Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
Prevalence of major depressive disorder among hemodialysis patients compared with healthy people in Japan using the Structured Clinical Interview for DSM-IV
Authors Tomita T , Yasui-Furukori N, Sugawara N , Ogasawara K, Katagai K, Saito H, Sawada K, Takahashi I, Nakamura K
Received 20 February 2016
Accepted for publication 13 June 2016
Published 30 September 2016 Volume 2016:12 Pages 2503—2508
DOI https://doi.org/10.2147/NDT.S106817
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Tetsu Tomita,1 Norio Yasui-Furukori,1 Norio Sugawara,1,2 Kohei Ogasawara,3 Koki Katagai,3 Hisao Saito,4 Kaori Sawada,5 Ippei Takahashi,5 Kazuhiko Nakamura1
1Department of Neuropsychiatry, Graduate School of Medicine, Hirosaki University, Hirosaki, Japan; 2Aomori Prefectural Center for Mental Health and Welfare, Aomori, Japan; 3School of Medicine, Hirosaki University, Hirosaki, Japan; 4Department of Urology, Oyokyo Kidney Research Institute, Hirosaki, Japan; 5Department of Social Medicine, Graduate School of Medicine, Hirosaki University, Hirosaki, Japan
Background: We investigated the prevalence of depression in hemodialysis (HD) patients using the Center for Epidemiologic Studies for Depression (CES-D) scale and the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID) and compared the rates with those of community dwelling people in Japan.
Patients and methods: A total of 99 patients undergoing HD were recruited. Blood sampling was performed no later than 2 weeks prior to assessment. As a reference group for SCID and CES-D evaluation, 404 age- and sex-matched healthy controls who had participated in the Iwaki Health Promotion Project were included in this study. The SCID and the CES-D scale were administered to all participants to diagnose their depression. Participants who met the criteria of a major depressive episode according to the SCID were classified as SCID depression and the participants whose CES-D score was 16 or higher were classified as CES-D depression.
Results: Ninety-nine HD patients completed the evaluation and data collection. There were no significant differences in age, sex, or CES-D scores between HD patients and controls. There were 12 cases of SCID depression in HD patients and four cases in controls. There was a significant difference between HD patients and controls in the prevalence of SCID depression. There were no significant differences between the two groups with regard to demographic or clinical data. There were 19 HD patients and 24 controls who showed CES-D depression. There was no significant difference between HD patients and controls in the prevalence of CES-D depression. There was a significant difference in potassium level between the two groups, but there were no significant differences in any of the other items.
Conclusion: There were significantly more HD patients showing SCID depression than controls in the present study. In clinical settings, the SCID might be useful in surveying cases of depression detected by screening tools among HD patients.
Keywords: depression, Center for Epidemiologic Studies for Depression, Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, diagnosis
Introduction
Patients with chronic disease frequently have comorbid psychiatric disease or psychological distress. Many studies have investigated the association between patients with end-stage renal disease (ESRD) or those on hemodialysis (HD) and depression.1–7 A review of the literature shows that 25%–50% of HD patients exhibit depressive symptoms.1,2,8 Although some single-center studies reported that rates of HD patients with depression or major depressive disorder (MDD) were 25%–30%,9–11 a multicenter international study showed large differences in rates between the countries where the investigations were conducted; the rate was 2% in Japan and 21.7% in the USA.12
The Center for Epidemiologic Studies for Depression (CES-D) is frequently used to evaluate depressive symptoms in clinical settings or psychiatric research and was used in previous studies investigating depression in HD patients.12–14 Kim et al13 reported that the rate of depression in Korean HD patients was 75% in their study using CES-D with a cutoff of ≥16. Using the short version of the CES-D and a cutoff of ≥10, Lopes et al12 reported that the rate of depression was 43% in a multicenter international study investigating 9,382 patients.12 In a recent study, Fan et al14 reported that the rate of depression was 26% in HD patients in the USA. Thus, CES-D was used in previous studies with varied results.
In some previous studies, the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (SCID) was used to diagnose depression and MDD. The SCID is based on the DSM-IV and is used to diagnose MDD and other psychiatric disorders. In general, the CES-D is used as a screening tool for depression, and the SCID is considered the gold standard for the clinical diagnosis of depression. Hedayati et al10 investigated depression in HD patients using the CES-D scale and the SCID.10 They reported that the prevalence of depression defined by the SCID was 26.5%. A receiver-operating characteristic curve analysis of SCID data in HD patients demonstrated that a cutoff value of 18 for the CES-D score defined depression in these patients. Arapaslan et al15 investigated the diagnosis of MDD according to the SCID in patients having had successful renal transplantation and reported that the MDD rate was 25%. Kalender et al16 also used the SCID to evaluate depression and reported that the MDD rate in HD patients was 33.8% and that the rate in ESRD patients was 24.1%.
Thus, previous studies have investigated depression in HD and ESRD patients using the CES-D scale and the SCID, but such a study has not been conducted in Japan for Japanese HD patients. The correlation between rates of depression of HD patients and healthy subjects has not been investigated well in previous studies. In the present study, we investigated rates of depression in HD patients using the CES-D scale and the SCID and compared these to rates of depression in healthy controls in Japan; in addition, we aimed to show the utility and reliability of the SCID in evaluating depression among HD patients.
Material and methods
Participants
This study was conducted between June 2014 and April 2014. A total of 99 patients (58 males and 41 females) undergoing HD were recruited from Oyokyo Kidney Research Institute in Japan. This institute is a private center that is located in a rural area of Hirosaki city. The institute has 151 HD stations, and the distribution of the patients is representative of Japanese patients on HD. Clinical information was obtained from medical records. We collected the results of blood examinations to consider whether somatic conditions or HD efficacy might have influenced the psychiatric condition of the patients. Blood sampling was performed no later than 2 weeks prior to assessment. Albumin, total protein, sodium, potassium, uric acid, creatinine, blood urea nitrogen, and the amount of HD were measured by standard analytical techniques.
As a reference group for SCID evaluation, 201 age- and sex-matched healthy volunteers (126 males and 75 females, aged 40 years and above) who participated in the Iwaki Health Promotion Project of 2010 were included. As a reference group for the CES-D scale evaluation, 203 age- and sex-matched healthy volunteers (121 males and 82 females, aged 35 years and above) who participated in the Iwaki Health Promotion Project of 2011 were included.
Two well-trained researchers administered the questionnaires and evaluated patients for depression using the SCID in a multipatient ward as the patients were undergoing HD, while considering patient’s privacy, in Oyokyo Kidney Research Institute. The care providers of the HD patients did not participate as researchers. In total, ten well-trained researchers evaluated subjects in the Iwaki Health Promotion Project. The researchers in the present study were trained by senior psychiatrists using Japanese manuals.
The total study population was 113 patients, and the sample size was determined using the G-power program with an effect size w of 0.34, an α =0.05, and a power (1–β) =0.95 for chi-square (χ2) tests to compare the rate of depression between HD patients and controls. The effect size w was calculated as a result, and we estimated that the prevalence rate of depression in HD patients would be at least twice as high as that of controls.
The study protocols were approved by the Ethics Committee of the Hirosaki University School of Medicine, and all subjects provided written informed consent before participating in this study.
Assessment of depression
The Japanese version of the SCID was administered to all participants to diagnose their depression.17 The interview was conducted by well-trained researchers and psychiatrists. Participants meeting the criteria of a major depressive episode according to the SCID were defined as having SCID depression.
The Japanese version of the CES-D scale was also administered to all participants to measure their depressive status.18 The questionnaire has been widely used to measure depressive symptoms in community populations, and it is also used as a screening tool for depression.19 The CES-D scale is a 20-item, self-report scale that focuses on depressive symptoms within the week prior to administration of the questionnaire. The maximum score is set at 60, and higher scores are associated with depression. CES-D scores of 16 or higher have generally been thought to indicate clinically relevant depressive symptoms, including both minor or subthreshold depression and MDD.20,21 Participants whose CES-D score was 16 or higher were defined as having CES-D depression. In all subjects, Cronbach’s α was 0.802. The Japanese versions of the SCID and CES-D have been used in many previous studies and have been previously validated.22–27
Statistical analysis
We used Student’s t-tests and χ2 tests to compare HD patients and controls with regard to demographic data and depression. We compared the demographic and clinical data of HD patients with and without SCID or CES-D depression, respectively. The data were analyzed using SPSS for Windows 21 (IBM Japan, Tokyo, Japan). A P-value ≤0.05 was considered statistically significant.
Results
Ninety-nine HD patients completed the evaluation, and data were collected from them. Table 1 shows the demographic data and CES-D scores of HD patients and controls. There were no significant differences in age, sex, or CES-D score between HD patients and controls.
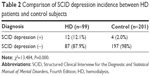
Table 2 shows the prevalence of SCID depression and the results of the χ2 test. There were 12 HD patients and four controls who showed SCID depression. There was a significant difference between HD patients and controls in the prevalence of SCID depression.
Table 3 shows the results of a t-test between HD patients with and without SCID depression. There were no significant differences in demographic or clinical data between the two groups.
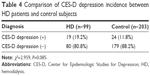
Table 4 shows the prevalence of CES-D depression and the results of the χ2 test. There were 19 HD patients and 24 controls who showed CES-D depression. There was no significant difference between HD patients and controls in the prevalence of CES-D depression.
Table 5 shows the results of the t-test between HD patients with and without CES-D depression. There was a significant difference in potassium level between the two groups, but there were no significant differences in any other items.
Discussion
In the present study, we investigated the prevalence of depression among HD patients using the SCID and the CES-D scale. The prevalence of depression in HD patients was compared to controls. SCID depression was found in 12.1% of HD patients. This rate was significantly higher than that found in controls. There was no significant difference between HD patients and controls in the rate of CES-D depression. This is the first study to compare depression rates between healthy controls and HD patients and showed the superiority of SCID in evaluating depression in HD patients. In Japan, this is the first study to investigate the prevalence of depression evaluated according to the SCID.
The present study found that the SCID is more useful for screening depression in HD patients than the CES-D scale cutoff. Some control subjects with high CES-D scores also had SCID depression; therefore, stricter CES-D scale cutoff values might be useful to reveal the difference between depression rates of HD patients and controls. Hedayati et al10 argued that a CES-D cutoff value of ≥18 was the most accurate means of defining depression according to their study investigating HD patients (Hedayati et al10). A CES-D cutoff value other than ≥16 might be suitable to screen depression among HD patients.
In the present study, the prevalence of SCID depression and CES-D depression among HD patients was lower than the rate reported in previous studies.10,12–14 It is unknown why there is such a difference of prevalence rates between these studies and the present study. There was no significant difference in the duration of HD between the patients with and without depression in the present study. However, the mean duration of HD of the patients included in the previous studies was shorter than that of the patients included in the present study. Thus, the characteristics of the patients included in each of the studies might account for the differences in prevalence rates of depression found in the studies. The detailed investigation of the characteristics of the patients and differences between studies, demographic and laboratory data, personality traits, the cause of HD, quality of life, and social function might make it possible to show a consistent prevalence rate of depression among HD patients.
In total, three HD patients with SCID depression did not have CES-D depression, and ten HD patients with CES-D depression did not have SCID depression. The CES-D scores of the ten patients might reflect a “depressive state” and not depression, thus they might not indicate SCID depression. On the other hand, the three patients who did not have CES-D depression seemed to have depression based on their SCID evaluation.
There was a significant difference in potassium level between the HD patients with and without CES-D depression, but we were not able to clarify why there was such a difference. A previous study reported that depressive state correlates to dietary nonadherence of the HD patients.28 The HD patients with CES-D depression in the present study might show dietary nonadherence because of depressive symptoms leading to greater potassium intake than the HD patients without CES-D depression. However, there was no significant difference in potassium levels between the HD patients with and without SCID depression. Therefore, the depressive state or depressive symptoms might not influence the potassium levels or dietary nonadherence. Characteristics of the HD patients with CES-D depression, other than the depressive state or depressive symptoms, might be associated with the significant difference in potassium levels between the HD patients with and without CES-D depression.
The present study has some limitations. First, the HD patients in the present study did not include all of the HD patients in the hospital. We were not able to investigate the characteristics of the patients hesitant to participate in the study. They might hesitate to participate in the study because of their depressive symptoms or because some of them might have greater depressive symptoms than the patients who participated in the study. Second, there were differences between the date of the laboratory data collections and the interview for evaluation of depression in some participants. The accuracy of the laboratory data in the present study might therefore be limited for these participants. Third, we could not collect information about some factors associated with HD and depression: causes of HD, comorbidities, marital status, and sociodemographic data. Many studies have reported an association between diabetes mellitus and depression.29–31 The difference in utility of the SCID and CES-D might not depend on HD status. An investigation regarding the cause of HD and other factors related to HD and depression might reveal more clinical suggestions than the present study.
Conclusion
In conclusion, we investigated the prevalence of depression among HD patients using the SCID and the CES-D scale and compared the prevalence of depression and the characteristics of HD patients and controls. Significantly more HD patients than controls showed SCID depression in the present study. In the clinical settings, the SCID might be useful to survey depression detected by screening tools among HD patients.
Acknowledgments
The authors thank all of their coworkers on this study for their skillful contributions to collecting and managing the data.
Disclosure
The authors report no conflicts of interest in this work.
References
Kimmel PL, Weihs K, Peterson RA. Survival in hemodialysis patients: the role of depression. J Am Soc Nephrol. 1993;4(1):12–27. | ||
Finkelstein FO, Finkelstein SH. Depression in chronic dialysis patients: assessment and treatment. Nephrol Dial Transplant. 2000;15(12):1911–1913. | ||
Kimmel PL, Peterson RA, Weihs KL, et al. Multiple measurements of depression predict mortality in a longitudinal study of chronic hemodialysis outpatients. Kidney Int. 2000;57(5):2093–2098. | ||
Kimmel PL. Psychosocial factors in dialysis patients. Kidney Int. 2001;59(4):1599–1613. | ||
Lopes AA, Bragg J, Young E, et al. Depression as a predictor of mortality and hospitalization among hemodialysis patients in the United States and Europe. Kidney Int. 2002;62(1):199–207. | ||
Mitrou GI, Grigoriou SS, Konstantopoulou E, et al. Exercise training and depression in ESRD: a review. Semin Dial. 2013;26(5):604–613. | ||
Chilcot J, Spencer BW, Maple H, Mamode N. Depression and kidney transplantation. Transplantation. 2014;97(7):717–721. | ||
Zalai D, Szeifert L, Novak M. Psychological distress and depression in patients with chronic kidney disease. Semin Dial. 2012;25(4):428–438. | ||
Watnick S, Wang PL, Demadura T, Ganzini L. Validation of 2 depression screening tools in dialysis patients. Am J Kidney Dis. 2005;46(5):919–924. | ||
Hedayati SS, Bosworth HB, Kuchibhatla M, Kimmel PL, Szczech LA. The predictive value of self-report scales compared with physician diagnosis of depression in hemodialysis patients. Kidney Int. 2006;69(9):1662–1668. | ||
Cukor D, Coplan J, Brown C, Peterson RA, Kimmel PL. Course of depression and anxiety diagnosis in patients treated with hemodialysis: a 16-month follow-up. Clin J Am Soc Nephrol. 2008;3(6):1752–1758. | ||
Lopes AA, Albert JM, Young EW, et al. Screening for depression in hemodialysis patients: associations with diagnosis, treatment, and outcomes in the DOPPS. Kidney Int. 2004;66(5):2047–2053. | ||
Kim JA, Lee YK, Huh WS, et al. Analysis of depression in continuous ambulatory peritoneal dialysis patients. J Korean Med Sci. 2002;17(6):790–794. | ||
Fan L, Sarnak MJ, Tighiouart H, et al. Depression and all-cause mortality in hemodialysis patients. Am J Nephrol. 2014;40(1):12–18. | ||
Arapaslan B, Soykan A, Soykan C, Kumbasar H. Cross-sectional assessment of psychiatric disorders in renal transplantation patients in Turkey: a preliminary study. Transplant Proc. 2004;36(5):1419–1421. | ||
Kalender B, Ozdemir AC, Koroglu G. Association of depression with markers of nutrition and inflammation in chronic kidney disease and end-stage renal disease. Nephron Clin Pract. 2006;102(3–4):c115–c121. | ||
Takahashi S, Kitamura T, Okano T, Tomita T, Kikuchi A. Japanese Version of Structured Clinical Interview for DSM-VI Axis I Disorders. Tokyo, Japan: Nihon Hyoronsha; 2003. Japanese. | ||
Shima S, Shikano T, Kitamura T, Asai M. New self-rating scales for depression. Clin Psychiatry. 1985; 27:717–723. Japanese. | ||
Zich JM, Attkisson CC, Greenfield TK. Screening for depression in primary care clinics: the CES-D and the BDI. Int J Psychiatry Med. 1990;20(3):259–277. | ||
Beekman AT, Deeg DJ, Van Limbeek J, Braam AW, De Vries MZ, Van Tilburg W. Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): results from a community-based sample of older subjects in the Netherlands. Psychol Med. 1997;27(1):231–235. | ||
Berkman LF, Berkman CS, Kasl S, et al. Depressive symptoms in relation to physical health and functioning in the elderly. Am J Epidemiol. 1986;124(3):372–388. | ||
Kawase E, Karasawa K, Shimotsu S, et al. Evaluation of a one-question interview for depression in a radiation oncology department in Japan. Gen Hosp Psychiatry. 2006;28(4):321–322. | ||
Hayashi N, Igarashi M, Imai A, et al. Psychiatric disorders and clinical correlates of suicidal patients admitted to a psychiatric hospital in Tokyo. BMC Psychiatry. 2010;10:109. | ||
Hayashi N, Igarashi M, Imai A, et al. Pathways from life-historical events and borderline personality disorder to symptomatic disorders among suicidal psychiatric patients: A study of structural equation modeling. Psychiatry Clin Neurosci. 2015;69(9):563–571. | ||
Nagase Y, Uchiyama M, Kaneita Y, et al. Coping strategies and their correlates with depression in the Japanese general population. Psychiatry Res. 2009;168(1):57–66. | ||
Horikawa C, Otsuka R, Kato Y, et al. Cross-sectional association between serum concentrations of n-3 long-chain PUFA and depressive symptoms: results in Japanese community dwellers. Br J Nutr. 2016;115(4):672–680. | ||
Tomitaka S, Kawasaki Y, Ide K, Yamada H, Miyake H, Furukaw TA. Distribution of Total Depressive Symptoms Scores and Each Depressive Symptom Item in a Sample of Japanese Employees. PloS One. 2016;11(1):e0147577. | ||
Khalil AA, Frazier SK. Depressive symptoms and dietary nonadherence in patients with end-stage renal disease receiving hemodialysis: a review of quantitative evidence. Issues Ment Health Nurs. 2010;31(5):324–330. | ||
Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008;31(12):2383–2390. | ||
Baumeister H, Hutter N, Bengel J. Psychological and pharmacological interventions for depression in patients with diabetes mellitus: an abridged Cochrane review. Diabet Med. 2014;31(7):773–786. | ||
Van Der Donk LJ, Pouwer F. Psychological and pharmacological interventions for depression in patients with diabetes mellitus: an abridged Cochrane review: some critical comments. Diabet Med. 2015;32(6):839. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.