Back to Journals » Journal of Blood Medicine » Volume 8
Prevalence of RhD variants among blood donors at Gulu Regional Blood Bank, Gulu, Northern Uganda
Authors Ojok P, Oyet C, Webbo F , Mwambi B, Taremwa IM
Received 4 July 2017
Accepted for publication 25 August 2017
Published 15 September 2017 Volume 2017:8 Pages 151—154
DOI https://doi.org/10.2147/JBM.S145550
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin Bluth
Video abstract presented by Ivan M Taremwa
Views: 319
Polycarp Ojok,1,2 Caesar Oyet,1 Fred Webbo,1,3 Bashir Mwambi,1 Ivan M Taremwa1
1Institute of Allied Health Sciences, International Health Sciences University, Kampala, 2Gulu Regional Blood Bank, Gulu, 3Lancet Laboratories, Kampala, Uganda
Aim/objective: The aim of this study was to determine the prevalence of RhD variant phenotypes among voluntary non-remunerated blood donors (VNRBDs) at Gulu Regional Blood Bank (GRBB), Northern Uganda.
Materials and methods: We conducted a cross-sectional study, in which the first 4.0 mL of ethylenediaminetetraacetic acid (EDTA) blood samples were collected from VNRBDs and typed for their ABO and RhD blood group status using IgM and IgG monoclonal typing antisera, respectively. Blood samples that tested as RhD negative were further investigated for RhD variant phenotypes using indirect antihuman globulin hemagglutination technique.
Results: We assayed 138 RhD-negative blood samples obtained from VNRBDs. Of these, 66.7% (n=92) were males. Their median age was 24.4 years (range, 14–33 years). Majority of the participants were of ABO blood group O (62.8%, n=86), followed by A (19.7%, n=27), then B (13.9%, n=19) and least AB (3.6%, n=6). The prevalence of RhD variant phenotypes was 0.7% (n=1; 95% confidence interval, 0.5–0.9). There was no statistical association of RhD variant phenotypes with donor gender, tribe and their ABO blood groups.
Conclusion: This study has revealed a high prevalence of RhD variant among blood donors at GRBB in Northern Uganda. It further highlights a potential risk of alloimmunization, as the present blood typing practices do not identify RhD variant phenotypes.
Keywords: Rh blood group, D variants, D antigen, weak D, partial D, Uganda
Introduction
The Rh blood group system was discovered in 1940 by Karl Landsteiner and Weiner. It consists of D, d, C, c, E and e blood group antigens.1 The D antigen is highly considered in blood banking and transfusion medicine,2 and on this antigenic basis, individuals are typed as either RhD positive or negative. Although the frequency of RhD-positive phenotypes are reportedly high (~95% in sub-Saharan Africa and >99.5% in eastern Asia),3 there exists a plethora of D variants categorized as weak D, partial D and DEL phenotypes.4
The weak D variant results from a single point mutation in the transmembranous or intracellular region of the RHD gene and is reflected by reduced quantities of the normal D antigen. The partial D variant is as a result of mutation in the extracellular regions and replacement of RhD exons by the RHCE counterparts, leading to an altered or new epitopes. Individuals with partial D contain normal number of the D antigens but with a reduced quantity of D-specific epitopes on the RhD proteins. The DEL D variant expresses very low quantities of the RhD antigen.2,4–6
The frequency of the RhD variants was reported at 6.45% among Ghanaian blood donors, 4.5% in blood donors of Egypt and 0.4% in blood donors of Morocco.7–9
RhD variants are of clinical importance owing to their high immunogenicity and potential to cause alloimmunization among RhD-negative individuals following transfusion of D-positive red blood cells.4,10 In short, this results in adverse effects such as hemolytic disease of the fetus and new born, autoimmune hemolytic anemia and hemolytic blood transfusion reaction.11,12
In blood banking, RhD variant phenotypes are critical aspects of blood transfusion safety. In the laboratory, RhD typing techniques involve the use of anti-D sera to ascertain the expression of the D antigens on the surface of red blood cells. Classification of RhD variant phenotypes relies on the typing using anti-D reagent;13 on this basis, RhD variants are mistyped as D negative while using polyclonal antisera and D positive for monoclonal anti-D antisera.14 Despite the wide recommendation and utilization of monoclonal anti-D antisera, it is now more evident that most immunogenic RhD variants cannot be detected by direct hemagglutination; consequently, such donor units when cross matched for D negative, recipient’s risk is being alloimmunized. Whereas immunohematological assays such as indirect antihuman globulin (AHG) test and adsorption–elution technique ably detect RhD variant phenotypes, the present Uganda blood transfusion RhD typing procedure involves RhD typing using direct hemagglutination with monoclonal anti-D that falls short as it can miss out RhD variants.15 Thus, this study sought to determine the prevalence of RhD variant phenotypes among voluntary non-remunerated blood donors (VNRBDs) at Gulu Regional Blood Bank (GRBB), Northern Uganda.
Materials and methods
Study participant
Our study participants comprised of VNRBDs at GRBB whose blood pressures were between 60–90/90 and140 mmHg, hemoglobin values were not <12.5 g/dL (for females) or 13.5 g/dL (for males), as estimated using specific gravity technique with copper II sulfate solution, and body weight was of ≥50 kg.
Sample collection
We used the first 4.0 mL of ethylenediaminetetraacetic acid (EDTA) blood collected through a small pouch connected with a Vacutainer holder that leads to blood bag containing citrate phosphate dextrose adenine anticoagulant (CPDA-1 [USP]; Agary® blood bag; Agary Pharmaceutical Ltd., Shandong, China). Following blood donation, the samples in the EDTA Vacutainer and the CPDA donor unit were stored between 2 and 8°C in the blood bank. The EDTA blood samples were detached from respective donor packs and then grouped for ABO and RhD status.
Laboratory analysis
Routine forward grouping technique was performed to determine the ABO and RhD blood group status using IgM and IgG monoclonal grouping antisera, respectively (Plasmatec Laboratory Products, Dorset, UK). For all donor units that were detected RhD negative, they were analyzed using indirect AHG test (Biotech Laboratory Limited, Suffolk, UK). All blood samples that did not show hemagglutination during the immediate spin phase were considered as RhD negative and were considered for this study. RhD variants were determined by serological laboratory testing of blood samples using immediate spin phase, followed by incubation and finally the antiglobulin phase. This involved preparing a 3% suspension of washed red blood and control cells in normal saline. All the tubes were mixed thoroughly and centrifuged for 1 minute at 1,000 revolutions per minute (rpm). The tubes were gently resuspended for red cell button and read macroscopically for agglutination starting with control cells followed by test cells. All tubes that showed negative or inconclusive results were incubated at 37°C for 20 minutes. Following incubation, cells were washed twice in phosphate-buffered saline, and saline was decanted off completely. Two volumes of polyspecific antihuman globulins were added to the dry cell button of all tubes and mixed gently to resuspend the cells. The suspension was then centrifuged at 2,460 rpm for 15 seconds. All tubes were gently resuspended and examined macroscopically for agglutination starting with control cells. We adhered to standard operating procedures as set by American Association of Blood Banks (AABB) and strictly followed reagent manufacturer’s instructions for use. The results were recorded as (+) for hemagglutination and (-) for no hemagglutination. A known donor of blood group “O” RhD positive was used as a positive control; another known donor of “O” RhD negative was used as a negative control.
Statistical analysis
Data collected from blood donor register and laboratory test were recorded in a data record sheet that was organized into column of serial number, blood unit number, ABO blood group, RhD status (at immediate spin and antihuman globulin tests). Statistical significance of association between RhD variant phenotypes, donor ABO blood group, tribe and gender was determined using chi-square test. P-value <0.05 was considered as statistically significant at 95% confidence interval (CI).
Ethical considerations
The research protocol was reviewed and approved by the Faculty Research and Ethics Committee (FREC) of the Institute of Allied Health Sciences of International Health Sciences University (IHSU). Permission to use donor blood samples was obtained from the principal medical officer, GRBB.
Results
We analyzed 138 RhD-negative EDTA blood samples. Our blood donors comprised 66.7% (n=92) males. Their median age was 24.4 years (range, 14–33 years). Donors were of varied ethnic tribes, and they had varied ABO blood groups as indicated in Table 1.
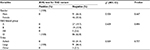  | Table 1 Gender, ABO blood group and ethnicity of blood donor participants Abbreviations: AHG, antihuman globulin; CI, confidence interval. |
Using the antihuman globulin test, the prevalence of RhD variants was 0.7% (95% CI, 0.5–0.9).
There was no statistical association of RhD variant phenotypes with donor gender, tribe and their ABO blood groups.
Discussion
Laboratory analyses to establish and understand RhD antigens have been a major focus for safety in blood transfusion; consequently, >200 variant phenotypes have been described.16,17 The D variants are critical, albeit laboratory typing techniques remain substandard to guarantee blood recipient safety.3,11,12
In this study, the prevalence of RhD variant phenotypes was at 0.7%. This finding is comparable to 0.4% that was reported among RhD-negative blood donors in Morocco;8 however, <4.5% was reported among blood donors in Egypt,7 2.1% in the donor population at the Regional Blood Transfusion Centre in Kenya18 and 6.5% among blood donors in Ghana.9 The difference is attributed to the rather low sample size in our study. The obtained RhD variant phenotype is of great concern considering that this was initially typed as RhD negative, a phenomenon that has been widely attributed to the technique and reagents used.13,19,20 The D antigen is very immunogenic, with ~20–30% of recipients producing anti-D.21–23 To ensure blood safety, it is imperative that D-positive red cells as a result of RhD variant phenotypes are not transfused to patients with anti-D, patients with a history of having anti-D, D-negative women of childbearing age or patients with potential for transfusion dependency. In a concerted effort, the use of indirect AHG test on all RhD-negative donors has been widely recommended to minimize the risk of alloimmunization against the missing epitopes; however, these have not been pragmatically followed in Uganda. To this effect, neglect of such procedures may result in hemolytic blood transfusion reactions and hemolytic disease of fetus and the new born. Additionally, as RhD-negative blood donors are very rare, critical selection and identification of RhD variant phenotypes from RhD-negative donors ought to be rigorous to ensure recipient blood safety as hitherto recommended.3,13,22
Our study used the serological methods to detect RhD variant phenotypes; consequently, it did not distinguish between weak D, partial D and DEL D variants.
Conclusion
The study reveals important findings from which it can be inferred that the unit of blood from the donor who was RhD variant posed a potential risk of alloimmunization when transfused to RhD-negative recipient. Therefore, the universal acceptance for RhD variant tying of all RhD-negative blood donors using indirect antihuman globulin technique has been justified by the outcome of this study.
Acknowledgments
The authors wish to thank the blood donors and the team at GRBB. They acknowledge logistic support from Uganda Blood Transfusion Services (UBTS). They are grateful to Ms. Hope Mbabazi Rukundo and Dr. Bernard Natukunda for reviewing this manuscript.
Author contributions
PO, CO, FW, BM and IMT participated in study conception and design; data acquisition, analysis and interpretation; manuscript drafting and revising. CO, BM and IMT critically revised the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Avent ND, Reid ME. The Rh blood group system: a review. Blood. 2000;95(2):375–387. | ||
Dean L [webpage on the Internet]. Blood group antigens are surface markers on the red blood cell membrane. Blood Groups and Red Cell Antigens. (Chap. 2). Bethesda, MD: National Center for Biotechnology Information (US); 2005. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2264/. Accessed August 26, 2017. | ||
Daniels G. Variants of RhD – current testing and clinical consequences. Br J Haematol. 2013;161(4):461–470. | ||
Flegel WA. Molecular genetics and clinical applications for RH. Transfus Apher Sci. 2011;44(1):81–91. | ||
Flegel WA. The genetics of the Rhesus blood group system. Blood Transfus. 2007;5(2):50–57. | ||
Rizzo C, Castiglia L, Arena E, et al. Weak D and partial D: our experience in daily activity. Blood Transfus. 2012;10(2):235–236. | ||
Hussein E, Teruya J. Weak D types in the Egyptian population. Am J Clin Pathol. 2013;139(6):806–811. | ||
Kabiri Z, Benajibaa M, Hajjout K, Dakka N, Bellaoui H. Prévalence du phénotype Rh D faible chez les donneurs de sang Rh D négatif au Maroc. Immunoanal Biol Spéc. 2013;28(1):36. | ||
Opoku-Okrah C, Amidu N, Amoah-Sakyi S. Detection of weak D (Du) phenotype among Rh-D negative males and females in Kumasi, Ghana. J Sci Technol. 2008;28:34–40. | ||
Kumpel B. Are weak D RBCs really immunogenic? Transfusion. 2006;46(6):1061–1062; discussion 1062–1066. | ||
Chaudhary RK, Das SS. Autoimmune hemolytic anemia: from lab to bedside. Asian J Transfus Sci. 2014;8(1):5–12. | ||
Strobel E. Hemolytic transfusion reactions. Trans Med Hemother. 2008;35(5):346–353. | ||
Westhoff CM. The Rh blood group system in review: a new face for the next decade. Transfus Apher Sci. 2004;44:1663. | ||
Calhun L, Petz LD. Erythrocyte antigens and antibodies. In: Beutler E, Litchman MA, Coller BS, Kipps TJ, editors. Williams Hematology: Fifth Edition. New York: McGraw-Hill Inc; 1995:1595–1610. | ||
Wagner FF, Eicher NI, Jorgensen JR, Lonicer CB, Flegel WA. DNB: a partial D with anti-D frequent in Central Europe. Blood. 2002;100(6):2253–2256. | ||
Scott ML. The complexity of the Rh system. Blood Transfus. 2004;87(1):58–62. | ||
Wagner FF, Frohmajer A, Landewig B, et al. Weak D alleles express distinct phenotype. Blood. 2000;95(8):2699–2708. | ||
Rachel G, Kennedy MK. Prevalence of Weak RhD Phenotype in the Blood Donor Population of Nairobi Regional Blood Transfusion Centre. Vol. 18. Kenya: Africa Sanguine; 2016. | ||
Denomme GA, Dake LR, Vilensky D, Ramyar L, Judd WJ. Rh discrepancies caused by variable reactivity of partial and weak D types with different serologic techniques. Transfusion. 2008;48(3):473–478. | ||
Williams M. Monoclonal reagents for rhesus-D typing of Irish patients and donors: a review. Br J Biomed Sci. 2000;57(2):142–149. | ||
Frohn C, Dumbgen L, Brand J-M, Gorg S, Luhm J, Kirchner H. Probability of anti-D development in D–patients receiving D+RBCs. Transfusion. 2003;43:893–898. | ||
Klein HK, Anstee DJ. Mollison’s Blood Transfusion in Clinical Medicine. 11th ed. Oxford, UK: Blackwell Publishing; 2005. | ||
Yazer MH, Triulzi DJ. Detection of anti-D in D –recipients transfused with D+red blood cells. Transfusion. 2007;47(12):2197–2201. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
