed theory and research agenda. Nurs Ethics. 2002;9(6):636–650. | ||
Tiedje LB. Moral distress in perinatal nursing. J Perinat Neonatal Nurs. 2000;14(2):36–43. | ||
Austin W, Lemermeyer G, Goldberg L, Bergum V, Johnson MS. Moral distress in healthcare practice: the situation of nurses. HEC Forum. 2005;17(1):33–48. | ||
Corley MC, Elswick RK, Gorman M, Clor T. Development and evaluation of a moral distress scale. J Adv Nurs. 2001;33(2):250–256. | ||
Raines ML. Ethical decision making in nurses. Relationships among moral Reasoning, coping style, and ethics stress. JONAS Healthc Law Ethics Regul. 2000;2(1):29–41. | ||
Rodney P. Moral distress in critical care nursing. Can Crit Care Nurs J. 1988;5(2):9–11. | ||
Deady R, McCarthy J. A study of the situations, features, and coping mechanisms experienced by Irish psychiatric nurses experiencing moral distress. Perspect Psychiatr Care. 2010;46(3):209–220. | ||
Corley MC, Minick P, Elswick RK, Jacobs M. Nurse moral distress and ethical work environment. Nurs Ethics. 2005;12(4):381–390. | ||
Førde R, Aasland OG. Moral distress among Norwegian doctors. J Med Ethics. 2008;34(7):521–525. | ||
Sporrong SK, Höglund AT, Arnetz B. Measuring moral distress in pharmacy and clinical practice. Nurs Ethics. 2006;13(4):416–427. | ||
Schwenzer KJ, Wang L. Assessing moral distress in respiratory care practitioners. Crit Care Med. 2006;34(12):2967–2973. | ||
House RJ, Rizzo JR. Role conflict and ambiguity as critical variables in a model of organizational behavior. Organ Behav Hum Perform. 1972;7(3):467–505. | ||
Rokeach M. The Nature of Human Values. New York: Free Press; 1973. | ||
Hamric AB, Borchers CT, Epstein EG. Development and testing of an instrument to measure moral distress in healthcare professionals. AJOB Prim Res. 2012;3(2):1–9. | ||
Rayner S. Hume’s moral philosophy. Macalester J Philos. 2005;14(1):2. | ||
Robaee N, Atashzadeh-Shoorideh F, Ashktorab T, Baghestani A, Barkhordari-Sharifabad M. Perceived organizational support and moral distress among nurses. BMC Nurs. 2018;17(1):2. | ||
Fernandez-Parsons R, Rodriguez L, Goyal D. Moral distress in emergency nurses. J Emerg Nurs. 2013;39(6):547–552. | ||
O’Connell CB. Gender and the experience of moral distress in critical care nurses. Nurs Ethics. 2015;22(1):32–42. | ||
Silén M, Svantesson M, Kjellström S, Sidenvall B, Christensson L. Moral distress and ethical climate in a Swedish nursing context: perceptions and instrument usability. J Clin Nurs. 2011;20(23–24):3483–3493. | ||
Karagozoglu S, Yildirim G, Ozden D, Çınar Z. Moral distress in Turkish intensive care nurses. Nurs Ethics. 2017;24(2):209–224. | ||
Almutairi AF. Fostering a supportive moral climate for health care providers: toward cultural safety and equity. NursingPlus Open. 2015;1:1–4. | ||
Almutairi AF, McCarthy A, Gardner GE. Understanding cultural competence in a multicultural nursing workforce: registered nurses’ experience in Saudi Arabia. J Transcult Nurs. 2015;26(1):16–23. | ||
De Veer AJ, Francke AL, Struijs A, Willems DL. Determinants of moral distress in daily nursing practice: a cross sectional correlational questionnaire survey. Int J Nurs Stud. 2013;50(1):100–108. | ||
Cummings CL. The effect of moral distress on nursing retention in the acute care setting [UNF Graduate Theses and Dissertation]. Accra: University of Florida; 2009. | ||
Robinson R. Registered nurses and moral distress. Dimens Crit Care Nurs. 2010;29(5):197–202. | ||
Fumis RRL, Junqueira Amarante GA, de Fátima Nascimento A, Vieira Junior JM, Amarante GA, Junior JM. Moral distress and its contribution to the development of burnout syndrome among critical care providers. Ann Intensive Care. 2017;7(1):71. | ||
Elpern EH, Covert B, Kleinpell R. Moral distress of staff nurses in a medical intensive care unit. Am J Crit Care. 2005;14(6):523–530. | ||
Gutierrez KM. Critical care nurses’ perceptions of and responses to moral distress. Dimens Crit Care Nurs. 2005;24(5):229–241. | ||
McClendon H, Buckner EB. Distressing situations in the intensive care unit: a descriptive study of nurses’ responses. Dimens Crit Care Nurs. 2007;26(5):199–206. | ||
Elpern EH, Covert B, Kleinpell R. Moral distress of staff nurses in a medical intensive care unit. Am J Crit Care. 2005;14(6):523–530. | ||
Pendry PS. Moral distress: recognizing it to retain nurses. Nurs Econ. 2007;25(4):217. | ||
Abbasi M, Nejadsarvari N, Kiani M, et al. Moral distress in physicians practicing in hospitals affiliated to medical sciences universities. Iran Red Crescent Med J. 2014;16(10):e18797. | ||
Whitehead PB, Herbertson RK, Hamric AB, Epstein EG, Fisher JM. Moral distress among healthcare professionals: report of an institution-wide survey. J Nurs Scholarsh. 2015;47(2):117–125. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


