Back to Journals » Clinical Ophthalmology » Volume 12
Prevalence of ocular morbidity among children aged 17 years or younger in the eastern India
Authors Rao GN, Sabnam S, Pal S, Rizwan H, Thakur B, Pal A
Received 20 April 2018
Accepted for publication 10 July 2018
Published 6 September 2018 Volume 2018:12 Pages 1645—1652
DOI https://doi.org/10.2147/OPTH.S171822
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Video abstract presented by G Nageswar Rao.
Views: 142
G Nageswar Rao,1 Silpa Sabnam,2 Sweta Pal,2 Huma Rizwan,2 Bhaskar Thakur,3 Arttatrana Pal4
1Department of Ophthalmology, Kalinga Institute of Medical Sciences, Kalinga Institute of Industrial Technology, Bhubaneswar, India; 2School of Biotechnology, KIIT Deemed to be University, Bhubaneswar, India; 3Department of Ophthalmology, Kalinga Institute of Medical Sciences, KIIT Deemed to be University, Bhubaneswar, India; 4Department of Zoology, School of Life Sciences, Mahatma Gandhi Central University, Motihari, Bihar, India
Purpose: Childhood ocular morbidity involves a spectrum of eye diseases that critically impact the mental development, future education and quality of life. However, there is limited evidence about the early detection and appropriate treatment of ocular morbidity in children <20 years. This study was aimed to assess the prevalence and make a comparison between the different types of ocular morbidity in children of both sexes in the age group of 6–17 years in the eastern India.
Methods: A cross-sectional survey of ocular morbidity among children <17 years of age who presented at the Department of Ophthalmology, Kalinga Institute of Medical Sciences, Bhubaneswar, and Vision Care Center for Retina, Bhubaneswar, in the eastern India between January 2015 and March 2018 was accomplished. Demographic information, visual acuity, type of eye injury, refractive errors and other detailed ophthalmic examination were screened.
Results: A total of 633 children (age 6–17 years) were examined in this study. The majority of cases were observed in children of age 12–17 years, accounting for almost close to half of all the cases. The prevalence of ocular morbidity was 45.92% in males and 53.97% in females. The most common ocular morbidity in children encountered was refractive error (54.62%), followed by congenital abnormalities (9%), allergic conjunctivitis (8.52%) and traumatic eye injury (7.1%). There was an increase in ocular morbidity with age, especially the refractive error and congenital abnormalities.
Conclusion: A large number of ocular morbidity was observed in children of age <17 years. Since most of this morbidity was preventable or treatable, reasonable service for ocular morbidity and early age screening are effective methods to reduce this load. Moreover, health education for the prevention of childhood ocular morbidity and, at the same time, early presentation of children to ophthalmic hospitals for the treatment of eye disorders are essential.
Keywords: ocular morbidity, prevalence, eye injury, children, eastern India
Introduction
Visual dysfunction is a global problem being faced today that has a tremendous influence on the economically backward society. Although it is more prevalent in elderly individuals, a lot of children also develop vision disabilities in early age in some or the other form. According to the current estimates, 285 million people are affected by vision disabilities worldwide, 39 million people with blindness and 246 million people with subnormal vision.1 More importantly, information about the prevalence of eye disorders in younger populations specifically in children is limited. Recently, studies have demonstrated that >30% of India’s blind people lose their vision before the age of 17 years, and interestingly, many of them are <5 years also.2,3
The global scenario reveals uncorrected refractive errors as the cause in most cases, leading to moderate and severe visual dysfunction. Recently, a population-based survey in Nairobi, Africa, had reported that only 0.1% of the sample was blind, while ocular morbidities such as conjunctival disorders and refractive error were found in 7.6% and 5.6% of the population, respectively.4 A similar kind of study was observed in Pakistan and it was found that prevalence of ocular morbidity what the authors termed non-vision impairing conditions was 30.6% including presbyopia.5 On the other hand, ocular trauma is an important cause of eye disorder in children worldwide, which has a significant socioeconomic impact.6 A recent study has revealed that childhood blindness was a priority area to look after because of the number of years of blindness that ensues.3 Ocular trauma in children accounts for up to one-third of all ocular trauma admissions, with significant economic allusions for health care providers. More importantly, development of strategies against ocular morbidity to reduce the incidence and severity of pediatric ocular trauma requires an understanding of the epidemiology of these injuries and their characteristics.2,3 However, there is no standardized methodology or techniques for the collection of global cross-sectional data or information in pediatric ocular morbidity and the ability to undertake detailed epidemiological and health economic analyses.
More importantly, information on the prevalence and causes of blindness and severe visual impairment in children is needed for planning and evaluating preventive and curative majors for children. Effective methods of vision screening in children are useful in detecting correctable causes of visual dysfunction and in minimizing long-term visual disability.7 Let no child miss the beauty of the nature, pleasure and opportunities that this world has for them. Therefore, we have aimed to diagnose the prevalence of ocular morbidity among children of the age group 6–17 years.
Methods
Study design and participants
A cross-sectional retrospective study was carried out in children who have attended the Department of Ophthalmology, Kalinga Institute of Medical Sciences (KIMS), KIIT, Bhubaneswar, India, and Vision Care Center for Retina, Bhubaneswar, India, from January 2015 to March 2018. Moreover, we included all the children who were referred from other departments of KIMS, including pediatric department with minor eye complications. The study was approved by the ethics committee of the KIMS Hospital. After explaining the purpose of the study and what was required of a subject, permission and written informed consent were obtained from children and from each participant or parent/guardian in the case of a child. Along with eye complications, patient history was recorded from the children and the parents. Basically, all the data were recorded and questions were asked from each patient attending the Department of Ophthalmology. However, the parents were asked the questions in children of age <12 years. On the whole, the questionnaire dealt with information regarding the children’s age, sex, residential address (location of resident), studying or not studying, chief complications related to one eye or both the eyes and duration of complications. In addition, the questionnaire included detailed ophthalmic examinations for diagnosing ocular morbidity and recording of vitamin A deficiency signs and their ocular manifestations. The basic ophthalmological examinations such as visual acuity (VA) test by using Snellen VA chart at 6 m with the best-corrected vision, syringing and probing to find out and rule out the patency or blockage of the lacrimal drainage system were carried out in each child by an optometrist. The more specific eye examination such as slit-lamp examination for anterior segment, when needed dialated fundus examination by using slit lamp with +90 diopter lens and indirect ophthalmoscope, tear film breakup time for the diagnosis of dry eye, fluorescein staining of the cornea for the detection of corneal abrasion and intraocular pressure measurement by an applanation tonometer were carried out by an ophthalmologist. Children with VA <6/9 underwent a pinhole vision to differentiate refractive errors from pathological conditions. Refractive error was diagnosed when a VA worse than 6/9 improved using the pinhole test. Cycloplegic refraction in younger children <12 years of age and undilated retinoscopy in older children >12 years of age followed by subjective correction was done with uncorrected VA <6/6. The VA worse than 6/60 was recorded as counting fingers (CF; at a certain number of feet), hand motion (HM), light perception (LP), or no light perception (NLP). Moreover, the conversion of Snellen acuity to CF acuity was then recorded. Ocular movements were checked, and convergence insufficiency was elicited by noting the near point of convergence diagnosed if it was reduced along with decreased positive fusional convergence amplitudes at near.8 Visual axis alignment was checked using the cover test. Children with a history of night blindness were thoroughly examined to rule out vitamin A deficiency, keeping in mind the telltale signs such as conjunctival xerosis, Bitot’s spots, corneal xerosis or keratomalacia and fundus abnormalities. Children with headache having no evidence of ocular pathology were subjected to otolaryngology expert to rule out frontal sinusitis.
Statistical analysis
Interpretation and analysis of the data were done using PrismPad software and Student’s t-test analysis.
Results
A total of 633 children of age 6–17 years were examined for ocular morbidity. The children were divided into four groups: Group I (6–9 years), Group II (9–12 years), Group III (12–15 years) and Group IV (15–17 years). There were 34 males and 43 females in Group I, 69 males and 92 females in Group II, 143 males and 159 females in Group III and 45 males and 48 females in Group IV. Age group and sex-wise distribution of children having ocular morbidity was carried out. Overall prevalence of ocular morbidity among all children of age 6–17 years was calculated in both males and females (Table 1). Myopia (24.8%) constituted the major cause of ocular morbidity followed by myopic astigmatism (15.63%), congenital abnormalities (9%), allergic conjunctivitis (8.53%), hypermetropia (7.74%), traumatic eye injury (7.1%), hypermetropic astigmatism (6.47%), blepharitis (5.05%), vitamin A deficiency (4.58%), strabismus (4.1%), anisometropic amblyopia (3.94%) and frontal sinusitis (3%). There was sex-wise preponderance for overall prevalence of ocular morbidity. More importantly, in females, ocular morbidities such as myopia, myopic astigmatism, hypermetropic astigmatism, anisometropic amblyopia, strabismus, allergic conjunctivitis, congenital abnormalities and traumatic eye injuries were more prevalent than in males, and hypermetropia, blepharitis, vitamin A deficiency and frontal sinusitis were more prevalent in males. Further, Table 2 lists groupwise distribution of various types of ocular morbidity in children aged <17 years. Irrespective of sex, all the ocular morbidities were more prevalent in 12–15 age group and statistically significant (P<0.0001). However, blepharitis and traumatic eye injuries were significantly more prevalent in 9–12 age group (P<0.0001). Next, Table 3 shows the comparison of ocular morbidity between children of both sexes <12 years of age and >12 years of age. In both the age groups, females had shown a higher prevalence of myopia, myopic astigmatism, hypermetropic astigmatism, anisometropic amblyopia, strabismus, congenital abnormalities and frontal sinusitis, whereas the males were more prevalent for hypermetropia, vitamin A deficiency and blepharitis. Children aged <12 years had shown a higher prevalence for allergic conjunctivitis, and traumatic eye injury was common in older children aged >12 years.
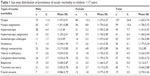  | Table 1 Sex-wise distribution of prevalence of ocular morbidity in children <17 years |
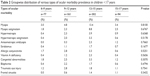  | Table 2 Groupwise distribution of various types of ocular morbidity prevalence in children <17 years |
  | Table 3 Comparison of prevalence of ocular morbidity between children <12 years vs children >12 years |
Myopia was a common disability affecting 11.53% of males and 13.27% of females as against hypermetropia affecting 4.42% of males and 3.31% of females (Figure 1A and B). On the other hand, refractive errors were the most common ocular disorders in children aged <17 years. Out of 633 children examined, a total of 346 children between 6 and 17 years of age were detected with refractive errors. From the rest, 25 were detected with anisometropic amblyopia, 26 with strabismus, 54 with allergic conjunctivitis, 29 with vitamin A deficiency, 57 with congenital abnormalities, 32 with blepharitis, 45 with traumatic eye injury and 19 with frontal sinusitis. Likewise, alternate divergent strabismus or squint was more common than alternate convergent squint. A total of 8.53% (males 3.63%, females 4.89%) of children were detected with allergic conjunctivitis, more specifically vernal conjunctivitis. Vernal keratoconjunctivitis is a recurrent, bilateral and self-limiting inflammation of conjunctiva, having a periodic seasonal incidence (Figure 2A and B). In all, 4.58% (male 2.68%, female 1.89%) were detected with vitamin A deficiency. In all, 9% (males 3.79%, females 5.21%) of children were detected with congenital abnormalities. A total of 5.05% (males 3%, females 2.05%) of children were diagnosed with blepharitis, characterized by inflammation of the eyelids. In all, 7.10% (males 3.31%, females 3.79%) of children were having traumatic eye injuries ranging from a trivial injury manifested as subconjunctival hemorrhage (Figure 3), corneal foreign body (Figure 4), more severe vision threatening retinal injuries like commotio retinae (Figure 5A), posterior pole choroidal tear with subretinal hemorrhage (Figure 5B), large lacerated retinal tear (Figure 5C) and rhegmatogenous retinal detachment (Figure 5D). Again, 3% (males 1.10%, females 1.89%) of children were diagnosed with frontal sinusitis.
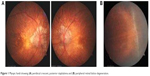  | Figure 1 Myopic fundi showing (A) peridiscal crescent, posterior staphyloma and (B) peripheral retinal lattice degeneration. |
  | Figure 2 Right eye showing VKC (A) early stage and (B) late stage. |
  | Figure 3 Eye showing subconjunctival hemorrhage. |
  | Figure 4 Eyes showing superficially embedded corneal foreign body. |
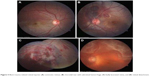  | Figure 5 Blunt trauma-related retinal injuries: (A) commotio retinae, (B) choroidal tear with subretinal hemorrhage, (C) badly lacerated retina, and (D) retinal detachment. |
Discussion
This study conducted in Bhubaneswar, Odisha, a part of eastern India, confirms the high prevalence of ocular morbidity in children. More importantly, the prevalence of ocular morbidity among children is not gamely available for India except few cases, that to a specific locality. In addition, the results of available studies are not comparable because of different methodologies and criteria used in these studies. Here, our results are similar to the findings from other studies in India, suggesting that ocular morbidity is a serious and significant health issue among children that requires an adequate health system response and an urgent need of appropriate eye care programs targeting children to reduce the burden of visual impairment among the younger population.
In our study, we compared the groupwise distribution of various types of ocular morbidity prevalent in different age groups of children from 6 to 17 years of age. The refractive error was the most common and leading cause of the ocular morbidity, which is consistent with other studies done in the same setting.9 Specifically, in case of myopia, 7.89% of children were affected within the age group of 6–12 years, which increased to almost two-fold in the age group of 12–17 years, ie, 16.89%. In myopic astigmatism also, we observed increase, ie, from 4.25% to 11.36% (almost three-fold increase), compared to both the age groups. In all other cases, there was an increase in percentage of occurrence but with slight changes. The prevalence of ocular morbidity was 45.92% in males and 53.97% in females. These results were comparable with a Delhi-based study conducted by Kumar et al10 who reported a 22.7% prevalence. Gupta et al3 reported a similar 31.6% prevalence in Shimla. A study by Chaturvedi and Aggarwal11 reported 40% prevalence, which was also comparable with that in our study. The present study showed a rise in ocular morbidity with increasing age, which was comparable with a study conducted by Kumar et al.10 This could be due to increase in awareness among children with age, which enables them to talk about their problems more openly with the doctor, resulting in higher reporting of ocular problems among older children. However, the study conducted by Desai et al12 reported a decline in the ocular morbidity with increasing age, which did not match with the results of our study. Younger children are unable to express themselves due to which many diseases go unnoticed. Hence, children in the younger age group should be regularly, thoroughly and patiently examined so that early detection can be done and long-term visual impairment can be reduced.
Myopic astigmatism increased almost four-fold (2.36%–8.84%) between these age groups. However, hypermetropia and hypermetropic astigmatism did not show such an increase. In case of anisometropic amblyopia, strabismus, allergic conjunctivitis, vitamin A deficiency, congenital abnormalities, blepharitis, traumatic eye injury and sinusitis, there was no significant increase in the percentage of occurrence and was uniformly divided in all age groups. More importantly, the range of age groups covered in the abovementioned studies in different geographical localities of India was also more as compared to that in the present study conducted at eastern India. On the other hand, lower prevalence, ~15%, of ocular morbidity was reported from Kolkata, another locality of eastern India, among children of 5–13 years.13 Apart from India, many studies have demonstrated a lower prevalence of ocular morbidity in children aged 7–19 years in Africa, Finland, Chile and Nepal as compared to the present study.14–16 May be the difference in prevalence of ocular morbidity in different continents are due to racial and ethnic variations and also partly due to different lifestyles, living conditions and food habits.
Myopic astigmatism and hypermetropic astigmatism are a combination of astigmatism and myopia or hypermetropia where an optometrist assesses the difference in shape of each of the meridians of the eye of patients. This is characterized by an irregularly shaped cornea; however, varying optical shapes can cause differences in vision. It is the result of an inability of the cornea to appropriately focus an image onto the retina of eye, resulting in blurred image. Myopic astigmatism and hypermetropic astigmatism constituted 6.79% and 2.52% in males and 8.84% and 3.94% in females, respectively. From the rest, 3.94% (males 1.73%, females 2.21%) of children were detected with anisometropic amblyopia. A research report demonstrated that anisometropic amblyopia occurs when unequal focus between the two eyes causes chronic blur on one retina.17 In all, 4.10% (males 1.42%, females 2.68%) of children were detected with strabismus or crossed eyes. This is a condition in which the eyes do not properly align with each other when looking at an object at one time.18 If present during a large part of childhood, it may result in amblyopia or loss of depth perception in children and may lead to double vision. Starting from myopia till frontal sinusitis, a negligible number of children were found to be <9 years of age. However, it started increasing steadily in children of the age group 9–17 years.
Essentially, vitamin A includes three forms such as retinol, beta-carotene and carotenoid.19 An earlier report by Desai et al12 demonstrated that prevalence of vitamin A deficiency decreased with increasing age. The prevalence of vitamin A deficiency in the present study is comparable to results of earlier studies showing prevalence to vary from 0.29% to 0.3% in different parts of India such as Haryana and North India,20,21 and 5.3% and Bitot’s spots as 0.6% among school children of age 7–19 years in Tanzania, Africa.21 Many studies have reported that the prevalence of squint varies in children in the age group of 5–19 years in Haryana, Rajasthan, West Bengal and Delhi,19,20 which is comparable with the findings of the present study.
Similar to other studies of ocular morbidity, the allergic conjunctivitis is very common in different age groups of children. There was a strong association between these ocular morbidities, which increased with the age of children. Conjunctival conditions were associated with younger age groups, most likely due to a high prevalence of allergic conjunctivitis (3%–17.5%) among younger children,22–24 which is similar to our present study (8.52%, 3.63% in males and 4.89% in females). The variation in the prevalence of conjunctivitis in different age groups of children and sexes may be due to differences in socioeconomic status, personal hygiene of children, seasonal variations of occurrence of conjunctivitis, lifestyle and geographical location. There is minor variation in the prevalence of ocular diseases among male and female children in the present study, which is comparable to the results of the study by Sehgal et al25 in Delhi (males 46.1% and females 48.3%). On the other hand, the higher prevalence in female children (73.5%) as compared to male children (49.4%) in Haryana, India.19 Basically, this was due to prevalence of infectious diseases such as trachoma, conjunctivitis and blepharitis, which was high among females. More importantly, this is a hospital-based retrospective study design and sample size was not calculated; all eligible subjects from January 2015 to March 2018 were taken into consideration.
Conclusion
The findings from Odisha, eastern India, suggest that a range of different eye complications affects a large number of individuals and highlights the urgent need to implement health facility-based, cost-effective strategies and appropriate eye care programs targeting both early and late-aged children to reduce the burden of visual impairment among the younger children. Health education activities should be intensified regarding signs and symptoms of ocular complications, and particular attention needs to be given for training and supervision of skilled staff and adequate information and referral systems to the locality. Poor vision in childhood affects performance in daily activities in school or at work and has a negative influence on the future life of children. Early detection and management reduce the disease progression and can prevent visual disability. This study will be very helpful, which has been carried out in eastern India, reporting the prevalence of pediatric ocular morbidity and providing comprehensive comparative data of the ocular disease pattern prevalent in the region. It would form a foundation pillar for future planning and management in Odisha.
Acknowledgments
We would like to thank all the staff of the Department of Ophthalmology, KIMS, KIIT Deemed to be University Bhubaneswar, India, and Vision Care Center for Retina, Bhubaneswar, India, for skilful technical assistance.
Disclosure
The authors report no conflicts of interest in this work.
References
Mariotti SP. World Health Organization. 20 Avenue Appia, 1211 Geneva 27. Switzerland; 2010. | ||
Vision screening in school children. In: Training Module. Danish Assistance to the National Programme for Control of Blindness; New Delhi, India. 1. | ||
Gupta M, Gupta BP, Chauhan A, Bhardwaj A. Ocular morbidity prevalence among school children in Shimla, Himachal, North India. Indian J Ophthalmol. 2009;57(2):133–138. | ||
Karimurio J, Kimani K, Gichuhi S, Marco S, Nyaga G. Eye disease and visual impairment in Kibera and Dagoreti Divisions of Nairobi, Kenya. East African Journal of Ophthalmology. 2008;14:41–49. | ||
Hussain A, Awan H, Khan MD. Prevalence of non-vision-impairing conditions in a village in Chakwal district, Punjab, Pakistan. Ophthalmic Epidemiol. 2004;11(5):413–426. | ||
Kimani K, Lindfield R, Senyonjo L, Mwaniki A, Schmidt E. Prevalence and causes of ocular morbidity in Mbeere District, Kenya. Results of a population-based survey. PLoS One. 2013;8(8):e70009. | ||
Saxena R, Vashist P, Tandon R, et al. Incidence and progression of myopia and associated factors in urban school children in Delhi: The North India Myopia Study (NIM Study). PLoS One. 2017;12(12):e0189774. | ||
Von Noorden GK. Binocular vision and ocular morbidity: Theory and management of Strabismus. Mosby year book. 5th ed; 1995:468–476. | ||
Khan AR, Lateef ZN, Yousuf SA, Alramadan MJ, Khan SA, Fatima S. A study of ocular morbidity, utilization, and impact on patient’s satisfaction in an ophthalmic clinic at primary health center in Al Ahsa district of Saudi Arabia. Quality in Primary Care. 2015;23:78–84. | ||
Kumar R, Mehra M, Dabas P, Kamlesh, Raha R. A study of ocular infections amongst primary school children in Delhi. J Commun Dis. 2004;36(2):121–126. | ||
Chaturvedi S, Aggarwal OP. Pattern and distribution of ocular morbidity in primary school children of rural Delhi. Asia Pac J Public Health. 1999;11(1):30–33. | ||
Desai S, Desai R, Desai NC, Lohiya S, Bhargava G, Kumar K. School eye health appraisal. Indian J Ophthalmol. 1989;37(4):173–175. | ||
Singh V, Malik KPS, Malik VK, Jain K. Prevalence of ocular morbidity in school going children in West Uttar Pradesh. Indian J Ophthalmol. 2017;65(6):500–508. | ||
Datta A, Choudhury N, Kundu K. An epidemiological study of ocular condition among primary school children of Calcutta Corporation. Indian J Ophthalmol. 1983;31(5):505–510. | ||
Laatikainen L, Erkkilä H. Refractive errors and other ocular findings in school children. Acta Ophthalmol. 1980;58(1):129–136. | ||
Maul E, Barroso S, Munoz SR, Sperduto RD, Ellwein LB. Refractive Error Study in Children: results from La Florida, Chile. Am J Ophthalmol. 2000;129(4):445–454. | ||
Negrel AD, Maul E, Pokharel GP, Zhao J, Ellwein LB. Refractive Error Study in Children: sampling and measurement methods for a multi-country survey. Am J Ophthalmol. 2000;129(4):421–426. | ||
Singal A, Aggarwal P, Pandhi D, Rohatgi J. Cutaneous tuberculosis and phlyctenular keratoconjunctivitis: a forgotten association. Indian J Dermatol Venereol Leprol. 2006;72(4):290–292. | ||
Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243–260. | ||
Deng L, Gwiazda JE. Anisometropia in children from infancy to 15 years. Invest Ophthalmol Vis Sci. 2012;53(7):3782–3787. | ||
Khurana AK, Sikka KL, Parmar IP, Aggarwal SK. Ocular morbidity among school children in Rohtak City. Indian J Public Health. 1984;28(4):217–220. | ||
Pratap VB, Lal HB. Pattern of paediatric ocular problems in north India. Indian J Ophthalmol. 1989;37(4):171–172. | ||
Wedner SH, Ross DA, Balira R, Kaji L, Foster A. Prevalence of eye diseases in primary school children in a rural area of Tanzania. Br J Ophthalmol. 2000;84(11):1291–1297. | ||
Robinson B, Acorn CJ, Millar CC, Lyle WM. The prevalence of selected ocular diseases and conditions. Optom Vis Sci. 1997;74(2):79–91. | ||
Sehgal K, Kant L, Jain BK, Lal K. Prevalence of eye diseases in a semi-urban area. Indian J Public Health. 1984;28(4):189–193. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
