Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 13
Prevalence of Metabolic Syndrome and Its Association with Sociodemographic Characteristics in Participants of a Public Chronic Disease Control Program in Medellin, Colombia, in 2018
Authors Higuita-Gutiérrez LF , Martínez Quiroz WJ, Cardona-Arias JA
Received 18 December 2019
Accepted for publication 3 March 2020
Published 16 April 2020 Volume 2020:13 Pages 1161—1169
DOI https://doi.org/10.2147/DMSO.S242826
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Luis Felipe Higuita-Gutiérrez,1 Wilson de Jesús Martínez Quiroz,2 Jaiberth Antonio Cardona-Arias3
1Cooperative University of Colombia, University of Antioquia, Medellín, Colombia; 2Metrosalud, Medellín, Colombia; 3School of Microbiology, University of Antioquia, Medellín, Colombia
Correspondence: Luis Felipe Higuita-Gutiérrez Calle 70 Número 52 – 51, Medellín, Colombia
Tel +5742198486
Fax +5742195486
Email [email protected]
Background: Metabolic syndrome has increased to epidemic levels in low- and middle-income countries. The knowledge on metabolic syndrome and its related diseases constitutes a clinical, epidemiological, and economic challenge of great relevance. The frequency of metabolic syndrome may vary between populations depending on age, sex, lifestyle, and culture; however, in Colombia, there is only little research, and the available studies focus on small populations that do not allow estimating their prevalence and distribution in different sociodemographic groups. We aimed to estimate the prevalence of metabolic syndrome and its association with sociodemographic characteristics in participants attending public chronic disease control programs in Medellin, Colombia, in the year 2018.
Methods: We conducted a cross-sectional study in all patients who participated in a public chronic disease control program. Involved in this study were 68,288 individuals who attended at 10 hospital units and were strategically distributed in the city. The diagnostic criteria of the metabolic syndrome and its components were based on the consensus of the Latin American Diabetes Association. The data on age, sex, blood pressure, weight, height, physical activity, medications, lipid profile, and glycemic and glycosylated hemoglobin levels were obtained for clinical records. The prevalence, Pearson’s chi-square test, prevalence ratios (Kato-Katz method), and odds ratios (Woolf method) were estimated with 95% confidence intervals. A multivariate adjustment model was used with a logistic regression model to identify potential confounders using Epidat 4.2 and SPSS® 25.0.
Results: The prevalence of the syndrome was 35.4%, with abdominal obesity in 82.3% individuals, hypertension in 48.6%, glucose intolerance in 25.5%, and hypertriglyceridemia in 22%. The prevalence of the syndrome exhibited statistical differences according to the area of residence. It was 15% higher in women; 31% and 59% higher in young and older adults, respectively, than in individuals aged < 25 years; 11% and 13% higher in the illiterate population and population with primary studies than in individuals with higher education; and approximately 200 times higher than those who are sedentary.
Conclusion: A high prevalence of the syndrome and its constitutive factors in the study population demonstrated the importance of controlling it and increasing community-based prevention strategies, prioritizing the identified groups that are at the highest risk.
Keywords: prevalence, metabolic syndrome, risk factor, Colombia
Background
Obesity is a clinical problem related with hypertension, heart disease, stroke, locomotor disorders, some types of cancer, and diabetes mellitus.1 In terms of public health, it causes 3 million deaths per year globally, in addition to approximately 36 million people that die of related pathologies like the chronic diseases.2,3 The increase in obesity has been parallel to the increase in the prevalence of metabolic syndrome, which has been related to factors, such as improvement of the financial situation, nutritional changes, genetic predisposition, and reduction of physical activity, which affect most of the adults – women in particular.4,5
In this order of ideas, several systematic reviews have reported a high prevalence of metabolic syndrome.6,7 Thus, in a study published in 2017 which included 18 researches involving approximately 57,000 adults in 51 Asian countries, the prevalence ranged between 12% and 49% and was higher in women and residents of urban areas. Despite differences in the diagnostic criteria and study methodologies, it was concluded that approximately 20% of subjects were affected, with an increase of approximately 10% in the last decade.6 A systematic review of 59 studies reported a heterogeneous frequency between countries and years of study, in ranges of 2.2–44% in Turkey, 16–41% in Saudi Arabia, 14–63% in Pakistan, 26–33% in Qatar, 9–36% in Kuwait, 22–50% in the UAE, 6–42% in Iran, and up to 23% in Yemen. The combined prevalence estimate was 25%, with an attributable risk of 15.9%, 11.7%, and 16.2% for cardiovascular disease, coronary heart disease, and stroke, respectively.7
The high prevalence of metabolic syndrome was generally associated with high-income countries, but currently, metabolic syndrome and obesity have presented a rapid increase in their prevalence in low- and middle-income countries due to the epidemiologic transition characterized by population growth, aging, nutritional transition with increased consumption for calories, and sedentary lifestyles. These factors increase morbidity and mortality.5
In Colombia, there has been an accelerated nutritional transition with a progressive decrease in the prevalence of delayed height and a parallel increase in obesity.8 In addition, the prevalence of current smoking in Colombian adult women is 3% and leisure time or physical inactivity is 93.7%.9 The demographic transition reflects an accelerated population aging with a rate of 40.4%, and the population over 60 years increased from 6.5% in 2005 to 9.1% in 2018.10
These characteristics of the Colombian population suggest that the metabolic syndrome may have important proportions. However, this issue has been addressed by a few studies. A prevalence of 9% has been reported in 494 children aged between 5 and 9 years, and it was associated with age and low socioeconomic level.11 In 129 Colombian adults who worked as drivers, a prevalence of 49.6% was found, which was associated with low levels of weekly physical activity.12 Specifically, in Medellin, Colombia, only one study was found with a prevalence of 20–24%, which was conducted with 271 women who attended a clinic in 2002.13
The high impact of the management of the syndrome and associated diseases in low- and middle-income countries have shown the need to implement different interventions and community programs involving all age groups.4,5 Nevertheless, it is necessary for the design and success of these interventions, adequate knowledge of the magnitude of the population affected by the metabolic syndrome, and particularly the associated factors in each case and place. In this sense, the objective of this study was to estimate the general prevalence of metabolic syndrome and its specific prevalence according to sociodemographic factors of participants in the public chronic disease control program of Medellin in the year 2018, with the purpose of reporting the population data to the national statistics which could focus on ways to control this problem.
Methods
Study Design and Setting
This was a cross-sectional study in the city of Medellin. Medellin is the second-largest city in Colombia. It is divided into 16 communes and four corregimientos (rural area), with a population of 2,376,330 people. About 72.3% of its habitants aged between 15 and 64 years, where 47% are men and 53% are women. Regarding the socioeconomic aspects, Medellin, with a Gini coefficient of 0.52, is a region with high inequality.10,14
This study involved 68,288 individuals over 17 years of age who voluntarily participated in a public chronic disease control program from January to December of 2018 which was conducted by the most important public hospital network in the city, which includes 10 hospital units (Figure 1) located in strategic sites throughout the city of Medellin and its corrections [provinces] with 50 attention points. The actions developed in the program are covered by a health plan (care by a doctor and/or nursing, diagnostic aids, medicines, and care and support from professionals and specialists according to the parameters defined by the country’s regulations) and do not generate any type of payment by users.
 |
Figure 1 Medellin’s communes and distribution of programs in hospital units. |
Participants
In this study, the sampling process serves as a census in which we include the totality of individuals who met the next criteria. The inclusion criterion was an active engagement in the program with at least two follow-ups during the year 2018. The prevalence was defined as compliance with metabolic syndrome criteria in any control performed during the year. Individuals whose clinical records had issues regarding logical verification (poorly entered data, such as out-of-range values, residences in different municipalities, etc.) and those who had information from duplicate consultations were excluded to avoid overestimation of the frequency of the diseases studied. The underestimation of metabolic syndrome was avoided with the inclusion of all population. The measurement of weight, height, and blood pressure was performed by experienced medical practitioners. The determination of biochemical parameters was performed in authorized laboratories.
Definition of Operational Terms
The definition of metabolic syndrome was based on the Latin American Diabetes Association consensus, which also corresponds to the International Diabetes Federation criteria of Europe.11 This includes abdominal obesity (which means waist circumference of ≥94 cm in men and ≥88 cm in women) and two of the following criteria:
- High triglyceride levels of >150 mg/dl or undergoing lipid-lowering treatment.
- Low high-density lipoprotein cholesterol (cHDL) level of <40 mg/dl in men and <50 mg/dl in women or in treatment with effect on cHDL.
- High blood pressure with systolic blood pressure (SBP) of ≥130 mm Hg and/or diastolic blood pressure (DBP) of ≥85 mm Hg or in antihypertensive treatment.
- Impaired glucose regulation of ≥100 mg/dl in fasting blood glucose test or diabetes.15
The measurement of smoking and alcoholism was based on patient’s consumption in the last month, at least once a week. For regular physical activity, the performance of intense or moderate physical activities at least three times a week (inactive/active) was evaluated.
Data Sources
A secondary source of information was used, which comprised of the electronic clinical history form that is routinely filled out by the physician at the health institution, from which the following variables were extracted: age; sex; weight; height; body mass index; blood pressure; medications, such as diuretics, angiotensin-converting enzyme (ACE) inhibitors, calcium antagonists, beta-blockers, alpha-blockers, and insulin- and lipid-lowering drugs; and the progress on complementary tests, including the testing lipid profile and glycemic and glycosylated hemoglobin levels.
Statistical Methods
The description of age was made with summary measures and the remaining variables with frequencies. The prevalence of metabolic syndrome and each of its components were estimated to have 95% confidence intervals. The specific prevalence of the syndrome was estimated according to the sociodemographic conditions of the population. They were compared using the Pearson’s chi-square test, prevalence ratios (Kato-Katz method), and odds ratios (Woolf method), with 95% confidence intervals. For the last two, the formula [(OR-PR)/(OR-1)] was used to evaluate a possible overestimation of the odds ratio. Given the statistical equality of both ratios and low proportion (<0.5) of overestimation, the multivariate adjustment model was used with a logistic regression model to identify potential confounders (we evaluated whether the bivariate statistical association was preserved while making adjustments based on third variables; independent variables of the model were those that fulfilled the three requirements required for potential confounders that were as follows: being associated with the event, being associated with another independent variable, and not being an intermediate step in the potential causal horizon), whose goodness of fit was determined using Wald’s and Hosmer–Lemeshow formulas. In logistic models, the dependant variable was dichotomic (presence or absence of MS), and in case of independent variables, the group with the lowest MS occurrence was considered as a reference group. In case of polytomic variables, dummy variables were developed by comparing each group against the group with the lowest MS occurrence.
Before performing a confusion analysis, logistic regression models were developed to rule out the presence of interactions, in which variables would appear as independent variables related to MS and their interaction factor with other independent variables would be shown. Because there were five independent variables, interactions existing between each variable and the remaining ones were evaluated based on the following models (a similar model was developed for each independent variable):
Y = β0 + β1X1 + β2X2 + β3X3 + β4X4 + β5X5 + β1,2(X1*X2) + β1,3(X1*X3) + β1,4(X1× X4) + β1,5(X1 × X5)
This provides evidence that there is no interaction, assuming that in the logistic model ORs correspond to expβ.
Ethical Aspects
The project has the approval of the ethics committee of Metrosalud according to approval number 1400/4.3.
Results
From a total population of 89,271 patients, 54 were excluded because they were <18 years, 20,780 were excluded because they had less than two follow-up visits in the program in 2018, and 149 were excluded because their clinical records had logical verification problems. The program included individuals coming from all urban areas of the city (north, center, and south) and two villages; the majority were women adults over the age of 44 years, with a low level of formal education. Records of tobacco and alcohol consumption were low (Table 1).
 |
Table 1 Description of the Sociodemographic Characteristics of 68,288 participants of a Public Chronic Disease Control Program in Medellin in the Year 2018 |
The overall prevalence of metabolic syndrome was 35.4%. When analyzing the components of metabolic syndrome individually, a high prevalence of abdominal obesity (82.3%) and hypertension (48.6%) were found. A large proportion of subjects in the program is at a high risk of developing the syndrome owing to the presence of obesity and an additional component, such as abdominal obesity, arterial HTN, diabetes mellitus or intolerance, and low cHDL or hypertriglyceridemia (Table 2).
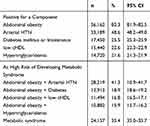 |
Table 2 Prevalence of Metabolic Syndrome and Its Components in 68,288 Participants of a Public Chronic Disease Control Program in Medellin in the Year 2018 |
The prevalence of metabolic syndrome showed statistical differences according to the area of residence, sex, age group, schooling, and physical activity, and it was 40% greater in Buenos Aires (area of greater prevalence) than in San Cristobal (area of lower prevalence); it was 15% higher in women than in men, 31–59% higher in adults than in individuals aged <25 years; 11% higher in the illiterate population and 13% higher in individuals with primary education than in those with higher education; and close to 200 times more in the population without regular physical activity (Table 3). There was no significant difference in the prevalence of metabolic syndrome between individuals who did (34.5% [n = 753]) or did not belong (35.4% [n = 23,404]) to the black ethnicity.
In the multivariate adjustment, all variables retained their statistical significance found via the bivariate analyses, showing the absence of possible changes in the effect. In addition, the measure of association adjusted by the variables of the model (area of residence, sex, age group, education, and physical activity) did not show statistical differences compared with the raw ones. Thus, a higher risk for MS was observed in the following groups: individuals living in Nuevo Occidente with OR of 1.64 (95% CI: 1.44–1.86) as opposed to those who lived in San Cristóbal (who showed lower risk), women with OR of 1.19 (95% CI: 1.14–1.24), patients aged between 45 and 64 years and OR of 1.91 (95% CI: 1.32–2.76), illiterate individuals or individuals with elementary school studies and OR of 1.16 (95% CI: 1.00–1.35), and sedentary patients with OR of 288 (95% CI: 129–643; Table 4).
 |
Table 4 Adjusted or with Multivariable Regression for Frequency of Metabolic Syndrome in 68,288 Participants of a Public Chronic Disease Control Program in Medellin in the Year 2018 |
Discussion
In this study, a prevalence of 35.4% was found in a population of 68,288 subjects who participated in a public program follow-up of chronic diseases, with a presence in all areas of Medellin, Colombia. It presented high frequency in individuals of both sexes and all age groups and levels of schooling, thus, increasing the possibilities of extrapolation of the results and indirectly showing that the population of the city was at risk for the syndrome and its related diseases.
The prevalence of metabolic syndrome (35.4%) found in this study is higher than the weighted average reported in two systematic reviews of Asian countries, wherein the combined values were 20% and 25%.6,7 However, the result obtained in this study is consistent with those of the studies included in the abovementioned reviews, in which a high heterogeneity was demonstrated, with a prevalence of 2.2–66%. This reveals the importance of standardizing the diagnostic criteria and conducting studies in each population of interest, given that the evidence of the magnitude of the syndrome is not consistent.6,7
The prevalence of metabolic syndrome was lower in the selected population included in this study than other studies in Colombia, such as adults working as drivers, where it was 50%,12 and adults between the ages of 25 and 64 years of Antioquia, where it was 40.7%16 and was higher than two studies in adolescents with 9.5%17 and 6.0%,18 respectively, and one study of healthcare personnel at the University of Antioquia 17.5%.19 The differences between the studies can be attributed to two reasons: on the one hand, the age of the population included is divergent and includes an adolescent population over 40 years old; on the other hand, the criteria for defining the metabolic syndrome were heterogeneous when taking into account the definition provided by the International Diabetes Federation (IDF), the Adult Treatment Panel III (ATP III), or Latin American Diabetes Association (ALAD). In addition, the studies described include samples of 280 to 1300 people out of 68,288 individuals included in this study. Also, it should be considered that the number of affected individuals in this study may increase, given that a high proportion of subjects 82.3% (81.9–82.5) is at risk of developing the syndrome owing to the presence of obesity. In a previous analysis in the ARIC cohort, it was reported that obesity was associated with 4.5 times the risk of developing incident metabolic syndrome over the three follow-up visits;20 this reveals the epidemic levels this metabolic disorder is reaching and the permanent risk of its increase if its constitutive factors are not addressed.
Abdominal obesity was observed in 82.3% individuals, arterial hypertension in 48.6%, glucose intolerance in 25.5%, and dyslipidemias (low cHDL or hypertriglyceridemia) in 22%. This coincides with global trends, wherein obesity (general and visceral) and the other components of the syndrome constitute one of the main public health problems worldwide, particularly in adults and teenagers. They also result in atherosclerosis, insulin resistance, and other clinical problems, leading to heart and cerebrovascular diseases, which could reduce the overall life expectancy.21
The prevalence of metabolic syndrome was associated with statistical differences according to the area of residence, sex, age group, schooling, and physical activity, which coincides with the risk factors that have been identified in other populations.4–6 The prevalence was 15% higher in women than in men, and in this group, metabolic syndrome was observed to be related to specific risk factors, such as early age of menarche, menopause, premenstrual syndrome, polycystic ovary, oral contraceptives, and pre-eclampsia or history of preterm births, to which the following risk factors are common to the majority of those affected, such as family and personal history of changes in blood pressure as well as lipid and glucose metabolism, smoking, sedentary lifestyle, and age.22
A greater risk was also identified with an increase in age, which was in agreement with findings of a majority of publications in this field;4–6,22 even in a longitudinal study, after controlling for various risk factors, it was concluded that metabolic syndrome increases by 2% for each year of increase in age, and this has been explained in terms of metabolism change and energy expenditure in adults. This demonstrates the importance of prioritizing young individuals for interventions based on health promotion or primary prevention and adults as individuals who require greater epidemiologic vigilance for control and care programs.23–25
Physical inactivity presented the highest adjusted risk in this population, which demonstrates the importance of improving public policies related to good use of free time and promotion of physical activity because this is associated with metabolic syndrome and a wide range of health problems. In addition, it is a risk factor for which effective and cost-effective interventions are available.26–28
Schooling had an effect independent of sex, age, physical activity level, and place of residence, with a higher risk in subjects belonging to a lower educational status, which demonstrated the importance of this social health determinant to improve the health actions. As indicated in previous publications, the identification of this type of health determinant is key for guiding programs focused on the prevention of health inequalities (in this case, in the distribution of metabolic syndrome) according to social status. It is important to identify groups in which there would be a greater impact or those in which it is necessary to prioritize actions for social justice and health equity.29
The foregoing statement emphasizes the need to improve primary prevention actions to reduce the morbidity and mortality associated with metabolic syndrome, costs of the management of the syndrome per se, and associated diseases as well as population studies that are useful in monitoring this epidemic in specific locations and maximize the benefits of public budgets in the health sector.6
The diseases triggered by the syndrome must be added to its high cost. To that effect, a previous study systematized the economic burden of 18,070 patients with cancers associated with metabolic syndrome, which represented an expense of 200 million dollars in 2018, demonstrating the need to reduce the burden of the syndrome and, thus, lower the economic burden associated with obesity, its syndromes, and subsequent diseases.30
Among the limitations of the study is the underreporting of other risk factors because physicians usually have a very limited consultation time coupled with a low public budget for health promotion actions, disease prevention, health surveillance, and public health actions in the Colombian health system framework. Despite these limitations, this study has advantages, such as being one of the first with a large sample size and being representative of the population of one of the main cities in the country because the hospital that runs the program has its presence across all the municipalities of Medellin.
Conclusion
In this study, a high prevalence of the syndrome and its constituent factors were found, being of greater concern the prevalence in women, adults, low school, sedentary, and those who reside in semi-urban areas of the city. This demonstrates the importance of controlling the risk factors of the identified groups at greatest risk as well as the organization of actions according to the needs of the groups in different sociodemographic strata.
Abbreviations
cHDL, high-density lipoprotein cholesterol; HDL, high-density lipoprotein; SBP, systolic blood pressure; DBP, diastolic blood pressure; HTN, hypertension; ACEIs, angiotensin-converting enzyme inhibitors.
Data Sharing Statement
The data that support the findings of this study are available from Metrosalud, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request at email [email protected] and with the permission of Metrosalud.
Ethics and Consent Statement
The project has the approval of the ethics committee of Metrosalud according to approval number 1400/4.3. Patients consented to the use of the information for investigative purposes and the analyses are based on data that do not contain information which could lead to the identification of the student. In Colombia, the scientific, technical, and administrative standards for health research are found in resolution 8430 of 1993. In it, research is classified as research without risk, with minimal risk, and with risk greater than the minimum. In Article 11 of that resolution, the research we carry out is classified as a risk-free investigation because it is a study that uses documentary research techniques and methods and in which no intervention or intentional modification of the biological, physiological, psychological or social variables of the individuals participating in the study.
Consent for Publication
Patients consented to the use of the information for investigative purposes, and the analyses are based on data that do not contain information which could lead to the identification of the patient.
Acknowledgments
E.S.E. Metrosalud Health institution provided the data of the subjects for this study.
Author Contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
Resources in kind were received from Metrosalud and Cooperative University of Colombia including working time for researchers, money for dissemination of results and software license.
Disclosure
The authors declare that they have no competing interests.
References
1. World Health Organization. Obesity and overweight; 2019. Available from: https://www.who.int/es/news-room/fact-sheets/detail/obesity-and-overweight.
2. World Health Organization. Ten facts about obesity; 2017. Available from: https://www.who.int/features/factfiles/obesity/es/.
3. World Health Organization. Chronic diseases; 2018. Available from: https://www.who.int/topics/chronic_diseases/es/.
4. Misra A, Bhardwaj S. Obesity and the metabolic syndrome in developing countries: focus on South Asians. Nestle Nutr Inst Workshop Ser. 2014;78:133–140. doi:10.1159/000354952
5. Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93:S9–S30. doi:10.1210/jc.2008-1595
6. Ranasinghe P, Mathangasinghe Y, Jayawardena R, Hills A, Misra A. Prevalence and trends of metabolic syndrome among adults in the Asia-pacific region: a systematic review. BMC Public Health. 2017;17:101. doi:10.1186/s12889-017-4041-1
7. Ansarimoghaddam A, Adineh H, Zareban I, Iranpour S, HosseinZadeh A, Kh F. Prevalence of metabolic syndrome in Middle-East countries: meta-analysis of cross-sectional studies. Diabetes Metab Syndr. 2018;12(2):195–201. doi:10.1016/j.dsx.2017.11.004
8. Lemus-Lemus F, Díaz Quijano DM, Rincón-Rodríguez CJ, Huertas-Moreno ML. Advances in understanding Colombia’s nutrition transition. Rev Gerenc Polit Salud. 2012;11(23):121–133.
9. Mendoza-Romero D, Urbina A, Cristancho-Montenegro A, Rombaldi A. Impact of smoking and physical inactivity on self-rated health in women in Colombia. Prev Med Rep. 2019;16:100976. doi:10.1016/j.pmedr.2019.100976
10. DANE. National Population and Housing Census; 2018. Available from: https://www.dane.gov.co/index.php/estadisticas-por-tema/demografia-y-poblacion/censo-nacional-de-poblacion-y-vivenda-2018/cuantos-somos. Accessed April 1, 2020.
11. Suarez-Ortegón M, Aguilar-de Plata C. Prevalence of metabolic syndrome in children aged 5–9 years from southwest Colombia: a cross-sectional study. World J Pediatr. 2016;12(4):477–483. doi:10.1007/s12519-016-0008-z
12. Rodríguez-Miranda C, Jojoa-Ríos J, Orozco-Acosta L, Nieto-Cárdenas O. Metabolic syndrome in public service drivers in Armenia, Colombia. Rev salud pública. 2017;19(4):499–505. doi:10.15446/rsap.v19n4.69758
13. Sánchez F, Jaramillo N, Vanegas A, et al. Prevalence and behaviour of risk factors in metabolic syndrome according to different age intervals, in a female cohort of the area of influence of the Clínica de las Américas in Medellín, Colombia. Rev Colomb Cardiol. 2008;15(3):102–110.
14. Medellin How are we doing. Medellin quality of life report; 2018. Available from: https://www.medellincomovamos.org/download/documento-informe-de-calidad-de-vida-de-medellin-2018/. Accessed April 1, 2020.
15. Rosas Guzmán J, González Chávez A, Aschner P, Bastarrachea R. Latin American Consensus of the Latin American Diabetes Association (LADA) Epidemiology, Diagnosis, Control, Prevention and Treatment of Metabolic Syndrome in Adults. LADA. 2010;XVIII(1):25–44.
16. Davila EP, Quintero MA, Orrego ML, et al. Prevalence and risk factors for metabolic syndrome in Medellin and surrounding municipalities, Colombia, 2008–2010. Prev Med. 2013;56(1):30–34. doi:10.1016/j.ypmed.2012.10.027
17. Serrano N, Villa-Roel C, Gamboa-Delgado EM, Barrera JG, Quintero-Lesmes DC. Early evaluation of the metabolic syndrome in Bucaramanga, Colombia. Transl Pediatr. 2019;8(5):363–370. doi:10.21037/tp.2019.04.04
18. Martínez-Torres J, Correa-Bautista J, González-Ruíz K, et al. A Cross-sectional study of the prevalence of metabolic syndrome and associated factors in colombian collegiate students: the FUPRECOL-adults study. Int J Environ Res Public Health. 2017;14(3):233. doi:10.3390/ijerph14030233
19. González-Zapata LI, Deossa GC, Monsalve-Álvarez J, Díaz-García J, Babio N, Salas-Salvadó J. Metabolic syndrome in healthcare personnel of the university of Antioquia-Colombia; LATINMETS study. Nutr Hosp. 2013;28(2):522–531. doi:10.3305/nh.2013.28.2.6315
20. Bradshaw PT, Monda KL, Stevens J. Metabolic syndrome in healthy obese, overweight, and normal weight individuals: the Atherosclerosis Risk in Communities Study. Obesity (Silver Spring). 2013;21(1):203–209. doi:10.1002/oby.20248
21. Engin A. The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol. 2017;960:1–17. doi:10.1007/978-3-319-48382-5_1
22. Molina D, Muñoz D. Metabolic syndrome in women. Rev Colomb Cardiol. 2018;25(S1):21–29. doi:10.1016/j.rccar.2017.12.006
23. World Health Organization. Global health risks. Mortality and burden of disease attributable to selected major risks. Geneva; 2009. Available from: https://apps.who.int/iris/handle/10665/44203.
24. Pajuelo J, Sánchez J. Metabolic syndrome in adults in Peru. An Fac Med. 2007;68(1):38–46. doi:10.15381/anales.v68i1.1237
25. Mejía C, Quiñones D, Cruzalegui C, Arriola I, Pérez L, Gomero R. Age as a risk factor for the occurrence of metabolic syndrome in mining workers at high altitudes. Argentine J Clin Endocrinol Metab. 2016;53(1):29–35. doi:10.1016/j.raem.2016.05.002
26. Mostafavi F, Ghofranipour F, Feizi A, Pirzadeh A. Improving physical activity and metabolic syndrome indicators in women: a transtheoretical model-based intervention. Int J Prev Med. 2015;6:28. doi:10.4103/2008-7802.154382
27. Messing S, Rütten A, Abu-Omar K, et al. How can physical activity be promoted among children and teenagers? A systematic review of reviews across settings. Front Public Health. 2019;7:55. doi:10.3389/fpubh.2019.00055
28. Cradock A, Barrett J, Kenney E, et al. Using cost-effectiveness analysis to prioritize policy and programmatic approaches to physical activity promotion and obesity prevention in childhood. Prev Med. 2017;95:S17–S27. doi:10.1016/j.ypmed.2016.10.017
29. Fernández A, Hernández S, Guadalupe M. Social determinants in health: their relationship with metabolic syndrome. Enf Neurol (Mex). 2013;12(3):122–127.
30. Kim D, Yoon S, Gong Y, et al. The economic burden of cancers attributable to metabolic syndrome in Korea. J Prev Med Public Health. 2015;48(4):180–187. doi:10.3961/jpmph.15.022
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

