Back to Journals » Infection and Drug Resistance » Volume 15
Prevalence of HCV Infection Among Hemodialysis Patients in Lanzhou of Northwestern China
Authors Bao K , Chen J, Liu R, Xiang Y, Gao W
Received 17 June 2022
Accepted for publication 15 September 2022
Published 22 September 2022 Volume 2022:15 Pages 5609—5617
DOI https://doi.org/10.2147/IDR.S378600
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Kai Bao,1,* Jijun Chen,2,* Ruifang Liu,1,3 Yuanyuan Xiang,1 Wenlong Gao1
1Institution of Epidemiology and Health Statistics, School of Public Health, Lanzhou University, Lanzhou, Gansu, People’s Republic of China; 2STD and AIDS Prevention and Control Institute, Lanzhou Municipal Center for Disease Control and Prevention, Lanzhou, Gansu, People’s Republic of China; 3Department of Science and Education, Xi’an No. 5 Hospital, Xi’an, Shanxi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wenlong Gao, Lanzhou University, No. 222 South Tianshui Road, Lanzhou, Gansu, People’s Republic of China, Tel +8613919026975, Email [email protected]
Objective: To investigate the prevalence of hepatitis C virus (HCV) infection among hemodialysis (HD) patients in Lanzhou of Northwestern China, we interviewed 565 patients from five randomly sampled HD centers in Lanzhou with a structured questionnaire including sociodemographic characteristics, past medical history and HD-related factors.
Methods: The testing results of anti-HCV and HCV-RNA in a recent HD from clinical information system were collected. A generalized estimated equation (GEE) logistic regression model was used to identify the determinants of HCV infection among HD patients.
Results: The prevalence of anti-HCV or HCV-RNA infection among HD patients was 1.77% or 1.42% respectively. GEE model showed that history of kidney transplantation (HCV-RNA: OR=19.79, 95%CI: 12.69– 30.85) could dramatically increase the risk of current HCV infection in dialysis patients. Compared with never using of blood products, using of blood products (anti-HCV: OR=2.38, 95%CI: 1.22– 4.64; HCV-RNA: OR=15.23, 95%CI: 1.79– 129.49) could increase the risk of HCV infection in dialysis patients. Moreover, with the increase of HD duration, the risk increased one time or so (anti-HCV: OR=1.83, 95%CI: 1.22– 2.72; HCV-RNA: OR=2.00, 95%CI: 1.11– 3.61). Furthermore, dialysis in multiple hospitals possessed more than three times risk of HCV infection (anti-HCV: OR=3.56, 95%CI: 3.11– 4.08; HCV-RNA: OR=3.35, 95%CI: 1.88– 5.96). Besides, HD patients having the history of acupuncture (HCV-RNA: OR=5.56; 95%CI: 1.16– 26.67) or surgery (HCV-RNA: OR=6.39; 95%CI: 2.86– 14.29) caused an about-six-times risk of current infections.
Conclusion: It could be concluded that the prevalence of HCV infection was mild and using of blood products or kidney transplantation, long dialysis duration, dialysis in multiple hospitals, surgery or acupuncture treatment were some risk factors of HCV infection among HD patients in Lanzhou of Northwestern China.
Keywords: hemodialysis, hepatitis C virus, generalized estimating equation introduction
Introduction
Hepatitis C virus (HCV) infection has become a global health issue that is linked to several hepatic and extrahepatic disorders, including malignancies.1 According to updated WHO estimates, globally 1.75 million new HCV infections occurred and 71 million people were living with HCV infection in 2015, and approximated 399,000 people died from HCV in 2016.2,3 It was generally acknowledged that HCV infection was strongly associated with blood transfusions, unsafe injections and improper medical practices.4 Nevertheless, unsafe health-care procedures and injection drug use were the leading causes of new HCV infections.1,4
Hemodialysis (HD), as one of the important clinical practices for end-stage renal diseases, was often used to treat the patients with extracorporeal circulation and frequent puncture during dialysis which facilitated the transmission of those blood-borne pathogens like HCV. In addition, due to the protracted nature and frequency of HD treatment, HD patients suffered from some adverse health problems such as malnutrition, anemia, and low immunity, which severely weakened the body’s ability to resist pathogens.5,6 As a result, HCV infection became an important complication in end-stage renal failure patients receiving maintenance dialysis. The prevalence of HCV infection among HD patients had been documented, but major variations existed among different geographical regions and over time.1,2 But, this prevalence in developing countries was always higher than that in developed countries.7 Regional studies indeed showed a relatively high HCV prevalence among HD patients in developing countries, ie 10.5% in Brazil,8 25.3% in the Middle East,9 33.5% in northern India,10 50% in Egypt and even as high as 54% in Syria,9 in comparison to the data from those developed countries, such as less than 5% in northern Europe and approximately 10% in most countries of southern Europe and the United States.11 The prevalence of HCV among HD patients, except for the associations of the diverse blood-related factors, patients’ characteristics such as age, race, and longer dialysis vintage, and the history of cirrhosis and golmerulonephritis, hepatitis B virus and HIV positivity, as well as substance abuse were also associated with HCV positivity.12 In addition, a study on gene-related prevalence of HCV also indicated the high risk of dental therapy and surgery on different genotypes of HCV infection.13,14
In China, the HCV prevalence of HD patients was ~4.4% according to sentinel surveillance population,15 which were far higher than that in the general population. Still, nosocomial infection was an important way of contracting HCV infection in HD patients. A recent study showed that the majority of patients with HCV in China were infected via blood transfusion prior to 1996.16 Therefore, it continued to maintain a serious challenge to strengthen the prevention and management of HCV infection in HD patients in China.
At present, few studies on HCV infection in HD patients in northwestern China were reported. A large regional difference in prevalence of HCV infection and the differentiated factors related to HCV infection made it necessary to highlight the regional information that could be used to develop regional, national, and global estimates. Local targeted strategies with the aim of preventing transmission of all blood-borne pathogens also need to be supported with accurate data. Therefore, the current study attempts to explore the prevalence of HCV infection and its correlates in HD patients to provide some insights for clinical prevention and control of HCV infection in HD patients.
Materials and Methods
Sample Population and Data Collection
A cross-sectional survey was conducted in HD centers of five hospitals from April to June 2018, including Gansu Provincial People’s Hospital (Hospital 1), First Hospital of Lanzhou University (Hospital 2), Second Hospital of Lanzhou University (Hospital 3), Lanzhou Municipal First People’s Hospital (Hospital 4) and Lanzhou Municipal Second People’s Hospital (Hospital 5). Those hospitals were selected with a random cluster sampling out of 17 hospitals where HD treatment had been launched in Lanzhou, based on the proportion of the number of dialysis patients in each hospital to the total number of dialysis patients in the 17 hospitals in the year before the survey. In the period of the survey, those patients who accessed the HD centers of five selected hospitals for HD treatment and were willing to provide written informed consent would be interviewed face to face with a structured questionnaire which included sociodemographic information (sex, age, ethnicity, education, marriage, occupation, and family income), HD-related factors (dialyzer reuse, dialysis duration, hemorrhage and multiple hospital dialysis), epidemiological history (kidney transplantation, blood transfusion, using of blood products, surgery, oral therapy, invasive examination, traumatic beauty program, acupuncture therapy of Chinese traditional medicine). All interviewed patients should be aged 14 years or above and were only interviewed for the first time during the survey. The results of their anti-HCV test and HCV-RNA test in the recent HD were obtained from hospital case management systems.
Infection Control in the Hemodialysis Centers in Lanzhou
Iatrogenic infection is one of the important ways of HCV transmission, so it is necessary to improve HCV infection control in hemodialysis centers to block the transmission of HCV. In Lanzhou, all the hemodialysis centers consistently adhered to the principles of early screening, early diagnosis and early treatment. Throughout the management of dialysis patients, these centers conducted timely universal screening of high-risk groups for HCV infection, implemented standard prevention strictly based on the principles of environmental hygiene and infection control, used medical devices safely, equipped with protective equipment reasonably, classified treatment of waste and contaminated items, and implemented safe blood using measures. According to the hospital’s infection management requirements, they cleaned and disinfected dialysis bed units, replaced the associated items and maintained records. In addition, they strengthened health education and training for people at high risk of HCV infection. Their medical staff were trained mainly in occupational exposure prevention and treatment of viral hepatitis and the aseptic concept of nurses to prevent cross-infection.
In the hemodialysis centers, all the dialysis patients tested regularly for anti-HCV and HCV-RNA. Those patients with HCV-RNA+ were consulted by the hepatology department and given antiviral treatment. All patients in routine hemodialysis were screened for HCV infection every six months and examined monthly for liver and kidney function. Hemodialysis patients with anti-HCV+ or HCV-RNA+ received specialized hemodialysis in the infectious disease isolation dialysis treatment area, were given special nurses and equipped with special dialysis operating supplies, and were supplied with the infection control measures strictly during the hemodialysis.
HCV Infection
In the study, anti-HCV and HCV-RNA were tested for each HD patient so those patients with only positive anti-HCV in a recent HD were identified with previous HCV infection and those with positive HCV-RNA in a recent HD were identified with current HCV infection.17
Study Variables
In the current study, previous or current HCV infection was regarded as outcome variables of interest. In the subsequent multivariate analysis, age and dialysis duration of the patients were referred to as the continuous variables. Taking into consideration the downward trend in distribution frequency of patients with the increase of dialysis duration, the true values of dialysis duration were transformed logarithmically. In addition, sex (male/female), ethnicity (the Han/others), education (junior school or below/senior high school or above), marriage (married/others), occupation (employee/others), family income (≤3000CNY/>3000CNY), kidney transplantation (yes/no), blood transfusion (yes/no), use of blood products (yes/no), surgery (yes/no), oral therapy (yes/no), acupuncture therapy of Chinese traditional medicine (yes/no), dialyzer reuse (yes/no) and multiple hospital dialysis (yes/no) as categorical variables were all referred to as potential predictors of HCV infection.
Statistical Analysis
The data obtained from the questionnaire was entered in EpiData 3.0 by dual entry and later statistically analyzed with SPSS v 25.0 (IBM Corporation, Armonk, NY, USA). Enumeration data was described with the rates or proportions, and measurement data with normality were described with mean and standard deviation (SD) and those without normality were described with medium and quartile range (QR). While adjusting for the correlation in prevalence of HCV infection among the participants from the same hospital, the generalized estimating equation (GEE) model was used to explore the correlates of previous or current HCV infection among HD patients. Considering the possible potential interactions among the social demographic variables, epidemiological factors or HD-related factors, we used a multistage modeling technique to assess the associations between the possible predictors and previous or current HCV infection. The specific steps are as follows: Stage 1, only sociodemographic variables were assessed with a GEE logistic regression model (Model 1); Stage 2, epidemiological variables were assessed after controlling for sociodemographic variables with P<0.05 with a GEE logistic regression model (Model 2); Stage 3, HD-related factors together with those variables with P<0.05 from Model 2 were entered into a GEE logistic regression model (Model 3) to obtain the potential predictors of HCV infection among HD patients. The odds ratios (ORs) of those variables entered in each model and 95% confidence interval (95%CI) are estimated. All P-values were two-tailed and at last the level of significance of statistical inference was set to 0.05.
Results
Basic Characteristics, Epidemiological History and HD Conditions
A total of 565 questionnaires were available from the HD centers of five hospitals, including 401 males and 164 females. Of all respondents, 28% came from Hospital 1, 16.1% from Hospital 2, 41.1% from Hospital 3, 12% from Hospital 4 and the rest from Hospital 5. Their average age was 55.30 years with a SD of 14.8 years. Vast majority was Han ethnicity or married. Slightly more than a half received an education of high school or above. About one third was regular employees. Their family income per month was generally low. Less than 3% had a kidney transplant. Just over half had dialysis duration of less than 37 months and their medium dialysis duration was 33 months with a QR from 12 to 54 months. Figure 1 describes the distribution of dialysis duration by sex. With the increase of dialysis duration, the proportion of HD patients at different dialysis time point had an obvious drop regardless of sex. Besides, above a half had never had a blood transfusion, which situation was very similar to use of blood products. Less than 6% had reused dialyzer. Approximately 15% had been on dialysis at multiple hospitals. Less than three-fold had a history of surgery and over three-fold had a history of oral treatment. Slightly below one fifth had been examined invasively. Less than 15% had been acupunctured in the treatment of Chinese traditional medicine. Table 1 depicts basic characteristics, epidemiological history and HD situation of the respondents.
 |
Table 1 Basic Characteristics, Epidemiological History and HD Situation of the Respondents by Hospital. |
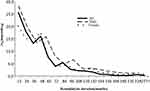 |
Figure 1 The distribution of dialysis duration by sex. |
HCV Infection Among HD Patients
Of all participants, 10 patients were tested anti-HCV positive with a 1.77% positive rate of anti-HCV (95%CI: 0.83%–3.26%, estimated with Poisson distribution) and eight were tested HCV-RNA positive with a 1.42% positive rate of HCV-RNA (95%CI: 0.60%–2.80%, estimated with Poisson distribution).
Risk Factors for HCV Infection Among HD Patients
Table 2 shows the results of multivariate analysis of HCV infection among HD patients using GEE logistic models. The results of GEE logistic regression model showed that history of kidney transplantation could dramatically increase the risk of current HCV infection in dialysis patients (HCV-RNA: OR=19.79, 95%CI: 12.69–30.85). Compared with never using of blood products, using of blood products (anti-HCV: OR=2.38, 95%CI: 1.22–4.64; HCV-RNA: OR=15.23, 95%CI: 1.79–129.49) could increase the risk of HCV infection in dialysis patients, but blood transfusion was not found an increased risk of either previous or current infection. Moreover, while HD duration increased, the risk of HCV infection increased one times or so (anti-HCV: OR=1.83, 95%CI: 1.22–2.72; HCV-RNA: OR=2.00, 95%CI: 1.11–3.61). Furthermore, dialysis in multiple hospitals possessed more than three times risk of HCV infection (anti-HCV: OR=3.56, 95%CI: 3.11–4.08; HCV-RNA: OR=3.35, 95%CI: 1.88–5.96). Besides, HD patients having the history of acupuncture (HCV-RNA: OR=5.56; 95%CI: 1.16–26.67) or surgery (HCV-RNA: OR=6.39; 95%CI: 2.86–14.29) caused an about-six-times risk of current infections. In addition, high family income seemed to be related to low risk of current HCV infection among HD patients.
 |
Table 2 GEE Logistic Regression Model for Previous or Current HCV Infection in Hemodialysis Patients. |
Discussion
This retrospective study estimated the prevalence of HCV infection and explored the associations between some risk factors and HCV infection among HD patients in Lanzhou, Northwestern China. The results of this study showed that the positive rate of anti-HCV among HD patients in Lanzhou was 1.77% which was slightly higher than a 1.42% rate of HCV-RNA+. Compared to that in the general population in China recently (0.91%), the rate of anti-HCV+ was still quite high,18 but much lower than the homochronous result in Romania, Olt county (14.43%),19 which indicated a mild prevalence of HCV infection among HD patients in Lanzhou. Even so, HCV infection could reduce the survival rate of HD patients after renal transplantation and lead to higher risk of death, hospitalization, anemic complications, and worse quality-of-life scores.20,21 So, those HD patients with positive results of any index should be given a higher level of risk warning and appropriate prevention measures should be taken to ensure the safety of other patients uninfected with HCV who were on HD.
The results of the GEE model analysis showed that history of kidney transplantation (HCV-RNA: OR=19.79, 95%CI: 12.69–30.85) could dramatically increase the risk of current HCV infection among HD patients. Infection risk was significantly higher in patients with a history of previous renal transplantation; this has already been demonstrated in other reports. Transplantation and immunosuppression were thought to increase the risk of liver disease and death in HCV-positive dialysis patients. HCV could have been transmitted to these patients from infected organ donors or, more likely, through blood transfusions, which were often required during transplants.22 Compared with never using of blood products, usage of blood products (anti-HCV: OR=2.38, 95%CI: 1.22–4.64; HCV-RNA: OR=15.23, 95%CI: 1.79–129.49) could still increase the risk of current HCV infection among HD patients by more than 14 times, which seemed to hint that the production or use of blood products maybe had a blind in supervision so that it entailed that some targeted measures were urgently implemented to further strengthen the management in the production and sources of blood products, especially human blood products. Before 1998, the paid blood donations in medical institutions or blood stations were not strictly regulated or banned with legislative forms so selling unsafe blood or paying for blood donation in China led to potentially rapid transmission of blood-borne diseases including HCV. Some studies indeed had shown that compared with the blood of unpaid blood donors, HD patients had high HCV infection rates after injecting the blood of paid donors.23 On the contrary, after 1998, blood donation laws standardized the procedure of the blood donation and guaranteed the safety of blood use. The paid blood donation began to be promulgated strictly in China. The blood donors were compulsively examined and tested for HCV. Some temporal observational studies had found that the HCV infection rate of blood donors had decreased significantly since 1998, and the safety of blood transfusion had been greatly improved.24 In the current study, blood transfusion was not a risk factor for HCV infection, which pointed out that a serial of national safeguard strategies for blood donation or blood use was efficient in reducing the transmission of blood-borne diseases like HCV.
The current study found that the duration of HD was significantly associated with the increased risk of HCV infection (anti-HCV: OR=1.83, 95%CI: 1.22–2.72; HCV-RNA: OR=2.00, 95%CI: 1.11–3.61). No wonder that the longer the dialysis duration was, the more risk from iatrogenic infections would accumulate over time, and the possibility of non-standard disinfection of dialysis equipment or nursing environment, rupture of membrane, and bleeding during dialysis operation would increase, which may lead to a greater chance of iatrogenic infection of HCV. Liu et al’s study reported that patients with HD duration for three years or more were more prone to be infected than those with less than three years.25 Su et al’s study also showed that compared with HD patients with dialysis during less than six years, the risk of HCV infection was doubled in dialysis patients with dialysis time of 6–10 years, and the risk of HCV infection among dialysis patients with dialysis time of more than 10 years increased by eight times.26 In addition, multiple hospital dialysis also possessed more than three times the risk of previous or current HCV infection (anti-HCV: OR=3.56, 95%CI: 3.11–4.08; HCV-RNA: OR=3.35, 95%CI: 1.88–5.96). Not at all surprising, the more dialysis hospitals were chosen, the greater the chance of exposure to contaminated blood or equipment was. Some studies also showed that HD at more than one center indicated nosocomial transmission due to inappropriate infection control practices as the main HCV transmission route.27,28
The current study found that patients with a history of acupuncture (HCV-RNA: OR=5.56, 95%CI: 1.16–26.67) could increase the risk of current HCV infection. A previous study reported that a history of acupuncture was a risk factor for HCV infection in patients with HD.29 Certainly, the existence of acupuncture needle reuse and incomplete sanitation in some Chinese medicine clinics could cause possible transmission of blood-borne pathogens such as HCV. So, it was urgent to standardize the use of acupuncture in Chinese medicine and strengthen the management of disinfection. Moreover, in the current study, HD patients having the history of surgery could increase the risk of current HCV infection. Unsterilized medical devices and unprofessional handling in surgery increased the opportunity for the spread of HCV via blood due to more possible exposure to shared materials and the necessity for blood transfusion.30
In the current study, it is worth noting that the number of male patients in HD was more than that of females. Some studies also suggested that there existed sex and gender disparities in related characteristics of chronic kidney disease including its prevalence.31–33
Some limitations of the current study should be acknowledged. First of all, all data on the influencing factors of HCV infection were collected on the basis of patients’ recall, so the estimated results of HCV infection are subject to recall bias. Moreover, incomplete tests of anti-HCV positive and HCV-RNA in all participants maybe led to some bias in data analysis. Finally, for blood transfusion or use of blood products, the numbers of HD patients before 1998 both were a bit small due to short survival duration of patients with HD-related diseases to reduce their test power and yield a big deviation in risk estimation.
In summary, usage of blood products, long dialysis duration and invasive treatment could significantly increase the risk of HCV infection. In the clinical practices, special attention should be paid to strengthening the pre-dialysis HCV monitoring and avoid HCV nosocomial infection among HD patients.
Ethics Approval and Informed Consent
The study complied with the Declaration of Helsinki and was reviewed and approved by the Ethics Committee of Lanzhou Municipal Center for Disease Prevention and Control and written informed consent had been obtained from all the study participants. All kidneys were donated voluntarily with written informed consent and the organ donations were conducted in accordance with the Declaration of Istanbul.
Acknowledgments
We acknowledge the contribution of all staff who participated in this study as well as the study participants who shared their time with us. Kai Bao and Jijun Chen had the same contribution for this study.
Funding
Financial support came from Lanzhou Innovation and Entrepreneurship Project for Talents (2021-RC-109), Lanzhou Health Science and Technology Development Project (2021018) and Health Industry Project of Gansu Province (SWSKY-2019-10).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Thrift AP, El-Serag HB, Kanwal F. Global epidemiology and burden of HCV infection and HCV-related disease. Nat Rev Gastroenterol Hepatol. 2017;14:122–132. doi:10.1038/nrgastro.2016.176
2. World Health Organization. Global hepatitis report; 2017. Available from: https://www.who.int/publications/i/item/9789241565455.
3. World Health Organization. Fact sheets, Hepatitis C; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/hepatitis-C.
4. Spearman CW, Dusheiko GM, Hellard M, et al. Hepatitis C. Lancet. 2019;394:1452–1466. doi:10.1016/S0140-6736(19)32320-7
5. Shergill R, Syed W, Rizvi SA, et al. Nutritional support in chronic liver disease and cirrhotics. World J Hepatol. 2018;10:685–694. doi:10.4254/wjh.v10.i10.685
6. Tsiakalos A, Voumvas T, Psarris A, et al. Circulating autoantibodies to endogenous erythropoietin are associated with chronic hepatitis C virus infection-related anemia. Hepatobiliary Pancreat Dis Int. 2017;16:289–295. doi:10.1016/s1499-3872(16)60131-5
7. Rahnavardi M, Hosseini Moghaddam SM, Alavian SM. Hepatitis C in hemodialysis patients: current global magnitude, natural history, diagnostic difficulties, and preventive measures. Am J Nephrol. 2008;28:628–640. doi:10.1159/000117573
8. Silva LK, Silva MB, Rodart IF, et al. Prevalence of hepatitis C virus (HCV) infection and HCV genotypes of hemodialysis patients in Salvador, Northeastern Brazil. Braz J Med Biol Res. 2006;39:595–602. doi:10.1590/s0100-879x2006000500005
9. Ashkani ES, Alavian SM, Salehi MM. Prevalence of hepatitis C virus infection among hemodialysis patients in the Middle-East: a systematic review and meta-analysis. World J Gastroenterol. 2017;23:151–166. doi:10.3748/wjg.v23.i1.151
10. Malhotra R, Soin D, Grover P, et al. Hepatitis B virus and hepatitis C virus co-infection in hemodialysis patients: a retrospective study from a tertiary care hospital of North India. J Nat Sci Biol Med. 2016;7:72–74. doi:10.4103/0976-9668.175076
11. Söderholm J, Millbourn C, Büsch K, et al. Higher risk of renal disease in chronic hepatitis C patients: antiviral therapy survival benefit in patients on hemodialysis. J Hepatol. 2018;68:904–911. doi:10.1016/j.jhep.2017.12.003
12. Jadoul M, Bieber BA, Martin P, et al. Prevalence, incidence, and risk factors for hepatitis C virus infection in hemodialysis patients. Kidney Int. 2019;95:939–947. doi:10.1016/j.kint.2018.11.038
13. Gómez-Gutiérrez C, Chávez-Tapia NC, Ponciano-Rodríguez G, Uribe M, Méndez-Sánchez N. Prevalence of hepatitis C virus infection among patients undergoing haemodialysis in Latin America. Ann Hepatol. 2015;14:807–814. doi:10.5604/16652681.1171751
14. Petruzziello A, Coppola N, Loquercio G, et al. Distribution pattern of hepatitis C virus genotypes and correlation with viral load and risk factors in chronic positive patients. Intervirology. 2014;57:311–318. doi:10.1159/000363386
15. Ding GW, Ye SD, Hei FX, et al. Sentinel surveillance for viral hepatitis C in China, 2016–2017. Chinese. Chin J Epidemiol. 2019;40:41–45. doi:10.3760/cma.j.issn.0254-6450.2019.01.009
16. Pan Y, Zheng Y, Qin T, et al. Disease progression in Chinese patients with hepatitis C virus RNA-positive infection via blood transfusion. Exp Ther Med. 2016;12:3476–3484. doi:10.3892/etm.2016.3792
17. Guss D, Sherigar J, Rosen P, et al. Diagnosis and management of hepatitis C infection in primary care settings. J Gen Intern Med. 2018;33(4):551–557. doi:10.1007/s11606-017-4280-y
18. Gao Y, Yang J, Sun F, et al. Prevalence of anti-HCV antibody among the general population in mainland china between 1991 and 2015: a systematic review and meta-analysis. Open Forum Infect Dis. 2019;6:888–891. doi:10.1093/ofid/ofz040
19. Caragea DC, Mihailovici AR, Streba CT, et al. Hepatitis C infection in hemodialysis patients. Curr Health Sci J. 2018;44:107–112. doi:10.12865/CHSJ.44.02.02
20. Chapman JR. The KDIGO clinical practice guidelines for the care of kidney transplant. Transplantation. 2010;89:644–645. doi:10.1097/TP.0b013e3181d62f1b
21. Goodkin DA, Bieber B, Jadoul M, et al. Mortality, hospitalization, and quality of life among patients with hepatitis C infection on hemodialysis. Clinical J Am Soc Nephrol. 2017;12:287–297. doi:10.2215/CJN.07940716
22. Pereira BJ, Levey AS. Hepatitis C virus infection in dialysis and renal transplantation. Kidney Int. 1997;51(4):981–999. doi:10.1038/ki.1997.139
23. Hayashi J, Yoshimura E, Nabeshima A, et al. Seroepidemiology of hepatitis C virus infection in hemodialysis patients and the general population in Fukuoka and Okinawa, Japan. J Gastroenterol. 1994;29:276–281. doi:10.1007/BF02358365
24. Gao X, Cui Q, Shi X, et al. Prevalence and trend of hepatitis C virus infection among blood donors in Chinese mainland: a systematic review and meta-analysis. BMC Infect Dis. 2011;11:88. doi:10.1186/1471-2334-11-88
25. Liu YB, Xie JZ, Zhong CJ, et al. Hepatitis C virus infection among hemodialysis patients in Asia: a meta-analysis. Eur Rev Med Pharmacol Sci. 2014;18:3174–3182.
26. Su Y, Yan R, Duan Z, et al. Prevalence and risk factors of hepatitis C and B virus infections in hemodialysis patients and their spouses: a multicenter study in Beijing, China. J Med Virol. 2013;85:425–432. doi:10.1002/jmv.23486
27. Jakupi X, Mlakar J, Lunar MM, et al. A very high prevalence of hepatitis C virus infection among patients undergoing hemodialysis in Kosovo: a nationwide study. BMC Nephrol. 2018;19:304–312. doi:10.1186/s12882-018-1100-5
28. Hinrichsen H, Leimenstoll G, Stegen G, et al. Prevalence and risk factors of hepatitis C virus infection in haemodialysis patients: a multicentre study in 2796 patients. Gut. 2002;51(3):429–433. doi:10.1136/gut.51.3.429
29. Van Remoortel H, Moorkens D, Avau B, Compernolle V, Vandekerckhove P, De Buck E. Is there a risk of transfusion-transmissible infections after percutaneous needle treatments in blood donors? A systematic review and meta-analysis. Vox Sang. 2019;114:297–309. doi:10.1111/vox.12780
30. Vidales-Braz BM, da Silva NM, Lobato R, et al. Detection of hepatitis C virus in patients with terminal renal disease undergoing dialysis in southern Brazil: prevalence, risk factors, genotypes, and viral load dynamics in hemodialysis patients. Virol J. 2015;12:8. doi:10.1186/s12985-015-0238-z
31. Carrero J. Gender differences in chronic kidney disease: underpinnings and therapeutic implications. Kidney Blood Press Res. 2010;33:383–392. doi:10.1159/000320389
32. Cobo G, Hecking M, Port FK, et al. Sex and gender differences in chronic kidney disease: progression to end-stage renal disease and haemodialysis. Clin Sci. 2016;130:1147–1163. doi:10.1042/CS20160047
33. Carrero J, Hecking M, Chesnaye NC, Jager KJ. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat Rev Nephrol. 2018;14:151–164. doi:10.1038/nrneph.2017.181
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
