Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 11
Prevalence of Exclusive Breast Milk Feeding at Discharge and Associated Factors Among Preterm Neonates Admitted to a Neonatal Intensive Care Unit in Public Hospitals, Addis Ababa, Ethiopia: A Cross-Sectional Study
Authors Degaga GT, Sendo EG , Tesfaye T
Received 10 May 2019
Accepted for publication 7 December 2019
Published 20 January 2020 Volume 2020:11 Pages 21—28
DOI https://doi.org/10.2147/PHMT.S215295
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Gosa Tesfaye Degaga, 1 Endalew Gemechu Sendo, 2 Tewodros Tesfaye 2
1Department of Nursing, Ambo University, Ambo, Ethiopia; 2School of Nursing and Midwifery, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Tewodros Tesfaye
School of Nursing and Midwifery, College of Health Sciences, Addis Ababa University, P.O. Box 9086, Addis Ababa, Ethiopia
Tel +251913698081
Email [email protected]
Background: Studies show that rates of breast milk feeding are much lower among preterm infants than term infants, and breast milk feeding at discharge varies widely between countries. However, research examining factors associated with exclusive breast milk feeding at discharge among preterm neonates in Ethiopia is limited. The study aimed to assess the prevalence of exclusive breast milk feeding at discharge and associated factors among preterm neonates at the neonatal intensive care unit (NICU) in public hospitals, Addis Ababa, Ethiopia.
Methods: This facility-based cross-sectional study was conducted from February to March 2017 among preterm infants discharged from the NICU of public hospitals. Data were collected using pretested structured questionnaires. Purposive sampling technique was used. Factors associated with exclusive breast milk-fed infants at discharge among preterm neonates were determined using bivariate and multivariate logistic regression models. Statistically significant associations were declared at P< 0.05.
Results: The study assessed 263 mother-preterm dyads. The findings from this study revealed that 71.9% of exclusive breast milk-fed infants at discharge at NICU of the selected Public hospitals in Addis Ababa. Factors associated with exclusive breast milk-fed infants at discharge included duration of hospital stay for 7– 14 days (AOR 0.19, 95% CI 0.049– 0.808) and more than 14 days (AOR 0.20, 95% CI 0.046,0.891), Initiation of breast milk expression later than 48 hrs postpartum (AOR 0.10, 95% CI 0.032– 0.365) and receiving hospital support (AOR 39.00, 95% CI 11.676– 130.290).
Conclusion: In this study, nearly ¾ of the NICU premature population exclusively breast milk fed at discharge, which designates to establish exclusive breastfeeding in the majority of preterm infants in this cohort. Thus, support for exclusive breast milk fed should be at the forefront of maternity practice in hospital and mothers of preterm infants to be guided to initiation of early breast milk expression as soon after delivery as possible and frequent expression thereafter.
Keywords: breast milk feeding, preterm infant, NICU, Addis Ababa
Introduction
In this study, exclusive breast milk feeding was defined as breast milk obtained from a wet nurse and/or early initiation of breast milk expression in the hospital setting.1 Breast milk is widely recognized as the optimal form of nutrition for infants of all gestational ages.2 Human milk (HM) provides a unique combination of all the nutrients that an infant needs in the first 6 months of life, including fat, carbohydrates, proteins, vitamins, minerals and water.1 Human milk feeding has also been shown to improve neurodevelopment outcomes,3 decrease gastrointestinal and upper respiratory infections4 and lower the risk of sudden infant death syndrome (SIDS).5,6 In addition, the use of human milk in preterm infants, compared to formula, is associated with decreased short-term morbidity such as necrotizing enterocolitis (6), sepsis and meningitis.2
Despite these benefits, the rates of breastfeeding are much lower among preterm infants than term infants, and breast milk fed at discharge varies widely between units and countries from less than 20% to more than 90%.7–10 An Australian retrospective population-based study revealed that late-preterm infants were 70% less likely to initiate breastfeeding, and 60% less likely to be discharged exclusively breast milk fed from hospital when compared to 37-week gestation infants.11 Another study from the Danish national birth cohort reported that at discharge, 68% of the preterm infants were exclusively breast milk fed and 17% partially.12 In Morocco, while 80% of preterm infants received partial breast milk feeding at discharge, only 12.4% were exclusive breastfeeding.13
Suboptimal breast feeding, especially lack of exclusive breastfeeding is the major contributor for infant and child mortality. It attributes 45% of neonatal infectious deaths, 30% of diarrheal deaths and 18% of acute respiratory deaths.13
It is realistic that exclusive breast feeding can significantly reduce the burden of under-5 deaths in Africa particularly sub-Saharan Africa (SSA) where 41% of global under-5 deaths occur mainly due to inadequate breastfeeding practices in combination with high levels of disease.14,15
Breastfeeding-rates of preterm infants at and beyond hospital discharge are reported to vary considerably in the literature. This could possibly be explained by several facilitators and barriers to breast milk feeding in preterm infants. Some of them are related to infants and mothers, while others are related to ward specific factors, i.e., the support the hospital and the NICU offer and the clinical methods used at the NICU. To the best of our knowledge, there are limited research reports on the prevalence of exclusive breast milk feeding and associated factors in preterm infants in Ethiopia. This study aimed to assess prevalence and factors associated with exclusive breast milk feeding among preterm neonates at discharge from neonatal intensive care unit in public hospitals, Addis Ababa, Ethiopia.
Methods
Study Setting and Period
Facility-based cross-sectional study was conducted from February to March 2017 in Addis Ababa Public hospitals. Six hospitals out of 12 were purposively selected for the study as they have basic neonatal intensive care units (NICU). These are Tikur Anbessa Specialised Teaching Hospital, St. Paul Millennium Medical College Specialised Teaching Hospital, Zewditu Memorial Hospital, Gandhi Memorial Hospital, Yekatit 12 Medical College Hospital, and Tirunesh Beijing General Hospital.
Sample Size Determination and Sampling Procedure
Sample size was determined by using single population proportion formula:
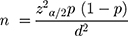
Assumptions: n = required sample size, z α/2 = critical value for normal distribution at 95% confidence level (1.96), P = 50% prevalence (P) of exclusive breastfeeding among preterm, d = 0.05 (margin of error). The formula used for the sample size calculation n = (((zα/2) ^2)* p* (1-p))/d2 led to a number of 384. However, as the study population was <100,000, correction formula was used with 10% for non-response, Nf = 263.
Study Variables
In this study, exclusive breast milk feeding was defined as breast milk obtained from a wet nurse and/or early initiation of breast milk expression in the hospital setting. Exclusive breast milk-fed infants at discharge were the outcome variable. Independent variables included were Maternal factors (age, socioeconomic status, mode of delivery, parity, breast feeding experience, obstetrical condition, and length of hospital stay), factors in infant (low gestation, multiple births, birth weight, gender), and hospital support (supports consistent with baby-friendly initiative ten steps of successful breast feeding, timing of initiation of breast milk expression, kangaroo mother carei.e. skin-to-skin care in Kangaroo position practiced as continuous and intermittent skin-to-skin contact).
Data Collection Tools and Procedures
Data were collected using structured and interviewer-administered questionnaire adapted from the literature.12 First, the questionnaire was prepared in English and translated it into local language [Amharic], and then translated back into English to check its consistency. Five BSc nurses were recruited and trained for 2 days to collect the data. The questionnaire was pretested before actual data collection. The Amharic version was used for data collection.
Data Management and Processing
The data were entered into statistical software Epi-info version 3.5.3 upon creating the questionnaire template in the QES file of the software. The entered data were subjected to cleaning using simple frequency and tabulation to ensure the validity of the data. Then, the analysis was made with IBM SPSS version 21.0 after exporting the prepared data. Descriptive statistics such as frequency distribution was computed to describe the major variables of the study. Odds ratio and p-value were computed to see whether any relationship exists between the two variables under question. P<0.05 was considered as statistically significant for association. Binary logistic regression was conducted to see the effect of each of the independent variables on the outcome variable and variables which showed statically significance at 0.05 level were put into the final model (multivariate analysis) to control for confounding.
Ethical Consideration
Ethical clearance was sought and obtained from Addis Ababa University, College of Health Sciences School of Nursing and Midwifery Ethical Committee. A formal written letter from the committee was given to Addis Ababa Health Bureau and Medical directors of respective hospitals. Objective of the study, benefit and risk of participation in the study, confidentiality of their information, participation on their free will was clearly informed first. Participants of the study were then asked to provide informed voluntary written consent. Assent was also signed by parents for participants under the age of 18 years to be included in the study.
Results
A total of 263 mother-preterm dyads participated in this study with a response rate of 100%.
Neonatal and Maternal Characteristics
The mothers had a mean age of 27.65 years (SD ±5.42) with the range being 16 to 45 years. There were 127(48.3%) females and 136(51.7%) male preterm infants. Single births comprise the highest percentage (80.6%) of babies in this cohort. The mean birth weight of the infants was 1732.19 g (SD ± 523.699g), which ranges from 800g to 3500g (Table1).
 |
Table 1 Neonatal and Maternal Characteristics in Public Hospitals, Addis Ababa, Ethiopia, June 2017 |
Components of Support Provided by Hospital NICU Regarding Breastfeeding Preterm Neonates
Nearly 2/3 of the study subjects, 167(63.5%), reported that they received hospital support services while 96(36.5%) did not. Only 95(36.1%) of the infants had skin-to-skin contact with the mother and less than half 126(47.9%) of the mothers initiated breast milk expression before 48 hrs of postpartum (Table 2).
 |
Table 2 Components of Support Provided by Hospital NICU Regarding Breastfeeding Preterm Neonates in Public Hospitals, Addis Ababa, Ethiopia, 2017 |
Prevalence of Exclusive Breast Milk Feeding
At discharge, 71.9% were exclusively breast milk fed, 20.90% used mixed feeding (Formula and mother’s own milk) whereas 7.2% fed only formula milk at the time of discharge (Figure 1).
 |
Figure 1 Mode of feeding among preterm neonates at discharge from neonatal intensive care unit in public hospitals, Addis Ababa, Ethiopia, 2017. |
Factors Associated with Exclusive Breast Milk Feeding at NICU Discharge
The multivariable analysis showed that delayed initiation of breast milk expression was independently associated with higher odds of failure of exclusive breast milk feeding at discharge (AOR=0.11, 95% CI: 0.032, 0.365). Longer duration of hospital stay was statistically associated with higher odds of failure of exclusive breast milk feeding at discharge. In this study, preterm infants had less than half the odds of exclusive breast milk feeding at 7–14 days or >14 days postpartum as compared with < 7-day postpartum infants (AOR=0.19, 95% CI 0.049–0.808) and (AOR=0.20, 95% CI: 0.046, 0.891) respectively. Moreover, mothers who received continuous hospital support were about 39 times more likely to feed their infants exclusively breast milk than those who received limited hospital support (AOR 39.00, 95% CI 11.676–130.290) (Table 3).
Discussion
This cross-sectional study assessed the prevalence as well as factors associated with exclusive breast milk feeding among preterm neonates at discharge in Public Health Facilities of NICU in Addis Ababa.
The findings from this study revealed that 71.9% of infants fed exclusive breast milk at discharge from NICU, which is slightly lower than the finding reported in a Danish study (68%) in a large preterm cohort.16 However, we found a higher rate of exclusive breast milk feeding at discharge (71.9%%) compared to the study findings in preterm infants of Europe (6–29%), USA (6%), Japan (22.6%) and Morocco (12.4%).7,13,17 The possible explanation for the differences observed between countries could be due to methodological difference employed, definition of breast milk feeding (exclusive or partial), time of investigation of the nutritional method (NICU discharge), and cross-cultural difference in breast milk feeding practice.
The present study also indicates that the initiation of breast milk expression later than 48 hrs of postpartum had a negative correlation to exclusive breast milk feeding, while the length of NICU stay and receiving substantial hospital support showed a positive correlation to exclusive breast milk feeding. Length of NICU stay has been documented in previous studies18,19 reporting difficulty for mothers to supply babies who have a longer hospital stay with a sufficient amount of milk. It is critical to support ongoing and frequent breast milk expression throughout the mother’s postpartum stay as well as throughout her infants’ hospitalization. Early initiation (6 hrs or less postpartum) is important, but mothers will ultimately experience low breast milk production if they are not supported to frequently express their breast milk.
For breast milk feeding failure at discharge, we found that the later the initiation of breast milk expression (> 48-hrs postpartum), the higher the odds for breastfeeding failure at discharge. This is in line with other studies reporting that breast milk expression should be initiated at an early stage after the delivery.19–22
As a bundle of practices, uninterrupted hospital support is strongly predictive of exclusive breastfeeding. Mothers who receive continuous hospital support were about 39 times more likely to feed their infants exclusively breast milk than those who received less hospital support. The finding was supported by similar studies which speculate improvement of exclusive breastfeeding success with clinical practices consistent with UNICEF and WHO Baby-Friendly Hospital Initiative of “Ten Steps” to protect, promote and support breastfeeding in maternity services.12,23–27
Studies have shown that factors such as younger maternal age,7,28 lower educational attainment, lower socioeconomic status,29 having no breast feeding experience,30 caesarean section,11 more prematurity (i.e. very low birth weight, less than 28 weeks)7,11,12,31 and low birth weight7,12,16,31 are associated with decreased success in breast milk provision for preterm infants.
Strengths of the Study
This study is the first to assess the prevalence of exclusive breast milk feeding at discharge and associated factors among preterm neonates at the neonatal intensive care unit (NICU) in public hospitals, Addis Ababa, Ethiopia. Nearly all NICUs in Addis Ababa were participated and a consecutive sample of all preterm infants receiving neonatal intensive care were included in the study. However, this cross-sectional study can only be generalized to this cohort of mother/infant dyads.
Limitation of the Study
This cross-sectional study cannot determine cause and effect. Timing of the study period is also a limitation of the study as results are limited by the cross-sectional time period. The information obtained from mothers could be subject to recall bias.
Conclusion
In this study, nearly ¾ of the NICU premature population exclusively breast milk fed at discharge, which designates to establish exclusive breastfeeding in the majority of preterm infants in this cohort. We found out that hospital support and early initiation of breast milk expression are critical to maternal ability to provide breast milk for her preterm infant at discharge. Thus, support for exclusive breast milk fed should be at the forefront of maternity practice in hospital and mothers of preterm infants to be guided to initiation of early breast milk expression as soon after delivery as possible and frequent expression thereafter.
Acknowledgements
We are indebted to Addis Ababa University, College of Health Sciences for its financial support for data collection. We are indebted to Addis Ababa City Health Bureau for providing us permission to conduct the study in public health facilities. Finally, the authors are also thankful to the study participants and data collectors.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors have no conflicts of interest to disclose.
References
1. World Health Organization. Infant and Young Child Feeding: Model Chapter for Textbooks for Medical Students and Allied Health Professionals. Geneva: WHO; 2009.
2. Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012; 129:e827–e841. Breastfeeding policy statement. Breastfeed Med. 2012;7(5):323–324. doi:10.1089/bfm.2012.0067
3. Kramer MS, Aboud F, Mironova E, et al. Breastfeeding and child cognitive development: new evidence from a large randomized trial. Arch Gen Psychiatry. 2008;65(5):578–584. doi:10.1001/archpsyc.65.5.578
4. Duijts L, Jaddoe VW, Hofman A, Moll HA. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics. 2010;126(1):e18–25. (). doi:10.1542/peds.2008-3256
5. Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics. 2011;128(1):103–110. (). doi:10.1542/peds.2010-3000
6. Hermann K, Carrol K. An exclusively human milk diet reduces necrotizing enterocolitis. Breastfeed Med. 2014;9(4):184–190. doi:10.1089/bfm.2013.0121
7. Härtel C, Hasse B, Browning-Carmo K, et al. Does the enteral feeding advancement affect short-term outcomes in very low birth weight infants? J Pediatr Gastroenterol Nutr. 2009;48(4):464–470. (). doi:10.1097/MPG.0b013e31818c5fc3
8. Krishnamurthy S, Gupta P, Debnath S, Gomber S.Slow versus rapid enteral feeding advancement in preterm newborn infants 1000–1499 g: a randomized controlled trial. ActaPaediatrica. 2010;99(1):42–46.
9. Berrington JE, Heam RI, Bythell M, Wright C, Embleton ND. Deaths in preterm infants: changing pathology over 2 decades. J Pediatr. 2012;160(1):49–53. (). doi:10.1016/j.jpeds.2011.06.046
10. Bonet M, Blondel B, Agostino R, et al. Variations in breastfeeding rates for very preterm infants between regions and neonatal units in Europe: results from the MOSAIC cohort. Arch Dis Child Fetal Neonatal Ed. 2011;96(1):2009–2012.
11. Radtke J. The paradox of breastfeeding-associated morbidity among late preterm infants. J ObstetGynecol Neonatal Nurs. 2011;40:9–24. doi:10.1111/j.1552-6909.2010.01211.x
12. Akerstrom S, Asplund I, Norman M. Successful breastfeeding after discharge of preterm and sick newborn infants. ActaPaediatrica. 2007;96:
13. Flacking R, Nyqvist KH, Ewald U. Effects of socioeconomic status on breastfeeding duration in mothers of preterm and term infants. Eur J Public Health. 2007;17:579–584. doi:10.1093/eurpub/ckm019
14. Ayton J, Hansen E, Quinn S, Nelson M. Factors associated with initiation and exclusive breastfeeding at hospital discharge: late preterm compared to 37 week gestation mother and infant cohort. Int Breastfeed J. 2012;7(1):1–6.
15. Maastrup R, Hansen BM, Kronborg H, Bojesen SN. Breastfeeding progression in preterm infants is influenced by factors in infants, mothers and clinical practice: the results of a national cohort study with high breastfeeding initiation rates. PLoS One. 2014;9:9.
16. Zachariassen G, Faerk J, Grytter C, Esberg B, Juvonen P, Halken S. Factors associated with successful establishment of breastfeeding in very preterm infants. Acta Paediatr. 2010;99(7):1000–1004. doi:10.1111/apa.2010.99.issue-7
17. Hallowell SG, Rogowski JA, Spatz DL, Hanlon AL, Kenny M, Lake ET, International Journal of Nursing Studies. Factors associated with infant feeding of human milk at discharge from neonatal intensive care: cross-sectional analysis of nurse survey and infant outcomes data. Int J Nurs Stud. 2016;53:190–203. doi:10.1016/j.ijnurstu.2015.09.016
18. Imdad A, Yakoob MY, Bhutta ZA. Effect of breastfeeding promotion interventions on breastfeeding rates, with special focus on developing countries. BMC Public Health. 2011;11(Suppl 3):S24.
19. Callen J, Pinelli J. A review of the literature examining the benefits and challenges, incidence and duration, and barriers to breastfeeding in preterm infants. Adv Neonatal Care. 2005;5:72–88. doi:10.1016/j.adnc.2004.12.003
20. Morton J
21. Ohyama M, Watabe H, Hayasaka T. Manual expression and electric breast pumping in the first 48 h after delivery. PediatrInt. 2010;52:39–43.
22. Clemons S, Amir L. Breastfeeding women’s experience of expressing: A descriptive study. J Hum Lact. 2010;26:258–265. doi:10.1177/0890334410371209
23. White-Traut R, Pham T, Rankin K, Norr K, Shapiro N, Yoder J. Exploring factors related to oral feeding progression in premature infants. Adv Neonatal Care. 2014;13(4):288–294.
24. Hwang Y, Ma M, Tseng Y. Associations among perinatal factors and age of achievement of full oral feeding in very preterm infants. Pediatr Neonatol. 2013;54(5):309–314. doi:10.1016/j.pedneo.2013.03.013.
25. Jadcherla SR, Wang M, Vijayapal AS, Leuthner SR. Impact of prematurity and co-morbidities on feeding milestones in neonates: a retrospective study. J Perinatol. 2009;30(3):201–208. doi:10.1038/jp.2009.149.
26. Filippa M, Devouche E, Arioni C, Imberty M, Gratier M. Live maternal speech and singing have beneficial effects on hospitalized preterm infants. ActaPaediatr. 2013;102(10):1017.
27. Picciolini O, Porro M, Meazza A, et al. Early exposure to maternal voice: effects on preterm infant’s development. Early Hum Dev. 2014;90(6):287–292. doi:10.1016/j.earlhumdev.2014.03.003
28. Federal ministry of health: health sector development program IV woreda based annual core plan. Addis Ababa, Ethiopia; 2010.
29. Bhutta Z. Lives Saved Tool (LiST) analysis for global nutrition report independent expert group, Pakistan, Bangladesh, and Ethiopia. 2014;1–30. Available from: globalnutritionreport.org/files/2014/.../gnr14_tn_n4g_02list_analysis.pdf.
30. Cleveland LM. Parenting in the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs. 2008;37(6):666–691. doi:10.1111/j.1552-6909.2008.00288.x
31. World Health Organization. Indicators for assessing infant and young child feeding practices: conclusions of a consensus meeting held 6–8 November 2007 in Washington D.C., USA. WHO, Geneva; 2008. Available from: http://www.unicef.org/nutritioncluster/files/IYCFE_WHO_Part1_eng.pdf.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

