Back to Journals » Clinical Audit » Volume 10
Prevalence of metabolic syndrome in a population served by assertive community treatment teams: a retrospective chart review
Authors Fairbairn J , Munshi T, Naeem F, Baldock J, Feakins M
Received 9 November 2017
Accepted for publication 4 July 2018
Published 1 November 2018 Volume 2018:10 Pages 15—19
DOI https://doi.org/10.2147/CA.S156596
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ming-Hui Zou
Jonathan Fairbairn,1 Tariq Munshi,1 Farooq Naeem,2 Jane Baldock,1 Martin Feakins1
1Department of Psychiatry, Queen’s University, Kingston, ON, Canada; 2Department of Psychiatry, University of Toronto, Toronto, ON, Canada
Background: Metabolic syndrome (MetS) is defined as the co-occurrence of risk factors for both type 2 diabetes and cardiovascular disease. This includes abdominal obesity, hyperglycemia, dyslipidemia, and hypertension. MetS is associated with significant morbidity and mortality from cardiovascular events and from all-cause mortality. MetS occurs at a higher rate in patients with serious mental illness compared to the general population.
Methods: A retrospective chart review was performed to determine the MetS prevalence and antipsychotic prescribing patterns for patients followed by 2 assertive community treatment teams (ACTTs; n=59). MetS criteria including blood pressure, body mass index, waist circumference, fasting cholesterol, and fasting blood sugar levels were extracted. Additional information including patient demographics, psychiatric diagnosis, and prescription medications were also collected and analyzed.
Results: The prevalence of the MetS among ACTT patients was 52.5%. The use of the metabolically favorable antipsychotic aripiprazole (n=10) remains limited in this population. There were no patients in this sample who were prescribed ziprasidone, lurasidone, or asenapine, all of which are associated with limited metabolic side effects.
Conclusion: MetS is prevalent among patients with severe and persistent mental illness followed by ACTTs. Despite the high rate of MetS in this patient population, the use of antipsychotics with favorable metabolic profiles remains limited.
Keywords: metabolic syndrome, atypical antipsychotics, severe and persistent mental illness
Introduction
Metabolic syndrome (MetS) is associated with a 2–6-fold increase risk of developing coronary heart disease and a 3–5-fold increase of developing diabetes.1,2 MetS has been identified as a significant public health challenge, and prevalence rates are increasing worldwide. Patients with severe and persistent mental illness (SPMI) are at significantly increased risk for developing MetS compared to the general population.3 This is contributed to by genetic factors and psychosocial factors which include unhealthy dietary choices, limited physical activity, cigarette smoking, and poor access to medical care.
MetS contributes to the health disparity observed in patients with SPMI compared to the general population, including high rates of morbidity and a 10–25 years reduction in their life expectancy.4 These outcomes are in a large part due to the increased prevalence of chronic physical conditions including cardiovascular and respiratory issues, diabetes and hypertension.5
There is increasing evidence of the effect of second-generation antipsychotics increasing obesity, hyperglycemia, and dyslipidemia.6–8 It has been shown that all antipsychotics are associated with some weight gain, and that olanzapine and clozapine are associated with severe weight gain. The abnormalities in glucose and lipid metabolism may be mediated by both obesity-related and obesity-unrelated biochemical mechanisms.9 In our study, we aimed to further characterize the prevalence of MetS and antipsychotic prescribing patterns among assertive community treatment teams (ACTT) patients.
Methods
Ethics approval PSIY-407–13 was obtained from the Health Sciences Research Ethics Board at Queens University. Patients in this study provided verbal consent for physical health monitoring, including physical examination and bloodwork, as a part of routine clinical practice. Written consent was not required as the archival data collected was anonymized, and the potential for harm among participants was minimal. The research data were collected and analyzed in accordance with institutional policies to ensure patient confidentiality.
The retrospective chart review was performed for patients followed by 2 ACTTs, serving the community of Kingston, ON, Canada. As part of routine care patients are regularly monitored for blood pressure, body mass index, waist circumference, fasting cholesterol, and fasting blood sugar levels. Charts were reviewed for patient demographics, DSM-5 psychiatric diagnosis, MetS criteria, and prescription medications.
The International Diabetes Federation consensus criteria for MetS was used for this study.10 This criterion requires increased waist circumference, with ethnic and gender-specific cut-points (eg, for Europids waist circumference ≥94 cm for men and ≥80 cm for women). In addition, 2 or more of the following criteria need to be present:
- Triglycerides ≥150 mg/dL (1.7 mmol/L) or treatment for elevated triglycerides,
- High-density lipoprotein (HDL) cholesterol <40 mg/dL (1.03 mmol/L) in men or <50 mg/dL (1.29 mmol/L) in women, or treatment for low HDL,
- Systolic blood pressure ≥130, diastolic blood pressure ≥85, or treatment for hypertension,
- Fasting plasma glucose ≥100 mg/dL (5.6 mmol/L) or previously diagnosed type 2 diabetes.
Results
Data analysis was completed for patients followed by the 2 ACTTs (n=59). Patients who had incomplete data were excluded from this study. Patient demographics, including their primary diagnosis, rate of comorbid substance use, and cigarette smoking (defined as ≥1 pack/d) are provided in Table 1. Statistical analysis was completing using the Mann–Whitney U test or χ2 test, with an α level of 0.05. There were no statistically significant differences in patient characteristics between individuals with and without MetS.
  | Table 1 Patient characteristics served by ACTTs (n=59) Abbreviations: ACTTs, assertive community treatment teams; MetS, metabolic syndrome; SUD, substance-use disorder. |
The prevalence of patients meeting the International Diabetes Federation criteria for MetS was 52.5%. The prevalence of patients meeting or exceeding cut-offs for individual MetS criteria are shown in Figure 1. Prescribing patterns for psychotropic medications are included in Table 2. Patients with MetS were significantly less likely to be prescribed the long-acting injectable form of risperidone (P-value <0.01).
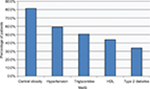  | Figure 1 MetS parameters in patients served by ACTTs. Abbreviations: ACTTs, assertive community treatment teams; HDL, high-density lipoprotein; MetS, metabolic syndrome. |
Discussion
The current study demonstrates an increased prevalence of MetS among patients with SPMI consistent with prevalence rates reported previously in the literature.3,11,12 Due to the high prevalence and significant morbidity associated with MetS, psychiatrists need to routinely screen patients for the development of MetS. Several national guidelines support incorporating regular monitoring of body mass index, lipid levels, fasting blood glucose levels, and blood pressure into routine psychiatric care.6,13,14 However despite this, the uptake of screening in clinical practice remains low.15 This can be problematic as patients with SPMI are less likely to access medical care from their primary care provider and their comorbidities are often underrecognized and suboptimally treated.16
Early detection of metabolic abnormalities allows for early intervention to treat these conditions. These interventions include lifestyle modification such as specific recommendations on diet and exercise with behavioral and cognitive strategies. These interventions can be delivered with individual sessions or in a group using a multidisciplinary model of care.17 If required, pharmacological therapy can offered to individual patient, aiming to normalize blood pressure, HDL cholesterol, triglycerides, and glucose values.
Psychiatrists need to be aware of the metabolic side effects of antipsychotic medications and weigh the risks and benefits accordingly when prescribing these medications. Weight gain occurs with most antipsychotic medications. Previous studies have shown that clozapine and olanzapine have been associated with the most significant metabolic side effects including weight gain, hyperglycemia, and hyperlipidemia. Risperidone, paliperidone, and quetiapine have been associated with moderate weight gain. The second-generation antipsychotics associated with a favorable metabolic profile include aripiprazole, ziprasidone, asenapine, and lurasidone.6,18
Conclusion
If a patient does not have significant clinical benefit that outweighs the health risks of metabolic side effects, a trial of an antipsychotic with lower propensity toward weight gain should be considered.13 In our study, we observed limited usage of metabolically favorable antipsychotics despite the high prevalence of MetS in the patient population. This suggests that despite the growing knowledge and awareness of the metabolic effects of antipsychotics medications, switching of these medications in clinical practice remains challenging. Future studies can examine interventions to change prescribing patterns to metabolically favorable antipsychotic medications, and models of care that promote routine monitoring of MetS. Further effective interventions are needed to help decrease the burden of MetS morbidity and mortality in patients with SPMI.
Disclosure
The authors report no conflicts of interest in this work.
References
Hanley AJ, Karter AJ, Williams K, et al. Prediction of type 2 diabetes mellitus with alternative definitions of the metabolic syndrome: the Insulin Resistance Atherosclerosis Study. Circulation. 2005;112(24):3713–3721. | ||
Sarti C, Gallagher J. The metabolic syndrome: prevalence, CHD risk, and treatment. J Diabetes Complications. 2006;20(2):121–132. | ||
Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, de Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders – a systematic review and meta-analysis. Schizophr Bull. 2013;39(2):1–13. | ||
Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13(2):153–160. | ||
De Hert M, van Winkel R, van Eyck D, et al. Prevalence of diabetes, metabolic syndrome and metabolic abnormalities in schizophrenia over the course of the illness: a cross-sectional study. Clin Pract Epidemiol Ment Health. 2006;2:14. | ||
Canadian Psychiatric Association. Clinical practice guidelines: treatment of schizophrenia. Can J Psychiatry. 2005;50(13 Suppl 1):7S–57S. | ||
Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123(2-3):225–233. | ||
Meyer JM, Davis VG, Goff DC, et al. Change in metabolic syndrome parameters with antipsychotic treatment in the CATIE Schizophrenia Trial: prospective data from phase 1. Schizophr Res. 2008;101(1–3):273–286. | ||
De Hert M, Detraux J, van Winkel R, Yu W, Correll CU. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. 2011;8(2):114–126. | ||
Alberti KG, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group. The metabolic syndrome: a new worldwide definition. Lancet. 2005;366(9491):1059–1062. | ||
Cohn T, Prud’homme D, Streiner D, Kameh H, Remington G. Characterizing coronary heart disease risk in chronic schizophrenia: high prevalence of the metabolic syndrome. Can J Psychiatry. 2004;49(11):753–760. | ||
Munshi T, Patel A, Mazhar MN, Hassan T, Siddiqui EU. Frequency of metabolic syndrome in psychiatric patients, is this the time to develop a standardized protocol to reduce the morbidity from an acute care psychiatry unit. J Pak Med Assoc. 2015;65(1):54–58. | ||
Lehman AF, Lieberman JA, Dixon LB, et al; American Psychiatric Association; Steering Committee on Practice Guidelines. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161(2 Suppl):1–56. | ||
Cooper SJ, Reynolds GP, Barnes T, et al. BAP guidelines on the management of weight gain, metabolic disturbances and cardiovascular risk associated with psychosis and antipsychotic drug treatment. J Psychopharmacol. 2016;30(8):717–748. | ||
Papanastasiou E. The prevalence and mechanisms of metabolic syndrome in schizophrenia: a review. Ther Adv Psychopharmacol. 2013;3(1):33–51. | ||
Lawrence D, Kisely S. Inequalities in healthcare provision for people with severe mental illness. J Psychopharmacol. 2010;24(4 Suppl):61–68. | ||
Dalle Grave R, Calugi S, Centis E, Marzocchi R, El Ghoch M, Marchesini G. Lifestyle modification in the management of the metabolic syndrome: achievements and challenges. Diabetes Metab Syndr Obes. 2010;3:373–385. | ||
Bak M, Fransen A, Janssen J, van Os J, Drukker M. Almost all antipsychotics result in weight gain: a meta-analysis. PLoS One. 2014;9(4):e94112. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.