Back to Journals » Drug, Healthcare and Patient Safety » Volume 10
Prevalence of medication errors in primary health care at Bahrain Defence Force Hospital – prescription-based study
Authors Aljasmi F , Almalood F , Al Ansari A
Received 1 August 2017
Accepted for publication 14 December 2017
Published 7 February 2018 Volume 2018:10 Pages 1—7
DOI https://doi.org/10.2147/DHPS.S147994
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Rajender R Aparasu
Fatema Aljasmi,1 Fatema Almalood,1 Ahmed Al Ansari2
1Department of Primary Health Care, 2Department of Training and Education, Bahrain Defence Force Hospital, West Riffa, Kingdom of Bahrain
Background: One of the important activities that physicians – particularly general practitioners – perform is prescribing. It occurs in most health care facilities and especially in primary health care (PHC) settings.
Objectives: This study aims to determine what types of prescribing errors are made in PHC at Bahrain Defence Force (BDF) Hospital, and how common they are.
Methods: This was a retrospective study of data from PHC at BDF Hospital. The data consisted of 379 prescriptions randomly selected from the pharmacy between March and May 2013, and errors in the prescriptions were classified into five types: major omission, minor omission, commission, integration, and skill-related errors.
Results: Of the total prescriptions, 54.4% (N=206) were given to male patients and 45.6% (N=173) to female patients; 24.8% were given to patients under the age of 10 years. On average, there were 2.6 drugs per prescription. In the prescriptions, 8.7% of drugs were prescribed by their generic names, and 28% (N=106) of prescriptions included an antibiotic. Out of the 379 prescriptions, 228 had an error, and 44.3% (N=439) of the 992 prescribed drugs contained errors. The proportions of errors were as follows: 9.9% (N=38) were minor omission errors; 73.6% (N=323) were major omission errors; 9.3% (N=41) were commission errors; and 17.1% (N=75) were skill-related errors.
Conclusion: This study provides awareness of the presence of prescription errors and frequency of the different types of errors that exist in this hospital. Understanding the different types of errors could help future studies explore the causes of specific errors and develop interventions to reduce them. Further research should be conducted to understand the causes of these errors and demonstrate whether the introduction of electronic prescriptions has an effect on patient outcomes.
Keywords: medical errors, general practice, prescribing errors, omission errors, commission errors, rational drug use
Introduction
PHC is responsible for promoting health by treating and preventing disease, and is therefore treated as the foundation of health care. It is the first contact between the patient and the health care system and is supported by secondary care’s referral system.1
It is extremely important for the international health care system to assess health care services for quality and accreditation.2 By determining errors in primary care and seeking to reduce them, the health care system can improve clinical outcomes, and reduce hospitalizations, costs, and lawsuits, while increasing the level of trust between patients and physicians.3
One of the most important responsibilities of physicians – particularly GPs in the setting of PHC – is to prescribe drugs,4 yet prescription errors continue to occur. The likelihood of such errors and the consequent harm to patients is increased by a high flow of patients, reduced consultation times, ignorance, and incompetence.4 It is therefore important to recognize how often each type of error occurs as a first step to creating policies that reduce the consequent harms and danger to patients.5
Studies show that there are errors in all stages of the therapeutic process from prescribing to patient compliance.6–8 Medical errors occur in primary care settings between five and 80 times per 100,000 consultations.5 Prescribing and prescription errors occur in up to 11% of all prescriptions in primary care settings.5 The factors shown to contribute to medication errors in primary care include polypharmacy, the variation in drug names (i.e. brand vs. nonbrand names), and the lack of good record-keeping.4,9
There is an insufficient number of studies concerning medication errors in the Middle East, and consequently little knowledge about the errors.6 Such ignorance includes the frequency of medication errors in Saudi Arabia.10 According to the existing studies, the proportion of inappropriately written prescriptions is high,4 and a cross-sectional study of randomly selected patients by Khoja et al used a Neville system of classification and found that 18.7% of prescriptions contained errors.12 A retrospective study by Al Khaja et al found that in Bahrain the proportion of incorrect prescriptions amounted to 90%,13 and this was as high as 90.5% for infants.6 Since there has been little research on the topic of medication errors in the Middle East, the present study investigated the drug-prescribing patterns and prescription errors in PHC at BDF Hospital, in an effort to improve patient safety.
Methodology
Setting
This study was conducted in the Kingdom of Bahrain’s second largest hospital, the BDF Hospital. Located in the middle of the country, it treats around 20,500 inpatients each year, and conducts over 400,000 outpatient consultations.14 The Australian Council on Healthcare Standards recognized the BDF Hospital’s commitment to “Quality, Safety, and Efficiency” and accredited the hospital in 2007.
The PHC department within BDF Hospital provides prevention and cure services to patients and families of various ages and from different parts of Bahrain. The PHC department provides services such as maternal and child health care, as well as diabetic, dermatology, and fundus examination of diabetic clinic, to all BDF-entitled patients with a wider scope than any other department, and also includes clinics for outpatient parenteral antimicrobial therapy. Services at the PHC aim at promoting physical, mental, and social health, and curing both acute and chronic issues. The general practice clinic runs from 7 am to 11 pm every day, and employs 20 physicians, including 16 postgraduate family physicians and four GPs. On average, it serves 349 patients each day, providing 7–10 minutes of consultation for each. The PHC department also has an outpatient pharmacy with two pharmacists present at any given time.
Data source and variability
This study used retrospective data from the PHC department of the BDF Hospital, including both general clinics and mini clinics. The PHC at BDF Hospital keeps all prescriptions for 3 months before discarding them. In the sample size calculation, the prevalence “p” was allowed a 5% margin of error, which is the amount of error that can be tolerated. With a 5% margin of error and 95% confidence interval, a minimum of 377 prescriptions was required, which is appropriate for this study as it has a sample size of 379. The data for the study consisted of 379 prescriptions that were selected using a simple randomization technique from the PHC pharmacy’s records, out of the prescriptions of 28,212 attendees between March and May 2013. In this study, each patient was given only one prescription, and this prescription could include multiple drug orders. No patient’s prescription was more likely to be selected than that of any other patient.
The primary investigator was the only one allowed to examine the prescription forms. The prescription was analyzed, and its information as well as an indication of any type of error was reported on an excel file by the primary investigator.
Ethical approval
This research was approved by the Research and Research Ethical Committee at the BDF Hospital. The study reference number was BDF/R&REC/2014-36. The information about the patients was made anonymous; therefore, the Committee did not require patient consent for this study.
Classification of errors
The system for the classification of errors used in this study was derived from the one used in a previous study in Bahrain with the addition of a new factor: skill-based errors.13,15 The classification reported in this study has been used previously in several studies and is applicable only to hand-written prescriptions.6,16–22 The following are the five types of prescription errors:
- -Major omission errors
- -Minor omission errors
- -Commission errors
- -Integration errors
- -Skill-related errors
Minor omission errors include leaving out/neglecting minor information such as date, personal identifiers of the patients, or the doctor’s stamp.16,17 For an omission error to be considered major, important elements of the prescription’s body, such as drug, dose/strength, drug form, frequency, and duration, must be left out, imprecise, incomplete, or indecipherable. Commission errors occur when the components of the prescription’s body are inappropriately written.17,18 Since this study concerns only what is written on prescription forms, it excluded integration errors and knowledge-based errors, such as those involving interactions between drugs and allergies, or between drugs and other drugs.18,21–23 Unlike minor omission errors which in this study involve neglect of minor information, skill-related prescription errors include errors in executing correctly planned actions due to skills such as illegible handwriting or unconventional abbreviations.22,23 Although these types of errors may seem to overlap, skill-based errors will be looked at separately.16,17,19,20,22 To check for skill-related prescription errors, the study referred to BDF’s policy concerning common abbreviations. This study excluded prescriptions involving nondrug items such as syringes and rubbing alcohol.
Appropriate use of drugs is essential for proper patient care. To assess performance in prescribing, the study used the World Health Organization (WHO) core drug use indicators. These indicators include:23–26
- -Average number of drugs per prescription
- -Percentage of drugs prescribed using a generic name
- -Percentage of prescriptions that included an antimicrobial or antimicrobials
- -Percentage of drugs that were prescribed from national medicine lists such as the BNF,19 WHO drug list,20 and BahNF.20
This study reviewed prescriptions using the above classification method, and calculated the percentage of errors in each category (major omission, minor omission, skill-related, commission). The data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 19 (SPSS Inc., Chicago, IL, USA), and are expressed as percentage, mean, and SD.
Results
Each prescription included one to nine drugs. The mean number of drugs in each prescription was 2.6, according to the WHO core drug use indicators (±1.4) (Table 1).20 Of the total patient prescriptions, 19.3% (N=73) included only a single drug. In the prescriptions, 8.7% of the drugs were prescribed using their generic names, and 28% (N=106) of prescriptions included an antibiotic or antibiotics. While all the prescribed drugs were from BNF and BahNF (N=992), only 57% (N=565) were from the WHO drug list.20
  | Table 1 Pattern of WHO core drug use indicators Abbreviations: BNF, British National Formulary; BahNF, Bahrain National Formulary; WHO, World Health Organization. |
Of the 379 analyzed prescriptions, those for males amounted to 206 (54.4%), while there were 173 prescriptions written for females (45.6%). There were prescriptions for patients ranging from newborn to 76 years of age; the average age was 28.9 years (mean ±19.9; median=26). Table 2 shows that the 0–10 and 21–30 age groups had the highest frequency of prescriptions, whereas the 60 and above age group had the lowest frequency.
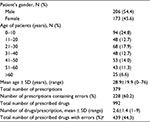  | Table 2 Demographic data of patients and prescription statistics Note: aErrors of omission (major), commission, and skill-related errors. |
Of the total prescriptions, 60.2% (N=228) contained errors. Table 3 shows the types of minor omission errors: 0.5% (N=2) were related to errors in name, age, sex, and date, and 7.9% (N=30) were related to a missing or unclear physician’s stamp.
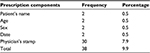  | Table 3 Prescription errors (minor omission) |
Of the 992 drugs prescribed, 44.3% (N=439) contained errors. As shown in Table 4, 73.6% (N=323) of the errors were major omission errors, 9.3% (N=41) were commission errors, and 17.1% (N=75) were skill-related errors.
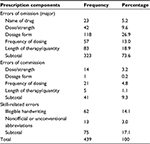  | Table 4 Errors in prescribed drugs |
The age group distribution, as well as the major omission errors, are presented in Table 5.
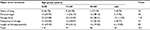  | Table 5 Omission errors (major) and age group Note: Data are presented as frequency (percentage). |
When examining the types of errors in the prescriptions studied, the prescriptions of 36% (N=137) of the patients were found to contain no errors, and there was only one type of error in the prescriptions of 39% (N=148) of the patients, two types of errors in those of 22% (N=82) of the patients, and three different types of errors in the prescriptions of 3% (N=12) of the patients. No prescriptions contained more than three different types of errors.
The types of errors present in prescriptions with an antibiotic prescribed were also examined separately. Of the prescriptions containing an antibiotic order, 11% (N=12) had minor omission errors, 62% (N=66) had major omission errors, 11% (N=12) had commission errors, and 15% had skill-related errors. There was no significant difference between the types of errors in prescriptions with antibiotics.
Discussion
This retrospective study used data from 379 prescriptions, and analyzed them with WHO core drug use indicators.27 These prescriptions included drugs for the treatment of a variety of conditions for patients with a mean age of 28.9 years, which is similar to the mean age of those in the military in Bahrain and their families.
This study used the WHO indicators to determine the amount of drugs prescribed per prescription. Although 19.3% (N=73) of prescriptions analyzed in the study only had a single drug, the average number of drugs in a prescription was 2.6. This was only slightly higher than the WHO-recommended average of 2.0 drugs per prescription.28 The results of this study also indicated a slightly higher average than a study of 10 developing countries in which a mean of 1.6 drugs was found, as well as findings from a private sector in Dubai which found a mean of 2.2 drugs per prescription and 37% of the prescriptions containing only one drug.29,30 On the other hand, the findings of this study indicated an improvement over a 2004 study of all PHC centers in Bahrain, which indicated 3.3 drugs per prescription on average, and only 6.3% of prescriptions with only one drug.30 However, some developing countries (Indonesia and Nigeria) had means of 3.3 and 3.8 drugs per perscription.29 This further suggests that the mean number of drugs prescribed per prescription found in this study is not too high; however, it is slightly higher than the average number of drugs prescribed per prescription recommended by the WHO, and so policies of rational drug use can be adopted to reduce the number of drugs administered and ensure this does not increase, to avoid negative drug interactions and unnecessary costs.
In this study, 8.7% (N=86) of drugs were prescribed by generic names rather than by their brand names. This figure was lower than that found in Lebanon, which was 2.9%.31 The reason for this is that physicians in the PHC at BDF Hospital prefer brand-name drugs over generic drugs. The physicians in many other countries prescribe a high number of generic drugs, and those in some countries, such as Niger,32 in fact prescribe only (or almost only) generic drugs. This is an important point to consider, since generic drugs in the PHC pharmacy are usually good-quality drugs, and come from drug manufacturers approved by the US Food and Drug Administration. It is likely that the high number of prescriptions using brand names is due to patients thinking there is an advantage of taking brand-name drugs over generic drugs.30
Another issue in the health care system is the overreliance on antibiotics, which is a hazard for international health. When antibiotics are prescribed irrationally, it can result in negative reactions and inappropriate hospital admissions, which can bring about errors in medication. Previous studies found that the proportions of prescriptions containing antibiotics were 45.8% in Bahrain,30 60.9% in Jordan,33 and 56.2% in Saudi Arabia.34 Our study, however, found a proportion of 28%, which matches the pattern of antibiotic prescription rates in Europe, for example, Andorra’s rate of 27%,35 and the rates in Central and South American countries such as Guatemala and Ecuador.29 Such low rates indicate that physicians are knowledgeable about how bacterial resistance increases if antibiotics are more frequently administered. However, in the prescriptions containing antibiotics, there was a high percentage of major omission errors (62%, N=66), and other types of errors also existed. This suggests that while the frequency of antibiotics administration is not a problem, medication errors in prescriptions containing an antibiotic could have a negative influence on the proper use of antibiotics. While the error percentages do not demonstrate the number of errors in separate antibiotic orders (as this was not measured in this study), the findings still demonstrate that prescription orders including an antibiotic still contained some errors. Future studies should look at the frequency and error rates of antibiotic orders separately to demonstrate whether antibiotics are being used appropriately.
This study found that minor omission errors comprise 9.9% (N=38) of all errors, with most of them being related to physician’s stamp. These results roughly matched those of Al Khaja et al’s study.6 A practical way to solve this issue would be to use an electronic prescription framework.
The proportions of major omission and commission errors found in our study were 73.6% (N=323) and 9.3% (N=41), respectively. These differed from another Bahrain study on PHC,15 which found proportions of 93.6% and 6.3%, respectively. One explanation for this difference could be that the error rates are related to physician’s experience: the hospitals where the studies took place had different proportions of family doctors vs. GPs.
This study found that 17.1% (N=75) of prescription errors were skill-related, with 14.1% (N=62) resulting from unreadable handwriting. This is another issue that could be easily remedied by using electronic prescriptions. Our data on integration errors such as drug–drug interaction and allergies to drugs were unsatisfactory, and therefore, more research is needed.
One limitation of this study was that it left out data on integration errors, which are significant because such errors have consequences related to drug–drug interactions and drug allergies. Therefore, more research needs to be done into such errors. On the other hand, one of the strengths of this study was that it was performed in a military PHC hospital, and its measurements of prescription errors can be utilized as a point of comparison for other studies.
Another limitation is that limited data were collected on variables which could influence the number of drugs prescribed as well as the error rate. For example, a future study should collect data on the comorbidities of the patients and well differentiate between prescribers (e.g. family doctors vs. GPs).
It should also be noted that much confusion and irrational drug prescription can be avoided by switching to generic names of drugs, which would clarify the options for drugs prescribed, and would lower costs.13 Understanding the types of prescription errors that occur is important because medication errors can be very harmful to patients and can lead to negative effects such as increased hospitalizations and reduced clinical outcomes.3 The results of this study provide awareness of the existence of prescription errors and the frequency of the different types of errors. This information can be used by future studies to identify the causes of these different types of errors as well as develop interventions to avoid them; this could in turn address the patient harm that medication error leads to.3 Since prescription errors are avoidable,9 it is important to educate physicians about rational drug use and the dangers of polypharmacy.36 In addition, drug formularies should be available to physicians as a way of achieving cost-effectiveness. Finally, an electronic prescription framework can be used to avoid omission errors and skill-related errors.11
Conclusion and recommendation
This study identified how common various types of prescription errors were in the PHC clinics in the BDF Hospital. It found that 60.2% (N=228) of prescriptions had errors, and 44.3% (N=439) of the prescribed drugs had errors. Both are unacceptably high levels. A possible way to avoid these errors is using an improved prescription-writing system (such as an electronic system), as well as educating physicians on rational drug prescription.
Abbreviations
BahNF, Bahrain National Formulary
BDF, Bahrain Defence Force
BNF, British National Formulary
GPs, general practitioners
PHC, primary health care
Author contributions
Authors Ahmed Al Ansari, Fatema Aljasmi and Fatema Almalood contributed to the conception and design of the study and worked on the data acquisition. Ahmed Al Ansari contributed to the data analysis and interpretation. All the authors contributed to the drafting of the manuscript and gave approval of the final version to be published.
Disclosure
The authors report no conflicts of interest in this work.
References
Ministry of Health – Kingdom of Bahrain. Primary health care. 2011. Available from: http://www.moh.gov.bh/EN/MOHServices/Services/primaryHealthCare.aspx. Accessed May 20, 2014. | ||
Morris CJ, Cantrill JA, Helper CD, Noyce PR. Preventing drug-related morbidity—determining valid indicators. Int J Qual Health Care. 2002;14(3):183–198. | ||
Kaprielian V, Østbye T, Warburton S, Sangvai D, Michener L. A system to describe and reduce medical errors in primary care. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 1: Assessment). Rockville, MD: Agency for Healthcare Research and Quality; 2008. | ||
Al-Hussein FA. Prescription non-conformities in primary care settings: how useful are guidelines. J Family Community Med. 2008;15(2):51–56. | ||
Sandars J, Esmail A. The frequency and nature of medical error in primary care: understanding the diversity across studies. Fam Pract. 2003;20(3):231–236. | ||
Al Khaja KA, Al Ansari TM, Damanhori AH, Sequeira RP. Evaluation of drug utilization and prescribing errors in infants: a primary care prescription-based study. Health Policy. 2007;81(2–3):350–357. Accessed December 5, 2014. | ||
ASPH guidelines on preventing medication errors in hospitals. Am J Hosp Pharm. 1993;50(2):305–314. | ||
National Coordinating Council for Medication Error Reporting and Prevention. About medications errors [cited June 2014]. Available from: www.nccmerp.org. | ||
Patel V, Vaidya R, Naik D, Borker P. Irrational drug use in India: a prescription survey from Goa. J Postgrad Med. 2005;51(1):9–12. | ||
Aljadhey H, Mahmoud MA, Hassali MA, et al. Challenges to and the future of medication safety in Saudi Arabia: a qualitative study. Saudi Pharm J. 2014;22(4):326–332. | ||
Velo GP, Minuz P. Medication errors: prescribing faults and prescription errors. Br J Clin Pharmacol. 2009;67(6):624–628. | ||
Khoja T, Neyaz Y, Qureshi NA, Magzoub MA, Haycox A, Walley T. Medication errors in primary care in Riyadh City, Saudi Arabia. East Mediterr Health J. 2011;17(2):156–159. | ||
Al Khaja KA, Sequeira RP, Al-Ansari TM, Damanhori AH. Prescription writing skills of residents in a family practice residency programme in Bahrain. Postgrad Med J. 2008;84(990):198–204. | ||
Bahrain Defence Force – Royal Medical Services 2015 annual report. Available from: http://rms/documents/annualreports/BDF_AR_2015_English.pdf. Available January 10, 2018. | ||
Al Khaja KA, Al-Ansari TM, Sequeira RP. An evaluation of prescribing errors in primary care in Bahrain. Int J Clin Pharmacol Ther. 2005;43(6):294–301. | ||
Howell RR, Jones KW. Prescription-writing errors and markers: the value of knowing the diagnosis. Fam Med. 1993;25(2):104–106. | ||
Shaughnessy AF, Nickel RO. Prescription-writing patterns and errors in a family medicine residency program. J Fam Pract. 1989;29(3):290–295. | ||
Rupp MT, Schondelmeyer SW, Wilson GT, Krause JE. Documenting prescribing errors and pharmacist interventions in community pharmacy practice. Am Pharm. 1988;NS28(9):30–37. | ||
Joint Formulary Committee. British National Formulary (BNF) (#63). London: Pharmaceutical Press; 2012. | ||
WHO. Essential medicines selection. Bahrain National Medicines List/Formulary/Standard Treatment Guidelines. Drug Formulary. 2009. Available from: http://www.who.int/selection_medicines/country_lists/bhr/en/. Accessed September 2017. | ||
Rosack J. Antipsychotics prone to prescribing errors. Psychiatric News. 2006;41(14):8–41. | ||
Aronson JK. Medication errors: definitions and classification. Br J Clin Pharmacol. 2009;67(6):599–604. | ||
Ferner RE, Langford NJ, Anton C, Hutchings A, Bateman DN, Routledge PA. Random and systematic medication errors in routine clinical practice: a multicentre study of infusions, using acetylcysteine as an example. Br J Clin Pharmacol. 2001;52(5):573–577. | ||
Sapkota S, Pudasaini N, Singh C, Sagar GC. Drug prescribing pattern and prescription error in elderly: a retrospective study of inpatient record. Asian J Pharm Clin Res. 2011;4(3):129–132. | ||
Desalegn AA. Assessment of drug use pattern using WHO prescribing indicators at Hawassa University Teaching and Referral Hospital, South Ethiopia: a cross-sectional study. BMC Health Serv Res. 2013;13:170. | ||
Enwere OO, Falade CO, Salako BL. Drug prescribing pattern at the medical outpatient clinic of a tertiary hospital in southwestern Nigeria. Pharmacoepidemiol Drug Saf. 2007;16(11):1244–1249. | ||
How to investigate drug use in health facilities: selected drug use indicators. EMD Research Series No. 007. 1993. | ||
Ghimire S, Nepal S, Bhandari S, Nepal P, Palaian S. A prospective surveillance of drug prescribing and dispensing in a teaching hospital in western Nepal. J Pak Med Assoc. 2009;59(10):726–731. | ||
Hogerzeil HV, Bimo, Ross-Degnan D, et al. Field tests for rational drug use in twelve developing countries. Lancet. 1993;342(8884):1408–1410. | ||
Otoom S, Culligan K, Al-Assoomi B, Al-Ansari T. Analysis of drug prescriptions in primary health care centres in Bahrain. East Mediterr Health J. 2010;16(5):511–515. | ||
Hamadeh GN, Dickerson LM, Saab BR, Major SC. Common prescriptions in ambulatory care in Lebanon. Ann Pharmacother. 2001;35(5):636–640. | ||
Mallet HP, Njikam A, Scouflaire SM. [Evaluation of prescription practices and of the rational use of medicines in Niger]. Sante. 2001;11(3):185–193. French [with English abstract]. | ||
Otoom S, Batieha A, Hadidi H, Hasan M, Al-Saudi K. Evaluation of drug use in Jordan using WHO prescribing indicators. East Mediterr Health J. 2002;8(4–5):537–543. | ||
Mahfouz AA, Shehata AI, Mandil AM, Al-Erian RA, Al-Khuzayem AA, Kisha A. Prescribing patterns at primary health care level in the Asir region, Saudi Arabia: an epidemiologic study. Pharmacoepidemiol Drug Saf. 1997;6(3):197–201. | ||
Vallano A, Montané E, Arnau JM, et al. Medical speciality and pattern of medicines prescription. Eur J Clin Pharmacol. 2004;60(10):725–730. | ||
Bateman DN, Eccles M, Campbell M, Soutter J, Roberts SJ, Smith JM. Setting standards of prescribing performance in primary care: use of a consensus group of general practitioners and application of standards to practices in the north of England. Br J Gen Pract. 1996;46(402):20–25. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
