Back to Journals » Risk Management and Healthcare Policy » Volume 14
Prevalence of Musculoskeletal Diseases of the Upper Extremity Among Dental Professionals in Germany
Authors Rickert C , Fels U, Gosheger G, Kalisch T , Liem D, Klingebiel S, Schneider KN, Schorn D
Received 22 April 2021
Accepted for publication 10 August 2021
Published 11 September 2021 Volume 2021:14 Pages 3755—3766
DOI https://doi.org/10.2147/RMHP.S316795
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Carolin Rickert,1,* Ulrike Fels,1,* Georg Gosheger,1 Tobias Kalisch,1 Dennis Liem,2 Sebastian Klingebiel,1 Kristian Nikolaus Schneider,1 Dominik Schorn1
1Department of General Orthopedics and Tumor Orthopedics, Münster University Hospital, Münster, Germany; 2Sporthopaedicum Berlin, Berlin, Germany
*These authors contributed equally to this work
Correspondence: Carolin Rickert
Department of General Orthopedics and Tumor Orthopedics, Münster University Hospital, Albert-Schweitzer Campus 1, Gebäude A1, Münster, 48149, Germany
Email [email protected]
Objective: Although many findings on occupational musculoskeletal complaints are available from American and European dentists, the corresponding data from Germany are still scarce. Therefore, the aim of this study was to provide additional information on the prevalence of and risk factors for musculoskeletal disorders of the upper extremity, particularly the shoulder in this specific population.
Methods: A written survey was carried out among 600 dentists in the state of North Rhine-Westphalia, Germany. Questionnaire items included physical and psychosocial workload, general health, and the occurrence of musculoskeletal symptoms during the previous 12 months that led to sick leave and medical care according to a modified version of the Nordic Musculoskeletal Questionnaire (NMQ). Regression analysis was used to evaluate relevant risk factors for severe musculoskeletal disorders.
Results: A total of 229 dentists were participated in the study (response rate 38%). Overall, 92.6% of the participants had already suffered from musculoskeletal symptoms in at least one body region. Symptoms were mostly reported in the neck (65.1%) and in the shoulder (58.1%). Limitations in daily activities were experienced by 15.9% due to neck pain and by 15.4% due to shoulder pain. Medical care was sought by 23.7% because of neck pain and by 21.1% due to shoulder pain. Risk factors for symptoms in the upper extremity regions were gender (female), increased physical load, and numerous comorbidities.
Conclusion: There is a high prevalence of musculoskeletal disorders among dentists. Suitable interventions are therefore needed to prevent musculoskeletal diseases and pain among dental professionals, with particular attention to female dentists.
Keywords: musculoskeletal disease, prevalence, dentists, risk factors, occupational exposure
Introduction
Musculoskeletal disorders (MSD) and pain are a common health burden among dental professionals in Western countries. A healthy musculoskeletal system is particularly important in the profession, as dental practice is physically and mentally demanding. Dentists have to perform precise movements with their hands, using oscillating instruments. They often work in static postures, performing repetitive activities over a longer period.1
As dental professionals mainly use the upper regions of the body while working, they are particularly vulnerable to MDS and pain in the upper extremity, as a recent meta-analysis of 30 studies showed.2 Particularly during treatment of patients and administrative work, which account for around 70% of all daily tasks, parts of the upper extremities such as the hand and shoulder are increasingly subject to muscle strain.3 The literature reports a prevalence of work-related MSD in 64–93% of dental professionals.4 Mainly involved regions of the body are the neck, lumbar back, shoulders and wrists.2,5–8 In the literature reported neck pain ranges from 20‐84.9% and shoulder pain from 18.9‐73.5%.9 Similar results were documented by an earlier review, which focused on neck and shoulder disorders. The authors reported a prevalence of 26‐73% for neck symptoms and 20‐65% for shoulder symptoms in dentists in the observation period of one year.9 Generally, symptoms may range from pain, decreased strength, or swelling of the affected area. These symptoms can manifest through a variety of mechanisms, including decreased muscle function, impaired nerve conduction, strains, and partial ruptures of muscles, tendons, and ligaments, or degeneration or microfracture of the bone. In addition to acute injury, chronic conditions that can result from long-term overexposure have also been described in the literature, including arthritis, tendinitis, osteoarthritis and carpal tunnel syndrome.4,10,11
While working, dentists usually maintain in uncomfortable static postures and keep their head in a rotated position, with the neck flexed and shoulders abducted, or tolerate other awkward positions for long periods of time.12–14 The complex fine-motor activities in the patient’s mouth require the focussed attention of the dentist, and therefore ergonomic posture is often neglected in favor of better vision. Holding a static awkward posture for long periods can lead to chronic muscular fatigue, discomfort, and pain. Even worse, frequent static loading on muscles and joints may result in adaptive alterations in the normal structures of the soft tissues, such as muscle shortening and other pathological effects.15,16
The potential consequences of MSD can be persistent for the affected person and have a high probability of developing into a chronic condition. This is particularly the case for hand complaints which have a higher risk of chronicity.17 As recent literature shows high prevalence of MSD in the upper extremity area18 the present study especially investigated these body region.
MSD and pain can lead not only to reduced productivity and a poorer quality of work, but also to decreased job satisfaction and sick leave,19–21 thereby resulting in high costs for medical treatments that may also have major financial consequences due to workers’ compensation. In Germany medical costs for musculoskeletal diseases amounted to €34.2 billion in 2015, representing 10.1% of all medical payments.22 Investigations of occupational diseases among professional dentists have been carried out in the United States, as well as some European countries, but there is still little data from Germany.2,3
The aim of the present study was therefore to examine the prevalence of and risk factors for musculoskeletal disorders in the upper extremity among German professional dentists, in order to gain a better understanding of the etiology of the symptoms and to identify or develop preventive measures.
Methods
Questionnaires were sent to 600 professional dentists in and around the city of Münster (with five-digit postal codes starting with 48) in November 2019. 38% of the dentists responded (229 participants). The inclusion criterion was at least 1 year of work experience, which deliberately excluded young entrants to the profession. A questionnaire on professional activity, health data, demographic details, as well as the modified Nordic Musculoskeletal Questionnaire (NMQ) and short version of the Disability of the Arm, Shoulder and Hand (DASH) score were mailed to the participants. The study was approved by the institutional review board of the University of Münster (reg. no. 2019–609-f-S) and conducted in accordance with the Declaration of Helsinki. The participants gave informed consent by sending back the completed questionnaire.
Data queried on individual characteristics and work history included questions on age, weight and height, gender, family situation, duration of employment, general health, nicotine abuse, and sick leave, as well as use of analgesics for musculoskeletal symptoms. Questions on the physical workload assessed average working hours per day, repetitive movements, awkward working postures in which the back is bent or twisted, prolonged sitting or standing. Furthermore, the frequency of strenuous arm positions, such as working with the hands in excessive tightening or arm abduction, and elevated arms while using vibrating tools or magnifying glasses were surveyed. For this purpose, a four-point scale was used, with the ratings “seldom or never,” “sometimes,” “often,” and “always” during a regular workday. The answers “often” and “always” were classified as representing high exposure.
The musculoskeletal symptoms were assessed using a modified Nordic Musculoskeletal Questionnaire.23 Four end points for each body region (back, neck, shoulder, elbow, and hand/wrist) were defined:
Musculoskeletal pain during the previous 12 months.
Musculoskeletal pain during the previous 12 months, restricting everyday as well as professional activities.
Musculoskeletal pain that led to medical care being sought during the previous 12 months.
Acute musculoskeletal pain during the previous 7 days.
In addition, to complete the data collection, the short version of the DASH questionnaire was used.
Statistical Analysis
Data were analyzed using SPSS (v26, SPSS Inc, Chicago, IL, USA). The participants’ characteristics (general health and socio-demographic data) were reported using descriptive statistics (mean and standard deviation or median and interquartile range).
One-tailed Spearman rank correlations were used to investigate the relation between the four below mentioned indices. Binary logistic regression analysis was used to estimate the impact of age, gender, comorbidity, physical load and workload on the outcome variable (ie musculoskeletal pain in the previous 12 month). Odds ratios with 95% confidence intervals (95% CI) derived from the model results were calculated as a measure of association. Gender and age were included because of a priori knowledge regarding their effect on musculoskeletal pain. Models were calculated based on these variables for each of the investigated body regions (neck, shoulder, upper back, lower back, elbow, hand/wrist). In a second calculation, the variables age and gender were always included as confounding factors and only the variables with significant regression coefficients (P ≤ 0.05) were kept in the corresponding models. Goodness of fit and the effect size of the models were reported using Nagelkerke’s R224 and Cohen’s f.25 A Cohen’s f of 0.1 was classified as a weak effect, a value of 0.25 as a medium effect, and a value of 0.40 as a strong effect accordingly.
The individual health situation of the participants was assessed by two scales: First, by means of the comorbidity index, which covers a range of health conditions (cardiovascular disease (+1 point), diabetes (+1 point), gastrointestinal disease (+1 point), psychological disease (+1 point), headache (+1 point), herniated intervertebral disk (+1 point), neurological disease (+1 point), nicotine abuse (+1 point) and body mass index > 25 (+1 point)) and is represented as a score from 0 (good health condition) to 9 (poor health condition). Second, by the pain index mapping musculoskeletal discomfort on a scale of 0 (good health condition) to 4 points (poor health condition) by examining the period of the last 12 months (musculoskeletal pain (+ 1 point), musculoskeletal pain preventing everyday as well as professional activities (+ 1 point), musculoskeletal pain that led to medical care being sought during the (+ 1 point)) and the period of the previous seven days (acute musculoskeletal pain (+ 1 point)).
In analogy, the individual workplace-related burden was also recorded by two indices. The physical load index was used to quantify the strain at the workplace with a sore ranging from 0 points (no musculoskeletal strain) to 28 points (heavy musculoskeletal strain) by inquiring about certain conditions ((awkward working posture (+1 point), prolonged sitting or standing (+1 point), strenuous arm positions (+1 point), hands in excessive tightening (+1 point), precise movements (+1 point), repetitive movements (+1 point), use of vibrating tools (+1 point)) × (1–4 points corresponding to the four-level rating scale from seldom to never)). The workload index, on the other hand, quantified individual occupational stress on a scale of 8 (short-term stress) to 120 (long-term stress) points by assessing the number of years on the job (1–30 and above years), multiplied with the average daily working hours (4–8 and above hours), and the average level of stress, corresponding to the four-level rating scale from seldom to never (1–4).
Results
Demographic Characteristics
The response rate was 38% (229 questionnaires). Participants comprised general dentists (73.8%) and also specialists, mainly orthodontists (9.6%), oral or maxillofacial surgeons (8.3%), endodontists, periodontists, and specialists in pediatric dentistry. The participating dentists were mainly self-employed (71.2%). Their average BMI was 24.2 (18.0–32.4).
Table 1 lists the participants’ demographic characteristics. Their average age was 50.4 ± 12.5 years; 87.3% of them were living with partners, 8.7% were single, and 3.9% did not provide information about their personal status. The dentists had been working for a mean of 19.9 ± 11.6 years. Their mean daily working hours were 8.1 ± 1.7.
 |
Table 1 Demographic Characteristics of All Participants (N=229) |
Prevalence of Musculoskeletal Disorders
Overall, 92.6% of the dentists were suffering from musculoskeletal symptoms in at least one of the body regions investigated. The results of the NMQ–based items showed a higher prevalence of pain symptoms in the neck and shoulder regions in comparison to the distal regions of the elbow and wrist/hand. Neck pain was the most prevalent symptom, reported by 65.1% of the participants, followed by 58.1% with symptoms in the shoulder and 49.3% with symptoms in the upper back (Figure 1).
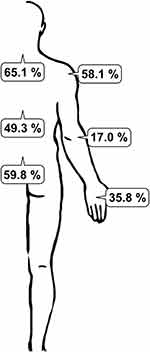 |
Figure 1 Prevalence rates of MSDs in affected body regions. |
Limitations in daily activities were due to neck pain in 15.9% of cases and shoulder pain in 15.4%; 23.7% of the dentists had sought medical care due to neck pain and 21.1% due to shoulder pain (Table 2). Acute problems during the previous 7 days had been experienced in the neck by 37.2%, in the shoulders by 29.1%, and in the upper back by 22.5%. Only 7.4% had been on sick leave; 36.2% were taking analgesics due to musculoskeletal pain.
 |
Table 2 Musulosceletal Complaints in the Last Twelve Months in Terms of Body Regions for All Participants |
The percentage of MSD increased with age: Dental professionals under 50 years showed lower percentages when compared to older dental professionals, with a peak between 51–65 years (98.7%). The prevalence of MSD according to occupation is reported in Figure 2. Orthodontics showed higher prevalences of MSDs in different body regions when compared to general dentists. Highest prevalence is documented with disorders of neck (81.8%) and shoulder (77.3%) in Orthodontics. Significantly lower rates are seen in prevalence of MSD in general dentists in the same body regions (neck 63.1%, shoulder 56.6%, p<0.05).
 |
Figure 2 Prevalence rates of MSDs in different dental disciplines. |
Higher working hours per day and treatment hours per per day demonstrated a greater percentage of MSD. Furthermore, the years of work showed to increase the percentage of MSD, with the highest percentages after 11–20 years of work (94.4%). Likewise, 93.8% of the dentists working since 31–40 years showed MSD. Females showed significantly higher percentages in relation to working hours per day, treatment hours per day and stress level (p < 0.05) (Table 3).
 |
Table 3 Work Related Characteristics of All Participants and Comparison Between Female and Male |
Females showed a significantly higher percentage of MSD when compared to males in all the evaluated parameters (p <0.05). Highest prevalence is documented in MSD of neck (83.5%) and shoulder (72.5%) (Figure 3).
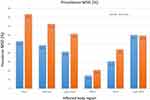 |
Figure 3 Prevalence rates of MSDs in female and male dentists. |
Correlations
Spearman correlation showed positive correlations between the pain index and the workload index (r = 0.131, P = 0.028), physical load index (r = 0.299, P < 0.001) and comorbidity index (r = 0.251, P < 0.001) (Figure 4).
 |
Figure 4 Correlation between different indices. |
Risk Factors for MSD
In relation to risk factors (P < 0.005), female sex was associated with disorders of the shoulder (P = 0.015; medium effect size) and hand (P = 0.000; large effect size). Female sex increased the likelihood of shoulder symptoms by +13.3% (+20.7% in relation to symptoms in the hands).
Increased physical load was also a risk factor for disorders in the upper back (P = 0.013; large effect size). The stepwise increase in physical load leads to an increase of 33.1% in the relative likelihood for upper back pain.
A large number of comorbidities was a risk factor for disorders of the hand (P = 0.000; large effect size) and lower back (P = 0.001; medium effect size). Increasing numbers of comorbidities led to stepwise increases of 19.5% in the probability of suffering from disorders of the hands and of 49.9% for disorders of the lower back (Table 4).
 |
Table 4 Risk Factors for MSD in Different Body Regions |
Exercise Activity
Eighty-five dentists (34 women, 51 men) stated that they were taking part in regular exercise or sporting activities; 37 reported no regular exercise (14 women, 24 men), and the rest did not provide any information regarding exercise activity. No differences were found in the pain index between those with or without exercise activity (P = 0.36).
Discussion
Prevalence of MSD and pain in our study is high with overall 92.6% of dentists suffering from musculoskeletal complaints in at least one body region. These findings are associated with higher workloads and existing comorbidities.
The reported prevalence rates for musculoskeletal complaints in the literature range from 10.8% to 97.9%.2 The highest prevalence rate (97.9%) was reported in a study of 575 dentists suffering from general musculoskeletal diseases within the previous 12 months.11 The lowest prevalence rate (10.8%) was documented in a Finnish investigation of 295 dentists who were suffering from osteoarthritis in the fingers.26 The prevalence rates in comparable studies with a moderate or high quality from Western countries are over 80%.27–30 Our results are in line with recent findings of Ohlendorf et al.31 They documented overall prevalence of MSD for the last 12 months from 92%. Most affected body regions included neck and shoulders (70.9% respectively 55.6%).
Similar results were found by Gandolfi et al among Italian dentists and dental hygienists.32 The most affected body areas in their study population were also neck (59.9%) and shoulders (43.3%) followed by lumbar region (52.1%), dorsal region (37.7%) and wrists (30.6%).
Neck pain was the most prevalent musculoskeletal symptom in the present study, reported by 65.1% of the participants — a level that is consistent with the literature results, which range from 34.3% to 84.8%.33,34 Vijay et al showed already among dental students neck pain occurs with a prevalence rate of 50%. Female respondents showed significant higher incidence of neck pain (58% vs 37%) as well as higher “average pain intensity” (mean 4.02 vs 3.43 VAS).35
Our findings also show that MSD and pain were common in the shoulders (with a prevalence of 58.1%). Several other studies have reported similar results among dental professionals.2,7,32 The findings correlate with the fact that dental professionals mainly use the upper body regions when working. Disorders in the shoulder region may be correlated to the repetitive motions, vibration and long duration of the procedures, prolonged shoulder abduction (>45◦) with elbow flexed and pronated with isometric and eccentric contraction, fatigue and strain deltoid, supraspinatus trapezius and serratus anterior.
We investigated the MSD distribution in female and male dentists meanwhile it is generally known that the sensitivity of pain differs between men and women. In our study most participants were men (N=136), working as practice owners in 79.5%. Participating women were more likely employees (42%) and younger than men (43.01 vs 50.4 years). In addition, female dentists stated to complete fewer working hours and treatment hours per day than men. In the present study, female sex increased the likelihood of the occurrence of symptoms in the shoulder and in the hands. The regions of highest MSD prevalence (neck, shoulder, upper back) were the same in both sexes. However, the actual prevalence was higher in women than in men, even though women work fewer hours per week than men. This is consistent with the results of other investigations in the literature. Ohlendorf et al also found that significantly more women than men suffered from pain in the areas of highest prevalence of MSD (neck: 84.7 respectively 67.5%; shoulder: 70.8% respectively 56.4%). Gandolfi et al documented significantly higher prevalence of MSD at the shoulders, wrists and ankles in female Italian dentists than in male.
Furthermore, Al-Mohrej et al reported that female dentists in Saudi-Arabia were approximately 1.5 times more likely to suffer from shoulder pain than male dentists.36 Another study among Thai dentists documented worse shoulder pain in women.37 One possible explanation for this might be that greater muscle forces are generated in women as a result of differing technique.
It is known that there are sex-related biological, kinematic, and electromyographic differences during lifting tasks, but detailed data are not available regarding differences in musculoskeletal loads.38 For example, Martinez et al have shown that women generate greater muscle forces and activations than men, regardless of the mass involved in lifting tasks. The study found that greater musculoskeletal loads were generated among women in comparison with men during a lifting task, which the authors describe as possibly resulting from “poor technique and strength difference”.39 Another finding was that women generate greater muscle forces and activations when working above shoulder level. This evidence needs to be taken into account when evaluating working techniques.
Lower back pain was more frequent in comparison with upper back pain (with prevalences of 59.8% and 49.3%, respectively). A typical twisting of the back during treatment of patients has been observed, caused by greater right tilting of the lumbar spine and left tilting of the thoracic spine.3 Other investigators have documented similar results and concluded that forced postures while sitting are significantly associated with lower back pain.40 High prevalence rates for lower back pain (> 57%) have also been reported among dental professionals in India and Saudi Arabia.19,41,42
The literature reports show comparatively lower prevalence rates for musculoskeletal disorders in the elbow and hand/wrist (17% and 35.8%, respectively), without documentation of handedness. Other studies have described a higher prevalence of musculoskeletal disorders on the right side than the left for the elbow and hand/wrist, in a group of predominantly right-handed respondents. The authors concluded that the finding is related to the operating position of the dominant hand during everyday work.43 In the present study, it was found that physical load, including awkward working postures, was an occupational risk factor. Pejčić et al reported that discomfort while working in a certain body position significantly increases the odds of musculoskeletal pain (odds ratio 10.82; 95% CI, 5.38 to 21.78).44 Other studies in Asia and South America have documented similar results among dental professionals.42,45,46
Awkward working postures result from specific dental tasks such as hand scaling and ultrasound scaling.47 Dental professionals are thus particularly vulnerable to musculoskeletal diseases and pain due to forced postures. In the present study, the workload parameter — ((years of work) × (average hours worked per day) × (average level of stress)) — correlated with increasing musculoskeletal pain. These findings are consistent with the literature.
The work schedule also appears to be associated with the risk of musculoskeletal diseases and pain. One study reported that having no breaks between interventions significantly increased the odds of musculoskeletal pain by 6.51 times (95% CI, 2.58 to 16.41).44 In another study. Martínez et al confirmed this finding among South American dental professionals.45 Insufficient breaks during dental activities that are very demanding on the musculoskeletal system lead to overstraining of the system. Musculoskeletal diseases and pain can occur as a consequence.
However, the findings on the effect of the number of years worked on the incidence and prevalence of musculoskeletal disorders are inconsistent. Some studies have reported that musculoskeletal disorders increase in relation to years of work,48 while other studies have documented a negative correlation between musculoskeletal pain and years worked among dentists.27,49 Some researchers have stated that dentists who have substantial experience learn to adapt their working posture and avoid musculoskeletal disorders, or that dentists who have musculoskeletal disorders may quit dentistry as a profession.50 The data of the present study suggest that recreational exercise activity does not appear to have any effect on preventing musculoskeletal disorders. In contrast, Koneru et al found that yoga was more effective than other modes of physical activity, such as aerobics or brisk walking.51 Several other interventional studies have reported, for example, that regular physical activity before and after work, back exercises, dynamic sitting, and the use of magnifying loupes can significantly contribute to reducing musculoskeletal diseases and pain among dentists.6,51–54 Further research is therefore needed to investigate specific exercise programs aimed at minimizing or preventing musculoskeletal disorders among dental professionals.
Ohlendorf et al55 introduced a novel study protocol for an ergonomic risk assessment of the cooperative treatment of dentists and dental assistants based on objective movement data by comparing four different treatment settings. By using a German wide online survey and biomechanical analysis this study will investigate MSD in the dental professional field. It may be expected that this study will provide new insights about ergonomic working methods and their possibility of prevention.
Limitations and Strengths
This study has several methodological strengths and limitations. Firstly, it used the Nordic Musculoskeletal Questionnaire, a well-validated and commonly used measurement tool that appears to be suitable for examining the prevalence of musculoskeletal diseases and pain.23 The clinical posture analysis and interviews were conducted using standardized checklists. The results were consequently accurate and comparable with the literature findings.
In view of the small sample size, it is difficult to generalize these findings for German dentists, and further studies in Germany are therefore needed. A differentiated investigation of the impact of exercise activity is lacking in the study. Future research is therefore needed to investigate the impact of specific exercise programs aimed at minimizing or preventing musculoskeletal disorders among dental professionals.
Conclusions
This study investigates for the prevalence rates for musculoskeletal disorders of the upper extremity among professional dentists in Germany. Pain, physical load, comorbidities, and female sex have been identified as possible risk factors for musculoskeletal diseases and pain. Suitable interventions for preventing musculoskeletal diseases and pain among dental professionals are therefore needed. Good ergonomic design of the dental workplace is essential in order to reduce awkward working postures during clinical practice. In addition to training courses on ergonomics, workplace organization, and occupational health, with special attention being given to female dentists, specific training programs for muscle strengthening of the neck and shoulder/arm should be developed.
Acknowledgments
Research for this study was supported by the Medical Faculty of the University of Münster (through a grant to C.R.).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest for this work.
References
1. Ayers KM, Thomson WM, Newton JT, Morgaine KC, Rich AM. Self-reported occupational health of general dental practitioners. Occup Med (Lond). 2009;59(3):142–148. doi:10.1093/occmed/kqp004
2. Lietz J, Kozak A, Nienhaus A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: a systematic literature review and meta-analysis. PLoS One. 2018;13(12):e0208628. doi:10.1371/journal.pone.0208628
3. Ohlendorf D, Erbe C, Hauck I, et al. Kinematic analysis of work-related musculoskeletal loading of trunk among dentists in Germany. BMC Musculoskelet Disord. 2016;17(1):427. doi:10.1186/s12891-016-1288-0
4. Hayes MJ, Smith DR, Cockrell D. An international review of musculoskeletal disorders in the dental hygiene profession. Int Dent J. 2010;60(5):343–352.
5. De Sio S, Traversini V, Rinaldo F, et al. Ergonomic risk and preventive measures of musculoskeletal disorders in the dentistry environment: an umbrella review. PeerJ. 2018;6:e4154. doi:10.7717/peerj.4154
6. Hayes M, Cockrell D, Smith D. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg. 2009;7(3):159–165. doi:10.1111/j.1601-5037.2009.00395.x
7. Haas Y, Naser A, Haenel J, et al. Prevalence of self-reported musculoskeletal disorders of the hand and associated conducted therapy approaches among dentists and dental assistants in Germany. PLoS One. 2020;15(11):e0241564. doi:10.1371/journal.pone.0241564
8. Ohlendorf D, Naser A, Haas Y, et al. Prevalence of Musculoskeletal Disorders among Dentists and Dental Students in Germany. Int J Environ Res Public Health. 2020;17(23):8740. doi:10.3390/ijerph17238740
9. Moodley R, Naidoo S, Wyk JV. The prevalence of occupational health-related problems in dentistry: a review of the literature. J Occup Health. 2018;60(2):111–125. doi:10.1539/joh.17-0188-RA
10. Alexandre PC, da Silva IC, de Souza LM, de Magalhaes Camara V, Palacios M, Meyer A. Musculoskeletal disorders among Brazilian dentists. Arch Environ Occup Health. 2011;66(4):231–235. doi:10.1080/19338244.2011.564571
11. Hodacova L, Sustova Z, Cermakova E, Kapitan M, Smejkalova J. Self-reported risk factors related to the most frequent musculoskeletal complaints among Czech dentists. Ind Health. 2015;53(1):48–55. doi:10.2486/indhealth.2013-0141
12. Akesson I, Hansson GA, Balogh I, Moritz U, Skerfving S. Quantifying work load in neck, shoulders and wrists in female dentists. Int Arch Occup Environ Health. 1997;69(6):461–474. doi:10.1007/s004200050175
13. Burdorf A, Sorock G. Positive and negative evidence of risk factors for back disorders. Scand J Work Environ Health. 1997;23(4):243–256. doi:10.5271/sjweh.217
14. Villanueva A, Dong H, Rempel D. A biomechanical analysis of applied pinch force during periodontal scaling. J Biomech. 2007;40(9):1910–1915. doi:10.1016/j.jbiomech.2006.09.001
15. McNee C, Kieser JK, Antoun JS, Bennani H, Gallo LM, Farella M. Neck and shoulder muscle activity of orthodontists in natural environments. J Electromyogr Kinesiol. 2013;23(3):600–607. doi:10.1016/j.jelekin.2013.01.011
16. Valachi B, Valachi K. Mechanisms leading to musculoskeletal disorders in dentistry. J Am Dent Assoc. 2003;134(10):1344–1350. doi:10.14219/jada.archive.2003.0048
17. Alexopoulos EC, Stathi I-C, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet Disord. 2004;5(1):16. doi:10.1186/1471-2474-5-16
18. Mulimani P, Hoe VC, Hayes MJ, Idiculla JJ, Abas AB, Karanth L. Ergonomic interventions for preventing musculoskeletal disorders in dental care practitioners. Cochrane Database Syst Rev. 2018;10:CD011261.
19. Aljanakh M, Shaikh S, Siddiqui AA, Al-Mansour M, Hassan SS. Prevalence of musculoskeletal disorders among dentists in the Hail Region of Saudi Arabia. Ann Saudi Med. 2015;35(6):456–461. doi:10.5144/0256-4947.2015.456
20. Aminian O, Alemohammad ZB, Hosseini MH. Neck and upper extremity symptoms among male dentists and pharmacists. Work. 2015;51(4):863–868. doi:10.3233/WOR-141969
21. Aminian O, Banafsheh Alemohammad Z, Sadeghniiat-Haghighi K. Musculoskeletal disorders in female dentists and pharmacists: a cross-sectional study. Acta Med Iran. 2012;50(9):635–640.
22. Stahl T. Krankheitsbedingte Kosten in der Bevölkerung im erwerbsfähigen Alter. Fehlzeiten-Report 2018. [Illness-related costs in the working-age population. Fehlzeiten-Report 2018]. Springer; 2018:559–567. German.
23. Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18(3):233–237. doi:10.1016/0003-6870(87)90010-X
24. Nagelkerke NJD. A note on a general definition of the coefficient of determination. Biometrika. 1991;78:691–692. doi:10.1093/biomet/78.3.691
25. Cohen J. Quantitative methods in psychology: a power primer. Psychol Bull. 1992;112(1):155–159. doi:10.1037/0033-2909.112.1.155
26. Ding H, Solovieva S, Vehmas T, Riihimäki H, Leino-Arjas P. Finger joint pain in relation to radiographic osteoarthritis and joint location–a study of middle-aged female dentists and teachers. Rheumatology (Oxford). 2007;46(9):1502–1505. doi:10.1093/rheumatology/kem185
27. Leggat PA, Smith DR. Musculoskeletal disorders self-reported by dentists in Queensland, Australia. Aust Dent J. 2006;51(4):324–327. doi:10.1111/j.1834-7819.2006.tb00451.x
28. Lindfors P, von Thiele U, Lundberg U. Work characteristics and upper extremity disorders in female dental health workers. J Occup Health. 2006;48(3):192–197. doi:10.1539/joh.48.192
29. Sustová Z, Hodacová L, Kapitán M. The prevalence of musculoskeletal disorders among dentists in the Czech Republic. Acta Medica (Hradec Kralove). 2013;56(4):150–156. doi:10.14712/18059694.2014.10
30. Warren N. Causes of musculoskeletal disorders in dental hygienists and dental hygiene students: a study of combined biomechanical and psychosocial risk factors. Work. 2010;35(4):441–454. doi:10.3233/WOR-2010-0981
31. Ohlendorf D, Haas Y, Naser A, et al. Prevalence of Muscular Skeletal Disorders among Qualified Dental Assistants. Int J Environ Res Public Health. 2020;17(10):3490.
32. Gandolfi MG, Zamparini F, Spinelli A, Risi A, Prati C. Musculoskeletal Disorders among Italian Dentists and Dental Hygienists. Int J Environ Res Public Health. 2021;18(5):2705. doi:10.3390/ijerph18052705
33. Droeze EH, Jonsson H. Evaluation of ergonomic interventions to reduce musculoskeletal disorders of dentists in the Netherlands. Work. 2005;25(3):211–220.
34. Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders and symptom severity among Australian dental hygienists. BMC Res Notes. 2013;6:250. doi:10.1186/1756-0500-6-250
35. Vijay S, Ide M. Musculoskeletal neck and back pain in undergraduate dental students at a UK dental school - a cross-sectional study. Br Dent J. 2016;221(5):241–245. doi:10.1038/sj.bdj.2016.642
36. Al-Mohrej OA, AlShaalan NS, Al-Bani WM, Masuadi EM, Almodaimegh HS. Prevalence of musculoskeletal pain of the neck, upper extremities and lower back among dental practitioners working in Riyadh, Saudi Arabia: a cross-sectional study. BMJ Open. 2016;6(6):e011100. doi:10.1136/bmjopen-2016-011100
37. Chowanadisai S, Kukiattrakoon B, Yapong B, Kedjarune U, Leggat PA. Occupational health problems of dentists in southern Thailand. Int Dent J. 2000;50(1):36–40. doi:10.1111/j.1875-595X.2000.tb00544.x
38. Bouffard J, Martinez R, Plamondon A, Côté JN, Begon M. Sex differences in glenohumeral muscle activation and coactivation during a box lifting task. Ergonomics. 2019;62(10):1327–1338. doi:10.1080/00140139.2019.1640396
39. Martinez R, Assila N, Goubault E, Begon M. Sex differences in upper limb musculoskeletal biomechanics during a lifting task. Appl Ergon. 2020;86:103106. doi:10.1016/j.apergo.2020.103106
40. Howarth SJ, Grondin DE, La Delfa NJ, Cox J, Potvin JR. Working position influences the biomechanical demands on the lower back during dental hygiene. Ergonomics. 2016;59(4):545–555. doi:10.1080/00140139.2015.1077274
41. Batham C, Yasobant S. A risk assessment study on work-related musculoskeletal disorders among dentists in Bhopal, India. Indian J Dent Res. 2016;27(3):236–241. doi:10.4103/0970-9290.186243
42. Kumar VK, Kumar SP, Baliga MR. Prevalence of work-related musculoskeletal complaints among dentists in India: a national cross-sectional survey. Indian J Dent Res. 2013;24(4):428–438. doi:10.4103/0970-9290.118387
43. Feng B, Liang Q, Wang Y, Andersen LL, Szeto G. Prevalence of work-related musculoskeletal symptoms of the neck and upper extremity among dentists in China. BMJ Open. 2014;4(12):e006451. doi:10.1136/bmjopen-2014-006451
44. Pejčić N, Petrović V, Marković D, et al. Assessment of risk factors and preventive measures and their relations to work-related musculoskeletal pain among dentists. Work. 2017;57(4):573–593. doi:10.3233/WOR-172588
45. Fals Martínez J, González Martínez F, Orozco Páez J, Correal Castillo SP, Pernett Gómez CV. Musculoskeletal alterations associated factors physical and environmental in dental students. Rev Bras Epidemiol. 2012;15(4):884–895. doi:10.1590/S1415-790X2012000400018
46. Samat RA, Shafei MN, Yaacob NA, Yusoff A. Prevalence and associated factors of back pain among dental personnel in North-Eastern State of Malaysia. Int J Collabor Res Intern Med Public Health. 2011;3(7):576–586.
47. Hayes MJ, Taylor JA, Smith DR. Predictors of work-related musculoskeletal disorders among dental hygienists. Int J Dent Hyg. 2012;10(4):265–269. doi:10.1111/j.1601-5037.2011.00536.x
48. Ratzon NZ, Yaros T, Mizlik A, Kanner T. Musculoskeletal symptoms among dentists in relation to work posture. Work. 2000;15(3):153–158.
49. Finsen L, Christensen H, Bakke M. Musculoskeletal disorders among dentists and variation in dental work. Appl Ergon. 1998;29(2):119–125. doi:10.1016/S0003-6870(97)00017-3
50. Leggat PA, Kedjarune U, Smith DR. Occupational health problems in modern dentistry: a review. Ind Health. 2007;45(5):611–621. doi:10.2486/indhealth.45.611
51. Koneru S, Tanikonda R. Role of yoga and physical activity in work-related musculoskeletal disorders among dentists. J Int Soc Prev Commun Dent. 2015;5(3):199–204. doi:10.4103/2231-0762.159957
52. Hayes MJ, Osmotherly PG, Taylor JA, Smith DR, Ho A. The effect of loupes on neck pain and disability among dental hygienists. Work. 2016;53(4):755–762. doi:10.3233/WOR-162253
53. Hayes MJ, Osmotherly PG, Taylor JA, Smith DR, Ho A. The effect of wearing loupes on upper extremity musculoskeletal disorders among dental hygienists. Int J Dent Hyg. 2014;12(3):174–179. doi:10.1111/idh.12048
54. Maillet JP, Millar AM, Burke JM, Maillet MA, Maillet WA, Neish NR. Effect of magnification loupes on dental hygiene student posture. J Dent Educ. 2008;72(1):33–44. doi:10.1002/j.0022-0337.2008.72.1.tb04450.x
55. Ohlendorf D, Maltry L, Hanel J, et al. SOPEZ: study for the optimization of ergonomics in the dental practice - musculoskeletal disorders in dentists and dental assistants: a study protocol. J Occup Med Toxicol. 2020;15:22. doi:10.1186/s12995-020-00273-0
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
