Back to Journals » Journal of Pain Research » Volume 11
Prevalence of pain-related diagnoses in patients with dementia: a nationwide study
Authors Lin PC , Li CH, Chou PL, Chen YM , Lin LC
Received 2 May 2018
Accepted for publication 21 June 2018
Published 3 September 2018 Volume 2018:11 Pages 1589—1598
DOI https://doi.org/10.2147/JPR.S172875
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Pei-Chao Lin,1,2 Chien-Hsun Li,3,4 Pi-Ling Chou,1,2 Yao-Mei Chen,1,5 Li-Chan Lin6
1School of Nursing, College of Nursing, Kaohsiung Medical University, Kaohsiung, Taiwan; 2Department of Medical Research, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan; 3Department of Neurology, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan; 4Department of Neurology, Kaohsiung Municipal Hsiao-Kang Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan; 5International Medical Service Center, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan; 6Institute of Clinical Nursing, National Yang-Ming University, Taipei, Taiwan
Purposes: To investigate the prevalence of pain-related diagnoses in patients with dementia and evaluate the association of pain-related diagnoses with demographic characteristics and dementia subtypes.
Patients and methods: In this population-based retrospective cohort study, participants were recruited from a cohort of 2 million people randomly sampled from the general population in the National Health Insurance Research Database of Taiwan from 2000 to 2013. The index year was defined as the period of 1 year from the date of the first diagnosis of dementia.
Results: The study group comprised 28,450 patients with the dementia subtypes of vascular dementia, Alzheimer’s disease, or other dementia subtypes. The mean age of patients with dementia was 76.75 years. Of all patients with dementia, 49.07% had at least one pain-related diagnosis documented in their outpatient or inpatient claim records within the index year. The top three pain-related diagnoses were osteoarthritis (29.27%), headache (12.53%), and osteoporosis (11.43%). Musculoskeletal diagnosis was more likely in female patients with vascular dementia. Although patients with vascular dementia had a significantly lower prevalence of pain-related diagnosis, they had a significantly higher risk of 1-year mortality than patients with other dementia subtypes.
Conclusion: During the index year, 49.07% of patients with dementia had at least one pain-related diagnosis. To investigate the differences of the use of pain medication in patients with different dementia subtypes and the difference of pain-related diagnosis and treatment in patients with and without dementia, future studies are recommended.
Keywords: Alzheimer’s, dementia, diagnosis, hospital, pain, prevalence
Introduction
With the aging of the global population, the prevalence of dementia is rapidly increasing. The global prevalence of dementia has been estimated to reach 65.7 million in 2030.1 A recent survey conducted in Taiwan showed that the prevalence of dementia was 8.04%, after adjustment for age and all-cause mortality in participants aged 65 years or older.2 Pain is a common symptom in older people with dementia, and its prevalence is 35.3–63.5%.3–6 About 36.6% of older nursing home residents with dementia had pain as measured by an observed pain behavior scale in Taiwan.7 Effective pain management is crucial for ensuring improved quality of life.8 In older patients with dementia, pain may be under-detected and undertreated, particularly in older people with advanced dementia who are unable to communicate their pain.9 One study showed that older people with more severe dementia might experience more severe pain.10
Different methods can be used to assess pain in people with dementia, including self-report scales, observational scales, and proxy reports.4,5 However, finding consistent and general assessment methods for recognizing pain in people with dementia is difficult. If health care professionals could identify patients with dementia who had pain-related diagnoses in a more timely manner, they, along with caregivers, could continuously monitor these patients and conduct pain assessment and treatment.
According to the literature, people with dementia who receive known pain-related diagnoses, such as cancer, headache, osteoporosis, arthritis, and hip fracture, have a higher risk of pain.11–13 These pain-related diagnoses are made by practicing physicians based on consensus diagnostic criteria that include objective physical assessments and relevant examinations. Therefore, pain-related diagnoses made using consistent assessment criteria or principles can reveal the prevalence of pain in the overall dementia population.
According to neurologists, painful experiences might be different among patients with different dementia subtypes because dementia lesions may affect nociceptive pathways,14 although a review article indicated no significant differences in the prevalence of pain in patients with different dementia subtypes;15 nevertheless, another study reported varied rates of self-reported pain in patients with different dementia subtypes and dementia stages.16 The currently available evidence is insufficient for determining whether painful experience and the prevalence of pain are different among patients with different dementia subtypes. In these studies, the pain was assessed by different methods that might not be suitable for the participants’ dementia stages. In addition, in studies only recruiting a few people with dementia, where the majority of dementia subtypes were vascular dementia and Alzheimer’s disease, the other subtypes of dementia were rare. This further lack of available evidence illustrates the challenge of determining whether pain experience is different among patients with different dementia subtypes. However, if primary data on the prevalence of pain-related diagnoses among patients with different dementia subtypes become available, the data might enable health care professionals to pay more attention to certain pain-related diagnoses in patients with specific dementia subtypes.
Researchers have examined the prevalence of pain-related diagnoses and pain treatment in older people with dementia by using health insurance claim data; however, no large-scale study has investigated the prevalence of pain-related diagnoses in people with dementia.17,18 Nearly 99.9% of the inhabitants of Taiwan are enrolled in the National Health Insurance (NHI) program.19 The National Health Insurance Research Database (NHIRD) database includes the medical records in clinics, emergency departments and hospitals, with all enrolled patients’ diagnoses and medicine prescriptions made by practicing physicians being recorded in the NHIRD of Taiwan; therefore, a preliminary nationwide study revealing the overall prevalence of pain-related diagnoses in patients with dementia might serve as a reference for additional pain management studies.
This study investigated the prevalence of pain-related diagnoses in people with dementia and evaluated the association of pain-related diagnoses with demographic characteristics and dementia subtypes by using nationwide data from the NHIRD in Taiwan.
Patients and methods
Design
This population-based retrospective cohort study was conducted using data from the NHIRD of Taiwan. Participants were recruited from a cohort of 2 million people randomly sampled from the general population in the NHIRD from 2000 to 2013. The medical expenditure of more than 99% of the residents of Taiwan (23 million) is covered by the National Health Insurance (NHI) program. All claim data for medical health care services, including hospitalization, emergency department and outpatient clinic visits, have been collected and encrypted in the NHIRD.20 The NHI program covers only the expenditure for medical care and not that for long-term care; therefore, the NHIRD does not include the claim data of nursing home residents. In 2016, our research protocol was approved by the institutional review board of Kaohsiung Medical University Chung-Ho Memorial Hospital (KMUHIRB-SV(I)-20150076).
Study population
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes in the NHIRD are mainly used for data subset construction. All diagnoses were made by practicing physicians on the basis of clinical symptoms and signs and supporting imaging reports from outpatient and/or inpatient departments, hospitals, and clinics. The study group comprised patients with the following dementia subtypes diagnosed based on ICD-9-CM codes: vascular dementia (ICD-9-CM code 290.4), Alzheimer’s disease (ICD-9-CM code 331.0), senile and presenile dementia (ICD-9-CM codes 290.0, 290.1, 290.2, and 290.3), dementia in conditions classified elsewhere (ICD-9-CM code 294.1), frontotemporal dementia (ICD-9-CM code 331.1), senile degeneration of the brain (ICD-9-CM code 331.2), and dementia with Lewy bodies/parkinsonism with dementia (ICD-9-CM code 331.82).21 In Taiwan, the process for dementia diagnosis involves a chief complaint by the patient, cognitive function examination, neurological examination, and laboratory test, and the diagnosis is made by licensed neurologists or psychiatrists.22 According to the diagnostic process, the persons with suspected dementia would visit the hospital at least one or two times for these examinations; therefore, to improve the identification of patients with dementia, only those with at least three outpatient or inpatient claim records of dementia-related diagnosis codes between January 1, 2000, and December 31, 2013,23 and/or those who had filled in a prescription for an anti-dementia drug (anatomical therapeutic chemical [ATC] code: N06D) were included in the study group.24 The date of the first diagnosis of dementia was assigned as the index date for all identified patients with dementia.
According to ICD-9-CM codes, dementia subtypes are categorized into three types: vascular dementia (ICD-9-CM code 290.4), Alzheimer’s disease (ICD-9-CM code 331.0), and others. If patients had filled in a prescription for an anti-dementia drug, they were included in the Alzheimer’s disease group. Demographic data including age, sex, education, marital status, geographic region, and comorbidities were sampled. Comorbidities included hyperlipidemia (ICD-9-CM codes 272.0–272.4), diabetes mellitus (ICD-9-CM code 250), hypertension (ICD-9-CM codes 401–405), acute myocardial infarction (ICD-9-CM code 410), congestive heart failure (ICD-9-CM code 428), cerebrovascular disease (ICD-9-CM codes 430–438), kidney diseases (ICD-9-CM codes 580–589), COPD (ICD-9-CM codes 490–496), head injury (ICD-9-CM codes 850–854 and 95901), depression (ICD-9-CM codes 296.2, 296.3, 300.4, and 31), and schizophrenia (ICD-9-CM code 295).23 The Charlson comorbidity score can predict 1-year mortality; thus, the score is an indicator of disease burden.25 Therefore, the Charlson comorbidity score was also calculated for the study population. The Charlson comorbidity scores were categorized as 0 (1-year mortality rate of 8%), 1 (25%), 2 (48%), and ≥3 (59%).25
Pain-related diagnosis
Because musculoskeletal conditions and fractures are common pain-related conditions and indications for analgesic prescriptions in older people, we included the following musculoskeletal diseases/conditions in this study: rheumatoid arthritis (ICD-9-CM code 714), osteoarthritis (ICD-9-CM code 715), osteoporosis (including osteoporotic fractures) (ICD-9-CM codes 733.0 and 733.1), hip fracture (ICD-9-CM codes 733.14, 733.15, 820, 821.0, and 821.1), wrist fracture (ICD-9-CM codes 813.4, 813.5, 813.8, and 813.9), and vertebral fracture (ICD-9-CM codes 733.13, 805, and 806). Pain-related diagnosis included cancer (ICD-9-CM codes 140–208) and headache (ICD-9-CM code 784.0)/migraine (ICD-9-CM code 346).17 At least one pain-related diagnosis was required to be documented in the outpatient or inpatient claim records within the index year.17 The index year was defined as the period of 1 year from the date of the first diagnosis of dementia.
Statistical analyses
Participants’ demographic characteristics, dementia subtypes, and pain-related diagnosis are presented as descriptive statistics. The chi-squared test and one-way analysis of variance were used to investigate relationships between demographic characteristics, dementia subtypes, and pain-related diagnoses. All tests of statistical significance were two-sided, and statistical significance was defined as α<0.05. Statistical analyses were conducted using SPSS 20.0 (IBM Corp., Armonk, NY, USA).
Results
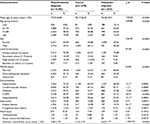
The study group comprised 28,450 patients with dementia, with a mean age of 76.75±9.16 years. Of all patients with dementia, 15,551 (54.66%) were women, and 19,711 (69.49%) had received only primary school education or had not received any education. The top three comorbidities were hypertension (69.10%), cerebrovascular disease (44.71%), and diabetes (31.36%). The mean Charlson comorbidity score was 3.03±2.03. Of all patients with dementia, 13,960 (49.07%) had at least one pain-related diagnosis documented in their outpatient or inpatient claim records within the index year. The top three pain-related diagnoses were osteoarthritis (29.27%), headache (12.53%), and osteoporosis (11.43%) (Table 1).
  | Table 1 Characteristics of patients with all dementia subtypes (N=28,450) |
A comparison of patient characteristics across different dementia subtypes (Table 2) revealed that the vascular dementia group had a significantly lower mean age than the Alzheimer’s disease group and the other dementia subtype group (F=815.59, P<0.0001). The vascular dementia group had a significantly higher percentage of men (52.71%), married people (61.75%), and people with hypertension (78.99%), cerebrovascular disease (74.62%), diabetes (38.08%), and hyperlipidemia (29.04%), compared with the Alzheimer’s disease group and the other dementia subtype group (P<0.0001). The Alzheimer’s disease group had a significantly higher percentage of women (59.02%) and people with a bachelor’s degree or above (10.49%) (P=0.0008). The other dementia subtype group had a significantly higher percentage of people with COPD (28.15%) or depression (17.23%) than the vascular dementia group and Alzheimer’s disease group (P<0.0001).
  | Table 2 Comparison of patient characteristics across different dementia subtypes |
Regarding pain-related diagnoses, the vascular dementia group had a significantly higher percentage of patients with no pain-related diagnosis (58.75%) than the Alzheimer’s disease group and the other dementia subtype group (P<0.0001). The other dementia subtype group had a significantly higher percentage of pain-related musculoskeletal diagnosis including osteoarthritis (30.29%), osteoporosis (11.91%), vertebral fracture (5.99%), hip fracture (4.89%), and wrist fracture (1.24%). Concerning cancer diagnosis, no significant differences were observed among the three dementia subtype groups (P=0.0735) (Table 2).
Table 3 shows a comparison of patient characteristics across different pain-related diagnoses. Demographic characteristics were significantly different among patients with no pain-related diagnosis, musculoskeletal diagnosis, cancer diagnosis, and headache/migraine diagnosis. Patients with dementia and cancer diagnosis were significantly older (78.17±8.47 years) than patients with dementia and other diagnoses. A significantly higher percentage of patients with dementia and musculoskeletal diagnosis were women (64.09%, P<0.0001) and divorced/widowed (41.15%, P<0.0001). Moreover, a significantly higher percentage of patients with dementia and cancer diagnosis were men (60.12%, P<0.0001) and married (63.53%, P<0.0001). Furthermore, a significantly higher percentage of patients with dementia and cancer diagnosis had a bachelor’s degree or above (12.81%, P<0.0001), compared with patients with dementia and musculoskeletal or headache/migraine diagnosis. A significantly higher percentage of patients with dementia and cancer diagnosis had comorbidities such as hypertension (69.34%), diabetes (33.71%), COPD (32.87%), kidney disease (18.98%), and congestive heart failure (13.47%) (P<0.0001).
Discussion
In this study carried out in Taiwan, the majority of patients with dementia were 75–84 years of age, female, married, and had a low education level. These findings of demographic characteristics of people with dementia were similar to the previous nationwide survey study with randomly sampled participants aged 65 years and older from 19 Taiwan counties.26 In the previous study, the majority of the non-dementia population were younger (65–74 years of age) and the percentage of males (51.37%) was slightly higher than females.26 The distribution of education years of non-dementia older people in the previous study was similar to the distribution of education years of older people with dementia in the current study.26 The majority of patients with dementia had a low education level because the education system and economic status in Taiwan were not well developed 50 years ago; however, a relatively high percentage of patients with Alzheimer’s disease had a bachelor’s degree or above. This result was different to the finding of a previous systematic review. The results of the previous review indicated that low education level was associated with a significantly increased risk for Alzheimer’s disease.27 The recent finding of a meta-analysis indicated that both low and high education showed a dose–response trend with risk of Alzheimer’s disease.28 The possible reasons for the results of the current study might be that older persons with high education and their family members have a higher level of awareness and were more willing to accept an established diagnosis of Alzheimer’s disease for treatment. In contrast, the older people with a low education level and their family might have perceived stigmatization of dementia.29 For the vascular subtype of dementia, the people with dementia and family members might like to think vascular dementia was a complication of stroke. Among patients with different dementia subtypes, common comorbidities were hypertension, cerebrovascular disease, and diabetes. The mean Charlson comorbidity score derived for patients with vascular dementia was significantly higher than that derived for patients with Alzheimer’s disease and other dementia subtypes. This finding implies that patients with vascular dementia have a higher risk of 1-year mortality. The findings also highlight that while monitoring patients with dementia for pain-related diagnoses, clinical health care professionals should be aware that patients with different dementia subtypes have a high risk of mortality.
In Taiwan, to be prescribed anticholinesterases (ATC code N06DA) by physicians, patients with Alzheimer’s disease are usually required to have examination reports indicating Alzheimer’s disease; thus, this prescription will be covered by the NHI program. However, patients with Lewy body dementia or Parkinson’s disease dementia are also prescribed other anti-dementia drugs (ATC code N06DX). Therefore, people with Lewy body dementia might be misclassified and erroneously included in the Alzheimer’s group. All other dementia subtypes, besides vascular dementia and Alzheimer’s dementia, were included into one group; this might lead to the group being heterogeneous.
According to our study finding, nearly 50% of patients with dementia had one pain-related diagnosis within the index year. This finding implies that health care professionals should complete primary pain assessment, which can be used as a reference by the multidisciplinary team caring for patients with dementia.18 Osteoarthritis (29.27%) was the most common pain-related diagnosis in patients with dementia in this study. Few studies have explored the prevalence of pain in patients with dementia in hospitals. A previous study showed a higher prevalence of pain due to musculoskeletal conditions including arthritis or osteoarthritis (41.2%) and fractures (4.6%) than that of pain due to headache (6.3%) and cancer (5.0%) in German patients with dementia.18 Similarly, the current study demonstrated that musculoskeletal pain-related diagnosis was more common (36.7%) than headache/migraine diagnosis (6.4%) or cancer diagnosis (5.9%) in patients with dementia. Another previous study indicated that 27% of participants with dementia admitted to general hospitals self-reported pain, and 42.4% of participants experienced pain on movement.6 The aforementioned results highlight that health care professionals in hospitals should assess the potential risks of pain in patients with dementia and musculoskeletal pain-related diagnoses.
A literature review revealed that few studies have explored the association between pain-related diagnoses and dementia subtypes. The findings of the current study indicate that a higher percentage of patients with other dementia subtypes had musculoskeletal pain-related diagnoses, compared with patients with vascular dementia or Alzheimer’s disease. The reason might that be Lewy body dementia and Parkinsonism with dementia were incorporated into the other subtypes dementia. According to the literature, patients with Parkinson’s disease experienced more musculoskeletal pain than the general population.30,31 In addition, patients with dementia with Lewy bodies had significantly poorer motor performance than patients with Alzheimer’s disease;32 consequently, the walking difficulties observed in patients with Lewy bodies and Parkinson’s disease might cause more fractures. Furthermore, a lower percentage of patients with vascular dementia had pain-related diagnosis compared with patients with Alzheimer’s dementia or other dementia subtypes. This finding contrasts with that of a previous study conducted on 199 nursing home residents with dementia.15 That previous study indicated that a higher percentage of residents with vascular dementia self-reported pain compared with residents with Alzheimer’s disease or other dementia subtypes.15 The contrasting findings might be because of the small sample size of the previous study; additionally, the prevalence of pain was measured using a self-report scale and an observational pain scale.15 Dementia lesions might affect nociceptive pathways;14 thus, dementia subtypes may affect the expression of pain and lead to the underdiagnosis of the disease. This hypothesis should be further explored.
The hospice care of patients with dementia under cancer pain is also an important issue.11 A previous study indicated that residents with dementia who died from cancer did not receive any opioids in the hospice.11 In the current study, the frequency of cancer diagnosis was not significantly different among patients with different dementia subtypes. The findings of the current study suggest that health care professionals should pay more attention to pain management in patients with dementia and cancer diagnosis, regardless of the dementia subtype. In addition, people with advanced dementia are also included in the population of hospice care, so it is necessary that health care professionals provide well pain care for people with dementia in hospice.
Strength and limitations
However, there are some limitations, as follows. First, in the current study, the inclusion criteria of patients with dementia were strict, and only patients with at least three outpatient or inpatient claim records of dementia-related diagnosis codes were included; however, these criteria might lead to the underestimation of patients with dementia, particularly among those who rarely visit hospitals or those diagnosed with dementia near the end of 2013. Second, due to the NHIRD database not containing reports or findings of such medical information, this study could not consider dementia severity or report any measure of cognitive function. Third, the insurance system of Taiwan, NHIRD, does not specifically separate the claim data of nursing home residents; therefore this study might have a bias in the identification of patients suffering from dementia in more severe and advanced phases. Future studies should explore the relationship of prevalence of pain, cognitive function, and dementia subtypes.
Fourth, neuropathic pain is a common form of pain in advanced age, and cardiovascular disease is a pain-related diagnosis; however, neuropathic pain is a symptom rather than a pathologic diagnosis,33 so identifying specific diagnostic codes for neuropathic pain in the NHIRD is difficult. Finally, this study included only pain-related diagnoses within 1 year from the date of the first diagnosis of dementia, which was considered the index date; therefore comorbidities and pain-related diagnosis could not be used to generalize the later condition of patients with dementia. Future longitudinal studies should explore the trajectory of pain-related diagnosis and control influencing factors.
The problem of pain in dementia is an increasing focus in health systems. The difficulty of pain assessment for people with dementia is still problematic. This population-based study was able to cover almost all the subjects with dementia from 2000 to 2013. The strength of this study was using differential analysis of pain risk in different subtypes of dementia. It needs to be emphasized that the identification of pain-related comorbidities in dementia only constitutes an estimate of the actual pain status of older people with dementia. The evidence produced in this study could be a reference and a reminder to health care providers to regularly use validated methods or scales to detect the presence of pain and the outcomes after interventions for people with dementia and pain-related comorbidity.
Conclusion
During the index year, half of the patients with dementia had at least one pain-related diagnosis. Musculoskeletal diagnosis was more likely in female patients with vascular dementia. The frequency of cancer diagnosis was not significantly different among patients with different dementia subtypes. Future studies should compare the use of pain medication in patients with different dementia subtypes or compare pain-related diagnosis and treatment in patients with and without dementia. The findings can serve as a reference for health care professionals in assessing pain in dementia in hospitals. Even assessment and treatment of pain in dementia are both complex and difficult. Hence, more knowledge about the prevalence of pain-related diagnosis in patients with dementia will help health care professionals in making decisions regarding pain assessment and treatment. Studies investigating the differences in use of pain medication in patients with different dementia subtypes and the differences of pain-related diagnosis and treatment in patients with and without dementia in the future are recommended.
Preventing painful conditions is one of the outcome indexes of medical and health care. Knowledge about the prevalence of pain-related diagnoses among patients with different dementia subtypes may enable health care professionals to offer more effective pain management. In addition, this study demonstrated that although patients with vascular dementia had a lower prevalence of pain-related diagnosis, they had a higher risk of 1-year mortality. These findings could contribute to better care for patients with dementia.
Acknowledgments
The authors thank the staff of the Center for Medical Informatics and Statistics, Kaohsiung Medical University for their help. This work was supported by the Ministry of Science and Technology, Republic of China (MOST 105-2314-B-037-071). The publication fee was supported by the Ministry of Science and Technology, Republic of China (MOST 106-2314-B-037-048-MY2).
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Prince M, Bryce R, Albanese E, et al. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9(1):63–75. | ||
Sun Y, Lee HJ, Yang SC, et al. A nationwide survey of mild cognitive impairment and dementia, including very mild dementia, in Taiwan. PLoS One. 2014;9(6):e100303. | ||
Barry HE, Parsons C, Passmore AP, Hughes CM. Pain in care home residents with dementia: an exploration of frequency, prescribing and relatives’ perspectives. Int J Geriatr Psychiatry. 2015;30(1):55–63. | ||
Lukas A, Schuler M, Fischer TW, et al. Pain and dementia: a diagnostic challenge. Z Gerontol Geriatr. 2012;45(1):45–49. | ||
Orgeta V, Orrell M, Edwards RT, et al. Self- and carer-rated pain in people with dementia: influences of pain in carers. J Pain Symptom Manage. 2015;49(6):1042–1049. | ||
Sampson EL, White N, Lord K, et al. Pain, agitation, and behavioural problems in people with dementia admitted to general hospital wards: a longitudinal cohort study. Pain. 2015;156(4):675–683. | ||
Lin PC, Lin LC, Shyu YI, Hua MS. Predictors of pain in nursing home residents with dementia: a cross-sectional study. J Clin Nurs. 2011;20(13–14):1849–1857. | ||
Booker SS, Booker RD. Shifting paradigms: advance care planning for pain management in older adults with dementia. Gerontologist. 2018;58(3):420–427. | ||
Hadjistavropoulos T, Herr K, Prkachin KM, et al. Pain assessment in elderly adults with dementia. Lancet Neurol. 2014;13(12):1216–1227. | ||
Rajkumar AP, Ballard C, Fossey J, et al. Epidemiology of pain in people with dementia living in care homes: longitudinal course, prevalence, and treatment implications. J Am Med Dir Assoc. 2017;18(5):453.e1–453.e6. | ||
Monroe TB, Carter MA, Feldt KS, et al. Pain and hospice care in nursing home residents with dementia and terminal cancer. Geriatr Gerontol Int. 2013;13(4):1018–1025. | ||
Velly AM, Mohit S. Epidemiology of pain and relation to psychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2017:S0278-5846(17)30194-X. | ||
Proctor WR, Hirdes JP. Pain and cognitive status among nursing home residents in Canada. Pain Res Manag. 2001;6(3):119–125. | ||
Álvaro González LC. The neurologist facing pain in dementia. Neurologia. 2015;30(9):574–585. | ||
van Kooten J, Binnekade TT, van der Wouden JC, et al. A review of pain prevalence in alzheimer’s, vascular, frontotemporal and lewy body dementias. Dement Geriatr Cogn Disord. 2016;41(3–4):220–232. | ||
van Kooten J, Smalbrugge M, van der Wouden JC, Stek ML, Hertogh C. Prevalence of pain in nursing home residents: the role of dementia stage and dementia subtypes. J Am Med Dir Assoc. 2017;18(6):522–527. | ||
Haasum Y, Fastbom J, Fratiglioni L, Kåreholt I, Johnell K. Pain treatment in elderly persons with and without dementia: a population-based study of institutionalized and home-dwelling elderly. Drugs Aging. 2011;28(4):283–293. | ||
Hoffmann F, van den Bussche H, Wiese B, Glaeske G, Kaduszkiewicz H. Diagnoses indicating pain and analgesic drug prescription in patients with dementia: a comparison to age- and sex-matched controls. BMC Geriatr. 2014;14:20. | ||
Cheng TM. The Taiwan Health Care System; 2017. Available from: http://international.commonwealthfund.org/countries/taiwan/. Accessed August 25, 2017. | ||
Center for Biomedical Resources of National Health Research Institutes. National Health Insurance Research Database, Taiwan. Available from: https://nhird.nhri.org.tw/en/index.html. Accessed October 14, 2017. | ||
Wang HK, Hung CM, Lin SH, et al. Increased risk of hip fractures in patients with dementia: a nationwide population-based study. BMC Neurol. 2014;14:175. | ||
Liu CK, Lai CL, Tai CT, et al. Incidence and subtypes of dementia in southern Taiwan: impact of socio-demographic factors. Neurology. 1998;50(6):1572–1579. | ||
Hsiao FY, Peng LN, Lin MH, Chen LK. Dose-responsive effect of psychotropic drug use and subsequent dementia: a nationwide propensity score matched case-control study in Taiwan. J Am Med Dir Assoc. 2014;15(7):509–513. | ||
Jensen-Dahm C, Palm H, Gasse C, Dahl JB, Waldemar G. Postoperative treatment of pain after hip fracture in elderly patients with dementia. Dement Geriatr Cogn Disord. 2016;41(3–4):181–191. | ||
Charlson ME, Pompei P, Ales KL, Mackenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. | ||
Chen TB, Yiao SY, Sun Y, et al. Comorbidity and dementia: a nationwide survey in Taiwan. PLoS One. 2017;12(4):e0175475. | ||
Sharp ES, Gatz M. Relationship between education and dementia: an updated systematic review. Alzheimer Dis Assoc Disord. 2011;25(4):289–304. | ||
Xu W, Tan L, Wang HF, et al. Education and risk of dementia: dose-response meta-analysis of prospective cohort studies. Mol Neurobiol. 2016;53(5):3113–3123. | ||
Lee IC. Patients wish to overcome stigma of dementia: report. Taipei Times; 2012. Available from: http://www.taipeitimes.com/News/taiwan/archives/2012/09/22/2003543392. Accessed October 14, 2017. | ||
Beiske AG, Loge JH, Rønningen A, Svensson E. Pain in Parkinson’s disease: Prevalence and characteristics. Pain. 2009;141(1–2):173–177. | ||
Hanagasi HA, Akat S, Gurvit H, Yazici J, Emre M. Pain is common in Parkinson’s disease. Clin Neurol Neurosurg. 2011;113(1):11–13. | ||
Fritz NE, Kegelmeyer DA, Kloos AD, et al. Motor performance differentiates individuals with Lewy body dementia, Parkinson’s and Alzheimer’s disease. Gait Posture. 2016;50:1–7. | ||
Shadd JD, Ryan BL, Maddocks HL, Mckay SD, Moulin DE. Neuropathic pain in a primary care electronic health record database. Eur J Pain. 2015;19(5):715–721. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.