Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 12
Prevalence of metabolic syndrome in dialysis and transplant patients
Authors Alshelleh S, AlAwwa I , Oweis A , AlRyalat SA , Al-Essa M , Saeed I , Alhawari HH , Alzoubi KH
Received 4 January 2019
Accepted for publication 11 March 2019
Published 29 April 2019 Volume 2019:12 Pages 575—579
DOI https://doi.org/10.2147/DMSO.S200362
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Sameeha AlShelleh,1 Izzat AlAwwa,1 Ashraf Oweis,2 Saif Aldeen AlRyalat,1 Mohammad Al-Essa,1 Iyad Saeed,1 Hussein H Alhawari,1 Karem H Alzoubi3
1Department of Internal Medicine, The University of Jordan, Amman 11942, Jordan; 2Department of Internal Medicine, Jordan University of Science and Technology, Irbid, Jordan; 3Department of Clinical Pharmacy, Faculty of Pharmacy, Jordan University of Science and Technology, Irbid, Jordan
Background: Several epidemiological studies have assessed various components of Metabolic Syndrome (MS) in different populations, but only a few compared the prevalence of metabolic syndrome in dialysis and transplant patients.
Aim: The aim of this study is to compare the prevalence of MS in dialysis and transplant patients. Two groups of patients were included; hemodialysis patients and patients with transplanted kidneys.
Methods: Demographic and clinical history, and lab data were collected. A total of 108 patients were included in this study with a mean age of 52.3 (±16.29) years. Study groups included 61 (56.5%) dialysis patients, and 47 (43.5%) patients with transplanted kidneys.
Results: Upon comparing the prevalence of metabolic syndrome between the two study groups, transplant patients had significantly lower prevalence of metabolic syndrome (34%) compared to that of metabolic syndrome in patients on dialysis (55.7%; P=0.016).
Conclusion: As metabolic syndrome plays an important role in the pathology of elderly patients, especially those with transplanted kidneys, such findings indicate the need for close monitoring of kidney transplant patients for the manifestations of metabolic syndrome.
Keywords: metabolic syndrome, renal transplant, chronic kidney disease, elderly
Introduction
In the past few years, the concept of metabolic syndrome emerged to denote patients who have at least three of the following: hypertension, diabetes mellitus, central obesity, hypertriglyceridemia, and low high-density lipoprotein (HDL).1 The metabolic syndrome basic theory indicates that every component is an independent predictor of disease where multiple factors combinations lead to synergistic risk, which is greater than the sum of risk from each component. It is now well-known that patients with metabolic syndrome have higher risk of cardiovascular and kidney diseases.2,3 The Third National Health and Nutrition Examination Survey showed that metabolic syndrome is a risk factor for developing chronic kidney disease.4
The manifestations of metabolic syndrome extend beyond being a risk factor for chronic kidney disease, as shown in studies on patients on dialysis and transplants. In renal transplant patients, a complex interaction between metabolic syndrome and renal transplant factors was observed, as metabolic syndrome can deteriorate renal function and increase rejection rates. Moreover, transplant-related medications could further exacerbate metabolic syndrome components.5 A complex relation with metabolic syndrome can also be observed in dialysis patients. For example, uremia that develops in the late stages in dialysis patients can lead to metabolic derangements, such as high blood pressure and glucose intolerance.6 Considering this complex role of metabolic syndrome in non-CKD, dialysis, and renal transplant patients, it is important to understand the prevalence of metabolic syndrome in each group, and to further explore which component plays the major role in metabolic syndrome development in each group. In this study, we aimed at studying the prevalence of metabolic syndrome in general, and each of its components in chronic kidney disease patients on hemodialysis versus those with renal transplant.
Methods
Participants
This cross-sectional study was approved by the institutional review board of Jordan University Hospital, Amman, and was conducted in concordance with the latest declaration of Helsinki. Written informed consent was obtained from all study participants. Hemodialysis patients and patients with transplanted kidneys were included. A survey was conducted via a one-on-one interview with recruits who were chosen during the period from January 2016 to April 2016. The interview included questions about demographic data, previous medical history in general, previous medical history related to the kidneys specifically (eg, kidney injury), medication history, and consent to participate in the study. Recruits were from the nephrology clinic, including; transplant clinic patients (transplant patients) and in-center chronic hemodialysis patients (dialysis patients) at Jordan University Hospital.
Patients on hemodialysis with the following criteria were included in the study: had dialysis three-times per week for the past year, never had kidney transplant, and not pregnant (for women). Transplant patients were included in the current study if they had at least one transplanted kidney, were not currently on dialysis,and not pregnant (for women). Notably, most transplant patients included in the current study were on dialysis before transplant (95.7% previously on dialysis versus 4.3% who had a preemptive renal transplant).
Measurements
At the end of the interview, which was done before dialysis session on the day of dialysis, the following were recorded for each patient: weight in kilograms by digital scale, height in meters, waist circumference in centimeters, and blood pressure. The blood pressure was measured using a Microlife validated blood pressure device for clinic use,7 with a suitable size cuff. This was done in a separate quiet room, with a confirmed sitting and relaxed state for at least 10 minutes, and confirmation of no stimulant use in the past hour. An average of three readings was considered for all previous measurements. Additionally, all patients were instructed to fast for 12 hours to do the following labs: kidney function test, fasting blood sugar, fasting lipid profile, and HbA1C.
Data reporting and statistical analysis
The absolute value for all the previously mentioned measurements was reported. Moreover, values of blood pressure, fasting blood glucose, waist circumference, triglyceride, and HDL were transformed into dichotomous (yes/no or 1/0) variables based on the definition of metabolic syndrome, and according to the harmonized definition of metabolic syndrome.1 Based on that, a new variable that represents the sum of all metabolic syndrome components, and another dichotomous variable that defines metabolic syndrome as having three or more components of the metabolic syndrome were produced.
SPSS 21.0 (IBM corporation, Armonk, NY,USA)was used for data analysis. Data were expressed as mean (±standard deviation) for continuous variables, and count (frequency) for descriptive variables. Independent sample t-test was used to compare gender mean age difference. The Chi-square test followed by Z-test of proportion were used to compare groups as per the presence of metabolic syndrome.
Ethics statement
Informed consent was obtained from all individual participants included in the study.
Results
Patients (n=108) were included in this study with a mean age of 52.3 (±16.29) years, consisting of 71 (65.7%) men with a mean age of 54.03 (±16.18) years, and 37 (34.3%) women with a mean age of 48.9 (±16.19) years (P>0.05). Dialysis patients (61; 56.5%) and patients with transplanted kidneys (47; 43.5%) were not different with regard to age or gender. Among the studied kidney transplant patients, the mean±SD time since transplant was 17.6±7.4 years. Table 1 details the characteristics of the study sample.
 | Table 1 General patients’ characteristics |
Upon comparing the prevalence of metabolic syndrome between both study groups, transplant patients had significantly lower prevalence of metabolic syndrome (34%), compared to that of metabolic syndrome in patients on dialysis (55.7%; P=0.016). The prevalence of each component of metabolic syndrome between both study groups was compared (Table 2). For hypertension, the prevalence of being hypertensive was significantly higher in patients on dialysis compared to transplant patients (P=0.001). For waist circumference (P<0.001), the prevalence of having increased waist circumference consistent with metabolic syndrome definition was significantly higher in transplant patients. For HDL (P=0.003), the prevalence of having low HDL was significantly higher in dialysis patients compared to transplant patients. For fasting blood sugar and triglyceride, there were no significant differences between study groups (P=0.732, P=0.352, respectively).
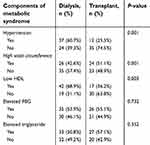 | Table 2 Comparisons of metabolic syndrome components between kidney transplant versus kidney dialysis patients |
Discussion
Findings of this study showed a higher prevalence of metabolic syndrome in dialysis patients compared to patients with transplanted kidneys. Only three out of five components of the metabolic syndrome were statistically significant between dialysis patients and patients with transplanted kidneys; they were hypertension, waist circumference, and HDL levels.
Previous studies showed that patients suffer more frequently from metabolic syndrome after renal transplantation.8 This increase in metabolic syndrome after kidney transplantation was proposed to be related to medication-induced effects on metabolic syndrome components, particularly dyslipidemia, glucose intolerance, and hypertension.5 In the current study, it was found that only a third of transplant patients had metabolic syndrome, compared to more than half of dialysis patients. In accordance with the current study, which showed a prevalence of 55.7% for metabolic syndrome in dialysis patients, a study on a US population showed a prevalence of 69.3% for metabolic syndrome among dialysis patients.9 Another study from Greece showed a prevalence of 56.3% of metabolic syndrome among dialysis patients.10 Among normal elderly patients, previous studies estimated that the prevalence of metabolic syndrome worldwide ranged from <10% to as much as 84% (57.3% in the present study), depending on individual factors including sex, age, race, and ethnicity; region, and environment of the population studied.11 In that respect, in two studies from France and Spain, patients had almost similar prevalence (32% and 37.7%) of metabolic syndrome after transplant.8,12
A recent meta-analysis showed that different components in the metabolic syndrome negatively affect the kidney in different proportions in terms of proteinuria, and it showed their effect in descending order to be hypertension, hypertriglyceridemia, low HDL, abdominal obesity, and impaired glucose intolerance.13 In the current study and upon comparing each component of the metabolic syndrome, a varying contribution of each component was observed where transplant patients had significantly low prevalence of hypertension (only 25.5%), low prevalence of low HDL (only 36.2%), but high prevalence of high waist circumference (51.1%). In a US study, an increase in the prevalence of all metabolic syndrome components after 1 year of transplantation was reported compared to pre-transplant status.8,14 For dialysis patients, current results showed high prevalence of hypertension (60.7%), high prevalence of low HDL (68.9%), but low prevalence of high waist circumference (only 42.6%). Young et al14 found high prevalence of hypertension (99%) and low HDL (66%) in dialysis patients, but, unlike the current study, higher prevalence of elevated fasting blood sugar (59%) was reported in that study along with a comparable prevalence of abdominal obesity (42%) . These discrepancies in the results of different studies could be attributed to the different population and healthcare settings between these studies and the current study.
The current study has some limitations, as it did not assess the metabolic syndrome status before renal transplantation or dialysis initiation (ie, longitudinal study design). Based on current findings, this is in fact a highly encouraged future study to assess the metabolic syndrome status before and after renal transplantation and dialysis initiation, which would further characterize the risk of metabolic syndrome induced by these two events. Moreover, future studies should consider including larger samples to confirm and further generalize current results.
Metabolic syndrome plays a major role in the progression of CKD in transplant patients with increased risk of proteinuria and eventually loss of graft function. The presence of metabolic syndrome could increase the risk for cardiovascular disease in both transplant and dialysis patients, which contributes to increased morbidity and mortality. The two most common factors found in the dialysis group (hypertension and low HDL) are well reported complications of chronic kidney disease where there is an interplay of both CKD factors and metabolic factors that affect whether these patients meet criteria for metabolic syndrome.
In conclusion, and as far as the prevalence of metabolic syndrome is concerned, patients with transplanted kidneys have lower metabolic syndrome prevalence compared to dialysis patients. Targeting hypertension and low HDL components in dialysis patients, and increased waist circumference in transplant patients could decrease the prevalence of metabolic syndrome and may further decrease morbidity and mortality.
Acknowledgments
This study was funded by Deanship of Scientific Research, University of Jordan. We would like to thank the Department of English Literature, University of Jordan for editing the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi:10.1161/CIRCULATIONAHA.109.192644
2. Stefansson VTN, Schei J, Solbu MD, Jenssen TG, Melsom T, Eriksen BO. Metabolic syndrome but not obesity measures are risk factors for accelerated age-related glomerular filtration rate decline in the general population. Kidney Int. 2018;93(5):1183–1190. doi:10.1016/j.kint.2017.11.012
3. Wahba IM, Mak RH. Obesity and obesity-initiated metabolic syndrome: mechanistic links to chronic kidney disease. Clin J Am Soc Nephrol. 2007;2(3):550–562. doi:10.2215/CJN.04071206
4. Chen J, Muntner P, Hamm LL, et al. The metabolic syndrome and chronic kidney disease in U.S. adults. Ann Intern Med. 2004;140(3):167–174.
5. Sgambat K, Clauss S, Moudgil A. Cardiovascular effects of metabolic syndrome after transplantation: convergence of obesity and transplant-related factors. Clin Kidney J. 2018;11(1):136–146. doi:10.1093/ckj/sfx056
6. Park SH, Lindholm B. Definition of metabolic syndrome in peritoneal dialysis. Perit Dial Int. 2009;29 Suppl 2:S137–S144.
7. Saladini F, Benetti E, Masiero S, Palatini P. Accuracy of Microlife WatchBP Office ABI monitor assessed according to the 2002 European Society of Hypertension protocol and the British Hypertension Society protocol. Blood Press Monit. 2011;16(5):258–261. doi:10.1097/MBP.0b013e32834af72e
8. Courivaud C, Kazory A, Simula-Faivre D, Chalopin JM, Ducloux D. Metabolic syndrome and atherosclerotic events in renal transplant recipients. Transplantation. 2007;83(12):1577–1581. doi:10.1097/01.tp.0000266898.93894.3d
9. Young DO, Lund RJ, Haynatzki G, Dunlay RW. Prevalence of the metabolic syndrome in an incident dialysis population. Hemodial int. 2007;11(1):86–95. doi:10.1111/j.1542-4758.2007.00158.x
10. Tsangalis G, Papaconstantinou S, Kosmadakis G, Valis D, Zerefos N. Prevalence of the metabolic syndrome in hemodialysis. Int J Artif Organs. 2007;30(2):118–123.
11. Kaur J. A comprehensive review on metabolic syndrome. Cardiol Res Pract. 2014;2014:943162. doi:10.1155/2014/943162
12. Porrini E, Delgado P, Bigo C, et al. Impact of metabolic syndrome on graft function and survival after cadaveric renal transplantation. Am J Kidney Dis. 2006;48(1):134–142. doi:10.1053/j.ajkd.2006.04.078
13. Thomas G, Sehgal AR, Kashyap SR, Srinivas TR, Kirwan JP, Navaneethan SD. Metabolic syndrome and kidney disease: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2011;6(10):2364–2373. doi:10.2215/CJN.02180311
14. Hricik DE. Metabolic syndrome in kidney transplantation: management of risk factors. Clin J Am Soc Nephrol. 2011;6(7):1781–1785. doi:10.2215/CJN.01200211
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
